Abstract
Purpose of Review
Joint hypermobility can increase complications in surgical management of musculoskeletal conditions. The purpose of this review is to 1) summarize clinical outcomes in patients undergoing various Orthopedic sports medicine surgical procedures by joint, and 2) compare outcomes in patients with and without hypermobility.
Recent Findings
A total of 38 studies consisting of 144,609 patients and 144,860 joints were included (140,625 shoulders, 2,043 hips, 1,499 knees, 689 ankles, and four elbows). Notable heterogeneity exists within the literature regarding outcomes in hypermobile patients undergoing Orthopedic sports medicine procedures. In general, outcomes for hypermobile patients undergoing procedures of the shoulder, elbow, hip, and knee demonstrated similar or slightly worse outcomes across various patient reported outcomes measures (PROMs) and in terms of recurrent instability or dislocation. There were consistently worse outcomes (e.g. higher rates of post-operative recurrent instability, PROMs) in studies evaluating hypermobile patients undergoing surgery for chronic lateral ankle instability (CLAI) compared to non-hypermobile controls.
Summary
Patients with joint hypermobility tend to have similar or worse outcomes following Orthopedic sports medicine procedures related to the shoulder, knee, hip, and elbow, and consistently worse outcomes for the ankle. Future studies are encouraged to focus on the effect of hypermobility on elbow and wrist sports pathologies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12178-025-09979-2.
Keywords: Ehlers Danlos Syndrome (EDS), Generalized ligamentous laxity, Joint hypermobility, Surgical outcomes, Sports procedures
Introduction
Ehlers-Danlos Syndrome (EDS) and joint hypermobility conditions represent a spectrum of inherited connective tissue disorders characterized by excessive joint mobility and tissue fragility [1, 2]. These conditions affect approximately one in 5000 individuals globally according to some estimates, though these vary significantly due to diagnostic challenges and phenotypic heterogeneity [3]. While these conditions affect multiple organ systems, joint manifestations often present the most significant burden on patient function and quality of life, with many patients reporting chronic musculoskeletal pain and instability [4, 5].
Large joints, including shoulders, elbows, wrists, hips, knees, and ankles, are particularly susceptible to recurrent subluxations, instability, and early-onset osteoarthritis [6, 7]. Studies have reported that dislocations and subluxations most frequently affect the shoulder and knee joints in these patients [6]. Management of large joint manifestations in EDS and hypermobility conditions presents unique challenges to clinicians. The inherent tissue fragility, delayed healing responses, and heightened risk of wound complications can complicate both conservative and surgical interventions [8, 9].
Despite significant impact on patient function, there remains considerable uncertainty regarding optimal treatment strategies. Current evidence suggests variable success rates between conservative and surgical approaches, with increased postoperative complication rates noted in the hypermobile cohort [10, 11]. While various therapeutic approaches have been described, ranging from physical therapy to complex surgical reconstructions, literature lacks comprehensive synthesis of treatment outcomes across different joint involvement patterns.
This systematic review aimed to evaluate outcomes among various surgical treatment modalities for symptomatic instability within the major joints (hip, knee, ankle, shoulder, elbow, wrist) in adolescent (> 12 years) and adult patients with EDS, joint hypermobility syndrome, and related conditions characterized by generalized ligamentous laxity. By analyzing treatment approaches across multiple large joint types, this review sought to provide an evidence-based framework for therapeutic decision-making in this challenging patient population.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A protocol was developed prior to initiating the review process.
Search Strategy
A comprehensive literature search was completed using two electronic databases (MEDLINE, EMBASE) for articles published on or before November 15 2024. The search strategy was developed to identify studies focusing on EDS, joint hypermobility conditions, and both operative and non-operative management. The following search terms were used: ("Ehlers-Danlos syndrome"OR"joint hypermobility."OR"generalized ligamentous laxity"OR"Beighton score") AND ("surgery” OR “treatment”) (Supplementary Table 1).
Studies were included if they met the following criteria: (1) mention of EDS, joint hypermobility syndrome, generalized ligamentous laxity, elevated Beighton score (≥ 4), or other descriptions of joint hypermobility/laxity; (2) inclusion of individuals over 12 years of age; (3) surgical treatment for sports medicine procedures in patients with joint hypermobility or laxity; (4) focus on large joints (shoulders, elbows, wrists, hips, knees, ankles); and (5) any level of evidence.
Studies were excluded if they: (1) focused exclusively on children under 12 years of age (to avoid comparing heterogenous populations); (2) primarily addressed genetic analysis, phenotyping, spine involvement, neurosurgical procedures, or pelvic procedures; (3) were non-human studies or published in languages other than English; 4) studies that did not specifically report on outcomes corresponding to a hypermobile cohort or an elevated Beighton score via numerical values or p-values.
Study Screening
Two authors independently completed title and abstract screening. If a conflict arose that could not be resolved through discussion, a third author made the final decision. Full-text screening and conflict-resolution followed the same protocol. Articles that passed the initial title and abstract screening underwent full-text review to confirm eligibility based on the inclusion and exclusion criteria.
Assessment of Agreement
The kappa (κ) statistic was calculated to assess inter-reviewer agreement during the screening process. Agreement levels were categorized a priori into six levels: almost perfect (κ = 0.91–0.99), considerable (κ = 0.71–0.90), high (κ = 0.61–0.70), moderate (κ = 0.41–0.60), fair (κ = 0.21–0.40), and no agreement (κ ≤ 0.20) [12].
Quality Assessment
Methodological quality was assessed using the MINORS criteria, a validated tool for non-randomized studies [13]. Quality thresholds were established prior to assessment following previously published guidelines (13). For non-comparative studies (maximum score 16), quality was categorized as: very low (0–4), low (5–7), fair (8–12), or high (≥ 13) (14). Comparative studies were evaluated on an expanded 24-point scale, with quality designated as: very low (0–6), low (7–10), fair (11–15), good (16–20), or high (≥ 20) (14).
Data Abstraction
Three reviewers independently extracted and summarised data from included articles using Google Sheets (Google LLC, Mountain View, CA, USA). The extraction form was organized into several major domains: study characteristics, patient demographics, clinical features, interventions, and outcomes. Study characteristics included study design, randomization methods, blinding status, and statistical approaches. Demographic data encompassed sample size, follow-up rates, age distributions, gender ratios, and activity levels.
Clinical information was collected regarding primary diagnoses, Beighton scores or definition of hypermobility, symptom duration, and previous treatments. Intervention details included specific surgical techniques, post-operative protocols, and rehabilitation parameters (duration, frequency, and compliance rates).
Outcome measures were systematically recorded, including primary and secondary endpoints, standardized outcome tools, baseline and follow-up scores with standard deviations, statistical analyses (confidence intervals, p-values, effect sizes), pain scores, functional outcomes, and patient satisfaction metrics. Complications were documented, including adverse events, failure rates, revision surgeries, and joint-specific complications. For joint-specific data, we extracted information about pathology patterns, instability direction, associated injuries, and previous surgical interventions.
Statistical Analysis
A narrative synthesis approach was adopted to analyze and present the findings due to the heterogeneous nature of the included studies. Descriptive statistics were calculated using Google Sheets (Google LLC, Mountain View, CA, USA), including means, ranges, standard deviations, 95% confidence intervals, and proportions where appropriate. P-values less than 0.05 were considered to be statistically significant.
Results
Study Characteristics
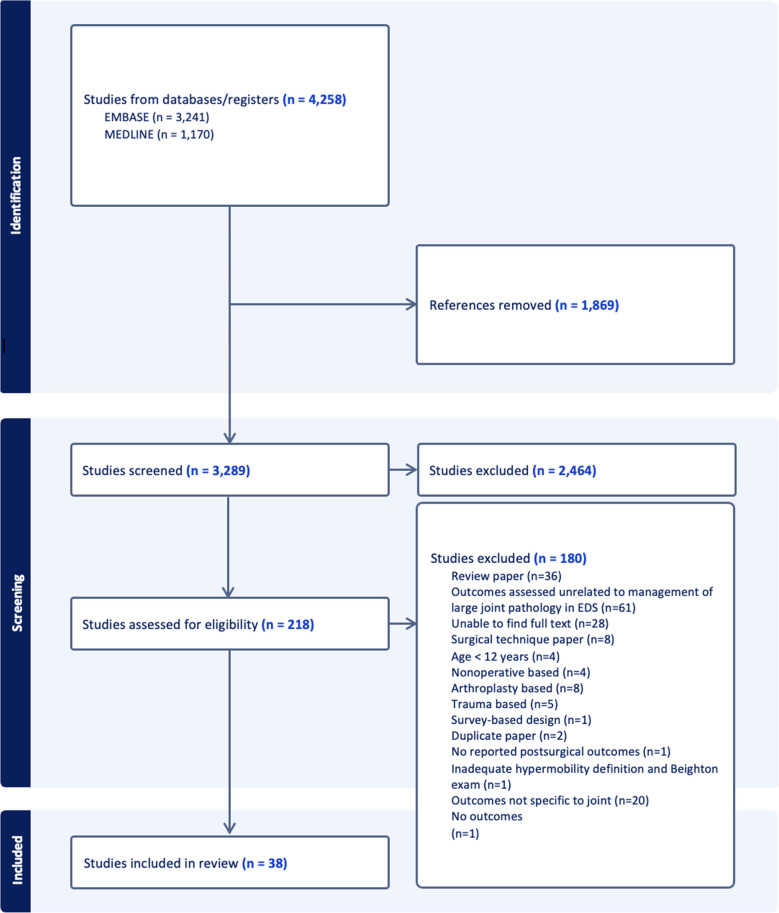
The initial search produced 4,258 articles, with 1,869 articles removed as duplicates. A total of 3289 titles and abstracts were screened, with 3071 identified as irrelevant. 218 full-texts were assessed for eligibility, and overall, 38 satisfied the eligibility criteria (Fig. 1). The agreement between reviewers was considerable during the title and abstract screening and full-text screening stages, with kappa values of 0.898 (95%CI 0.866–0.930) and 0.951 (95%CI 0.903–0.999), respectively. The 38 articles in this review included two prospective cohort studies (level II evidence), 18 retrospective cohort studies (level III evidence), 13 case series (level IV evidence), and five case studies (level V evidence). The mean MINORS score amongst comparative and non-comparative studies were 19.25 and 10.85, or of good and fair quality, respectively (Tables 1, 2, 3, 4 and 5). Among the studies that reported on specific study characteristics, mean age of patients among all studies was 26.7 years (range 14–43), mean post-operative follow-up was 35.9 months (range 12–96), and average percentage of hypermobile females was 63.1%.
Fig. 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram representing a scoping review on operative and nonoperative management of large joint pathologies in EDS and hypermobility conditions
Table 1.
