Abstract
Aim
To examine and synthesize qualitative data regarding the experiences of stroke survivors who underwent rehabilitation using virtual reality (VR).
Methods
We critically appraised the included study using the Joanna Briggs Institute Critical Assessment Checklist for Qualitative Research. Relevant qualitative studies were searched in PubMed, EMBASE, CINAHL, Web of Science, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Database, China Science and Technology Journal Database, and China Biomedical Literature Database from inception to December 2024. Two researchers independently extracted and analysed the data and integrated the results using a pooled meta-aggregation approach.
Results
Sixteen studies (n = 145 stroke survivors) were included. A total of 5 meta-themes, 12 categories, and 38 research results were extracted. The meta-themes included perceived benefits, facilitating factors of using VR, and hindering factors of using VR, changes in the physical and mental health following VR rehabilitation, and suggestions and expectations for VR rehabilitation.
Conclusion
Stroke survivors perceived the benefits and barriers of using VR-based rehabilitation (VRBR); therefore, it is a complex perceptual change for them. They require emotional support from family and peers, professional support from healthcare professionals, and financial support from the government. Moreover, rehabilitation motivation is an important factor that influences utilization. Updating VRBR content and functionality is essential to improve user experience.
Systematic review registration
PROSPERO CRD42024504700, https://www.crd.york.ac.uk/PROSPERO/search.
Keywords: stroke, virtual reality, rehabilitation, experience, meta-synthesis
1. Introduction
Stroke, a leading cause of death and disability (1), incurs a global cost estimated at over US$721 billion, which is 0.66% of the global GDP (2). Rehabilitation therapy effectively reduces disability in stroke survivors (3). In China alone, approximately 25 million stroke survivors required rehabilitation therapy in 2019 (4). Traditional rehabilitation treatments include physical therapy (5), speech therapy (6) and occupational therapy (7). New assistive technologies for rehabilitation therapy, such as virtual reality (VR), rehabilitation robots, and remote rehabilitation technology (8), are valued for their convenience and task-oriented training. VR combines computer graphics technology and related equipment, providing immersive and interactive virtual environments for patients and obtaining real-time feedback on their performance through multiple senses (9). Virtual reality-based rehabilitation (VRBR) can be tailored to a patient’s needs and is a personalized and progressive rehabilitation method (10). Currently, numerous quantitative studies have confirmed the effectiveness of VRBR on the upper limb (11), lower limb (12), and cognitive functions (13) of stroke survivors. However, qualitative research is needed to explore the motivation for rehabilitation, as well as facilitators and barriers to using VRBR. Qualitative meta-synthesis combines qualitative findings from disparate investigations (14) and meta-synthesis of existing qualitative studies, improving the generalization and resonance of the results. This study aimed to systematically evaluate the experiences and needs of individuals who survived a stroke when using VRBR to exercise upper limb, lower limb, balance, walking, and cognitive functions. This meta-synthesis of qualitative studies will propose specific strategies to improve VRBR interventions, providing a reference for future research on VRBR for stroke survivors.
2. Literature review
Previous studies have shown that although stroke patients have no preference for user interfaces (15), interesting and immersive virtual reality scenarios not only appeal to young stroke patients, but also have the potential to maintain stroke patients’ motivation for rehabilitation (16). In addition, virtual reality-based rehabilitation therapy has been experienced better in patients with other diseases. For instance, breast cancer patients had high levels of acceptance and satisfaction with VRBR interventions and are willing to recommend this approach to their peers (17). Finally, three key concepts mentioned in this study are explained here to the reader. VRBR is an innovative therapeutic approach utilizing virtual reality technology, which integrates motor learning, neuroplasticity, and ecological systems theory to deliver a dynamic, patient-centered, and task-oriented rehabilitation program (e.g., for stroke survivors) (10). Virtual reality-based rehabilitation (VRBR) employs immersive, task-specific virtual environments to promote motor learning and neuroplasticity through adaptive training paradigms, real-time biofeedback, and ecologically valid simulations that enhance skill transfer to daily living while maintaining patient engagement and personalized therapeutic challenge (18). Rehabilitation motivation refers to the psychological need for individuals to engage in exercise and therapy for rehabilitation (19). Social support in rehabilitation is defined as a comprehensive system of external factors, including family members, friends, healthcare professionals, and government financial support, that help individuals cope with illness or injury and promote their psychological and physical well-being (20).
3. Methods
3.1. Reporting guidelines
This study was conformed to the ENTREQ (Enhancing Transparency in Reporting the Synthesis of Qualitative Research) statement, which can improve the transparency of qualitative research synthesis reports (21). The search results were tracked and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) standards (22).
3.2. Inclusion and exclusion criteria
The inclusion criteria for the literature were determined according to the PICoS principles (23). Inclusion criteria: (a) study population (P): individuals who survived a stroke (age ≥18 years; non-acute phase); (b) phenomenon of interest (I): attitudes, experiences, and expectations of VRBR; (c) context (Co): experiences with VRBR in the hospital, community, or home; (d) study design (S): qualitative research, including phenomenological studies, descriptive qualitative research, rooted theory, ethnography.
Exclusion criteria: (a) duplicate publications (retaining only the one with the most information); (b) literature for which full text was not available, or data were incomplete; (c) literature not in Chinese or English; and (d) literature designed using mixed methods and qualitative data that cannot be separated.
3.3. Data sources and search strategy
PubMed, Embase, CINAHL, Web of Science, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Database, China Science and Technology Journal Database, and China Biomedical Literature Database were searched using a computer, and the retrieval time limit was from inception to December 2024. The words are retrieved in the following form: stroke (stroke*, cerebrovascular*, accident*, cerebral infarction*, cerebral haemorrhage*, apoplexy*, or poststroke*), virtual reality rehabilitation (virtual reality*, exergames*, gaming*, serious games*, motion-sensing games*, or interactive games*, virtual therapy*,or virtual rehabilitation*), qualitative (qualitative*, interview*, attitude*, experience*, phenomenology*, qualitative research*, qualitative thematic analysis*, semi-structured*). Additionally, we traced the reference lists of the included studies to identify potentially eligible studies.
3.4. Literature selection
The literature was imported into EndnoteX9.1, and duplicates were removed. The literature was independently screened by two researchers trained in evidence-based nursing, who cross-checked the extracted information. In cases of disagreement, a third researcher was consulted to assist in the judgment process. The extracts included authors, year, country, methodology, data collection, data analysis, study population, phenomena of interest, and main results.
3.5. Literature quality assessment
According to the Australian Joanna Briggs Institute Center for Evidence-Based Health Care’s (2016) quality assessment criteria for qualitative research, two researchers independently evaluated the methodology of the included literature. The assessment consisted of 10 elements, each rated as “yes,” “no,” “unclear,” or “not applicable.” The quality of the included literature was categorized into three grades: A (met all evaluation indicators), B (partially met), and C (did not meet). Studies with grade C were excluded. When disagreements occurred, the two researchers made decisions based on mutual agreement. If necessary, a third researcher included the literature.
3.6. Data analysis
In this study, the results were integrated using the meta-aggregation approach (23), which requires a three-step approach: (1) extracting all findings from the included studies with an accompanying illustration and an allocated level of plausibility for each finding; (2) grouping findings into categories, with at least two findings per category; and (3) synthesizing one or more findings from at least two categories. The results were thoroughly understood and meticulously analysed multiple times by two researchers to ensure accuracy and depth of interpretation. They grouped similar results into new categories, which were summarized into meta-themes.
3.7. Meta-theme results quality evaluation
The meta-theme results were rated for quality (high, medium, low, and very low) according to the Qualitative Research Integration Evidence Assessment Tool (confidence in the qualitative evidence, ConQual) (24) constructed by the JBI Center for Evidence-Based Health Care. Ratings began at “high” and were downgraded based on reliability and trustworthiness. Dependability was determined using five questions from the JBI Quality Evaluation Criteria for Qualitative Research, which mainly evaluated the quality of the original studies included in the meta-analysis. A result of 4–5 positive answers indicated “not downgraded,” 2–3 positive answers indicated “downgraded 1,” and 0–1 positive answer indicated “downgraded 2.” Credibility was examined for consistency between the integrated results (i.e., the authors’ interpretations) and the supporting data. The findings were rated on three levels: unequivocal, equivocal, and unsupported. “No downgrade” if the integrated evidence is all from unequivocal results; ‘downgrade 2’ if the integrated evidence is all from equivocal results; and ‘downgrade 4’ if the integrated evidence is all from unsupported results”.
4. Results
4.1. Results of the literature search
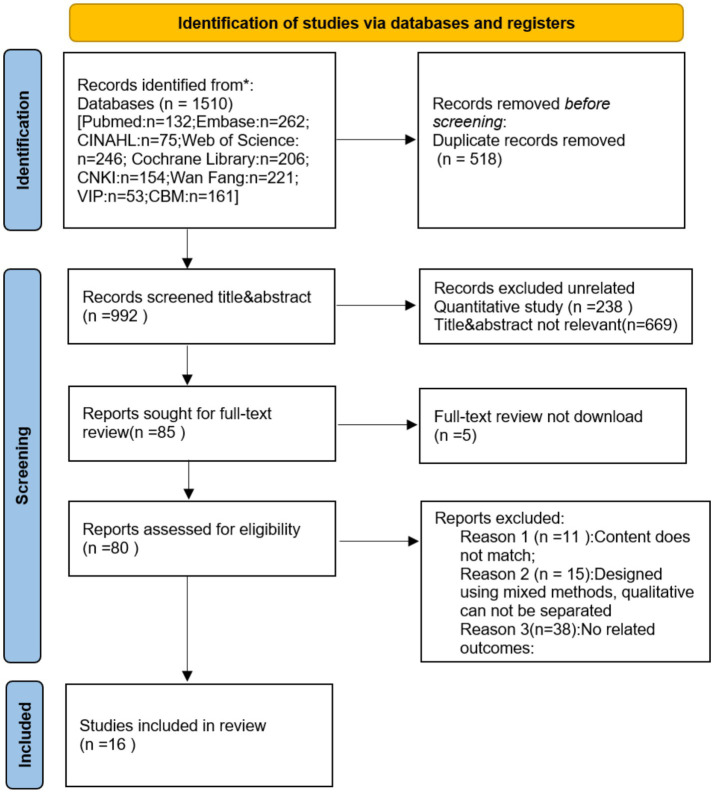
Our researchers initially examined 1,510 articles in the literature, ultimately retaining 16 literature. A detailed flowchart of the literature review is shown in Figure 1. Table 1 summarizes the features of the included studies.
Figure 1.
Flow chart of literature screening.
Table 1.
Characteristics of included literatures.
| Authors, year, country | Methodology | Data collection | Data analysis | Study population | Phenomenon of interest | Main results |
|---|---|---|---|---|---|---|
| Suai Li and Liu (2023) (28), China | Phenomenological | Semistructured interviews | Colaizzi’s analysis | Twelve ischemic stroke survivors | Exploring the experience of VRBR training for stroke survivors | 3 results: perceived benefits of using VR; perceived obstacles of using VR; needs of using VR for stroke patients |
| Tornbom and Danielsson (2018) (47), Sweden | Phenomenological | Semistructured interviews | Content analysis | Eight sub-acute stroke survivors | Exploring the treadmill walking experience in non-immersive virtual reality | 3 results: Enjoyable experience of using VR treadmill; Fatigue experience of using VR treadmill; Suggestions for improving the VR treadmill experience |
| Gustavsson et al. (2022) (48) Sweden | Descriptive research | Semistructured interviews | Thematic analysis | Six ischemic and one hemorrhagic stroke survivor | Exploring the experience of stroke survivors after VR training on commercial HTC Vive system | 3 results: Playing VR training experience; Perceived benefits and effects after VR training; Personalized VR training |
| Thomson et al. (2020) (49), Britain | Descriptive research | Semistructured interviews | Thematic analysis | Twelve stroke survivors (no stroke type mentioned) | Exploring the rehabilitation experience of stroke survivors using Nintendo Wii | 2 results: The experience of rehabilitation for stroke survivors using Wii; Companion has a positive effect on rehabilitation of stroke patients using Wii |
| Paquin et al. (2016) (25), Canada | Descriptive research | Semistructured interviews | Content analysis | Ten chronic stroke survivors (≥1 year) | Exploring the experience of stroke survivors using VR | 4 results: The experience of playing VR; The effect after using VR rehabilitation training; Professional guidance is required; The future of VR in stroke rehabilitation |
| Moan et al. (2021) (50), Norway | Descriptive research | Semistructured interviews | Thematic analysis | Mixed two types with one stroke survivor, two ischemic stroke survivors, and one hemorrhagic stroke survivor |
Exploring the treadmill walking experience in fully immersive virtual reality | 2 results: The experience of using VR treadmill; Recommendations for rehabilitation using VR treadmill |
| Lehmann et al. (2020) (29), Britain | Phenomenological | Semistructured interviews | Thematic analysis | Five stroke survivors (ischemic or hemorrhagic, including two right and three left hemiparesis) | Exploring the experience of the non-immersive virtual reality system You Grabber (YG) | 2 results: Medical and clinical elements (general experience of YG, expectations, feedback, arm function of YG, professional physiotherapist help); Social and personal elements (fatigue and positive experience of YG) |
| Amaya et al. (2018) (51), Britain | Descriptive research | Semistructured interviews | Thematic analysis | Twenty stroke aphasia survivors | Exploring the experience of stroke aphasia survivors using virtual reality EVA Park | 3 results: A fun experience after using EVA Park; Perceived benefits of using EVA Park; Perceptual barriers after using EVA Park |
| Pallesen et al, (2018) (30), Denmark | Phenomenological | Semistructured interviews | Giorgi’s analysis | Six sub-acute stroke survivors | Exploring the experience of stroke survivors with You Grabber (YG) upper limb training | 5 results: Motivational factors for using YG training; Engagement with YG training; Perceive the benefits of using YG training; Personalized YG training; Perceive technical barriers after training with YG; Satisfaction with YG training |
| Krishnan et al. (2023) (26), America | Phenomenological | Semistructured interviews | Thematic analysis | Eleven stroke survivors (>6 months) | Exploring the suggestions of using sports games for rehabilitation of stroke survivors | 2 results: Techniques used by stroke survivors; Perceived rehabilitation benefits and barriers using motor games in stroke survivors |
| Chen et al. (2020) (52), America | Phenomenological | Semistructured interviews | Thematic analysis | Thirteen chronic stroke survivors | Exploring the experience of stroke survivors on home tele-rehabilitation system | 5 results: Improved physical and mental health and social skills; Pleasant and convenient experience; Perceived obstacles factors; Peer attention increases motivation; The future and prospect of the system |
| Wingham et al. (2015) (53), Britain | Phenomenological | Semistructured interviews | Thematic analysis | Eighteen stroke survivors (no stroke type mentioned;<6 months) | Exploring the experience of arm rehabilitation with Wii | 5 results: frequency of using Wii; perceived the effectiveness of the Wii; acceptance of using Wii; Caregivers and social support; Setup and management of using Wii |
| Marika et al. (2018) (54), Canada | Phenomenological | Semistructured interviews | Thematic analysis | Seven sub-acute stroke survivors | Exploring the experience of stroke survivors using VR | 3 results: The usefulness of perceived VRBR; Satisfaction with virtual reality intervention; Aspects of virtual reality that need to be improved |
| Celinder et al. (2012) (27), Denmark | Phenomenological | Semistructured interviews | Content analysis | Nine stroke survivors (no stroke type mentioned) | Exploring the experience of stroke survivors using VR | 3 results: Perceive the relationship between VRBR and the diverse needs of daily life; Perceive the benefits of VRBR; Perceive the hindrance factors of using VR |
| Suzanne et al. (2024) (55), China | Phenomenological | Semistructured interviews | Thematic analysis | Eighteen ischaemic or haemorrhagic stroke survivors | Exploring the experience of stroke survivors using VR | 3 results: Shift in attitudes toward VR technology; Perceptions of VR effectiveness; Practical drawbacks and design recommendations |
| Lo et al. (2024) (56), Britain | Descriptive research | Semistructured interviews | Thematic analysis | Eighteen stroke survivors (≥12 weeks) | Exploring the experience of stroke survivors using VR | 5 results: Influences on the use of virtual reality; Perceptions of pretrial preparation, in-trial support and communication; Device usability and comfort; Factors motivating persistence; Perceived effectiveness of the intervention |
VRBR is virtual reality-based rehabilitation; Nintendo Wii is non-immersive virtual reality; HTC Vive system is immersive virtual reality; You Grabber (YG) is immersive virtual reality.
4.2. Quality assessment of included studies
Among the 16 included studies, 5 had a quality rating of A, and 11 had a rating of B (see Table 2). Among them, item 6 (whether the researcher own situation is described in terms of cultural background and values) of 10 included studies were evaluated as “no.” Item 7 (whether the researcher influence on the research is described, or the research influence on the researcher) of 2 included studies were evaluated as “no,” the remaining entries were evaluated as ‘yes’.
Table 2.
Quality assessment of included studies.
| Literature | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Suai Li and Liu (2023) (28) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Tornbom and Danielsson (2018) (47) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | A |
| Gustavsson et al. (2022) (48) | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | B |
| Thomson et al. (2020) (49) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Paquin et al. (2016) (25) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Moan et al. (2021) (50) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Lehmann et al. (2020) (29) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Amaya et al. (2018) (51) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | A |
| Pallesen et al, (2018) (30) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Krishnan et al. (2023) (26) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | A |
| Chen et al. (2020) (52) | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | B |
| Wingham et al. (2015) (53) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | A |
| Marika et al. (2018) (54) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Celinder et al. (2012) (27) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | A |
| Suzanne et al. (2024) (55) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
| Lo et al. (2024) (56) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | B |
1. Whether the philosophical basis is consistent with the methodology; 2. Whether the methodology is consistent with the research question or research objectives; 3. Whether the methodology is consistent with the method of data collection; 4. Whether the methodology is consistent with the representativeness of the data and the method of data analysis; 5. Whether the methodology is consistent with the interpretation of the results; 6. Whether the researcher own situation is described in terms of cultural background and values; 7. Whether the researcher influence on the research is described, or the research influence on the researcher; 8. Whether the research object is typical and adequately represents the research subject and its views; 9. Whether the conclusions are drawn in accordance with current ethical norms; 10. Is the researcher influence on the research, or the researcher influence on the research; 8. Is the subject of the research typical and adequately representative of the subject and its views; 9. Is the research consistent with current ethical norms; 10. Are the conclusions drawn from the analysis and interpretation of the data.
4.3. Meta-synthesis
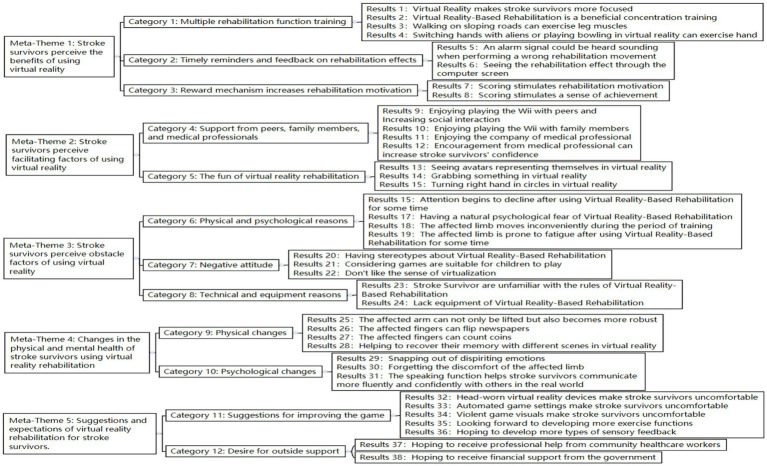
Two researchers interpreted the 16 literature, extracting 38 research findings. Similar results were summarized into 12 new categories, and a comprehensive summary of the five meta-themes was obtained. A detailed generalization and integration of the results are shown in Figure 2.
Figure 2.
Generalization and integration of research results.
4.3.1. Meta-theme 1: stroke survivors perceive the benefits of using VR
4.3.1.1. Category 1: diversification of rehabilitation function training
VRBR includes various rehabilitation function training (e.g., concentration training, walking on sloping roads to exercise leg muscles, and stroke survivors switching hands with aliens or using their hands to play bowling in a virtual environment) (10, 18, 21, 22, 25, 26). VR games require focused attention, which is “entirely different than being at the rehabilitation centre” (22). One stroke survivor mentioned, “It’s training in concentration and very beneficial “(25). Others consider walking in VR an effective muscle workout, stating, “Suddenly, there’s a small decline that can tense your muscles differently” (18). In addition to exercising the legs, VRBR involves hand exercises. Aliens in VR could “keep the hand moving” (25) for stroke survivors, and “that game seemed to work” (25). Playing bowling in VR requires “a proper push down” (27) of the hand.
4.3.1.2. Category 2: timely reminders and feedback on rehabilitation effects
In addition to the mentioned rehabilitation training, timely reminders in VR are very useful, and feedback on rehabilitation effects helps stroke survivors correct their rehabilitation movement (10, 23). One participant noted, “When you make a mistake, you can hear the alarm signal, you register it” (23). Another stroke survivor stated, “I think VR rehabilitation is excellent; it can show the rehabilitation effect through a computer screen. I just did the right actions” (10).
4.3.1.3. Category 3: reward mechanism increases rehabilitation motivation
Stroke survivors reported that their motivation and sense of achievement increased as their VR scores increased (19, 26, 28). As one person expressed, “You get motivated to go down there” because “beating your record and getting more and more points” can “motivate you for the next session” (26). Seeing points “went from 3,000 to 30,000” is “some sort of enjoyment in that “(19).
4.3.2. Meta-theme 2: stroke survivors perceive facilitating factors of using VR
4.3.2.1. Category 4: support from peers, family members, and medical professionals
Stroke survivors expressed that playing Wii with family members or peers enhances social interaction, encourages medical professionals to answer questions promptly, and increases their confidence (10, 20, 21). One stroke survivor stated, “Sometimes I play with my niece’s son; we play ten-pin bowling. My niece’s daughter will say, it is my shot; it is my shot. My family has all been in and tried it” (20). Another stroke survivor expressed, “I’ve got friends that will play with the Wii. You could spend all night playing” (20). Playing Wii can “lift the mood and give people something to talk about” (20). Additionally, stroke survivors need the support and encouragement of medical professionals. As stroke survivors mentioned, “during the process of recovery, I want doctors and nurses to be with me at all times, and when I have questions, they can answer them promptly” (10). Medical professionals “kept motivating me to keep going. The encouragement was always encouragement” (21).
4.3.2.2. Category 5: the fun of VR rehabilitation
Stroke survivors reported that seeing avatars representing themselves and performing movements such as grabbing something or turning their right hand in circles were novel and exciting (10, 21, 23). One survivor stated, “When participating in the training project ‘Digital Grid’, I could see a virtual animated character representing myself on the screen, which was very interesting” (10). Another expressed, “For me, to work my hands, my right hand, in circles and stuff, that was entertaining for me” (21). With the help of VR, stroke survivors can “grab something and see it working, although the hand is not open,” which is “interesting” (29).
4.3.3. Meta-theme 3: stroke survivors perceive hindering factors of using VR
4.3.3.1. Category 6: physical and psychological reasons
Stroke survivors reported that decreased attention, natural psychological fear, and affected limbs prevented them from using VR for rehabilitation (10, 19, 23). One stroke survivor expressed, “After a while, you notice your concentration is lessening, then you make more mistakes; this can be seen clearly” (23). The affected limb was prone to fatigue after using VRBR. One stroke survivor stated, “I get tired very quickly and feel tired in the whole body” (19). The affected limbs of stroke survivors can move inconveniently during training. Another stroke survivor said, “I find it inconvenient because, at the moment, I can only walk forward, not backward yet” (10). Moreover, the problems of stroke survivors who cannot walk or stand have been resolved, but they “still have a sense of fear during the VR rehabilitation process” (10).
4.3.3.2. Category 7: negative attitude
Some stroke survivors had stereotypes about rehabilitation games in VR, viewing them as suitable for only children, while others disliked the virtual experience (20, 27, 28). One survivor stated, “At first, I thought, oh God no, I mean it’s, how ashamed am I going to use it? I mean it is for children. That’s what I thought, oh gosh, it’s for, it’s a game, it’s something for kids” (20). Another said, “I do not think you can get that [the effect of walking up a hill] with VR or AR” (27). Stroke survivors are more willing to interact with the natural world; one mentioned, “Doing my dusting and polishing and things like that, I am, probably look around now and see a cobweb is giving me more satisfaction than sitting down playing that [Wii]” (28).
4.3.3.3. Category 8: technical and equipment reasons
Unfamiliarity with rehabilitation rules and insufficient equipment have limited the use of VR rehabilitation among stroke survivors (28, 30). In the beginning, the stroke survivor expressed, “I found it hard to figure out what it was that gave points the rules of the game? Uh! What is it that gives points, what is it I have to go after” (25). This confusion renders their use more challenging. Another important reason was that stroke survivors found that “after being discharged from the hospital, they still want to continue receiving rehabilitation training, unlike traditional rehabilitation that can be done anytime, anywhere, VR rehabilitation requires hardware facilities” (10).
4.3.4. Meta-theme 4: changes in the physical and mental health of stroke survivors using VR rehabilitation
4.3.4.1. Category 9: physical changes
Stroke survivors reported substantial physical improvements (e.g., the ability to lift the affected arm and increased strength, and the affected fingers can flip newspapers or count coins, helping recover their memory of different scenes in VR) (18, 19, 21, 29). As the stroke survivor expressed, “The more I trained, the pain went away, and now I can lie on this side—I can turn” (19). Another stroke survivor stated, My arm started getting stronger. I could reach more, you know, and I practiced it. I started reaching the refrigerator with my right hand and doorknobs (29). Moreover, affected fingers can flip newspapers or count coins. One stroke survivor said, “Well, I can turn a page in the newspaper, you know, with my left hand if I have to. I even handle small coins when I pick them for parking. I pulled them out and counted them. I separate them with my left hand” (21). Additionally, different scenes in VR may help stroke survivors to recover their memories. As one stroke survivor said, “It is easier to bring your memory back for a person who has had a stroke. You know, some people used to go to the sea, while others liked to sit in the forests. This helps them to return to their memories” (18).
4.3.5. Category 10: psychological changes
Stroke survivors reported that they experienced many psychological changes (such as overcoming dispiriting emotions and forgetting the discomfort of the affected limb), and the speaking function helped stroke survivors communicate more fluently and confidently with others in the real world (24, 25, 28). As the stroke survivor expressed, “I was feeling emotional after the…stroke, um, because I was not well enough to do anything round the house… but that [the Wii] just perked me up and made me feel useful” (28). Another stroke survivor mentioned, “I felt, especially at the start, discomfort about that (points to her arm). I do not want to say actual pain but discomfort in that bad arm. So, it has helped me forget discomfort and train” (25). Another said, “I’m more fluent and more confident in outside situations” (24). Additionally, another stroke survivor expressed, “I’m not afraid now of saying what I want to say, so the words come out. Thus, confidence is returned. Cos before I was full of it, but now, after the stroke, it all disappeared” (24).
4.3.6. Meta-theme 5: suggestions and expectations for VR rehabilitation from stroke survivors
4.3.6.1. Category 11: suggestions for improving the game
Head-worn VR devices, automated game settings, and violent game visuals made stroke survivors uncomfortable. They expressed a desire for more exercise options and varied sensory feedback (18, 19, 23, 28). Stroke survivors wanted to wear VR devices in a more comfortable position because one stroke survivor stated, “I would like to have the screen dark and just listen to the sounds, but I get a headache from this headband” (18). Stroke survivors disliked the automated game settings or violent game visuals in VR. A stroke survivor expressed, “Sometimes the Wii would decide that you were going into the sand or going out, and there’s nothing you can do about it” (28). Another stated, “Once, one had a bow, and then you were supposed to shoot those; it’s not allowed really, to shoot someone to death” (18). They proposed improvements in VRBR. As one stroke survivor mentioned, “I would have wanted to put it in more sense! You can have a fan that blows and breezes little over your face as you walk and smell if you go past a lilac hedge, that would have been lovely” (18). Another stroke survivor said, “So in a sense, I was hoping it offers new exercise options, and in my opinion, that is the case” (23).
4.3.6.2. Category 12: desire for outside support
Stroke survivors expressed a desire for guidance on the standard rehabilitation programs from community healthcare workers. As one stroke survivor mentioned, “I was a person who was intent on getting better, and I investigated the internet, did all of these searches, to try and find different ways I could get better. I did not learn about the standard rehabilitation program until approximately 1 year after my stroke. And to me, that’s lost time” (21). Additionally, some stroke survivors discontinued their internet connections because of financial constraints. As one stroke survivor mentioned, “I have a computer, but I gave up my internet for financial reasons” (26). They hope to receive financial support from the government.
4.4. ConQual quality evaluation of meta-theme results
Of the 38 extracted research findings, 31 were considered “equivocal.” Among the 14 included studies, 3 assessed the dependability of the three positive responses (Table 3).
Table 3.
ConQual quality evaluation of meta-theme results.
| Meta-theme | Dependability | Credibility | ConQual ratings | Explanation of ratings |
|---|---|---|---|---|
| Stroke survivors perceive the benefits of using virtual reality | Medium | High | Medium | Nine studies were included, of which two were downgraded by one level in reliability by including three “positive answers.” Eight research findings were “unequivocal,” and credibility was maintained at a high level. |
| Stroke survivors perceive the facilitating factors of using virtual reality | Medium | High | Medium | Four studies were included, of which one was downgraded by one level in reliability by including three “positive answers.” Seven research findings were “unequivocal,” and credibility was maintained at a high level. |
| Stroke survivors perceive the hindering factors of using virtual reality | Medium | High | Medium | Seven studies were included, of which three were downgraded by one level in reliability by including three “positive answers.” Nine research findings were “unequivocal,” and credibility was maintained at a high level. |
| Changes in the physical and mental health of stroke survivors using virtual reality rehabilitation | Medium | Medium | Low | Seven studies were included, of which two were downgraded by one level in reliability by including three “positive answers.” Seven research findings had a mix of “unequivocal” and “equivocal,” so the credibility was downgraded by one level. |
| Suggestions and expectations of virtual reality rehabilitation for stroke survivors | Medium | High | Medium | Five studies were included, of which one was downgraded by one level in reliability by including three “positive answers.” Seven research findings were “unequivocal,” and credibility was maintained at a high level. |
5. Discussion
This review provides qualitative evidence of stroke survivors’ experiences with VR rehabilitation, focusing on their needs and perspectives.
5.1. The use of VRBR is a complex perceptual change for stroke survivors
This review revealed that some stroke survivors reported improved physical, cognitive, speech, and psychological health through functional exercise with VRBR. This finding aligns with Blazquez-Gonzalez’s study, which indicated that VR could improve depression symptoms in stroke survivors (31), and Demeco’s study, which demonstrated that fully immersive VR improves upper limb flexibility, gait performance, and dynamic balance (32). However, negative attitudes and psychological fear hindered stroke survivors who used VRBR. The underlying causes of this complex perceptual variation may be related to individual differences in stroke survivors (e.g., personality, hobbies, culture, stroke type and location, and other factors). Sports games, such as bowling, are included in the VRBR content; this review found that stroke survivors who enjoyed sports quickly adapted to the intensity of rehabilitation. Stroke survivors may be more receptive to using VRBR in familiar environments, such as at home with family and friends. Some stroke survivors have stereotyped the use of the VRBR, believing that its games are intended for children.
5.2. The effect of rehabilitation motivation on the use of VRBR
Motivation is a critical component of a successful rehabilitation program (33). Several factors may influence the use of VRBR among stroke survivors. For example, reward strategies may encourage participation, as many stroke survivors reported that increasing grades motivated them. However, poor upper limb motor function may hinder stroke survivors’ motivation to participate in rehabilitation (34). Additionally, marital intimacy (35) affects the rehabilitation motivation of stroke survivors. Maintaining a strong motivation for rehabilitation improves stroke survivors’ activities of daily living (36), enhancing their quality of life and well-being. Therefore, several potentially relevant factors should be considered when engaging stroke survivors in functional exercises using a VRBR to stimulate motivation and adherence.
5.3. External support and assistance are important in the success of using VRBR
This review found that family members, peers, healthcare professionals, and government financial support are important external factors in using VRBR by stroke survivors. Family members and friends offer strong emotional support by accompanying stroke survivors during VRBR sessions. This companionship may increase interpersonal interactions and help restore social connections for stroke survivors. However, the extent and nature of this support may vary depending on cultural norms and healthcare system structures. In regions with limited healthcare resources, informal caregivers often play a central role, whereas in systems with well-established rehabilitation infrastructures, formal healthcare professionals tend to be the primary providers of support (37). Stroke survivors view expert guidance and encouragement from healthcare professionals as key forces in sustaining VRBR use. Studies have shown that music can ameliorate subjective anxiety caused by VR (38), suggesting that integrating calming elements such as music into VR sessions could improve user experience, particularly when fear or discomfort arises.
5.4. Optimize VRBR’S content settings and function modes and improve user experience
This review found that violent game visuals, uncomfortable head-worn VR devices, and complex rehabilitation rules are unsuitable for stroke survivors. This finding is similar to Sandra’s study in which a few older adults actively chose violent game visuals (39). Simplicity and ease of understanding are critical factors in older adults’ willingness to use new technology (40). Existing VR rehabilitation content settings and functions may not meet the needs of stroke survivors. Feasibility testing of sports games helps develop more features to meet user needs (41). Feasibility tests can be required the joint engagement of patients with post-stroke aphasia, healthy volunteers, healthcare professionals, and VR experts (42). Therefore, it is recommended that stroke survivors participate in feasibility tests to optimize the content settings and functional modes of VRBR.
6. Implications for research and practice
Currently, personalized exergames for in-home rehabilitation after stroke are already in the pilot phase (43). To enhance the usability and acceptance of VRBR systems, future development should incorporate participatory design methods, where stroke survivors are actively involved in co-designing interfaces, interactions, and content. This approach ensures that VRBR platforms align with users’ physical abilities, cognitive capacities, and emotional needs, thereby increasing engagement and adherence. At the same time, technology developers should optimize the VRBR support system (e.g., enriched content and improved functionality) and develop more comfortable virtual training equipment. Reward strategies have been identified as an effective way to increase rehabilitation motivation (44). In the future studies, healthcare professionals and rehabilitation therapists should conduct longitudinal trials of the effectiveness of VRBR interventions tailored based on meta-synthesis findings. Such trials could assess outcomes including motor recovery, psychological well-being, and reintegration into daily living over extended follow-up periods. Lin et al. (45) suggests that stroke survivors have numerous unmet needs when transitioning from hospitalization to the community or home. Thus, healthcare professional should actively promote the integration of VRBR into the community and at home to create a continuum of care. Healthcare professionals and rehabilitation therapists should continue exploring the relationship between reward mechanisms, motivation, and long-term adherence. Finally, stroke survivors should receive high attention from relevant government departments (46). Policymakers should prioritize improving accessibility to VR technology, especially in under-resourced settings, and strategies may include subsidizing VR equipment.
7. Limitations
Our meta-synthesis of qualitative studies has certain limitations. Nine studies had a quality rating of B, and one equivocal research finding was identified in 38 research findings. Three included studies had a dependability assessment of three positive responses, which may have created a risk of bias and weakened the overall confidence in our meta-synthesis results. It is important to acknowledge that most of the studies reviewed were conducted in high-income countries, which may limit the generalizability of the findings to other contexts. Beyond these methodological issues, VR-based rehabilitation itself presents broader challenges, such as accessibility barriers (e.g., limited availability of VR systems in clinical or home settings), challenges in aging-friendly design, high costs of VR equipment and treatment (10) and varying levels of technological literacy among stroke survivors, which may hinder widespread adoption and effectiveness.
8. Conclusion
VRBR is a complex perceptual change for stroke survivors that requires external support and assistance. Moreover, rehabilitation motivation is an important factor that influences utilization. The VRBR content settings and function modes must be updated to improve user experience.
Funding Statement
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Social Science Foundation of China Major Project: Disability Prevention Strategies and Applied Research in the Context of Population Aging (21&ZD188).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
JC: Writing – original draft, Writing – review & editing. BL: Data curation, Writing – original draft. MS: Writing – review & editing. QW: Methodology, Supervision, Writing – review & editing. LZ: Methodology, Supervision, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Collaborators, G.B.D.S . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke. (2022) 17:18–29. doi: 10.1177/17474930211065917, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Liu K, Yin M, Cai Z. Research and application advances in rehabilitation assessment of stroke. J Zhejiang Univ Sci B. (2022) 23:625–41. doi: 10.1631/jzus.B2100999, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao P, Sun H. Evaluating the rehabilitation needs of stroke patients in China: a trend analysis from 1990 to 2019. Brain Behav. (2025) 15:e70389. doi: 10.1002/brb3.70389, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang J, Ji JR, Liang C, Zhang YZ, Sun HC, Yan YH, et al. Effects of physical therapy-based rehabilitation on recovery of upper limb motor function after stroke in adults: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med. (2022) 11:521–31. doi: 10.21037/apm-21-3710, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Zumbansen A, Kneifel H, Lazzouni L, Ophey A, Black SE, Chen JL, et al. Differential effects of speech and language therapy and rTMS in chronic versus subacute post-stroke aphasia: results of the NORTHSTAR-CA trial. Neurorehabil Neural Repair. (2022) 36:306–16. doi: 10.1177/15459683211065448, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Un KK, Sue KT, Won OH. The effect of convergency: using digital contents action observation educations and task-oriented occupational therapy on activity of daily living and upper extremity function in patients with stroke. J Digit Converg. (2015) 13:445–52. doi: 10.14400/jdc.2015.13.7.445 [DOI] [Google Scholar]
- 8.LinMeng D, HonghongLiu YQ. Research progress on new technologies for stroke rehabilitation treatment. Chin J Contemp Neurol Neurosurg. (2017) 17:171–5. doi: 10.3969/j.issn.1672-6731.2017.03.003 [DOI] [Google Scholar]
- 9.Bargeri S, Scalea S, Agosta F, Banfi G, Corbetta D, Filippi M, et al. Effectiveness and safety of virtual reality rehabilitation after stroke: an overview of systematic reviews. EClinicalMedicine. (2023) 64:102220. doi: 10.1016/j.eclinm.2023.102220, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aderinto N, Olatunji G, