Abstract
Microarrays were used to identify genes of Porphyromonas gingivalis W83 differentially expressed during invasion of primary human coronary artery endothelial cells. Analyses of microarray images indicated that 62 genes were differentially regulated. Of these, 11 genes were up-regulated and 51 were down-regulated. The differential expression of 16 selected genes was confirmed by real-time PCR.
Several epidemiological studies have led to the hypothesis of an infection theory of atherosclerosis (31, 39). An accumulation of evidence suggests that periodontopathogenic bacterial species, among others, may be involved in cardiovascular diseases (1, 8, 22, 29, 30, 32). In addition to these data, there is also biological evidence for such a relationship. For example, periodontal pathogens can be detected in atheromas dissected from vascular tissues (17), and Porphyromonas gingivalis has been shown to accelerate atherosclerosis in apolipoprotein E-deficient mice (16, 26, 28). In addition, several studies have demonstrated that P. gingivalis internalizes within arterial endothelial cells and smooth muscle cells in vitro (7, 10) and can also induce foam cell formation and secretion of monocyte chemoattractants, both important phenomena in atherosclerotic lesion formation (25). Most recently, a direct correlation between the presence of P. gingivalis in periodontal plaque and the progression of atherosclerosis (9), as well as the isolation of viable P. gingivalis from atherosclerotic tissue (24), has been reported. P. gingivalis is known to have a direct route to the circulatory system in periodontitis patients (3, 38). Therefore, invasion of coronary artery cells by P. gingivalis may be involved in atherosclerosis.
To identify genes differentially expressed during the course of P. gingivalis invasion of human coronary artery endothelial cells (HCAEC), T-75 flasks with 90% confluence of HCAEC were infected with P. gingivalis strain W83 for 2.5 h as described previously (11, 27). Total RNA was isolated from both 10 ml of broth culture (prior to invasion) and internalized bacteria by using 10 ml of Trizol reagent followed by RNA isolation as described by the manufacturer (Invitrogen Life Technologies, Carlsbad, CA). All RNA samples were DNase treated and purified using the RNeasy kit (QIAGEN Inc., Valencia, CA). To separate bacterial total mRNA from poly(A) mRNA, cellular and internalized bacterial RNAs were also treated with the Oligotex kit (QIAGEN) according to the manufacturer's instructions and the supernatant (invasion RNA) was again treated with Trizol LS reagent (Invitrogen Life Technologies). Reverse transcription (RT) and microarray reactions were performed either with 2.0 μg of total bacterial RNA (control) or with invasion RNA (200 μg of total RNA containing 2.0 μg of bacterial RNA), collected from one T-75 flask of invaded HCAEC (per microarray slide), as previously described (14, 37). Details of the microarrays can be found at http://www.tigr.org. The resulting images were analyzed by TIGR Spotfinder 1.0 and TIGR Multiple Experiment Viewer software 1.2 (The Institute for Genomic Research [TIGR] [http://www.tigr.org]). The generated files were imported into Microsoft Excel (Microsoft Corporation, Redmond, WA) for subsequent analyses. The results represent the common findings of three independent biological replicate arrays performed with three different RNA samples. Genes were identified as differentially expressed if there was a 2.0-fold difference in their average expression values. To confirm the microarray data, 16 different genes were subjected to RT-PCR (Table 1) using an iCycler Thermal Cycler and iQ SYBR green supermix according to the manufacturer's instructions (Bio-Rad Laboratories). DNA fragments of each gene were used as internal controls and standard curves. Subsequent data normalization and analysis were performed by using the iCycler and Microsoft Excel softwares. All locus numbers and operon predictions were obtained from the website for TIGR.
TABLE 1.