Characteristics and results of hip studies evaluating patients with joint hypermobility
| Femoroacetabular Instability | ||||||||||||||
| Study | Patients,n (Hips) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Hips, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) |
Hypermobile Female (n) |
Beighton Score, (mean) | Treatment |
Recurrent Instability or Tear (n, (%)) |
PROMs | MINORS |
| Stone et al. (2019) |
25 (25) (hypermobile) 100 (100) (matched controls) |
Prospective Cohort (II) | No significant differences in post-operative outcomes between patients with and without GJL in patients undergoing hip arthroscopy for FAI Syndrome at 2-year follow-up |
GJL: 23 EDS: 2 |
GJL: Beighton score ≥ 4 9-point Beighton test EDS: NR |
NR | 29.3 | 21.7 (hypermobile) | 25 | 6.04 (hypermobile) |
Standard hip arthroscopy with interportal capsulotomy, acetabular rim trim if indicated, labral repair if indicated, T-capsulotomy & femoral osteoplasty if indicated All capsulotomies closed with capsular plication |
0 (0) |
Hypermobile Group ᇫHOS-ADL 31.3 ± 23.9 ᇫHOS-SS 35.1 ± 27.3 ᇫmHHS 23.7 ± 18.5 ᇫVAS-pain −59.5 ± 29.28 ᇫVAS-satisfaction 92.9 ± 17.9 |
21/24 |
|
Soriano et al (2023) |
37 (40) (hypermobile) 37 (40) (matched cohort) |
Retrospective Cohort (III) | Patients with GLL in setting of FAI can be effectively treated with arthroscopy via periportal capsulotomy and capsular closure | GLL: 40 |
Beighton score > 4 5-point Beighton test |
6 (13) | Minimum 2 years | 29.7 (hypermobile) | 35 | 5 (hypermobile) |
Standard hip arthroscopy with periportal capsulotomy, labral repair, femoroplasty, acetabuloplasty as indicated All GLL had capsular plication of MAP, ALP not closed. Matched cohort capsule not closed |
0 (0) |
Hypermobile Group SF-12 PCS: Pre: 30.7 Post: 48.4 (p < 0.001) SF-12 MCS: Pre: 48.4 Post: 47.8 (p = 0.798) VAS pain: Pre: 4.0 Post: 1.5 (p = < 0.001) HOOS-Symptoms: Pre: 51.6 Post: 77.9 (p < 0.001) HOOS-Pain Pre: 57.9 Post: 84.7 (p < 0.001) HOOS-ADL Pre: 66.7 Post: 91.7 (p < 0.001) HOOS-Sports Pre:38.0 Post: 81.6 (p < 0.001) HOOS-QOL Pre: 26.7 Post: 70.9 (p < 0.001 ) |
19/24 |
| Mojica et al. (2022) |
40 (IPT group) 40 (control group) |
Retrospective Cohort (III) | For each one-point increase in the Beighton score, there was a 1.69 (95% confidence interval, 1.25–2.29; P <.001) increased odds of IPT development post-operatively. A high (4) versus low (< 4) Beighton score was associated with an increased likelihood of tendinitis (odds ratio, 9.82; 95% confidence interval, 2.79–34.58; P <.001) |
3 “connective tissue” disease (IPT group) 4 “connective tissue” disease (control group) |
Beighton > 4 9-point Beighton test |
NR | 27.6 |
34.8 (IPT group) 34.4 (control group) |
Total Study 36 (IPT group) 29 (control group) |
4 (3.8) (IPT group) 2 (1.9) (control group) p < 0.001 |
Standard hip arthroscopy with interportal capsulotomy, labral repair when indicated, femoral and acetabular osteoplasties as indicated All patients underwent standard capsular repair and portal closure |
N/A | NR | 20/24 |
| Maldono et al. (2020) |
57 (57) (hypermobile) 88 (88) (matched control) |
Retrospective Cohort (III) | Satisfactory outcomes in patients with GLL after hip arthroscopy for symptomatic FAI with appropriate labral and capsular management with similar post-operative PROM scores and complications despite significantly higher patient satisfaction reported in control group at 2y follow up (8.43(2.41) vs. 7.71(2.38); p = 0.012) | GLL: 57 |
Beighton ≥ 4 Patient self-reported questionnaire |
42 (14.9) | 33.6 (hypermobile) | 32.9 (hypermobile) | 50 | 5.68 (hypermobile) |
Standard hip arthroscopy with interportal capsulotomy, labrum debrided, repaired, or reconstructed when indicated, acetabuloplasty when indicated, femoral osteoplasty when indicated All patients received capsular plication unless excessive stiffness,adhesive capsulitis, insufficient capsular tissue |
6 (10.5%) (hypermobile (n = 6 retorn labrum, n = 1 stiffness, n = 1 recalcitrant GT bursitis, n = 1 hip flexor tedinitis) |
mHHS: Pre: 61.0 (14.9) Post: 83.9 (17.9) (p < 0.001) NAHS: Pre: 62.2 (18.1) Post: 84.2 (17.0) (p < 0.001) VAS: Pre: 5.28 (1.95) Post: 2.46 (2.64) (p < 0.001) HOS-SSS: Pre: 41.2 (24.1) Post: 75.5 (28.3) (p < 0.001) |
11/16 |
|
Naal et al (2017) |
232 (244) | Retrospective Cohort (III) | No significant associations between Beighton scores and post-operative PROM values or subjective failure rates. Patients who objectively failed had lower Beighton score than non-failures (1.6 vs 2.6; p = 0.049) | GJL: 84 |
Beighton ≥ 4 Patient self-reported questionnaire |
NR | 44.4 | 35.8 |
118 (total study) |
2.5 ± 2.7 34.3% patients ≥ 4 18.0% patients ≥ 6 |
Surgical hip dislocation (n = 130) Mini-open surgery (n = 67) Hip arthroscopy (n = 130) |
11 objective failures—significantly lower Beighton scores than did the nonfailures (1.6 vs 2.6; P =.049) 9 objective failures no significant associations between Beighton scores and post-operative subjective failure rate |
Weak inverse association (P <.05) between Beighton scores and pre-operative PROM values (r = 20.16 to 20.30) No significant associations between Beighton scores and post-operative PROM values |
11/16 |
| Saadat et al. (2019) |
Beighton Score 0—882 (882) (non hypermobile) 0–3—1120 (1120) (non-hypermobile) > 1—499 (499) (non-hypermobile) > 4—261 (261) (hypermobile) |
Retrospective Cohort (III) | Patients with higher pre-operative Beighton scores has increased hip ROM and smaller intra-operative labral size and tear dimensions. They were more likely to undergo labral repair, capsular plication, and iliopsoas fractional lengthening | GLL: 261 |
Beighton ≥ 4 9-point Beighton test |
NR | NR |
Beighton Score 0—40 (15.4) 0–3—38.9 (15.2) > 1—32.8 (13.7) > 4—31.0 (13.3) |
Beighton Score 0—477 0–3—655 > 1—420 > 4—242 |
NR (Mean Beighton) |
Standard hip arthroscopy with interportal capsulotomy, labral debridement, repair, or reconstruction when indicated, acetabuloplasty and/or femoroplasty when indicated, iliopsoas fractional lengthening when indicated, capsular release vs. repair/plication when indicated | NR | NR | 14/16 |
|
Larson et al (2015) |
12 (16) | Case Series (IV) | Meticulous capsular plication, labral preservation, and correct of FAI when present led to successful outcomes and subjective stability without any iatrogenic dislocations in this patient population | EDS: 16 | EDS-hypermobile type diagnosed via geneticist for all patients | 0 (0) | 44.6 | 26.0 | 11 | NR |
Standard hip arthroscopy with interportal capsulotomy, cetabular rim trim if indicated, labral repair if indicated, all inside femoral osteoplasty if indicated All capsulotomies closed with capsular plication |
One patient underwent revision arthroscopy and capsular plication for recurrent pain, and subjective giving-way episodes |
mHHS: Pre: 45.6 Post: 88.5 (p = 0.002) SF-12: Pre: 62.4 Post: 79.3 (p = 0.027) VAS-pain: Pre: 6.5 Post: 1.6 (p = 0.0004) |
11/16 |
| Ligamentum Teres Reconstruction | ||||||||||||||
| Study | Patients (Hips) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Hips, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) |
Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, (%)) | PROMs | MINORS |
| Rosinsky et al. (2020) | 9 (10) | Case Series (IV) | Three of the seven hips (42.9%) in patients with EDS reported unfavorable outcomes, with two undergoing revision procedure | EDS: 7 |
Beighton ≥ 4 9-point Beighton test |
NR | 44.3 | 30.3 | 7 | > 4 all patients | Standard hip arthroscopy, labral debridement repair or reconstruction when indicated, acetabuloplasty and/or femoroplasty when indicated, reconstruction with either semtendinosus autograft or tibialis anterior allograft | 2(22.2) underwent THA |
mHHS: Pre: 44.1 (17.7) Post: 71.8 (22.7) (p < 0.05) NAHS: Pre: 47.5 (20.6) Post: 78.6 (14.6) (p < 0.05) iHOT-12 Pre: N/A Post: 61.0 (37.2) (p < 0.05) VAS: Pre: 7.8(1.2) Post:3.6(3.6) (p < 0.05) |
10/16 |
| Hammarstedt et al. (2015) | 1 (1) | Case Study (V) | Satisfactory results one year from surgery | EDS: 1 | EDS “type 2 and 3” diagnosed via collagen typing from skin sample | 0 (0) | 24 | 43 | 1 | NR | Standard hip arthroscopy with capsulotomy, labral repair, LT reconstruction with tibialis anterior allograft, capsular plication | 0 (0) |
mHHS: Pre: 36.3 Post:90.1 (p: NR) NAHS Pre: 27.5 Post: 50.0 (p: NR) HOS-ADL Pre: 30.9 Post: 48.5 (p: NR) HOS-SSS: Pre: 3.1 Post: 34.4 (p: NR) VAS: Pre: 8 Post: 0 (p: NR) |
11/16 |
PROM; patient reported outcome measure, MINORS; methodological index for non-randomized studies, NR; not reported, N/A; not applicable, GJL; generalized joint laxity, GLL; generalized ligamentous laxity, EDS; ehlers danlos syndrome, FAI; femoroacetabular impingement, ADL; activities of daily living, QOL; quality of life, HOOS; hip disability and osteoarthritis outcome score, HOS; hip outcome score, SSS; sport specific scale, mHHS; modified harris hip score, NAHS; non-arthritic hip score, VAS; visual analog scale, FAI; femoroacetabular impingement, SF-12; 12-Item short form health survey, MCS; mental component summary, PCS; physical component summary, MAP; mid-anterior portal; ALP; anterolateral portal, IPT; iliopsoas tendonitis, ROM; range of motion, iHOT-12; international hip outcome tool–12, “ ± ”; plus or minus, ≥; greater than or equal to, “ᇫ”; delta, “change in”
Table 2.
Characteristics and results of knee studies evaluating patients with joint hypermobility
| Study | Patients (Knees) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Knees, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) | Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, (%)) | PROMs | MINORS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patellar Instability | ||||||||||||||
| Kutschke et al. (2024) |
208 (208) total hypermobile patients < 11 controls Analysis of a population of EDS/MFS patients with the above undergoing surgical management for patellar instability |
Retrospective Cohort (III) | Rates of recurrent patellar instability after MPFL-R in patients with joint hypermobility were not different to matched controls (p = n.s) |
EDS: 185 MFS: 30 Total: 208—unspecified about 3 patients |
Specifics not reported—stated 9-point Beighton test most common. 7 different clinical scales to define GJH in total | NR | Minimum 24 (all) | NR | NR | NR | Unspecified patellar stabilization surgery(n = 208) | < 11 dislocations in hypermobile group relative to non-hypermobile group | NR | 15/24 |
| Howell al. (2012) |
25 (25) (hypermobile) 50 (50) (not hypermobile) |
Case control (III) | Patients without joint hypermobility had superior patient reported outcome measures (p < 0.001) than those with hypermobility | GJH: 25 |
Beighton ≥ 4 9-point Beighton test |
0 (0) | 15.0 (hypermobile) | 25.4 (hypermobile) | 23 | > 6 | Isolated MPFL-R | 0 (0%) |
IKDC Hypermobile Post: 55.0 Kujala Hypermobile Post: 64.3 |
10/16 |
| Parikh et al. (2024) | 31 (47) (hypermobile) | Case Series (IV) | High rate of revision patellar stabilization surgery in patients undergoing MPFL-R who have EDS | EDS: 47 | NR | 0 (0) | 86.4 | 14.9 | 27 | 6.8 | Isolated MPFL-R | 9/47 (19.1) |
KOOS: Post: Pain: 76.1 ADL: 82.3 S/R: 64.7 |
11/16 |
| Imerci et al. (2022) | 11 (17) (hypermobile) | Case Series (IV) | “Successful” outcomes in syndromic patients undergoing MPFL-R with TTO |
EDS: 6 Trichorhinophalangeal: 2 McCune-Albright: 1 Klippel Feil: 1 GJH: 4 Down Syndrome: 3 |
NR | 0 (0) | 26.4 | 14.8 | 7 | NR | MPFL-R + TTO | 2/17 (11.8) |
Kujala: Pre: 56 (10) Post: 86 (6) Lysholm: Pre: 53 (10) Post 85 (7) |
10/16 |
| Hiemstra et al. (2019) |
144/167 total 92 (hypermobile) |
Case Series (IV) | GJH did not influence outcomes following MPFL-R (did not investigate for dislocation) | GJH: 92 |
Beighton ≥ 4 9-point Beighton test |
8 (total) | 24.5 (hypermobile) | 22.9 (hypermobile) | 72 | > 4 for hypermobile patients | Isolated MPFL-R |
> 4 Beighton: 3/92 (3.3) 1 |
NR | 13/16 |
| Shubert et al. (2019) | 1 (2) (hypermobile) | Case study (V) | Satisfactory outcomes in one patient with EDS undergoing MPFL-R | EDS: 2 | EDS-hypermoible type diagnosed by “meeting all criteria for disease including Beighton score” | 0 (0) | 24 | 35 | 1 | NR | Isolated MPFL-R with lateral patellofemoral ligament reconstruction for iatrogenic injury | 0 (0) | NR | 10/16 |
| Anterior Cruciate Ligament Reconstruction | ||||||||||||||
|
Zsidai et al (2023) |
61 (61) (hypermobile) 164 (164) (non-hypermobile) |
Retrospective cohort (III) | GJH leads to higher rates of instability after ACLR relative to patients without GJH (p = 0.012) but did not result in significant difference in PROMs | GJH: 61 |
Beighton ≥ 5 9-point Beighton test |
0 | 12 | 22.3 (hypermobile) | 19 (hypermobile) | > 5 | ACLR | 7 (11.4) |
KOOS: Symptoms: 77.5 (range: 75.2–79.7) Pain: 87.2 (range: 85.5–88.9) ADL: 95.8 (range: 93.9–97.7) S/R: 69.9 (range: 66.6–73) QOL: 61.1 (range: 58.4–63.8 |
9/16 |
| Toker et al. (2022) | 68 (68) (hypermobile) | Retrospective cohort (III) | No difference in re-tears in patients between groups, but greater anterior and rotational laxity in patients with isolated ACLR as opposed to ACLR + ALL IB | GJH: 68 |
Beighton ≥ 5 9-point Beighton test |
0 |
ACLR group: 30.1 (n = 37) ACLR + ALL IB group: 28.1 (n = 31) |
ACLR group: 26.7 (n = 37) ACLR + ALL IB group: 33.2 (n = 31) |
ACLR group: 11 ACLR + ALL IB group: 16 |
NR | ACLR ± ALL IB |
ACLR group: 4(10.8) ACLR + ALL IB: 1(3.2) N.s KT-1000: Lower ATT in ACLR + ALL IB group (p < 0.01), better rotational stability with pivot-shift (p = 0.008) |
Lysholm: ACLR group: 86.3 (4.7) ACLR + ALL IB: 89.3 (5.2) n.s |
11/16: |
| Sundemo et al. (2021) |
76 (76) (hypermobile) 280 (280) (non-hypermobile) |
Retrospective cohort (III) | No significant difference in retears or KOOS subscale scores in patients with or without hypermobility | GJH: 76 |
Beighton ≥ 5 9-point Beighton test |
0 (0) | 12 (hypermobile | 26.3 (hypermobile) | 58 (hypermobile) | > 5 | ACLR | 9 (11.8) (hypermobile) |
KOOS Beighton (5–9) S/R: 65.8 (22.6) Pain: 85.4 (12.9) Symptoms: 76.7 (13.5) ADL: 94.4 (7.5) QOL: 57.6 (18.3) |
13/16 |
| Kim et al. (2009) |
Beighton/Horan Scale Score 0—75 (75) (non hypermobile) 1—29 (29) (non-hypermobile) 2—43 (43) (non-hypermobile) 3—64 (64) (non-hypermobile) 4—29 (29) (hypermobile) 5—32 (32) (hypermobile) |
Retrospective Cohort (III) |
Knee extension predicts post-operative stability and function regardless of generalized joint hypermobility In patients with knee hyperextension, bone-patellar tendon-bone autografts provided greater stability and function |
Joint laxity as per Beighton/Horan Scale: 4/5+ positive findings −61 | NR | Minimum 24 |
Beighton/Horan Scale Score 4 −29.1 (hypermobile) 5—28.4 (hypermobile) |
Beighton/Horan Scale Score 4 −11 (hypermobile) 5—15 (hypermobile) |
Beighton and Horan scale: 4/5 + positive findings | ACLR |
KT-1000 arthrometer (mm)—anterior tibial translation Beighton/Horan Scale Score 4 −3.6 (1.2) (hypermobile) 5—4.1 (1.4) (hypermobile) Thumb opposition (ρ = 0.305, p = 0.001) Little finger dorsiflexion (ρ = 0.271, p = 0.005) Knee hyperextension (ρ = 0.461, p = 0.000) |
Lysholm: Beighton/Horan Scale Score 4 −88 (10.2) (hypermobile) 5—81.1 (7.7) (hypermobile) Knee hyperextension (ρ = −0.285, p = 0.000) |
8/16 | |
| Kim et al. (2010) | 61 (61) (hypermobile) | Case series (IV) | SB ACLR results in significantly higher ATT and lower PROMs than DB ACLR in patients with GJH | GJH: 61 |
Beighton ≥ 4 5-point Beighton test |
0 | 24 |
SB: 28.9 (n = 32) DB: 25.3 (n = 29) |
SB: 18 DB: 18 |
> 4 | ACLR |
KT-2000: SB: 3.4 (1.8) DB: 2.0 (1.1) p = 0.02 |
Lysholm: SB: 89.4 DB: 91.1 p = 0.02 |
9/16 |
| Hishimura et al. (2022) | 1 (1) | Case study (V) | Satisfactory outcomes in a patient undergoing ACLR with EDS | EDS: 1 | EDS-hypermobile type diagnosed by pediatric physician at 2y old based on history | 0 (0) | 36 | 18 | 0 | 6 | ACLR | 0 (0) |
KOOS: ADL: 98 Sport: 85 Pain: 94.4 QOL: 87.5 |
10/16 |
PROM; patient reported outcome measure, MINORS; methodological index for non-randomized studies, NR; not reported, N/A; not applicable, N.S.; not significant, GJL; generalized joint laxity, GLL; generalized ligamentous laxity, GJH; generalized joint hypermobility, EDS; ehlers danlos syndrome, MFS; Marfam’s syndrome, MPFL-R; Medial patellofemoral ligament reconstruction, ACLR; anterior cruciate ligament reconstruction, KOOS; knee osteoarthritis and outcome score, SB; single bundle, DB; double bundle, ATT; anterior tibial translation, ALL IB; anterolateral ligament internal bracing, IKDC; international knee documentation committee, TTO; tibial tubercle osteotomy, ADL; activities of daily living, QOL; quality of life, S/R; sports and recreation, “ ± ”; plus or minus, ≥; greater than or equal to, “ᇫ”; delta, “change in”
Table 3.
Characteristics and results of ankle studies evaluating patients with joint hypermobility
| Study | Patients (Ankles) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Ankles, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) | Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, (%)) | PROMs | MINORS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronic Lateral Ankle Instability (CLAI) | ||||||||||||||
| Porter et al. (2022) |
21 (21) (hypermobile) 21 (21) (control) 21 (21) (> 90 kg) |
Prospective Cohort (II) |
Similar FAOOs and TAS scored in GLL patients post-operatively compared to controls. No recurrent instability, surgeries, major complications | GLL: 21 |
Beighton ≥ 5 NR |
3 (4.8) | 2 and 5 years time points | GLL: 25.1 | 13 | All ≥ 5 in GLL group | Open MBO + LARS augmentation | 0 (0) |
FAOOS: Pain: Pre: 75.8(5.37) Post: 89.1(4.62) Symptoms: Pre: 72.1(6.10) Post:92.3(3.76) ADL: Pre:71.0 (10.4) Post: 96.3(2.65) Sports: Pre: 63.2 (5.59) Post: 94.8 (3.77) QOL: Pre: 64.1(9.56) Post: 93.5(3.20) TAS: Pre: 8.19 (1.08) Post: 8.71 (0.71) |
20/24 |
| Wang et al. (2024) |
19 (19) AR 49 (49) MBO |
Retrospective Cohort (III) | Better clinical outcomes, fewer instability recurrences and higher rate to pre-injury high demand sport after AR compared with open MBO in patient with GJL | GJL: 68 |
Beighton ≥ 4 9-point Beighton test |
NR (11) |
AR: 38.3 MBO: 43.7 |
AR: 30.3 MBO: 29 |
AR: 10 MBO: 32 |
AR: 6.8 MBO: 6.2 |
Open MBO vs. Open anatomic with gracilis tendon autograft of ipsilateral knee |
AR: 0 (0) MBO: 11 (22.4) p = 0.027 |
AR FAOS: Pre: 62.8 (2.7) Post: 88.6 (7.4) Karlsson: Pre: 64.3 (4.5) Post: 86.9 (6.1) MBO FAOS Pre: 62.1 (5.8) Post: 88.2 (7.3) Karlsson Pre: 63.1 (4.2) Post: 82 (8.4) |
21/24 |
| Wang et al. (2023) | 61 (61) | Retrospective Cohort (III) | Arthroscopic MBO achieved similar short term outcomes to open MBO in patients with GJL | GJL: 61 |
Beighton ≥ 4 9-point Beighton test |
3 (4.7) | 24 |
Open: 28.6 Arthroscopic: 27.2 n.s |
39 |
Open: 6.2 Arthroscopic 5.5 n.s |
Open or arthroscopic MBO |
Open: 4 (12.9) Arthroscopic: 5 (16.7) n.s |
Open AOFAOS: Pre: 70.5(4.8) Post: 91.6 (7.1) Karlsson Pre: 60.7 (4.0) Post: 90.6 (6.3) VAS Pre: 4.8 (0.8) Post: 1.1 (1.2.) Arthroscopic AOFAOS: Pre: 69.1 (5.7) Post:91.9 (5.1) Karlsson Pre: 60.3 (5.8) Post: 90.3 (7.0) VAS Pre: 5.1 (1.2) Post: 1.2 (1.2) |
21/24 |
| Yeo et al. (2017) |
24 (24) (hypermobile) 75 (75) (non hypermobile) |
Retrospective Cohort (III) | No difference in clinical outcomes between laxity and no-laxity groups | GLL: 24 |
Beighton ≥ 4 9-point Beighton test |
2 (8.3) | 12 | 37.8 (hypermobile) | 19 | Beighton ≥ 4 in GLL group | Open MBO | 0 (0) |
AOFAS Pre: 58.5 (18.3) Post: 84.8 (12.9) p < 0.05 VAS Pre: 5.8 (2.5) Post: 2.7 (1.7) (p < 0.05) |
19/24 |
| Park et al. (2016) |
34 (42) (hypermobile) 181 (181) (control) |
Retrospective Cohort (III) |
GLL significantly associated with poor clinical and radiological outcomes. Independent predictor of poor outcomes and a risk factor for recurrent instability after MBO for CLAI | GLL: 42 |
Beighton ≥ 5 9-point Beighton test |
35 (15.7) (hypermobile) |
62.3 (hypermobile) |
29.4 (hypermobile) |
13 | Beighton ≥ 4 in GLL group | Open MBO |
10 (23.8) (hypermobile) 6 (3.8) (control) p < 0.001 |
Karlsson: Pre:54.6(7.1) Post: 87.9(7.2) (p < 0.001) |
18/24 |
| Xu et al. (2016) |
44 (44) (hypermobility) 56 (56) (control) |
Retrospective Cohort (III) |
Inferior clinical outcomes and significantly higher fail rates following MBO in those with GLL | GLL: 44 |
Beighton ≥ 5 9-point Beighton test |
0 (0) |
43.3 (hypermobile) |
34.6 (hypermobile) |
23 | Beighton ≥ 5 for GLL group | Open MBO |
GLL: 5 (11.4) Control: 1 (1.8) p < 0.05 |
AOFAS Pre: 60.9 Post: 89.5 Karlsson Pre: 53.2 Post: 87.4 |
17/24 |
| Cheng et al. (2002) | 13 (15) | Case series (IV) | Chrisman-Snook procedure showed favorable outcomes (excellent outcome group, 80% patients Beighton score 5 +) in those with GLL in this patient population | GLL: NR (“majority” had GLL) |
Beighton ≥ 5 9-point Beighton test |
5 (33.3) | 35.3 | 22.1 | 0 | 4.6 | Chrisman-Snook reconstruction | 2 (13) significant inversion sprain one year postop | Kaikkonen score: 14 (93%) had excellent or good outcomes | 10/16 |
| Cho et al. (2016) | 28 (28) | Case Series (IV) | Patients had significantly improved postoperative FAAM and FAOS scores, and low rates of recurrent instability | GLL: 28 |
Beighton ≥ 4 9-point Beighton test |
2 (6.7) | 35.8 | 29.5 | 9 |
Beighton = 4: 9 Beighton = 5: 11 Beighton = 6: 5 Beighton = 7: 2 Beighton = 8: 1 |
Open MBO + suture-tape augmentation | 1 (3.6) |
FAOS total: Pre: 63.2 (12.5) Post: 90.6 (5.2) (p < 0.001) FAAM total: Pre: 54.3 (15.4) Post: 89.5 (6.7) (p < 0.001) |
12/16 |
| Huang et al. (2016) | 32 (32) | Case Series (IV) | No correlation between Beighton score and Karlsson-Peterson ankle score at last follow up | GJH: 32 |
Beighton ≥ 4 9-point Beighton test |
2 (6.3) | 27.4 | 21.7 | 3 |
Beighton = 4: 15 Beighton = 5: 6 Beighton = 6: 4 Beighton = 7: 5 Beighton = 9: 1 Beighton = 9: 1 |
Open MBO |
9 ankle sprains (%) 6 mild 3 mechanically unstable on stress XR, patients satisfied clinically No reoperations |
Karlsson: Pre: 63.6 (7.1) Post: 90.4 (6.7) (p < 0.001) |
10/16 |
PROM; patient reported outcome measure, MINORS; methodological index for non-randomized studies, NR; not reported, N/A; not applicable, N.S.; not significant, GJL; generalized joint laxity, GLL; generalized ligamentous laxity, GJH; generalized joint hypermobility, EDS; ehlers danlos syndrome, MBO; modified-brostrom operation, AOFAOS; american orthopaedic foot & ankle society outcome score, Karlsson; karlsson-peterson scoring system for ankle function, VAS; visual analog scale, FAOS/FAOOS; foot and ankle outcome score, TAS; tegner activity scale, ADL; activities of daily living, QOL; quality of life, FAAM; foot and ankle ability measure, CLAI; chronic lateral ankle instability, AR; ankle reconstructionm, LARS; ligament augmentation and reconstruction system, “ ± ”; plus or minus, ≥; greater than or equal to, “ᇫ”; delta, “change in”
Table 4.
Characteristics and results of shoulder studies evaluating patients with joint hypermobility
| Study | Patients (Shoulders) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Shoulders, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) | Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, (%)) | PROMs | MINORS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Winschel et al. (2024) |
EDS/GJH: 756 (756) Control: 139,764 (139,764) |
Retrospective Cohort (III) | EDS patients were more likely to undergo open surgical procedures (open posterior stabilization, capsulorrhaphy, Latarjet) as opposed to arthroscopic procedures. There were no differences in ipsilateral revision rates at 2 years postoperative | EDS/GJH: 756 | NR | NR | 24 | NR | NR | NR |
EDS/HSD Open procedures: 55 Arthroscopic stabilization: 616 Control: Open: 15,982 Arthroscopic: 125,994 EDS/HSD patients were more likely to undergo open posterior, open capsulorraphy, latarjet patients, and significantly less likely to undergo arthroscopic bankart repair |
24 months: EDS: 18/454 (4.0) Non-EDS: 1029/40536 (2.5) n.s when adjusted or not adjusted for confounding variables |
NR | 22/24 |
|
Yang et al (2016) |
52 (52) | Retrospective Cohort (III) | The multivariate analysis showed WOSI score can be predicted based on number of previous procedures and Beighton score alone. Beighton score was also correlated with higher WOSI scores. A patient undergoing a Latarjet procedure would have an increase of 700 in WOSI score if he or she had a Beighton score of ≥ 7 | NR |
Beighton 5–6 defined as increased mobility Beighton 7–9 defined as hypermobile 9-point Beighton test |
5 (9.6) | 42 | 23.2 | 11 | 4.08 | Modified Latarjet procedure | 8 (15.4) | No hypermobile cohort specific outcome data | 18/24 |
| Vavken et al. (2018) | 15 (18) | Case Series (IV) | High rates of failure in patients with EDS/GJH undergoing open inferior capsular shift for multidirectional instability |
EDS: 5 GLL: 13 |
Beighton ≥ 6 for GLL Genetic testing for EDS |
NR | 90 | 17 | 11 (total study) | > 6 | Open inferior capsular shift | 7 (47) |
Follow-up: ASES: 87.7 QuickDASH: 13.9 |
12/16 |
| Abdelhady et al. (2015) | 13 (14) | Case Series (IV) | Modified Latarjet provided satisfactory results in patients with GLL | GLL: 14 |
Beighton ≥ 4 5-point Beighton test |
NR | 33.6 | 24.4 | 4 | 6 | Modified Latarjet Procedure |
1 (7) - occurred following"violent act" |
Rowe score: Pre-op: 47.5 Post-op: 91.07 p < 0.001 |
14/16 |
| Dewing et al. (2011) | 15 (20) | Case Series (IV) | High rates of failure in patients with EDS/GJH (30%) after ACR, patients with type III EDS had worse functional scores than patient with GJH |
EDS: 9 JHS: 11 |
NR | NR | 45.6 | 23.1 | 17 (total study) | NR | Open anterior Capsulolabral Reconstruction | 6 (30) |
Baseline: ASES score 43 (range 27 to 67) Follow-up: ASES score 84 (range 58 to 97) Patients with type III EDS had significantly lower ASES scores—71 [range: 58–92] vs 92 [range: 78–97] in patients with GJH (p < 0.05) |
11/16 |
| Khawaja et al. (2024) | 1 (1) | Case Report (V) | Latissimus Dorsi transfer improved posterior shoulder instability in a patient with EDS | EDS: 1 | NR | 0 (0) | 35 | 14 | 1 | 9 |
Arthroscopic-assisted latissimus dorsi tendon transfer. Arthroscopic pectoralis minor release Physical therapy, corticosteroid injections, Botox injection |
0 (0) |
Baseline VAS: 8/10 SANE: 5% ASES: 10 6 weeks: VAS 3/10, SANE 50% 3 months: VAS 0/10, SANE 80% 7, 11, 24 months: VAS 0/10, SANE 90%, ASES 85 Pain: 8/10 to 0/10 |
8/16 |
PROM = patient reported outcome measure; MINORS = methodological index for non-randomized studies; NR = not reported; N/A = not applicable; GJL = generalized joint laxity; GLL = generalized ligamentous laxity; JHS; joint hypermobility syndrome; HSD = hypermobility syndrome disorder; EDS = ehlers danlos syndrome; CSS = constant-murley score; SANE = single assessment numeric evaluation; ASES = american shoulder and elbow surgeons score; PASS = Patient Acceptable Symptomatic State; QuickDASH = quick disabilities of the arm, shoulder and hand; SPONSA = shoulder pain and disability index; OSS = oxford shoulder score; ACR = anteroinferior capsular redundancy; aTSA = anatomic total shoulder arthroplasty; RTSA = reverse total shoulder arthroplasty; WOSI = western ontario shoulder instability index; “ ± ” = plus or minus; ≥ = greater than or equal to; “ᇫ” = delta, “change in”
Table 5.
Characteristics and results of elbow studies evaluating patients with joint hypermobility
| Divergent Elbow Dislocation | ||||||||||||||
| Study | Patients (Elbows) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Elbows, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) |
Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, (%)) | PROMs | MINORS |
| Onode et al. (2021) | 1 (1) |
Case Study (V) |
Rare injury. Satisfactory clinical outcomes following open repair of annular ligament, anterior oblique ligament and capsule in patient with EDS. No documented post operative instability |
EDS: 1 Diagnosed postoperatively by specialist & genetic testing |
EDS-musculocontractural type diagnosed with genetic testing | 0 (0) | 96.0 | 32 | 0 | NR | Open reduction elbow, repair annular ligament, repair of anterior oblique ligament, capsular tightening | 0 (0) |
VAS Pre: NR Post: 0 pt QuickDASH Pre: NR Post: 16.7/100 |
12/16 |
| Recurrent Ulnohumeral instability | ||||||||||||||
| Study | Patients (Elbows) | Study Design (Level of Evidence) | Study Main Finding | Hypermobility Diagnosis (Elbows, n) | EDS/Hypermobility Diagnostic Criteria | Loss to follow-up (n, (%)) | Follow-up time (months) | Mean age (years) |
Hypermobile Female (n) |
Beighton Score (mean) |
Treatment | Recurrent Instability or Tear (n, %) | PROMs | MINORS |
| Cole et al. (2000) | 2 (3) |
Case Study (V) |
All 3 patients happy with surgical outcome, all had loss of full extension while maintaining functional ROM | EDS: 3 | NR | 0 (0) | 24 | 34 | 3 | NR | Tricep splitting approach to distal humerus, block of corticocancellous graft from iliac crest placed in olecrannon fossa with 2 AO cortical screws | 0 (0) | NR | 11/16 |
PROM; patient reported outcome measure, MINORS; methodological index for non-randomized studies, NR; not reported, N/A; not applicable, GJL; generalized joint laxity, GLL; generalized ligamentous laxity, EDS; ehlers danlos syndrome, VAS; Visual Analog Scale, QuickDASH; Quick Disabilities of the Arm, Shoulder, and Hand score, “ ± ”; plus or minus, ≥; greater than or equal to, “ᇫ”; delta, “change in”
Thirty of the 38 studies described how hypermobility or EDS was diagnosed (Tables 1, 2, 3, 4 and 5). All studies that included description for hypermobility diagnosis utilized the Beighton score, with 19 studies using the nine point Beighton test and three studies using the five point Beighton test. Majority of studies utilizing the nine point Beighton test used a score of > 4 to diagnose hypermobility (n = 11), while a minority used a score of ≥ 5 (n = 7) or ≥ 6 (n = 1). All studies that used the five point Beighton test used a score of ≥ 4 to diagnose hypermobility. Diagnostic criteria used for EDS was not as widely reported and overall quite heterogeneous.
Hip
Femoroacetabular Impingement
Seven studies [15–21] consisting of 2012 patients (2031 hips) evaluated outcomes in patients undergoing surgical management for symptomatic femoroacetabular impingement (FAI) (Table 1). Six studies [15–18, 20, 21] consisting of 1932 patients reported on hypermobility status, with a total of 458 patients (23.7%) with generalized hypermobility and 14 patients (0.72%) with a formal diagnosis of EDS. The mean age was 30.2 years (range: 16–65), with females comprising 1378 (68.5%) of the total patient cohort. Average follow up was 40.8 months (range: 12–99). The Beighton score was reported in five [15, 16, 18–21] of the studies, with four noting a mean Beighton score of four or greater in their hypermobility cohort. Although the remaining study [16] reported a mean Beighton score of 2.5, 34% of their patient cohort had a Beighton score of four or greater, and 18% had a score of six or more.
Six of the seven studies evaluated surgical outcomes in patients undergoing hip arthroscopy with additional concomitant procedures for relevant central compartment (ex: labral tears, pincer lesions) and peripheral compartment (ex: CAM lesions) pathology. One study [16] also included patients who underwent mini-open procedures to address their FAI due to surgeon preference. Four studies [15, 18, 20, 21] consisting of 383 hypermobile patients provided specific data on additional surgical procedures performed on patients with generalized hypermobility or EDS in addition to hip arthroscopy. Of the 383 patients in these studies, there were 356 patients (92.3%) that also underwent femoroplasty and 285 patients (74.4%) acetabuloplasty, 285 (74.4%) iliopsoas tendon fractional lengthening or release, 35 (9.1%) ligamentum teres debridement, and 26 (6.8%) subspine decompression. For labral pathology, 369 (96.3%) underwent labral repair, 16 (4.2%) resection, nine (2.3%) isolated debridement, and four (1.0%) reconstruction. For capsular pathology and closure, 367 (95.8%) patients underwent capsular repair or plication and 16 (4.2%) capsular release. All four studies indicated that patients with pre-operative hypermobility or EDS underwent capsular plication or repair unless otherwise indicated.
Four studies [15, 16, 18, 20] compared outcomes in patients with and without hypermobility. Various PROMs were assessed, with the most common being the Modified Harris Hip score (mHHS), Visual Analog Scale (VAS) for pain, and the various subtypes of the Hip Disability & Osteoarthritis Outcome Score (HOOS). In general, all four of the comparative studies found comparable outcomes in terms of improvement in PROMs and failure rates at short to mid-term follow up periods, although one study [20] did note statistically significantly higher satisfaction scores in their non-hypermobile group compared to their hypermobile group at two years follow up (n = 145, 8.43 (7.93–8.93) vs. 7.71 (7.10–8.33); p = 0.012) despite no statistically significant differences in other evaluated PROMs such as mHHS, Non-Arthritic Hip Score (NAHS), HOS-Sports Specific Subscale (SSS), International Hip Outcome Tool (iHOT-12), Veterans RAND 12-Item Health Survey (VR-12), and Short Form health survey (SF-12). No study found a statistically significant difference in post-operative failure or revision surgery among patients with and without hypermobility following hip arthroscopy for FAI, although one study [16] interestingly noted a significantly lower Beighton score in patients with objective post-surgical failure compared to non-failures (n = 11 failures, 1.6 vs. 2.6; p = 0.049).
In two of the comparative studies [15, 20], authors noted arthroscopic capsular plication or repair was performed in all patients, including those without hypermobility, unless pre-operative stiffness was documented. Another study [18] compared outcomes following hip arthroscopy for FAI, with capsule closure only performed in the hypermobile group. They concluded FAI patients with hypermobility had similar significant improvements compared to a matched cohort of FAIS patients without hypermobility at two years following surgery across a variety of PROM scores and that both cohorts achieved the Minimal Clinically Important Difference (MCID) for each HOOS sub-score (HOOS-symptoms, pain, ADL, sports, and QOL) at equivalent rates (70–88%). One study [16] evaluated the prevalence of hypermobility in FAI patients and its effect on outcomes included both arthroscopic and mini-open procedures due to surgeon preference. They performed a logistic regression to assess for predictive risk factors of subjective and objective failure post-operatively, and noted hypermobility was not consistently associated with subjective failures (OR 1.0 (0.8–1.2); p = 0.778) or objective failures (OR 1.0 (0.7–1.3); p = 0.0802).
Only one non-comparative study [17] had an all-EDS patient cohort that underwent hip arthroscopy for FAI with capsular plication/repair performed at end of procedure. They found statistically significant improvement in all outcome measures (mHHS, p = 0.002; SF-12 score, p = 0.027, and VAS score, p = 0.0004) and 93.8% of patients reported no feeling of subjective instability or giving way at final follow up (45 months, range 12–99). One hip (6.25%) underwent revision arthroscopy and capsular plication for recurrent pain and subjective giving-way episodes in the context of a previous hip arthroscopy prior to study.
One retrospective study [19] looking at patients undergoing hip arthroscopy for labral repair and FAI reported that patients with higher Beighton scores (≥ 4) are at a significantly increased risk of developing post-operative iliopsoas tendonitis following hip arthroscopy for FAI and labral pathology compared with lower Beighton scores (< 4). Another prospective study noted that patients presenting for hip arthroscopy are generally younger, have a lower BMI, and are more often female compared to patients with lesser degrees of laxity. They also noted that patients with higher pre-operative Beighton scores had increased hip ROM, smaller intra-operative labral size and tear dimensions, and were more likely to undergo labral repair, capsular plication, and iliopsoas fractional lengthening (p < 0.0001).
Ligamentum Teres Tears
Two studies [22, 23] comprising 10 patients (12 hips) investigated outcomes in patients undergoing arthroscopic ligamentum teres reconstruction (LTR) (Table 1). A total of eight hips (66.7%) had a formal diagnosis of EDS. Of the 10 patients, seven (70%) were female and all had diagnoses of EDS.. The mean age was 36.7 years (range: 17–44), and average follow up was 34.1 months (range: 24–72). One study [22] assessed the Beighton score, reported as four or greater in all nine patients.
All patients underwent arthroscopic LTR, one study [23] utilized tibialis anterior allograft while the other used either semitendinosus autograft or tibialis anterior allograft. Concomitant procedures were commonly performed, the most common being labral repair and capsular repair or plication (n = 12, 100%), femoroplasty (n = 7, 58.3%), acetabuloplasty (n = 3, 25%), and iliopsoas release (n = 2, 16.7%).
One study [22] noted statistically significant improvement in post-operative mHHS, NAHS, and VAS scores (p < 0.05) in nine of their eleven hips (81.8%), however, these results were not compared to non-EDS patients included within the study. Two hips within this study had unfavorable outcomes, both undergoing conversion to total hip arthroplasty (THA) at a mean of 21.2 months following surgery. The second study [23] followed a female patient with EDS, and noted improvement in all measured PROMs (mHHS, HOS-Activities of Daily Living, HOS-SSS, NAHS, VAS, satisfaction score) at three months and one year but did not report significance. There were no reported complications within the one year follow up period.
Knee
Patellofemoral Instability
Six studies [24–28] consisting of 470 patients (516 knees) investigated patients with patellofemoral instability, with 391 (75.8%) knees being classified as hypermobile (Table 2). A total of 240 and 121 patients had EDS and generalized joint hypermobility, respectively. Less common causes of hypermobility included trichorhinophalangeal (n = 2), McCune-Albright (n = 1), and Klippel-Feil (n = 1), and Down’s syndrome (n = 3). The mean age of patients with hypermobility amongst studies reporting values was 31.1 years (range of means:14.8–35 YEARS). A total of 131/262 (71.6%; range: 41.2–100%) with reported sex were female. Mean follow-up time was 20.6 months (range of means: 15–86.4 months). Three studies [25, 27, 29] reported on Beighton scores, with one reporting a mean value amongst patients (6.8) [25], and two reporting cutoffs for hypermobility as > 4 or ≥ 6 [27, 29]. Loss to follow-up ranged from 0–8%.
Amongst all hypermobile patients, 391 underwent patellar stabilization surgery (208 unspecified, 166 isolated medial patellofemoral ligament reconstruction (MPFL-R), 17 MPFL-R + tibial tubercle osteotomy (TTO)). Of 391 surgical patients with hypermobility, 66 suffered a redislocation (16.0%; range: 0–25%). One patient required lateral patellofemoral ligament reconstruction after iatrogenic injury. Three studies investigated the role of hypermobility on outcomes, compared to a non-hypermobile cohort [24, 27, 29]. Two studies compared dislocation rates, with both reporting that hypermobility did not influence outcomes [24, 27]. One study compared PROMs, finding that IKDC and Kujala AKPS scores were statistically significantly lower in the hypermobile group (p < 0.001) [29].
Anterior Cruciate Ligament Reconstruction
Six studies [30–34] consisting of 819 patients (983 knees) investigated patients requiring anterior cruciate ligament reconstruction (ACLR), with 338 being classified as hypermobile. A total of 337 had GJH, with one patient having EDS. The mean age of patients with hypermobility was 26.8 years (range: 18–29.7 years). A total of 166 hypermobile patients (50.6%; range: 0–76.3%) were female. Mean follow-up time was 20.1 months(range of means: 12–36 months). Five studies reported on Beighton scores, with one study [30] reporting a mean score of 6, and two studies each reporting a threshold of four [31, 35] and five [34, 36] for hypermobility.
All patients underwent ACLR, with 31 patients in one study [33] undergoing anterolateral ligament internal bracing (ALL IB). Of 206 knees with retear statuses reported amongst four studies [30, 33, 34, 36], 21 (10.2%; range: 0–11.8%) suffered a re-injury.
Two studies evaluated the effect of hypermobility on retear rates [34, 36], with only one reporting statistically significant more re-tears within the hypermobile cohort (14% vs 2.9%, p = 0.012). One study [35] reported the role of hypermobility on anterior tibial translation (ATT), finding that increased hyperlaxity with thumb opposition (n = 272, ρ = 0.305, p = 0.001), little finger dorsiflexion (ρ = 0.271, p = 0.005), and knee hyperextension (ρ = 0.461, p = 0.000) predicted greater ATT. Three [31, 34, 36] studies reported on the effect of hypermobility on PROMs after ACLR, with two reporting no differences in KOOS scores between hypermobile and non-hypermobile groups. One study reported a statistically significant association between knee hyperextension (n = 272, ρ = −0.285, p = 0.000) [35].
The main focus of two studies were to compare different techniques for ACLR in the generalized joint hypermobility population [33, 35]. One study compared single bundle with double bundle ACLR, finding lower ATT via KT-2000 (p = 0.02) and higher Lysholm scores (p = 0.02) in the double-bundle group [35]. One study compared ACLR ± ALL IB, finding no differences in re-tears and PROMs but lower ATT and pivot-shift grades in the ALL-IB group [33].
Ankle
Nine studies [37–45] comprising 679 patients (689 ankles) evaluated outcomes in patients with chronic lateral ankle instability (CLAI) undergoing open, anatomic, or combined procedures, including the modified Brostrom-Operation (MBO) or anatomic reconstruction (AR) with grafting (Table 3). Eight studies [37–44] comprising 666 patients (674 ankles) reported hypermobility status, with 320 patients classified as generalized hypermobility based on Beighton score. There were no patients reported to have a formal diagnosis of EDS. The mean age was 28.8 years (range 16–69 years), and mean follow up was 34.8 (12–97 months). Females comprised 50.3% (161 patients) of the total hypermobility patient population. The Beighton score was mentioned in all studies, and a score of ≥ 4 or 5 was generally reported as criteria for diagnosis of hypermobility.
All nine studies evaluated outcomes in patients undergoing surgical management of CLAI, eight of which documented hypermobility for a total of 320 patients under the generalized joint laxity category. The majority of these patients (n = 189, 58.9%) underwent a combined arthroscopic and open procedure when indicated, while 76 patients (24.1%) underwent an all-open procedure, and 56 (17.8%) underwent an all-arthroscopic procedure. In terms of procedure specifics, all patients who underwent arthroscopic procedures underwent an Modified-Brostrom Operation (MBO) with anterior talofibular ligament (ATFL) repair using inferior extensor retinaculum augmentation. Within the open or combined surgical procedures, 19 patients (7.2%) underwent AR using gracilis autograft. There were 197 patients (74.3%) who underwent MBO without augmentation using suture anchors alone, while 49 patients (18.5%) underwent MBO with augmentation. One study utilized the ligament augmentation reconstruction system (LARS) in 21 patients (42.9%), while the other study utilized internal bracing with suture tape as their augmentation in 28 patients (57.1%).
Four studies [39, 40, 42, 44] compared surgical outcomes in patients with hypermobility to non-hypermobile controls across various established procedures for CLAI. Two studies [42, 44] comparing open MBO without augmentation using suture anchors both noted significantly inferior results in the hypermobility cohorts for post-operative PROMs and rate of recurrent instability or failure (p < 0.001, p < 0.05). One study [42] consisting of 34 hypermobile patients demonstrated significantly worse post-operative Karlsson scores (82.8 ± 7.3 vs. 89.0 ± 6.6; p < 0.001) and higher rates of post-operative recurrent instability (23.8% vs. 3.8%; p < 0.001) in the hypermobility group compared to non-hypermobile controls. They also noted a statistically significantly higher incidence of syndesmotic widening in the hypermobility group and that GLL was the most important independent predictor of clinical failure with an adjusted odds ratio (OR) of 5.3 (95% CI, 2.3–12.5; p < 0.001). Prognostic significance of GLL in CLAI was analyzed using Kaplan–Meier curves revealing significant associated with clinical failure of CLAI and estimated clinical success rate calculated at final follow up revealed statistically significantly inferior results in those with hypermobility compared to those without (53.7% vs. 87.5%; p < 0.001). The second study demonstrated similar results, with significantly lower Karlsson, AOFOS, and Tegner scores (n = 100, p < 0.05) and higher rates of post-operative re-rupture or recurrent LAI (n = 100, p = 0.045). They noted in the 5 hypermobile patients (11.4%) that failed post-operatively, the Beighton score was seven in two patients and nine in three patients.
One study [39] compared results following MBO with LARS augmentation in hypermobile patients (n = 21), non-hypermobile controls (n = 21) and a third high-risk comparative group of non-hypermobile patients > 90 kg (n = 21). They noted all three patient groups had a statistically significant improvement in pre-operative TAS and FAOS at both two and five years follow up (p < 0.001), and no statistically significant differences in scores between the GLL and control groups at same follow up intervals for both TAS and FAOS. There were no reported episodes of recurrent instability or revision surgery at five year follow up in any group.
One study [40] compared results following all-arthroscopic MBO procedure, with no statistically significant differences noted at the final one-year follow-up for VAS and AOFAS score between hypermobile (n = 24) and non-hypermobile (n = 75) groups. Change in talar tilt angle from pre-operative to one year post-operative was statistically significantly greater in the hypermobility group (−6.9 ± 5.2 vs. −4.2 ± 4.2; p = 0.03), while no significant difference in actual talar tilt angle was noted between the groups.
Two studies [37, 38] compared differences in outcomes in patients with hypermobility undergoing various procedures for CLAI. One study [37] evaluated open MBO versus anatomic reconstruction with gracilis autograft in patients with hypermobility and found better clinical outcomes, less sprain recurrence and higher rate of return to pre-injury high demand sports following anatomic reconstruction. One study [38] evaluated open versus arthroscopic MBO in patients with hypermobility and noted no statistically significant differences between the groups in terms of functional scores, stress radiography, or failure rate post-operatively. However, the overall failure rate in the study was high at 19.7% (n = 32), although no statistically significant difference was found between failure rates in open and arthroscopic groups (16.1% vs. 23.3%).
Shoulder
Glenohumeral Instability
Six studies [46–51] comprising 140,616 patients (140,625 shoulders) assessed surgical management for glenohumeral instability (Table 4). Five of the six studies [46–49, 51] consisting of 140,546 shoulders, reported hypermobility status, with a total of 804 shoulders classified as hypermobile. There were 11 patients reported to have EDS, 37 generalized hypermobility, and one study [46] grouped 756 hypermobile patients as “EDS or generalized joint laxity”. Mean follow-up was 45.0 months. Among the hypermobile cohort, there were 44 female patients (40.6%), although sex was not reported in one study [46] that documented hypermobility status. The Beighton score was reported in four of the six studies [47, 49–51] as ≥ 6.
Amongst hypermobile patients, there were 112 open procedures (18 inferior capsular shift, 20 Bankart repair, 19 Latarjet, 55 unspecified). Of 617 arthroscopic procedures in this group, 616 were stabilization procedures while one was a latissimus dorsi transfer with concomitant pectoralis minor release).
Of 804 hypermobile patients, 40 patients (5.0%; range 0–47%) suffered a repeat dislocation, with the study reporting a rate of 47% reporting on patients with multidirectional stability [51].One study compared redislocation rates in patients with or without hypermobility, finding no statistically significant differences at 24 months post-operatively [46]. Patient Reported Outcome Measures (PROMs) including American Shoulder and Elbow Surgeons (ASES) scores, quickDASH, Single Assessment Numeric Evaluation (SANE), and Visual Analogue Scale (VAS) scores generally improved pre- to post-operatively. One study reported higher Beighton scores were associated with worse Western Ontario Shoulder Instability (WOSI) index values (p < 0.001) [50]. Another study compared patients with diagnosed Type III EDS and GJH, finding that the EDS group had worse ASES scores than the GJH group (71 vs 92, p < 0.05) [48].
Elbow
Two studies [52, 53] consisting of three patients (four elbows) evaluated surgical outcomes in patients with elbow instability in the setting of EDS (Table 5). The mean age was 34, and two (67%) of the patients were female. Mean follow up was 60 months (range 24–99 months).
One study [52] as a case report on a 32 year old man with EDS who sustained an acute transverse, divergent elbow dislocation following a snowboarding injury. He demonstrated satisfactory clinical outcomes on limited evaluation with PROMs and did not report any instability at eight year follow up.
The second study [53] evaluated two patients (three elbows) with chronic ulnohumeral instability that underwent open ulnohumeral stabilization with bony block to limit extension. Pre-operatively, both patients had elbow range of motion (ROM) from −30 to full flexion. One patient dislocated consistently at neutral extension, while the other demonstrated positive apprehension at 20 degrees from full extension. At one year post-operation, neither patient reported instability and had a functional ROM of at least 35 degrees to full flexion.
Discussion
The primary findings of this review were that patients with joint hypermobility either have similar or worse outcomes in surgical management for various sports medicine procedures for hips, knees, shoulders, and elbows and overall worse surgical outcomes in sports procedures involving the ankle. Female patients consisted of at least 50% of all patients, with larger numbers in presentations related to the hip and knee compared to other joints. There were very few studies that characterized their post-surgical complications or failures by sex, making it difficult to assess for any sex-based differences.
There has been recent interest in including joint hypermobility in consultation for sports medicine injuries, with the primary aim of improving outcomes in this patient population [36, 54, 55]. Several reasons exist for why some studies in this review found similar outcomes to non-hypermobile cohorts. One reason is that the diagnostic criteria using the Beighton scale may be over-representing the amount of patients with hypermobility. The majority of studies within all joint categories used a cutoff of four or more, which would group patients with a score of four with those with a score of nine, potentially skewing results. Some have proposed a threshold of five, or even six or more in adolescents, who tend to undergo the highest number of sports medicine procedures. Others have argued that the Beighton scale has an arbitrary selection of joints, and that a focus of hypermobility at the involved joint is important to avoid false positives [56]. The heterogeneity within the literature highlights the potential benefit of developing universally accepted gold standard diagnostic criteria for generalized joint hypermobility to aid in both diagnosis and managing surgical considerations.
Notably, all four studies concerning the ankle demonstrated statistically inferior outcomes in terms of re-injury in the GJH group. One systematic review of over 200,000 patients from multiple countries reported that the ankle was the most commonly injured joint in the majority of sports [57], therefore it is possible that there is a lower threshold of hypermobility that may cause recurrent injuries in the ankle. This is reinforced by reports of recurrent ankle injury in the GJH population to be as high as 93% [58]. Another reason for the conflicting results in reported differences between patients with and without hypermobility may be related to unreported surgical considerations that individual studies may have taken to address this phenomenon, likely introducing confounding variables. For example, concomitant LET in ACLR or paying special attention to capsular management in hip arthroscopy may improve outcomes that would otherwise have been less successful [54, 59].
This review highlighted some steps that surgeons can use to help improve outcomes in patients with hypermobility. For example, paying special attention to the anterolateral complex via ALL reinforcement was found to be beneficial in reducing anterior tibial translation and pivot shift grades in ACLR. Additionally, hamstring tendon autografts were found to be inferior to BPTB autografts in the hypermobile group. This was reported in a previous systematic review investigating GJH in ACLR as well, advocating for BPTB options in this group [36]. Hamstring options without concomitant LET have been associated with either similar or inferior outcomes in high-risk groups such as the revision ACLR population. Therefore, a similar principle may apply for the GJH group as another high-risk subsection of patients [14]. In the hip, one study found that patients with GJH were more likely to undergo capsular plication procedures to help tighten the capsule. A previous systematic review found that the most common surgical risk factor for iatrogenic hip instability after hip arthroscopy was an unrepaired capsulotomy, reinforcing the importance of capsular management, especially in the hypermobile population [60]. Similar to the hip, 35% of patients with hypermobility underwent capsular plication in patients undergoing arthroscopic stabilization of the shoulder for shoulder instability. Given the majority of studies did not directly compare surgical techniques and how they may contribute to outcomes for ankle instability, it is recommended that future high-quality studies investigate this topic.
There was a low number of studies investigating the effect of hypermobility on patients with elbow, hand or wrist conditions. Previous studies have reported a greater prevalence of hypermobility in ballet dancers and gymnasts [61], with the latter having a higher risk of elbow injuries, such as medial epicondylitis or ulnar collateral ligament (UCL) insufficiency. Furthermore, the repetitive loading of the wrist can lead to patients being ulnar positive, leading to triangular fibrocartilage complex (TFCC) tears. Given that these patients are at high risk, it is important for future studies to investigate the risk of hypermobility and how they affect non-surgical and surgical management of these conditions to better guide treatment decisions for physicians [62]. In addition, managing these patients with a multidisciplinary approach may be beneficial. For example, prolonged rehabilitation programs lasting up to four to six months may be beneficial, focusing on proprioception and balance-training [58].
Strengths and Limitations
The main strength of this review is that it involves a large amount of studies, providing an overview of how hypermobility may affect outcomes in patients undergoing a variety of surgical procedures based on joint. Limitations predominantly arise from the lack of high-quality studies (mainly level IV evidence). Furthermore, there was significant heterogeneity found in the literature for each joint evaluated, in terms of outcomes assessed, surgical techniques, and study design. Finally, there was a lack of studies in the literature on elbow and wrist pathology, with a relative overrepresentation of studies focusing on shoulder, knee, hip, and ankle pathologies. Future studies are encouraged to investigate how hypermobility may affect outcomes in patients undergoing TFCC repair, UCL reconstruction, or other sports medicine procedures related to the upper extremity.
Conclusion
Patients with joint hypermobility tend to have similar outcomes or slightly worse outcomes in patients undergoing sports medicine procedures related to the hip, knee, shoulder, and elbow and significantly worse outcomes in those conditions pertaining to the ankle, The most frequently reported threshold for hypermobility was a Beighton score of four or more amongst included studies. There are special considerations that can be performed for this patient population including anterolateral complex reinforcement in ACLR or capsular plication in hip arthroscopy.
Key References
- Schubart JR, Mills SE, Rodeo SA, Francomano CA. Outcomes of orthopaedic surgery in Ehlers-Danlos syndromes: a scoping review. BMC Musculoskelet Disord. 2024 Oct 24;25(1):846.
- A recent scoping review looking at surgical outcomes of general orthopaedic procedures in those with Ehlers-Danlos syndrome, noting inconsistent findings among various anatomical sites.
- Yonko EA, LoTurco HM, Carter EM, Raggio CL. Orthopedic considerations and surgical outcomes in Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2021 Dec;187(4):458–65.
- A recent systematic review look at surgical outcomes of 320 orthopedic surgeries, noting overall worse surgical outcomes in those with EDS compared to general population. Highlights heterogeneity within existing literature.
Supplementary Information
Below is the link to the electronic supplementary material.
