Abstract
Evidence for the effectiveness of existing treatments of patients with eating disorders is weak. Here we describe and evaluate a method of treatment in a randomized controlled trial. Sixteen patients, randomly selected out of a group composed of 19 patients with anorexia nervosa and 13 with bulimia nervosa, were trained to eat and recognize satiety by using computer support. They rested in a warm room after eating, and their physical activity was restricted. The patients in the control group (n = 16) received no treatment. Remission was defined by normal body weight (anorexia), cessation of binge eating and purging (bulimia), a normal psychiatric profile, normal laboratory test values, normal eating behavior, and resumption of social activities. Fourteen patients went into remission after a median of 14.4 months (range 4.9–26.5) of treatment, but only one patient went into remission while waiting for treatment (P = 0.0057). Relapse is considered a major problem in patients who have been treated to remission. We therefore report results on a total of 168 patients who have entered our treatment program. The estimated rate of remission was 75%, and estimated time to remission was 14.7 months (quartile range 9.6 ≥ 32). Six patients (7%) of 83 who were treated to remission relapsed, but the others (93%) have remained in remission for 12 months (quartile range 6–36). Because the risk of relapse is maximal in the first year after remission, we suggest that most patients treated with this method recover.
Eating disorders, i.e., anorexia and bulimia nervosa, are serious health problems in young women (less than 5% of patients are men), characterized by a disordered intake of food. Thus, anorexics eat only small amounts of food and lose body weight; bulimics eat large quantities of food and vomit or use other methods to maintain normal body weight. About 1% of all women develop anorexia at the age of 14–19 years, and 1–3% develop bulimia when 20–23 years old (1). Anorexics have less than a 50% chance of recovery within 10 years after the onset of the disorder, 25% develop into chronicity, and mortality can be as high as 25% (2). Bulimics have a better prognosis, but fewer than 50% recover, and 30% continue to binge eat and purge (2, 3).
There is a considerable amount of data on the time course and outcome of anorexia and bulimia nervosa (2–4), but the effect of treatment interventions has not been extensively evaluated. Hence, there is little scientific evidence for the selection of one kind of treatment rather than another. In fact, it was recently pointed out that the effects of most treatments are unknown (5). Evaluation of medical interventions should be done in randomized controlled trials (RCT) (6). Three RCTs have compared treatment effects in young anorexic patients. In the first, family therapy was effective in comparison with individual therapy in 10 patients who had been ill for about 1 year and who had been treated on average once before (7). The treatment had no effect in 70 other patients who participated in the trial. Similar results were obtained in the two other RCTs (8, 9). The RCTs that have been done on older anorexic patients have shown minor effects (10–12). The effectiveness of cognitive behavioral therapy in bulimia has been established in RCTs (13, 14), but only 50% of bulimic patients respond to treatment (13). Pharmacological treatment has not been effective in treating anorexia nervosa (15) but has some effect in patients with bulimia (16, 17).
The lack of effective treatment may be because there are relatively few physiologically plausible hypotheses of how eating disorders develop and how they are maintained (18). In an attempt to improve this situation, we pointed out that there are two known risk factors for anorexia: dieting and increased physical activity (19). Experiments on animals have shown that both these risk factors activate the mesolimbic dopaminergic reward and the locus coeruleus noradrenergic attention pathways in the brain (19). It might be hypothesized, therefore, that anorexia develops because it is initially rewarding to eat less and move more, and that subsequently anorexic behavior becomes conditioned to the stimuli that originally provided the reward because the brain's network for attention has been activated (19). Although this hypothesis is admittedly speculative and needs to be tested, it is realistic and may therefore serve as a theoretical starting point. From our perspective, psychopathology (20) is considered a consequence, not a cause, of starvation. Similarly, hypothermia (21) and a further increase in physical activity (22) emerge in the state of starvation.
Bulimics show all of the symptoms listed above, including hypothermia (23) and physical hyperactivity (24), and a psychopathology similar to that of anorexics (2). Bulimics differ from anorexics mainly in that they eat excessive amounts of food in a short period and vomit and are of normal weight (25). However, dieting may be a risk factor for bulimia (26), anorexics often develop bulimia (2), and a subgroup of anorexics show bulimic eating behavior (25). Thus, while their physical appearance is different, the similarities between the two groups of patients are more conspicuous than the differences. There is no compelling reason, therefore, to believe that bulimia develops from a different cause than does anorexia. Consequently, it should be possible to treat both groups of patients similarly.
With this framework, we have developed a treatment directed at the following symptoms: (i) disordered eating behavior and altered perception of satiety; (ii) hypothermia; (iii) physical hyperactivity; and (iv) disordered social life.
We have reported preliminary results in anorexic patients by using this method (27) and now report the results of a pragmatic RCT. Because it has been reported that almost half of the anorexic patients who have been treated to remission relapse within 1 year (4) and that many bulimics in remission may develop alternative eating disorder symptoms (28), we also report the rate of remission and relapse in a large group of patients treated with our method.
RCT: Participants and Methods
Selection of Patients.
Consecutively referred patients who fulfilled the diagnostic criteria for anorexia or bulimia nervosa (25), including two males, participated, but those with an eating disorder not otherwise specified (EDNOS) (25) or who required immediate medical care [body mass index (BMI)12 kg/m2, bradycardia (≤40 beats per minute), and hypokalemia (≤3.2 mmol/liter)] were excluded. The study was approved by the Ethics Committee at Huddinge University Hospital. Informed consent was obtained from all patients.
Randomization and Size of Study.
We used a computer-generated randomization list to assign patients to treatment or deferred treatment. On the basis of preliminary results (27), the latter group had to wait at least 7 months for treatment. Randomization was done in blocks of four consecutive patients at the time of the initial evaluation (see below). Treatment allocations were kept in numbered sealed envelopes.
We estimated that 80% of treated patients would be in remission within a period of 24 months, and that a maximum of 20% of the untreated patients would go into remission spontaneously. This estimation was based on the preliminary study of eight anorexic patients who went into remission after a median of 7 months (range 3.5–14) of treatment (27). We also took into consideration that it was not possible to start treating patients immediately after assignment, for practical reasons. With a one-sided log–rank survival test, 14 patients in each group were estimated to give a power of about 90%. In addition, we considered the possibility that some patients would have to be withdrawn or would drop out of the treatment program. Therefore, we allotted 16 patients to each group. These were selected out of 47 patients, from which we excluded 10 with an EDNOS and five anorexics who needed immediate medical attention.
Initial Evaluation.
Patients were evaluated in 1 day and returned 9 days later for information about the results. During the evaluation, the medical status of the patients was examined in detail.
Eating disorder history and psychopathology.
Patients were interviewed in detail concerning the development of their eating disorders and physical activity. They also completed the Comprehensive Psychopathological Rating Scale Self-Rating Scale for Affective Syndromes (CPRS-SA), which estimates state of depression, anxiety, and obsession (29). In addition, they filled out the Eating Disorder Inventory, a self-rating questionnaire estimating the state of the eating disorder (30).
Patient characteristics.
Some characteristics of patients are shown in Table 1. The patients in the treatment and control group were similar with regard to these characteristics and therefore were not kept separate. The patient with a BMI of 10.8 was 10 years old. One female patient with bulimia suffered from diabetes mellitus, but no diseases were present in other patients.
Table 1.
Some characteristics of the patients
| Variable | Anorexia nervosa (n = 19) | Bulimia nervosa (n = 13) |
|---|---|---|
| Age | 16 (10–33) | 19 (15–54) |
| Duration of disorder, years | 2 (0–21) | 4 (0–14) |
| BMI, kg/m2 | 15 (10.8–17.5) | 21.6 (17.9–31.8) |
| No. of previous treatments | 3 (1–3) | 2 (1–15) |
| Daily binge eating | 2* | 11 |
| Daily vomiting | 4* | 10 |
| Attempted/considered suicide | 3/9 | 5/6 |
| Psychopharmacological drugs | 8 | 2 |
| Alcohol (≥60 g/week) | 0 | 4 |
| Smoking (≥20 cigarettes/day) | 0 | 5 |
| Headache | 7 | 7 |
| Nausea | 5 | 7 |
| Fatigue | 12 | 10 |
| Insomnia | 11 | 7 |
| Dyspepsia/constipation | 10 | 10 |
| Lanugo hair | 8 | 0 |
| Menstruation | 0 | 10 |
| Heart rate | 46 (34–60) | 60 (50–72) |
| Blood pressure | 95/60 (85–127/60–90) | 110/75 (100–140/60–80) |
Refers to anorexic, binge-eating/purging type. Data are median and range.
Intervention.
In- and out-patient treatment.
Four patients with a BMI13.5 kg/m2, bradycardia (40 bpm), and /or hypokalemia (3.2 mmol/liter), and/or binge-eating and vomiting (5 times/day) were treated as in-patients during a median of 28.5 days (range 8–30). All others were treated as out-patients. The number of treatment occasions were gradually reduced from five per week to one per week to one every other week.
Body weight.
Anorexic patients were asked to indicate the weight gain that they could accept, with no less than a 2-kg gain accepted as their goal. When this weight was reached, a new weight was negotiated. Normal-weight bulimic patients were informed that their body weight would not change, and overweight bulimics were told that their weight would decrease. All patients were informed that psychiatric symptoms would decrease when their eating behavior normalized.