Comparison of RT-PCR and microarray expression values of selected genes
| Locus no.a | Putative identificationa | Expression value
|
|
|---|---|---|---|
| RT-PCRc | Microarrayb | ||
| PG0092 | Transporter, putative | 15.12 | 5.37 |
| PG0120 | UDP-N-acetylglucosamine 2-epimerase | −9.01 | −12.46 |
| PG0186 | Lipoprotein RagB | −1.59 | −13.27 |
| PG0195 | Rubrerythrin | 1.33 | −6.15 |
| PG0280 | ABC transporter, permease protein, putative | 9.01 | 6.67 |
| PG0686 | Conserved hypothetical protein | 23.84 | 10.51 |
| PG1116 | Methylenetetrahydrofolate dehydrogenase/methenyltetrahydrofolate cyclohydrolase | 25.06 | 4.63 |
| PG1172 | Iron-sulfur cluster binding protein, putative | 94.51 | 3.57 |
| PG1286 | Ferritin | 23.01 | 2.72 |
| PG1321 | Formate-tetrahydrofolate ligase | 11.19 | 5.73 |
| PG1492 | Hypothetical protein | −71.35 | −4.50 |
| PG1682 | Glycosyl transferase, group 1 family protein | 6.21 | 3.63 |
| PG1683 | Conserved hypothetical protein | 359.52 | 2.96 |
| PG1795 | Hypothetical protein | −5.28 | −7.92 |
| PG1864 | Leucine-rich protein | −60.67 | −6.69 |
| PG1896 | S-Adenosylmethionine synthase | 16.93 | 3.51 |
| PG2064 | Hypothetical protein | −3.34 | 5.19 |
Locus number and putative identification are according to the TIGR P. gingivalis genome database.
Expression values are expressed as average experimental intensities/average control intensity.
Expression values are expressed as average experimental starting quantity/average of control starting quantity.
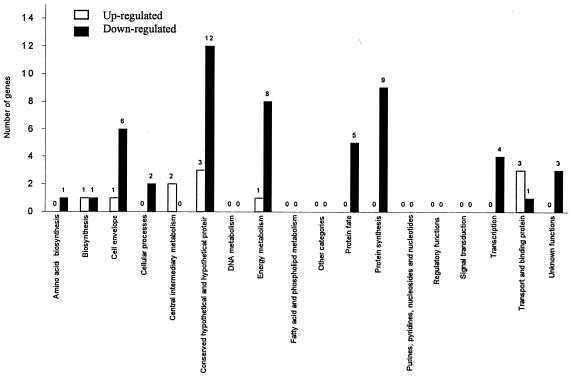
Analysis of microarray images showed that a total of 63 genes were differentially regulated (Fig. 1). Of these genes, 11 were up-regulated (Table 2) and 52 were down-regulated (Table 3) during invasion of HCAEC, compared with those growing in broth culture. Among the up-regulated genes are several that may be involved in intracellular trafficking and/or interactions with autophagosomal vesicles or other virulence functions. Examples are as follows. (i) PG1682 encodes a glycosyl transferase, and PG1683 encodes a conserved hypothetical protein which has homology to α-amylases. These enzymes have been suggested to be involved in the attachment of P. gingivalis to epithelial cells (glycosyl transferase) (4) and coaggregation of P. gingivalis with other oral bacterial species (hypothetical protein) (15, 23). Genes PG1682 and PG1683 might also be involved in the coaggregation of P. gingivalis with cell membranes (autophagosomes). (ii) PG0280 encodes a putative ABC transporter permease protein that is organized as a channeling pore complex through the membrane (34). The ABC transporter superfamily is responsible for the translocation of a wide variety of substances into or out of cells. However, the substrate of this particular ABC transporter has not yet been described. (iii) PG0092 encodes a putative transporter of unknown substrate which belongs to the HlyD secretion protein family (34). The HlyD family of secretion proteins is involved in the activation and release of hemolysins in Escherichia coli (19, 41, 42) as well as in the secretion of toxins in other bacterial species (18, 21). Perhaps related, PG1286 (ftn) encodes a ferritin and PG1172 encodes a putative iron-sulfur cluster binding protein, a prosthetic group present in a diverse set of proteins involved in environmental sensing, gene regulation, and substrate activation. (iv) PG1896 (metk) encodes an S-adenosylmethionine synthase, the product of which is S-adenosylmethionine (SAM), a major methyl donor in metabolism. SAM is an essential metabolite in yeasts (5), and the lack of SAM in E. coli cells has been shown to result in a cell division defect (35). In previous work in our laboratory, Dorn et al. (12) observed profiles of P. gingivalis dividing inside late autophagosomes. Therefore, PG1896 could be involved in intracellular replication of P. gingivalis. However, its up-regulation may be due to other metabolic processes necessary for the survival of P. gingivalis inside of HCAEC.
FIG. 1.
Distribution of differentially expressed genes grouped by functional classification according to the TIGR P. gingivalis genome database. Numbers above the bars indicate the number of genes differentially expressed in each functional group.
TABLE 2.
P. gingivalis genes up-regulated during invasion of human coronary artery endothelial cells
| Locus no. | Putative identificationa | Cellular rolea | Expression valueb |
|---|---|---|---|
| PG0092 | Transporter, putative | Transport and binding protein | 5.37 |
| PG0280 | ABC transporter, permease protein, putative | Transport and binding protein | 6.67 |
| PG0686 | Conserved hypothetical protein | Hypothetical protein | 10.51 |
| PG1116 | Methylenetetrahydrofolate dehydrogenase/methenyltetrahydrofolate cyclohydrolase | Biosynthesis of cofactors, prosthetic groups, and carriers | 4.63 |
| PG1172 | Iron-sulfur cluster binding protein, putative | Energy metabolism | 3.57 |
| PG1286 | Ferritin | Transport and binding protein | 2.72 |
| PG1321 | Formate-tetrahydrofolate ligase | Central intermediary metabolism | 5.73 |
| PG1682 | Glycosyl transferase, group 1 family protein | Cell envelope | 3.63 |
| PG1683 | Conserved hypothetical protein | Hypothetical protein | 2.96 |
| PG1896 | S-Adenosylmethionine synthase | Central intermediary metabolism | 3.51 |
| PG2064 | Hypothetical protein | Hypothetical protein | 5.19 |
Locus number, identification and functional classification are according to the TIGR P. gingivalis genome database.
Expression values are expressed as average experimental intensities/average control intensity.
TABLE 3.
P. gingivalis genes down-regulated during invasion of human coronary artery endothelial cells
| Locus no. | Putative identificationa | Cellular rolea | Expression valueb |
|---|---|---|---|
| PG0120 | UDP-N-acetylglucosamine 2-epimerase | Cell envelope | 12.46 |
| PG0121 | DNA-binding protein HU | Cell envelope | 4.70 |
| PG0145 | Hypothetical protein | Hypothetical protein | 14.60 |
| PG0176 | Cell surface protein, interruption | Cell envelope | 16.35 |
| PG0178 | Cell surface protein, interruption | Cell envelope | 9.29 |
| PG0186 | Lipoprotein RagB | Cell envelope | 13.27 |
| PG0195 | Rubrerythrin | Energy metabolism | 6.15 |
| PG0272 | Gliding motility protein GldE, putative | Cellular processes | 8.12 |
| PG0288 | Lipoprotein, putative | Cell envelope | 5.79 |
| PG0315 | Ribosomal protein L27 | Protein synthesis | 5.74 |
| PG0375 | Ribosomal protein L13 | Protein synthesis | 3.93 |
| PG0389 | Transcription antitermination protein NusG | Transcription | 24.85 |
| PG0390 | Ribosomal protein L11 | Protein synthesis | 7.59 |
| PG0392 | Ribosomal protein L10 | Protein synthesis | 14.78 |
| PG0616 | Thioredoxin, putative | Energy metabolism | 12.29 |
| PG0618 | Alkyl hydroperoxide reductase, C subunit | Cellular processes | 4.22 |
| PG0687 | Succinate-semialdehyde dehydrogenase | Energy metabolism | 6.71 |
| PG0689 | NAD-dependent 4-hydroxybutyrate dehydrogenase | Energy metabolism | 16.24 |
| PG0762 | Trigger factor, putative | Protein fate | 6.69 |
| PG0779 | Hypothetical protein | Hypothetical protein | 7.83 |
| PG0780 | Hypothetical protein | Hypothetical protein | 10.79 |
| PG0992 | Threonyl-tRNA synthetase | Protein synthesis | 9.35 |
| PG1078 | Electron transfer flavoprotein, alpha subunit | Energy metabolism | 12.55 |
| PG1084 | Thioredoxin family protein | Energy metabolism | 14.60 |
| PG1105 | RNA polymerase sigma-54 factor | Transcription | 5.08 |
| PG1153 | Hypothetical protein | Hypothetical protein | 4.85 |
| PG1189 | Hypothetical protein | Hypothetical protein | 6.52 |
| PG1256 | Ribonuclease, Rne/Rng family | Transcription | 15.55 |
| PG1265 | Hypothetical protein | Hypothetical protein | 8.33 |
| PG1304 | Hypothetical protein | Hypothetical protein | 3.89 |
| PG1492 | Hypothetical protein | Hypothetical protein | 4.50 |
| PG1602 | YibR protein | Unknown function | 12.45 |
| PG1703 | MazG family protein | Unknown function | 11.44 |
| PG1788 | Cysteine peptidase, putative | Protein fate | 19.58 |
| PG1795 | Hypothetical protein | Hypothetical protein | 7.92 |
| PG1807 | v-type ATPase, subunit K | Energy metabolism | 3.46 |
| PG1823 | Hypothetical protein | Hypothetical protein | 4.28 |
| PG1864 | Leucine-rich protein | Unknown function | 6.69 |
| PG1911 | DNA-directed RNA polymerase, alpha subunit | Transcription | 26.25 |
| PG1913 | Ribosomal protein S11 | Protein synthesis | 5.34 |
| PG1917 | Methionine aminopeptidase, type I | Protein fate | 17.61 |
| PG1918 | Preprotein translocase, SecY subunit | Protein fate | 24.52 |
| PG1926 | Ribosomal protein L5 | Protein synthesis | 12.25 |
| PG1935 | Ribosomal protein L2 | Protein synthesis | 9.48 |
| PG1937 | Ribosomal protein L4 | Protein synthesis | 9.86 |
| PG1944 | 3-Phosphoshikimate 1-carboxyvinyltransferase | Amino acid biosynthesis | 6.23 |
| PG1956 | 4-Hydroxybutyrate coenzyme A-transferase | Energy metabolism | 6.82 |
| PG1973 | Hypothetical protein | Hypothetical proteins | 1.86 |
| PG1974 | Hypothetical protein | Hypothetical proteins | 59.99 |
| PG2082 | POT family protein | Transport and binding proteins | 6.04 |
| PG2192 | Peptidase, M23/M37 family | Protein fate | 6.71 |
| PG2205 | 2-Dehydropantoate 2-reductase, putative | Biosynthesis of cofactors, prosthetic groups, and carriers | 19.30 |
Locus number, identification and functional classification according to TIGR P. gingivalis genome database.
Expression values are expressed as average experimental intensities/average control intensity.
In contrast to genes up-regulated during invasion assays, a larger number of genes (52 of 63) were down-regulated (Table 3). Several of the down-regulated genes (12 of 52) are hypothetical proteins; however, a substantial number of down-regulated genes (21 of 52) are likely involved in protein synthesis, transcription, and energy metabolism. This reduced level of expression may indicate a reduced intracellular bacterial growth rate and/or that intracellular P. gingivalis organisms at this time point have limited but more specific metabolic activity when compared with laboratory-grown late-log-phase bacteria.
This is the first report of a global genomic expression profile of intracellular P. gingivalis during invasion of endothelial host cells. The results presented here may provide new insights at the molecular level of P. gingivalis gene expression once inside human cells. It is expected that the gene expression profiles will differ at earlier or later times during invasion of HCAEC cultures. Similarly, P. gingivalis genetic expression profiles would be expected to differ in different cell lines, since P. gingivalis traffics intracellularly differently in different cell types (2, 6, 12, 13, 20, 33, 36, 40). We are currently studying these genes and their products to better understand the invasive mechanism of P. gingivalis.