(DOCX 2.18 MB)
Author Contributions
CS and AD developed the methods and prepared the manuscript. CS, SR, DB performed screening of titles and abstracts and full-text for inclusion in the review. All screening conflicts were resolved by CS. CS, PV, SR, VJ, AD, NS, and OA contributed significantly to the development of the methods and drafting of the manuscript. All authors reviewed the final manuscript.
Funding
None to disclose.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights
This review does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, et al. The 2017 international classification of the Ehlers–Danlos syndromes. Am J Med Genet C Semin Med Genet [Internet]. 2017 Mar [cited 2025 Mar 12];175(1):8–26. Available from: https://onlinelibrary.wiley.com10.1002/ajmg.c.31552. [DOI] [PubMed]
- 2.Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet C Semin Med Genet. 2017;175(1):148–57. [DOI] [PubMed] [Google Scholar]
- 3.Demmler JC, Atkinson MD, Reinhold EJ, Choy E, Lyons RA, Brophy ST. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case-control comparison. BMJ Open. 2019;9(11). [DOI] [PMC free article] [PubMed]
- 4.Tinkle B, Castori M, Berglund B, Cohen H, Grahame R, Kazkaz H, et al. Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome Type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. Am J Med Genet C Semin Med Genet. 2017 Mar;175(1):48–69. [DOI] [PubMed]
- 5.Rombaut L, Malfait F, Cools A, De Paepe A, Calders P. Musculoskeletal complaints, physical activity and health-related quality of life among patients with the Ehlers-Danlos syndrome hypermobility type. Disabil Rehabil. 2010;32(16):1339–45. [DOI] [PubMed] [Google Scholar]
- 6.Shirley ED, Demaio M, Bodurtha J. Ehlers-danlos syndrome in orthopaedics: etiology, diagnosis, and treatment implications. Sports Health. 2012;4(5):394–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henderson FC, Austin C, Benzel E, Bolognese P, Ellenbogen R, Francomano CA, et al. Neurological and spinal manifestations of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):195–211. [DOI] [PubMed] [Google Scholar]
- 8.Ericson WB, Wolman R. Orthopaedic management of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):188–94. [DOI] [PubMed] [Google Scholar]
- 9.Brady AF, Demirdas S, Fournel-Gigleux S, Ghali N, Giunta C, Kapferer-Seebacher I, et al. The Ehlers-Danlos syndromes, rare types. Am J Med Genet C Semin Med Genet. 2017;175(1):70–115. [DOI] [PubMed] [Google Scholar]
- 10.Schubart JR, Mills SE, Rodeo SA, Francomano CA. Outcomes of orthopaedic surgery in Ehlers-Danlos syndromes: a scoping review. BMC Musculoskelet Disord. 2024;25(1):846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yonko EA, LoTurco HM, Carter EM, Raggio CL. Orthopedic considerations and surgical outcomes in Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2021;187(4):458–65. [DOI] [PubMed] [Google Scholar]
- 12.McHugh ML. Interrater reliability: the kappa statistic. Biochem Medica. 2012;22(3):276–82. [PMC free article] [PubMed] [Google Scholar]
- 13.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non‐randomized studies ( MINORS ): development and validation of a new instrument. ANZ J Surg [Internet]. 2003 Sep [cited 2025 Mar 12];73(9):712–6. Available from: https://onlinelibrary.wiley.com/doi/10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed]
- 14.Vivekanantha P, Kahlon H, Hassan Z, Slawaska‐Eng D, Abdel‐Khalik H, Johnson J, et al. Hamstring autografts demonstrate either similar or inferior outcomes to quadriceps or bone–patellar tendon–bone autografts in revision anterior cruciate ligament reconstruction: A systematic review of comparative studies. Knee Surg Sports Traumatol Arthrosc [Internet]. 2025 Feb [cited 2025 Mar 12];33(2):413–27. Available from: https://esskajournals.onlinelibrary.wiley.com/doi/10.1002/ksa.12366. [DOI] [PubMed]
- 15.Stone AV, Mehta N, Beck EC, Waterman BR, Chahla J, Ukwuani G, et al. Comparable patient-reported outcomes in females with or without joint hypermobility after hip arthroscopy and capsular plication for femoroacetabular impingement syndrome. J Hip Preserv Surg [Internet]. 2019 Jan 1 [cited 2025 Mar 16];6(1):33–40. Available from: https://academic.oup.com/jhps/article/6/1/33/5381112. [DOI] [PMC free article] [PubMed]
- 16.Naal FD, Müller A, Varghese VD, Wellauer V, Impellizzeri FM, Leunig M. Outcome of Hip Impingement Surgery: Does Generalized Joint Hypermobility Matter? Am J Sports Med [Internet]. 2017 May [cited 2025 Mar 16];45(6):1309–14. Available from: https://journals.sagepub.com10.1177/0363546516688636. [DOI] [PubMed]
- 17.Larson CM, Stone RM, Grossi EF, Giveans MR, Cornelsen GD. Ehlers-Danlos Syndrome: Arthroscopic Management for Extreme Soft-Tissue Hip Instability. Arthrosc J Arthrosc Relat Surg [Internet]. 2015 Dec [cited 2025 Mar 16];31(12):2287–94. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806315004971. [DOI] [PubMed]
- 18.Soriano KKJ, Hartwell MJ, Nguyen TQ, Flores SE, Zhang AL. Hypermobile Patients With Femoroacetabular Impingement Syndrome Can Be Effectively Treated Utilizing Hip Arthroscopy With Periportal Capsulotomy Closure: A Matched Cohort Analysis Compared to Patients Without Joint Hypermobility. Arthrosc J Arthrosc Relat Surg [Internet]. 2023 Sep [cited 2025 Mar 16];39(9):2026–34. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806323002402. [DOI] [PubMed]
- 19.Mojica ES, Rynecki ND, Akpinar B, Haskel JD, Colasanti CA, Gipsman A, et al. Joint Hypermobility Is Associated With Increased Risk of Postoperative Iliopsoas Tendinitis After Hip Arthroscopy for Femoroacetabular Impingement. Arthrosc J Arthrosc Relat Surg [Internet]. 2022 Aug [cited 2025 Mar 16];38(8):2451–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806322001165. [DOI] [PubMed]
- 20.Maldonado DR, Chen JW, Yelton MJ, Rosinsky PJ, Shapira J, Brayboy C, et al. Achieving Successful Outcomes of Hip Arthroscopy in the Setting of Generalized Ligamentous Laxity With Labral Preservation and Appropriate Capsular Management: A Propensity Matched Controlled Study. Am J Sports Med [Internet]. 2020 Jun [cited 2025 Mar 16];48(7):1625–35. Available from: https://journals.sagepub.com10.1177/0363546520914604. [DOI] [PubMed]
- 21.Saadat AA, Lall AC, Battaglia MR, Mohr MR, Maldonado DR, Domb BG. Prevalence of Generalized Ligamentous Laxity in Patients Undergoing Hip Arthroscopy: A Prospective Study of Patients’ Clinical Presentation, Physical Examination, Intraoperative Findings, and Surgical Procedures. Am J Sports Med [Internet]. 2019 Mar [cited 2025 Mar 16];47(4):885–93. Available from: https://journals.sagepub.com10.1177/0363546518825246. [DOI] [PubMed]
- 22.Rosinsky PJ, Annin S, Maldonado DR, Kyin C, Meghpara MB, Shapira J, et al. Arthroscopic Ligamentum Teres Reconstruction: Minimum 2-Year Patient-Reported Outcomes With Subanalysis of Patients With Ehlers-Danlos Syndrome. Arthrosc J Arthrosc Relat Surg [Internet]. 2020 Aug [cited 2025 Mar 16];36(8):2170–82. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806320303455. [DOI] [PubMed]
- 23.Hammarstedt JE, Redmond JM, Gupta A, Domb BG. Arthroscopic Ligamentum Teres Reconstruction of the Hip in Ehlers-Danlos Syndrome: A Case Study. HIP Int [Internet]. 2015 May [cited 2025 Mar 16];25(3):286–91. Available from: https://journals.sagepub.com10.5301/hipint.5000228. [DOI] [PubMed]
- 24.Kutschke MJ, Albright JA, Winschel JM, He EW, Cruz AI, Daniels AH, et al. Increased Risk of Patellofemoral Instability Events and Surgical Management in Patients With Joint Hypermobility Syndromes: A Matched Cohort Analysis. Arthrosc Sports Med Rehabil [Internet]. 2024 Dec [cited 2025 Mar 16];6(6):100995. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666061X24001329. [DOI] [PMC free article] [PubMed]
- 25.Parikh SN, Nemunaitis J, Wall EJ, Cabatu C, Gupta R, Veerkamp MW. Midterm Outcomes of Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability in Ehlers-Danlos Syndrome. Orthop J Sports Med [Internet]. 2024 Jun [cited 2025 Mar 16];12(6):23259671241241096. Available from: https://journals.sagepub.com10.1177/23259671241241096. [DOI] [PMC free article] [PubMed]
- 26.Imerci A, McDonald TC, Rogers KJ, Thacker MM, Atanda A. Outcomes of medial patellofemoral ligament reconstruction and tibial tubercle osteotomy in syndromic adolescents with patellar dislocation. J Clin Orthop Trauma [Internet]. 2022 Feb [cited 2025 Mar 16];25:101770. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0976566222000066. [DOI] [PMC free article] [PubMed]
- 27.Hiemstra LA, Kerslake S, Kupfer N, Lafave MR. Generalized joint hypermobility does not influence clinical outcomes following isolated MPFL reconstruction for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc [Internet]. 2019 Nov [cited 2025 Mar 16];27(11):3660–7. Available from: https://link.springer.com/10.1007/s00167-019-05489-0. [DOI] [PubMed]
- 28.Shubert DJ, McDonough EB. Bilateral Medial and Lateral Patellofemoral Ligament Reconstruction in a Patient with Hypermobility Type Ehlers-Danlos Syndrome: A Case Report. JBJS Case Connect [Internet]. 2019 [cited 2025 Mar 16];9(3):e0359–e0359. Available from: https://journals.lww.com/01709767-201909000-00022. [DOI] [PubMed]
- 29.Howells NR, Eldridge JD. Medial patellofemoral ligament reconstruction for patellar instability in patients with hypermobility: A case control study. J Bone Joint Surg Br [Internet]. 2012 Dec [cited 2025 Mar 16];94-B(12):1655–9. Available from: https://online.boneandjoint.org.uk10.1302/0301-620X.94B12.29562. [DOI] [PubMed]
- 30.Hishimura R, Kondo E, Matsuoka M, Iwasaki K, Kawaguchi Y, Suzuki Y, et al. Double-bundle anterior cruciate ligament reconstruction using autologous hamstring tendon hybrid grafts in a patient with hypermobile Ehlers-Danlos Syndrome: A case report. The Knee [Internet]. 2022 Mar [cited 2025 Mar 16];35:81–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0968016022000138. [DOI] [PubMed]
- 31.Kim SJ, Moon HK, Kim SG, Chun YM, Oh KS. Does Severity or Specific Joint Laxity Influence Clinical Outcomes of Anterior Cruciate Ligament Reconstruction? Clin Orthop [Internet]. 2010 Apr [cited 2025 Mar 16];468(4):1136–41. Available from: https://journals.lww.com/00003086-201004000-00031. [DOI] [PMC free article] [PubMed]
- 32.Sundemo D, Senorski EH, Samuelsson K. Editorial Commentary: Diagnosis and Treatment of Generalized Joint Hypermobility in Patients With Anterior Cruciate Ligament Injury. Arthrosc J Arthrosc Relat Surg [Internet]. 2021 Jul [cited 2025 Mar 12];37(7):2348–50. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806321002929. [DOI] [PubMed]
- 33.Toker MB, Erden T, Toprak A, Taşer ÖF. Does anterolateral ligament internal bracing improve the outcomes of anterior cruciate ligament reconstruction in patients with generalized joint hypermobility? Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES. 2022;28(3):320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zsidai B, Piussi R, Thomeé R, Sundemo D, Musahl V, Samuelsson K, et al. Generalised joint hypermobility leads to increased odds of sustaining a second ACL injury within 12 months of return to sport after ACL reconstruction. Br J Sports Med [Internet]. 2023 Aug [cited 2025 Mar 16];57(15):972–9. Available from: https://bjsm.bmj.com/lookup10.1136/bjsports-2022-106183. [DOI] [PMC free article] [PubMed]
- 35.Kim SJ, Chang JH, Kim TW, Jo SB, Oh KS. Anterior Cruciate Ligament Reconstruction with Use of a Single or Double-Bundle Technique in Patients with Generalized Ligamentous Laxity: J Bone Jt Surg-Am Vol [Internet]. 2009 Feb [cited 2025 Mar 16];91(2):257–62. Available from: http://journals.lww.com/00004623-200902000-00001. [DOI] [PubMed]
- 36.Sundemo D, Hamrin Senorski E, Karlsson L, Horvath A, Juul-Kristensen B, Karlsson J, et al. Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. BMJ Open Sport Exerc Med [Internet]. 2019 Nov [cited 2025 Mar 12];5(1):e000620. Available from: https://bmjopensem.bmj.com/lookup10.1136/bmjsem-2019-000620. [DOI] [PMC free article] [PubMed]
- 37.Wang A, Jiang Y, Su T, Xie X, Jiao C, Hu Y, et al. Clinical Outcomes and Return to Preinjury Sports After Anatomic Reconstruction With a Gracilis Autograft Versus the Modified Broström Procedure in Patients With Generalized Joint Laxity. Orthop J Sports Med [Internet]. 2024 Mar [cited 2025 Mar 18];12(3):23259671241229443. Available from: https://journals.sagepub.com10.1177/23259671241229443. [DOI] [PMC free article] [PubMed]
- 38.Wang A hong, Su T, Jiang Y fang, Zhu Y chuan, Jiao C, Hu Y lin, et al. Arthroscopic modified Broström procedure achieved similar favorable short term outcomes to open procedure for chronic lateral ankle instability cases with generalized joint laxity. Knee Surg Sports Traumatol Arthrosc [Internet]. 2023 Sep [cited 2025 Mar 18];31(9):4043–51. Available from: https://link.springer.com/10.1007/s00167-023-07431-x. [DOI] [PubMed]
- 39.Porter MD, Trajkovska A, Georgousopoulou E. Ligament Augmentation Reconstruction System (LARS) for Ankle Lateral Ligament Reconstruction in Higher-Risk Patients: A 5-Year Prospective Cohort Study. Orthop J Sports Med [Internet]. 2022 May 1 [cited 2025 Mar 18];10(5):23259671221093968. Available from: https://journals.sagepub.com10.1177/23259671221093968. [DOI] [PMC free article] [PubMed]
- 40.Yeo ED, Park JY, Kim JH, Lee YK. Comparison of Outcomes in Patients With Generalized Ligamentous Laxity and Without Generalized Laxity in the Arthroscopic Modified Broström Operation for Chronic Lateral Ankle Instability. Foot Ankle Int [Internet]. 2017 Dec [cited 2025 Mar 18];38(12):1318–23. Available from: https://journals.sagepub.com10.1177/1071100717730336. [DOI] [PubMed]
- 41.Cho BK, Park KJ, Park JK, SooHoo NF. Outcomes of the Modified Broström Procedure Augmented With Suture-Tape for Ankle Instability in Patients With Generalized Ligamentous Laxity. Foot Ankle Int [Internet]. 2017 Apr [cited 2025 Mar 16];38(4):405–11. Available from: https://journals.sagepub.com10.1177/1071100716683348. [DOI] [PubMed]
- 42.Park KH, Lee JW, Suh JW, Shin MH, Choi WJ. Generalized Ligamentous Laxity Is an Independent Predictor of Poor Outcomes After the Modified Broström Procedure for Chronic Lateral Ankle Instability. Am J Sports Med [Internet]. 2016 Nov [cited 2025 Mar 18];44(11):2975–83. Available from: https://journals.sagepub.com10.1177/0363546516656183. [DOI] [PubMed]
- 43.Huang B, Kim YT, Kim JU, Shin JH, Park YW, Kim HN. Modified Broström Procedure for Chronic Ankle Instability With Generalized Joint Hypermobility. Am J Sports Med [Internet]. 2016 Apr [cited 2025 Mar 18];44(4):1011–6. Available from: https://journals.sagepub.com10.1177/0363546515623029. [DOI] [PubMed]
- 44.Xu HX, Lee KB. Modified Broström Procedure for Chronic Lateral Ankle Instability in Patients With Generalized Joint Laxity. Am J Sports Med [Internet]. 2016 Dec [cited 2025 Mar 18];44(12):3152–7. Available from: https://journals.sagepub.com10.1177/0363546516657816. [DOI] [PubMed]
- 45.Cheng M, Tho KS. Chrisman-Snook ankle ligament reconstruction outcomes–a local experience. Singapore Med J. 2002;43(12):605–9. [PubMed] [Google Scholar]
- 46.Winschel JM, Albright JA, Testa EJ, Kent VF, Byrne RA, He EW, et al. Surgical management of glenohumeral instability in patients with Ehlers-Danlos syndrome/hypermobility spectrum disorder and their risk of reoperation. JSES Rev Rep Tech [Internet]. 2024 Nov [cited 2025 Mar 19];4(4):757–61. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666639124000464. [DOI] [PMC free article] [PubMed]
- 47.Khawaja SR, Hussain ZB, Cooke H, Stern E, Karzon A, Gottschalk MB, et al. Dynamically rebalancing the unstable shoulder in Ehlers-Danlos syndrome: latissimus dorsi transfer for posterior shoulder instability. JSES Int [Internet]. 2024 Sep [cited 2025 Mar 19];8(5):954–62. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666638324001312. [DOI] [PMC free article] [PubMed]
- 48.Dewing CB, Horan MP, Millett PJ. Two-Year Outcomes of Open Shoulder Anterior Capsular Reconstruction for Instability From Severe Capsular Deficiency. Arthrosc J Arthrosc Relat Surg [Internet]. 2012 Jan [cited 2025 Mar 19];28(1):43–51. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806311006621. [DOI] [PubMed]
- 49.Abdelhady A, Abouelsoud M, Eid M. Latarjet procedure in patients with multiple recurrent anterior shoulder dislocation and generalized ligamentous laxity. Eur J Orthop Surg Traumatol [Internet]. 2015 May [cited 2025 Mar 19];25(4):705–8. Available from: http://link.springer.com/10.1007/s00590-014-1558-1. [DOI] [PubMed]
- 50.Yang JS, Mazzocca AD, Cote MP, Edgar CM, Arciero RA. Recurrent Anterior Shoulder Instability With Combined Bone Loss: Treatment and Results With the Modified Latarjet Procedure. Am J Sports Med [Internet]. 2016 Apr [cited 2025 Mar 19];44(4):922–32. Available from: https://journals.sagepub.com10.1177/0363546515623929. [DOI] [PubMed]
- 51.Vavken P, Tepolt FA, Kocher MS. Open inferior capsular shift for multidirectional shoulder instability in adolescents with generalized ligamentous hyperlaxity or Ehlers-Danlos syndrome. J Shoulder Elbow Surg [Internet]. 2016 Jun [cited 2025 Mar 19];25(6):907–12. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1058274615005819. [DOI] [PubMed]
- 52.Onode E, Takamatsu K, Kuroda T, Kazuki K, Nakamura H. Divergent Dislocation of the Elbow in an Adult with Ehlers–Danlos Syndrome: A Case Report. JBJS Case Connect [Internet]. 2021 Jul [cited 2025 Mar 16];11(3). Available from: https://journals.lww.com/10.2106/JBJS.CC.21.00159. [DOI] [PubMed]
- 53.Cole AS, Hill GA, Abela M, Carr AJ. Recurrent instability of the elbow in the Ehlers-Danlos syndrome: A REPORT OF THREE CASES AND A NEW TECHNIQUE OF SURGICAL STABILISATION. J Bone Joint Surg Br [Internet]. 2000 Jul [cited 2025 Mar 16];82-B(5):702–4. Available from: https://online.boneandjoint.org.uk10.1302/0301-620X.82B5.0820702. [DOI] [PubMed]
- 54.Owusu-Akyaw KA. Editorial Commentary: Successful Hip Arthroscopy for Patients With Hypermobility Requires a Patient-centric Approach, Meticulous Capsular Management, and Preservation of the Fibrous Capsular Ligaments. Arthrosc J Arthrosc Relat Surg [Internet]. 2023 Sep [cited 2025 Mar 12];39(9):2035–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806323003304. [DOI] [PubMed]
- 55.Zsidai B, Kaarre J, Svantesson E, Piussi R, Musahl V, Samuelsson K, et al. The days of generalised joint hypermobility assessment in all patients with ACL injury are here. Br J Sports Med [Internet]. 2024 May [cited 2025 Mar 12];58(9):461–3. Available from: https://bjsm.bmj.com/lookup10.1136/bjsports-2023-107188. [DOI] [PubMed]
- 56.Malek S, Reinhold EJ, Pearce GS. The Beighton Score as a measure of generalised joint hypermobility. Rheumatol Int [Internet]. 2021 Oct [cited 2025 Mar 12];41(10):1707–16. Available from: https://link.springer.com/10.1007/s00296-021-04832-4. [DOI] [PMC free article] [PubMed]
- 57.Fong DTP, Hong Y, Chan LK, Yung PSH, Chan KM. A Systematic Review on Ankle Injury and Ankle Sprain in Sports: Sports Med [Internet]. 2007 [cited 2025 Mar 12];37(1):73–94. Available from: https://link.springer.com/10.2165/00007256-200737010-00006. [DOI] [PubMed]
- 58.Wolf JM, Cameron KL, Owens BD. Impact of Joint Laxity and Hypermobility on the Musculoskeletal System: Am Acad Orthop Surg [Internet]. 2011 Aug [cited 2025 Mar 12];19(8):463–71. Available from: http://journals.lww.com/00124635-201108000-00002. [DOI] [PubMed]
- 59.Getgood AMJ, Bryant DM, Litchfield R, Heard M, McCormack RG, Rezansoff A, et al. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am J Sports Med [Internet]. 2020 Feb [cited 2025 Mar 12];48(2):285–97. Available from: https://journals.sagepub.com10.1177/0363546519896333. [DOI] [PubMed]
- 60.Yeung M, Memon M, Simunovic N, Belzile E, Philippon MJ, Ayeni OR. Gross Instability After Hip Arthroscopy: An Analysis of Case Reports Evaluating Surgical and Patient Factors. Arthrosc J Arthrosc Relat Surg [Internet]. 2016 Jun [cited 2025 Mar 12];32(6):1196–1204.e1. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0749806316000414. [DOI] [PubMed]
- 61.Schmidt H, Pedersen TL, Junge T, Engelbert R, Juul-Kristensen B. Hypermobility in Adolescent Athletes: Pain, Functional Ability, Quality of Life, and Musculoskeletal Injuries. J Orthop Sports Phys Ther [Internet]. 2017 Oct [cited 2025 Mar 12];47(10):792–800. Available from: https://www.jospt.org10.2519/jospt.2017.7682. [DOI] [PubMed]
- 62.Desai N, Vance DD, Rosenwasser MP, Ahmad CS. Artistic Gymnastics Injuries; Epidemiology, Evaluation, and Treatment. J Am Acad Orthop Surg [Internet]. 2019 Jul 1 [cited 2025 Mar 12];27(13):459–67. Available from: https://journals.lww.com/00124635-201907010-00001. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 2.18 MB)
Data Availability Statement
No datasets were generated or analysed during the current study.