Initiation of eating.
Two patients, who initially did not eat in front of the monitor described below, were trained to eat by adopting the Skinnerian principle of successive approximations (31). Thus, food was placed on the plate, patients placed empty forks in their mouths, food was placed on the fork, patients were encouraged to smell the food, and so forth. After three and six daily training sessions, patients started to eat in front of the monitor.
Feedback on eating and satiety.
Once per day, the patient ate from a plate situated on a scale embedded in a table. The scale was connected to a computer, which stored the weight loss of the plate. Regular warm meals (Findus, Bjuv, Sweden) were served. At 1-min intervals, a rating scale (32) appeared on a monitor, and the patient recorded her/his level of satiety by using a computer mouse. The computer stored the satiety ratings. The satiety scale has the following values: none at all (0), extremely weak (0.5), very weak (1), weak (2), moderate (3), strong (5), very strong (7), extremely strong (10), and an option “absolute maximum,” corresponding to the highest possible level, which has no numerical value. This system, Mandometer (AB Mando, Stockholm), allows simultaneous recording of eating rate and satiety.
After preliminary testing, patients were presented with a linear curve for eating rate and asked to follow the curve on the computer monitor while eating. This is possible, because the patient can see her/his rate of eating appear continuously on the monitor during the meal. The training aimed at teaching both anorexics and bulimics to ingest 350 g during 10–15 min.
During training sessions, a hypothetical curve for normal satiety was shown. The curve was a cubic spline interpolation of values generated by 10 healthy volunteers who ate on average 350 g in 11 min. Their eating rate was linear. The satiety values started at 0 and ended at 6.
The training curve for the eating rate always looked the same, but its values were modified on average twice (range 1–4) during treatment with a median of 35 days (range 10–72) between each change. Thus, anorexic patients ate progressively more food, and bulimics ate less, with a 20% increase and decrease in intake, respectively, at each modification of their training curves. The same satiety curve was shown throughout the treatment.
Supply of external heat.
After each meal, the patients rested for 1 h in a room in which they could set the temperature at up to 40°C.
Physical activity.
Anorexic patients were placed in wheel chairs or were allowed to walk slowly within the clinic. Bulimic patients were allowed to walk slowly for 30 min/day together with a member of the staff. Restrictions of physical activity were gradually reduced and, at time of remission, such restrictions were withdrawn.
Feeding schedule.
Breakfast was served between 7:00 and 8:00 a.m.; the first breakfast consisted of 1.5 dl of yogurt, a sandwich, 2 dl of orange juice, and a cup of tea or coffee. Every fourth week during treatment, the patients were encouraged to add a sandwich, but they were not asked to eat more than two sandwiches. Lunch was served between 11:30 a.m. and 12:30 p.m. by using the Mandometer procedure. Dinner was served between 4:30 and 5:30 p.m., and the amount of food was the same as that served for lunch. Each meal ended with a nutritional supplement (Nutricia, Meda, Sweden), which was withdrawn by the end of treatment. A snack was provided between meals. After 4 months of treatment, patients ate together and at restaurants with a member of the staff.
Social schedule.
Short-term goals, such as getting a haircut or joining friends at a café, as well as long-term goals, such as starting school, were determined, and the patients were told that normal eating behavior would enable them to reach these goals. All young patients went to school 1 h per day until an average of 2 months before remission, when they returned to full-time schooling. Older patients were offered work as volunteers in the community, and those previously employed returned to work. Treatment goals were modified every second week.
Drug treatment.
Cisapride (Prepulsid, 10–30 mg/day, Janssen-Cilag, Beerse, Belgium) was used to enhance gastric motility in seven anorexic patients, but psychopharmacological drugs, prescribed by the referring physician, were withdrawn and not given during treatment.
Patients in the control group.
Patients in the control group received no treatment while waiting for treatment. They were examined once more when they entered the treatment program.
Assessment of Outcome.
To be considered in remission, a patient could no longer meet the criteria for an eating disorder (25). The return of menstruation, however, was not used as a criterion for remission in anorexic patients for reasons mentioned in the Discussion. Bulimic patients should have stopped binge eating for at least 3 months. In addition, body weight, psychiatric profile, and laboratory tests had to be normal, the patients had to be able to state that food and dieting were no longer problems, and they had to be back in school or in professional activities.
Remission and Relapse: Participants and Methods
Patients.
Results from 168 patients who entered our treatment program between its start on October 28, 1993 and October 31, 2000 are reported. Of these, 85 fulfilled the criteria for anorexia nervosa, 38 fulfilled the criteria for bulimia nervosa, and 45 fulfilled the criteria for an EDNOS (25). Five (3%) were males. The characteristics of the patients, including those with an EDNOS, were similar to those in Table 1 (data not shown), and 52 (31%) of were treated as in-patients.
Followup.
Patients were examined 3, 6, 9, 12, 18, 24, 36, 48, and 60 months after remission. BMI was determined, patients filled out the Comprehensive Psychopathological Rating Scale Self-Rating Scale for Affective Syndromes and Eating Disorder Inventory questionnaires, and they were interviewed concerning ongoing treatment, use of drugs, social situation, menstruation, and eating patterns. The examination lasted 2.5 hours. If a patient had lost 4 kg of her/his body weight or had developed signs of binge eating/purging, the examination procedure described above was repeated, and if the patient fulfilled the criteria of an eating disorder (25), she/he was defined as having relapsed.
Statistical Analysis.
Time to remission was evaluated by using survival analysis (Kaplan–Meier plot and log-rank tests) (33) until the time at which the last patient in the control group entered the treatment program. Waiting time between allocation and start of treatment was included in the analysis. Data are expressed as median and range.
All patients were included in the analysis of the rate of remission and relapse in the larger group. Those who had withdrawn from treatment were considered not in remission at the end of the observation period. Data are expressed as median and quartile range. Time to remission, withdrawal, and relapse was estimated by using survival analysis. Time to remission between different diagnostic groups was compared with the χ2 test.
Results
RCT.
Patient withdrawal and censoring of data.
One patient in the control group withdrew consent after 1 day, and three other patients appeared in the emergency ward because of worsening symptoms 2.6, 3.1, and 6.5 months after entering the study. Data from these patients were censored at the corresponding times.
Patient outcome.
Patients in the treatment group waited to be treated for a median of 1.3 months (range 0–14.6) after initial evaluation, and those in the control group waited for 17.5 months (range 7.1–21.6).
Time to remission was similar in anorexics and bulimics, and the data were therefore combined.
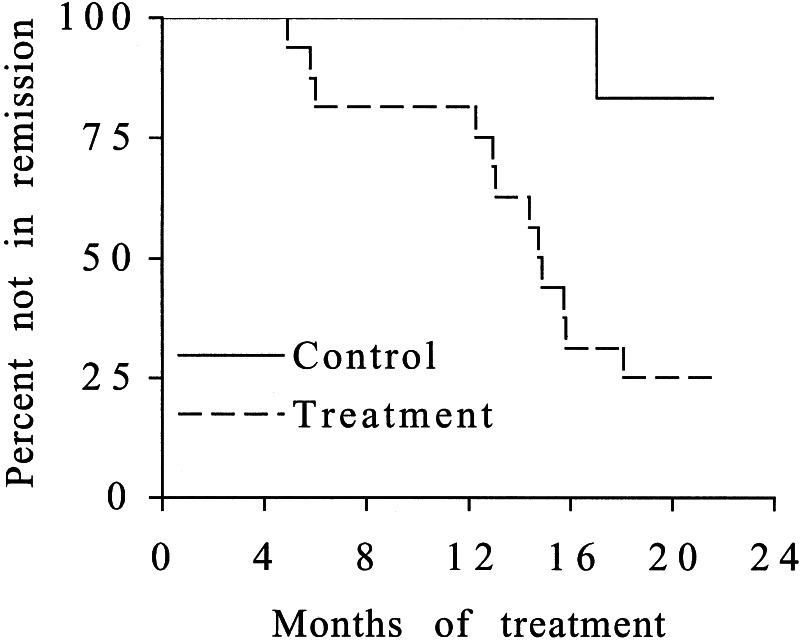
Treatment had a major effect on remission rates; 14 of 16 patients in the treatment group were in remission after a median of 14.4 months (range 4.9–26.5). By contrast, only one of the 16 patients in the control group went into remission during the 21.6-month observation period (P = 0.0057; Fig. 1).
Figure 1.
Kaplan–Meier plot of the number of patients in remission (%) in a group of 16 anorexic or bulimic patients who were treated and another group of 16 anorexic or bulimic patients who were waiting to be treated.
With the exception of the three patients who became acutely ill, patients in the control group were in a similar condition at the initial investigation (Table 1) and by the time they entered the treatment program (data not shown).
Eating behavior.
Initially, the bulimics ingested food twice as quickly [median 27.1 g/min (range 11.9–32.6)] as the anorexics [median 12 g/min (range 2.9–17.3)]. By the end of the training, the anorexic patients ate approximately the same amount of food [median 325 g (range 198–360)] as the bulimics [median 326 g (range 243–343)], and their eating rate [median 24.2 g/min (range 9.8–33.4)] was similar to that of the bulimics [26 g/min (range 22.9–28.3)]. At remission, anorexics and bulimics ate three regular meals per day.
BMI, psychopathology, medical status, and social adjustment.
BMI had increased to the normal level among the anorexic patients at remission, whereas that of the bulimics was unchanged (Table 2). The patient with a BMI of 15.4 was 11 years old.
Table 2.
BMI and psychopathology at admission and remission
| Variable | Anorexia
nervosa (n = 10)
|
Bulimia nervosa
(n = 4)
|
||
|---|---|---|---|---|
| Admission | Remission | Admission | Remission | |
| BMI, kg/m2 | 14.5 (10.8–17.6) | 18.6 (15.4–19.9) | 20.7 (19.3–23.2) | 21.3 (20.5–22.5) |
| Depression | 7.0 (3.0–20.0) | 1.0 (0.0–3.5) | 8.0 (5.0–13.0) | 2.0 (0.5–6.5) |
| Anxiety | 6.5 (3.0–22.0) | 1.5 (0.0–4.5) | 5.0 (4.5–7.5) | 2.0 (0.0–3.0) |
| Obsession | 8.0 (2.5–20.0) | 2.0 (0.5–3.0) | 8.0 (4.0–10.5) | 1.5 (1.0–7.0) |
| Eating disorder inventory | 81 (43–151) | 31 (19–56) | 106 (76–149) | 28 (21–61) |
Data are median and range.
Anorexic patients scored lower on the psychopathology and eating disorder scales after treatment than before (Table 2). The ratings of the bulimic patients were similar to those of the anorexics (Table 2).
None of the symptoms noted at admission (Table 1) were observed at remission except amenorrhea in seven anorexics.
Only four of the patients were in school or had a job at admission, but all were back in school on a full-time basis or had a job after treatment.
Remission and Relapse
Remission and Withdrawal.
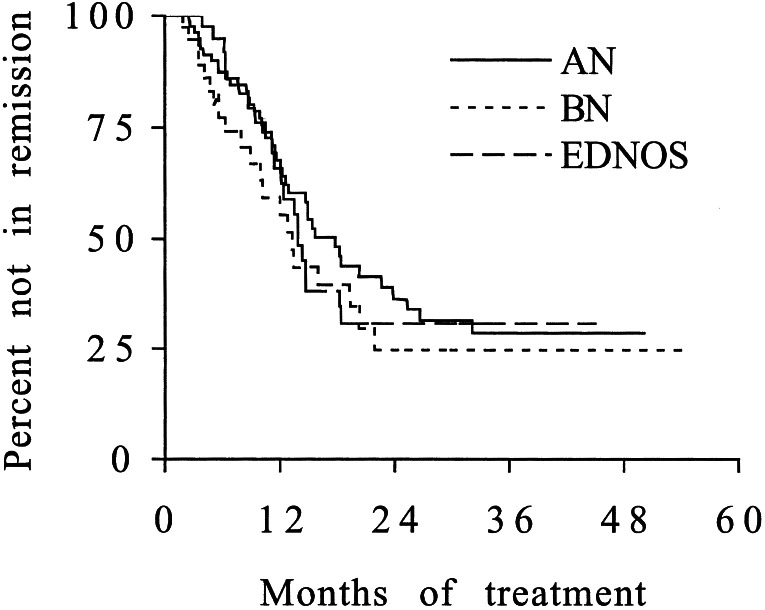
Eighty-three patients (49%) went into remission after a median of 11.8 months (quartile range 6.2–14.8) of treatment, 23 (14%) withdrew from treatment after a median of 19.6 months (quartile range 9.7–25.3), and 62 (37%) were in treatment for a median of 6.8 months (quartile range 3.7–10.9). These results gave an estimated time to remission of 14.7 months (quartile range 9.6 ≥ 32) and an estimated rate of remission of about 75% (Fig. 2).
Figure 2.
Kaplan–Meier plot of the number of eating disorder patients in remission (%) in a group of 168 patients.
There was no difference in time to remission depending on the diagnosis of the patient (χ2 = 2.24, NS, Fig. 3).
Figure 3.
Kaplan–Meier plot of the number of patients in remission (%) in a group of 85 patients with anorexia nervosa (AN), 38 patients with bulimia nervosa (BN), and 45 patients with an EDNOS.
Patients who withdrew from treatment did not do so at any specific time during treatment. Nine of these patients were in partial remission. Thus, they were back in school and social activities, or their eating behavior was normal. However, their BMI might not have been normal, or they might have had an episode of binge eating/purging despite a long period without bingeing.
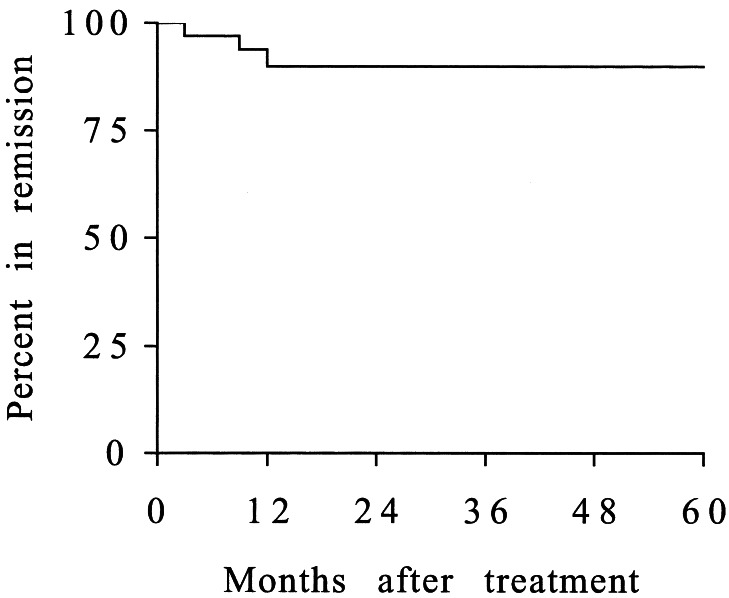
Relapse and Recovery.
The 83 patients who went into remission appeared for a median of 90% (quartile range 70–100) of their followup examinations. Six (7%) patients relapsed during the first year of followup, but the others (93%) remained free of symptoms for a median of 12 months (quartile range 6–36) (Fig. 4). None of the patients who were in remission participated in an alternative treatment program or received psychopharmacological drugs.
Figure 4.
Kaplan–Meier plot of the number of patients in remission (%) in a group of 83 patients treated to remission.
Thirty of the 41 (75%, one was a male) anorexic patients who went into remission menstruated after a median of 3 months (quartile range 0–9), and time to menstruation was estimated to be 3 months (quartile range 0–14.7) after remission. All but two bulimics and three patients with an EDNOS did not menstruate at remission, but these patients menstruated regularly within 6 months.
Discussion
There is one previous study in which the effect of treatment of a group of anorexic patients was compared with a control group that received no treatment (11). However, compliance was a problem; 14 of the 20 patients in the control group (70%) left to receive treatment outside the study protocol. In all other studies, the effect of one treatment has been compared with that of another one. This procedure has most likely been followed because of the consensus view that anorexic patients must be treated for prolonged periods of time (4); it is difficult for ethical reasons, therefore, not to treat patients. Similarly, the effect of treatment in bulimia has not been evaluated against an untreated control group (13, 14). As has been pointed out (5, 9), the precise effect of most treatment interventions is, therefore, unknown. However, because our preliminary results showed that the time to remission was short (27), the local ethics committee allowed us to assign patients randomly to treatment versus no treatment. Random assignment obviously is an essential requirement of RCT (6) and, because we obtained a significant effect, we conclude that our treatment has a beneficial effect in patients with anorexia or bulimia nervosa.
It is possible that the favorable outcome reported here depended on some characteristic of the patients. However, they had been ill for a considerable period, which is common in treatment studies of patients with eating disorders. Moreover, their medical and psychiatric status at admission was similar to that of patients in other studies. In addition, all of the patients had been treated before without success, which is likely to affect outcome negatively (2, 4). Also, the patients were consecutive referrals, and only those requiring immediate medical attention or not meeting the criteria for anorexia or bulimia nervosa were excluded. Thus, the present method of treatment is effective in a heterogenous group of patients that was selected by using a minimum of exclusion criteria to mimic the typical clinical setting.
When in remission, our patients showed neither eating disorder symptoms nor any other psychiatric symptoms, had normal laboratory test values, were back in school or had started to work, and also fulfilled other measures of social functioning. However, we did not include onset of menstruation as a criterion for remission, because some patients suffer from primary amenorrhea and have therefore not experienced all physiological events of puberty. We do not think that such a delay of normal physiology is indicative of an eating disorder, and most of our patients start menstruating during followup assessments.
In a comprehensive review of more than 150 long-term outcome studies of patients with anorexia nervosa, it was reported that about half of the patients achieve a good or intermediate outcome (4). A similar outcome was reported in a more recent study in which 103 patients were followed up for 6 years after receiving a variety of treatments, including relapse prevention (34). However, less than 25% of the patients were in full remission at followup. In a study reporting a better outcome, time to remission was very long, on average 6.6 years (35). Thus, there are very few published reports of effective treatments for patients with anorexia nervosa, and this conclusion is underscored in another recent review (2). By contrast, estimated time to remission was about 14 months, and the probability of going into remission was estimated to be about 75% in a large group of our patients.
One study reported a low rate of relapse in anorexic patients treated to remission with family therapy (36), but it is more often found that between 30 and 50% of anorexic patients in remission relapse within a year (2, 4, 34). Studies of bulimic patients have yielded better results (28, 37), but only a few followup studies have been reported because of the relative recency of a specific diagnosis of bulimia nervosa (2).
Because the rate of relapse is maximal within 1 year of remission, we follow our patients for a longer period. The patients appear for most of their followup appointments. By the time the present study was closed, half of the 83 patients treated to remission had been followed for at least 1 year after remission. Most of these patients remained free of symptoms. Also, the six patients that relapsed did so within the first year after cessation of treatment. These results suggest that most patients treated to remission with our method recover from their eating disorders. The results also support our suggestion that patients with eating disorders can be treated with this method independent of their diagnoses.
Although these results are promising, we realize the necessity to further develop our method. For example, we need to determine whether one of our interventions is more important than another as well as whether our procedures should be modified. Most important, however, is that an RCT comparing this method with the standard of care for eating disorders is required. However, replacement of a standard of care by any new method must also take the associated cost into consideration. It is noteworthy, therefore, that the estimated cost of the present method is considerably below that of other methods (38).
Acknowledgments
The cooperation of the patients is greatly appreciated. We thank Mss. Monica Calmar and Barbro Olofsson for collecting data from followup appointments and Prof. M. Leon, University of California, Irvine, CA, for helpful comments on the manuscript. This study was supported by grants from the Swedish Council for Research in Humanities and Social Sciences and the Vardal Foundation.
Abbreviations
- RCT
randomized controlled trial
- BMI
body mass index
- EDNOS
eating disorder not otherwise specified
References
- 1.Lewinsohn P M, Striegel-Moore R H, Seeley J R. J Am Acad Child Adolesc Psychiatry. 2000;39:1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Steinhausen H-C. In: Risks and Outcomes in Developmental Psychopathology. Steinhausen C-H, Verhulst F, editors. Oxford, U.K.: Oxford Univ. Press; 1999. pp. 210–230. [Google Scholar]
- 3.Keel P K, Mitchell J E, Miller K B, Davis T L, Crow S J. Arch Gen Psychiatry. 1999;56:63–69. doi: 10.1001/archpsyc.56.1.63. [DOI] [PubMed] [Google Scholar]
- 4.Pike K M. Clin Psychol Rev. 1998;18:447–475. doi: 10.1016/s0272-7358(98)00014-2. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Tovim D I, Walker K, Gilchrist P, Freeman R, Kalucy R, Esterman A. Lancet. 2001;357:1254–1257. doi: 10.1016/S0140-6736(00)04406-8. [DOI] [PubMed] [Google Scholar]
- 6.Pocock S J, Elbourne D R. N Engl J Med. 2000;342:1907–1909. doi: 10.1056/NEJM200006223422511. [DOI] [PubMed] [Google Scholar]
- 7.Russell G F, Szmukler G I, Dare C, Eisler I. Arch Gen Psychiatry. 1987;44:1047–1056. doi: 10.1001/archpsyc.1987.01800240021004. [DOI] [PubMed] [Google Scholar]
- 8.Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D. J Child Psychol Psychiatry. 2000;41:727–736. [PubMed] [Google Scholar]
- 9.Robin A I, Siegel P T, Moye A W, Gilroy M, Dennis A B, Sikand A. J Am Acad Child Adolesc Psychiatry. 1999;38:1482–1489. doi: 10.1097/00004583-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Channon S, de Silva P, Hemsley D, Perkins R. Behav Res Ther. 1987;27:529–535. doi: 10.1016/0005-7967(89)90087-9. [DOI] [PubMed] [Google Scholar]
- 11.Crisp A H, Norton K, Gowers S, Halek C, Bowyer C, Yeldham D, Levett G, Bhat A. Br J Psychiatry. 1991;159:325–333. doi: 10.1192/bjp.159.3.325. [DOI] [PubMed] [Google Scholar]
- 12.Dare C, Eisler I, Russell G, Treasure J, Dodge L. Br J Psychiatry. 2001;178:216–221. doi: 10.1192/bjp.178.3.216. [DOI] [PubMed] [Google Scholar]
- 13.Agras W S, Walsh T, Fairburn C G, Wilson G T, Kraemer H C. Arch Gen Psychiatry. 2000;57:459–466. doi: 10.1001/archpsyc.57.5.459. [DOI] [PubMed] [Google Scholar]
- 14.Fairburn C G, Jones R, Peveler R C, Hope R A, O'Connor M. Arch Gen Psychiatry. 1993;50:419–428. doi: 10.1001/archpsyc.1993.01820180009001. [DOI] [PubMed] [Google Scholar]
- 15.Attia E, Haiman C, Walsh B T, Flater S R. Am J Psychiatry. 1998;155:548–551. doi: 10.1176/ajp.155.4.548. [DOI] [PubMed] [Google Scholar]
- 16.Faris P L, Kim S W, Meller W H, Goodale R L, Oakman S A, Hofbauer R D, Marshall A M, Daughters R S, Banerjee-Stevens D, Eckert E D, Hartman B K. Lancet. 2000;355:792–797. doi: 10.1016/S0140-6736(99)09062-5. [DOI] [PubMed] [Google Scholar]
- 17.Walsh B T, Wilson G T, Loeb K L, Devlin M J, Pike K M, Roose S P, Fleiss J, Waternaux C. Am J Psychiatry. 1997;154:523–531. doi: 10.1176/ajp.154.4.523. [DOI] [PubMed] [Google Scholar]
- 18.Stice E. In: Eating Disorders. Striegel-Moore R H, Smolak L, editors. Washington, DC: Am. Psychol. Assoc.; 2001. pp. 51–73. [Google Scholar]
- 19.Bergh C, Södersten P. Nat Med. 1996;2:21–22. doi: 10.1038/nm0196-21. [DOI] [PubMed] [Google Scholar]
- 20.Matsunaga H, Kaye W H, McConaha C, Plotnicov K, Pollice C, Rao R. Int J Eat Disord. 2000;27:353–357. doi: 10.1002/(sici)1098-108x(200004)27:3<353::aid-eat14>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 21.Wakeling A, Russell G F. Psychol Med. 1970;1:30–39. doi: 10.1017/s0033291700039994. [DOI] [PubMed] [Google Scholar]
- 22.Kaye W H, Gwirtsman H E, Abarzanek E, George D T. Am J Clin Nutr. 1998;47:989–994. doi: 10.1093/ajcn/47.6.989. [DOI] [PubMed] [Google Scholar]
- 23.Palla B, Litt I F. Pediatrics. 1988;81:613–623. [PubMed] [Google Scholar]
- 24.Davis C, Katzman D K, Kaptein S, Kirsh C, Brewer H, Kalmbach K, Olmsted M P, Woodside D B, Kaplan A S. Comp Psychiatry. 1997;38:321–326. doi: 10.1016/s0010-440x(97)90927-5. [DOI] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Ed. Washington, DC: Am. Psychiatric Assoc.; 1995. [Google Scholar]
- 26.Brewerton T D, Dansky B S, Kilpatrick D G, O′Neil P M. Int J Eat Disord. 2000;28:259–264. doi: 10.1002/1098-108x(200011)28:3<259::aid-eat2>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 27.Bergh C, Eklund S, Eriksson M, Lindberg G, Södersten P. Lancet. 1996;348:611–612. doi: 10.1016/S0140-6736(05)64824-6. [DOI] [PubMed] [Google Scholar]
- 28.Fairburn C G, Norman P A, Welch S L, O'Connor M E, Doll H A, Peveler R C. Arch Gen Psychiatry. 1995;52:304–312. doi: 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- 29.Svanborg P, Åsberg M. Acta Psychiatr Scand. 1994;89:21–28. doi: 10.1111/j.1600-0447.1994.tb01480.x. [DOI] [PubMed] [Google Scholar]
- 30.Garner D M. Eating Disorder Inventory-2. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 31.Skinner B F. The Behavior of Organisms. Acton, MA: Copley; 1991. [Google Scholar]
- 32.Borg G. Borg′s Perceived Exertion and Pain Scales. Champagne, IL: Human Kinetics; 1998. [Google Scholar]
- 33.Pocock S J. Clinical Trials. New York: Wiley; 1998. [Google Scholar]
- 34.Fichter M M, Quadling N. Int J Eat Disord. 1999;26:359–385. doi: 10.1002/(sici)1098-108x(199912)26:4<359::aid-eat2>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 35.Strober M, Freeman R, Morrell W. Int J Eat Disord. 1997;22:339–360. doi: 10.1002/(sici)1098-108x(199712)22:4<339::aid-eat1>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 36.Eisler I, Dare C, Russell G F, Szmukler G, le Grange D, Dodge E. Arch Gen Psychiatry. 1997;54:1025–1030. doi: 10.1001/archpsyc.1997.01830230063008. [DOI] [PubMed] [Google Scholar]
- 37.Hay P J, Bacaltchuk J. The Cochrane Library. Oxford, U.K.: Update Software; 2000. [Google Scholar]
- 38.Bergh C, Södersten P. Lancet. 1998;351:1427–1429. doi: 10.1016/S0140-6736(97)12033-5. [DOI] [PubMed] [Google Scholar]