Acknowledgments
This work was supported by grant NIH DE013545.
We thank The Institute for Genomic Research (Rockville, MD) for kindly providing the microarray slides supported by NIH DE10510 and Henry Baker and Cecilia Lopez for advice and assistance with array screening.
Editor: J. B. Bliska
REFERENCES
- 1.Arbes, S. J., Jr., G. D. Slade, and J. D. Beck. 1999. Association between extent of periodontal attachment loss and self-reported history of heart attack: an analysis of NHANES III data. J. Dent. Res. 78:1777-1782. [DOI] [PubMed] [Google Scholar]
- 2.Belton, C. M., K. T. Izutsu, P. C. Goodwin, Y. Park, and R. J. Lamont. 1999. Fluorescence image analysis of the association between Porphyromonas gingivalis and gingival epithelial cells. Cell Microbiol. 1:215-223. [DOI] [PubMed] [Google Scholar]
- 3.Carroll, G. C., and R. J. Sebor. 1980. Dental flossing and its relationship to transient bacteremia. J. Periodontol. 51:691-692. [DOI] [PubMed] [Google Scholar]
- 4.Chen, T., H. Dong, R. Yong, and M. J. Duncan. 2000. Pleiotropic pigmentation mutants of Porphyromonas gingivalis. Microb. Pathog. 28:235-247. [DOI] [PubMed] [Google Scholar]
- 5.Cherest, H., and Y. Surdin-Kerjan. 1978. S-adenosyl methionine requiring mutants in Saccharomyces cerevisiae: evidences for the existence of two methionine adenosyl transferases. Mol. Gen. Genet. 163:153-167. [DOI] [PubMed] [Google Scholar]
- 6.Deshpande, R. G., M. Khan, and C. A. Genco. 1998. Invasion strategies of the oral pathogen Porphyromonas gingivalis: implications for cardiovascular disease. Invasion Metastasis 18:57-69. [DOI] [PubMed] [Google Scholar]
- 7.Deshpande, R. G., M. B. Khan, and C. A. Genco. 1998. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect. Immun. 66:5337-5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeStefano, F., R. F. Anda, H. S. Kahn, D. F. Williamson, and C. M. Russell. 1993. Dental disease and risk of coronary heart disease and mortality. BMJ 306:688-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desvarieux, M., R. T. Demmer, T. Rundek, B. Boden-Albala, D. R. Jacobs, Jr., R. L. Sacco, and P. N. Papapanou. 2005. Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Circulation 111:576-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorn, B. R., J. N. Burks, K. N. Seifert, and A. Progulske-Fox. 2000. Invasion of endothelial and epithelial cells by strains of Porphyromonas gingivalis. FEMS Microbiol. Lett. 187:139-144. [DOI] [PubMed] [Google Scholar]
- 11.Dorn, B. R., W. A. Dunn, Jr., and A. Progulske-Fox. 1999. Invasion of human coronary artery cells by periodontal pathogens. Infect. Immun. 67:5792-5798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dorn, B. R., W. A. Dunn, Jr., and A. Progulske-Fox. 2001. Porphyromonas gingivalis traffics to autophagosomes in human coronary artery endothelial cells. Infect. Immun. 69:5698-5708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duncan, M. J., S. Nakao, Z. Skobe, and H. Xie. 1993. Interactions of Porphyromonas gingivalis with epithelial cells. Infect. Immun. 61:2260-2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dziejman, M., E. Balon, D. Boyd, C. M. Fraser, J. F. Heidelberg, and J. J. Mekalanos. 2002. Comparative genomic analysis of Vibrio cholerae: genes that correlate with cholera endemic and pandemic disease. Proc. Natl. Acad. Sci. USA 99:1556-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellen, R. P., G. Lepine, and P. M. Nghiem. 1997. In vitro models that support adhesion specificity in biofilms of oral bacteria. Adv. Dent. Res. 11:33-42. [DOI] [PubMed] [Google Scholar]
- 16.Gibson, F. C., III, C. Hong, H. H. Chou, H. Yumoto, J. Chen, E. Lien, J. Wong, and C. A. Genco. 2004. Innate immune recognition of invasive bacteria accelerates atherosclerosis in apolipoprotein E-deficient mice. Circulation 109:2801-2806. [DOI] [PubMed] [Google Scholar]
- 17.Haraszthy, V. I., J. J. Zambon, M. Trevisan, M. Zeid, and R. J. Genco. 2000. Identification of periodontal pathogens in atheromatous plaques. J. Periodontol. 71:1554-1560. [DOI] [PubMed] [Google Scholar]
- 18.Highlander, S. K., M. J. Engler, and G. M. Weinstock. 1990. Secretion and expression of the Pasteurella haemolytica leukotoxin. J. Bacteriol. 172:2343-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holland, I. B., B. Kenny, and M. Blight. 1990. Haemolysin secretion from Escherichia coli. Biochimie 72:131-141. [DOI] [PubMed] [Google Scholar]
- 20.Houalet-Jeanne, S., P. Pellen-Mussi, S. Tricot-Doleux, J. Apiou, and M. Bonnaure-Mallet. 2001. Assessment of internalization and viability of Porphyromonas gingivalis in KB epithelial cells by confocal microscopy. Infect. Immun. 69:7146-7151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jansen, R., J. Briaire, A. B. van Geel, E. M. Kamp, A. L. Gielkens, and M. A. Smits. 1994. Genetic map of the Actinobacillus pleuropneumoniae RTX-toxin (Apx) operons: characterization of the ApxIII operons. Infect. Immun. 62:4411-4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joshipura, K. J., H. C. Wand, A. T. Merchant, and E. B. Rimm. 2004. Periodontal disease and biomarkers related to cardiovascular disease. J. Dent. Res. 83:151-155. [DOI] [PubMed] [Google Scholar]
- 23.Kamaguch, A., K. Nakayama, T. Ohyama, T. Watanabe, M. Okamoto, and H. Baba. 2001. Coaggregation of Porphyromonas gingivalis and Prevotella intermedia. Microbiol. Immunol. 45:649-656. [DOI] [PubMed] [Google Scholar]
- 24.Kozarov, E. V., B. R. Dorn, C. E. Shelburne, W. A. Dunn, Jr., and A. Progulske-Fox. 2005. Human atherosclerotic plaque contains viable invasive Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis. Arterioscler. Thromb. Vasc. Biol. 25:e17-e18. [DOI] [PubMed] [Google Scholar]
- 25.Kuramitsu, H. K., I. C. Kang, and M. Qi. 2003. Interactions of Porphyromonas gingivalis with host cells: implications for cardiovascular diseases. J. Periodontol. 74:85-89. [DOI] [PubMed] [Google Scholar]
- 26.Lalla, E., I. B. Lamster, M. A. Hofmann, L. Bucciarelli, A. P. Jerud, S. Tucker, Y. Lu, P. N. Papapanou, and A. M. Schmidt. 2003. Oral infection with a periodontal pathogen accelerates early atherosclerosis in apolipoprotein E-null mice. Arterioscler. Thromb. Vasc. Biol. 23:1405-1411. [DOI] [PubMed] [Google Scholar]
- 27.Lamont, R. J., A. Chan, C. M. Belton, K. T. Izutsu, D. Vasel, and A. Weinberg. 1995. Porphyromonas gingivalis invasion of gingival epithelial cells. Infect. Immun. 63:3878-3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li, L., E. Messas, E. L. Batista, Jr., R. A. Levine, and S. Amar. 2002. Porphyromonas gingivalis infection accelerates the progression of atherosclerosis in a heterozygous apolipoprotein E-deficient murine model. Circulation 105:861-867. [DOI] [PubMed] [Google Scholar]
- 29.Mattila, K. J., M. S. Nieminen, V. V. Valtonen, V. P. Rasi, Y. A. Kesaniemi, S. L. Syrjala, P. S. Jungell, M. Isoluoma, K. Hietaniemi, and M. J. Jokinen. 1989. Association between dental health and acute myocardial infarction. BMJ 298:779-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattila, K. J., M. S. Valle, M. S. Nieminen, V. V. Valtonen, and K. L. Hietaniemi. 1993. Dental infections and coronary atherosclerosis. Atherosclerosis 103:205-211. [DOI] [PubMed] [Google Scholar]
- 31.Mehta, J. L., T. G. Saldeen, and K. Rand. 1998. Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary artery disease. J. Am. Coll. Cardiol. 31:1217-1225. [DOI] [PubMed] [Google Scholar]
- 32.Meurman, J. H., S. J. Janket, M. Qvarnstrom, and P. Nuutinen. 2003. Dental infections and serum inflammatory markers in patients with and without severe heart disease. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 96:695-700. [DOI] [PubMed] [Google Scholar]
- 33.Nakhjiri, S. F., Y. Park, O. Yilmaz, W. O. Chung, K. Watanabe, A. El-Sabaeny, K. Park, and R. J. Lamont. 2001. Inhibition of epithelial cell apoptosis by Porphyromonas gingivalis. FEMS Microbiol. Lett. 200:145-149. [DOI] [PubMed] [Google Scholar]
- 34.Nelson, K. E., R. D. Fleischmann, R. T. DeBoy, I. T. Paulsen, D. E. Fouts, J. A. Eisen, S. C. Daugherty, R. J. Dodson, A. S. Durkin, M. Gwinn, D. H. Haft, J. F. Kolonay, W. C. Nelson, T. Mason, L. Tallon, J. Gray, D. Granger, H. Tettelin, H. Dong, J. L. Galvin, M. J. Duncan, F. E. Dewhirst, and C. M. Fraser. 2003. Complete genome sequence of the oral pathogenic bacterium Porphyromonas gingivalis strain W83. J. Bacteriol. 185:5591-5601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Newman, E. B., L. I. Budman, E. C. Chan, R. C. Greene, R. T. Lin, C. L. Woldringh, and R. D'Ari. 1998. Lack of S-adenosylmethionine results in a cell division defect in Escherichia coli. J. Bacteriol. 180:3614-3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Njoroge, T., R. J. Genco, H. T. Sojar, N. Hamada, and C. A. Genco. 1997. A role for fimbriae in Porphyromonas gingivalis invasion of oral epithelial cells. Infect. Immun. 65:1980-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peterson, S., R. T. Cline, H. Tettelin, V. Sharov, and D. A. Morrison. 2000. Gene expression analysis of the Streptococcus pneumoniae competence regulons by use of DNA microarrays. J. Bacteriol. 182:6192-6202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts, G. J. 1999. Dentists are innocent! “Everyday” bacteremia is the real culprit: a review and assessment of the evidence that dental surgical procedures are a principal cause of bacterial endocarditis in children. Pediatr. Cardiol. 20:317-325. [DOI] [PubMed] [Google Scholar]
- 39.Ross, R. 1999. Atherosclerosis—an inflammatory disease. N. Engl. J. Med. 340:115-126. [DOI] [PubMed] [Google Scholar]
- 40.Sandros, J., P. N. Madianos, and P. N. Papapanou. 1996. Cellular events concurrent with Porphyromonas gingivalis invasion of oral epithelium in vitro. Eur. J. Oral Sci. 104:363-371. [DOI] [PubMed] [Google Scholar]
- 41.Trent, M. S., L. M. Worsham, and M. L. Ernst-Fonberg. 1998. The biochemistry of hemolysin toxin activation: characterization of HlyC, an internal protein acyltransferase. Biochemistry 37:4644-4652. [DOI] [PubMed] [Google Scholar]
- 42.Wang, R. C., S. J. Seror, M. Blight, J. M. Pratt, J. K. Broome-Smith, and I. B. Holland. 1991. Analysis of the membrane organization of an Escherichia coli protein translocator, HlyB, a member of a large family of prokaryote and eukaryote surface transport proteins. J. Mol. Biol. 217:441-454. [DOI] [PubMed] [Google Scholar]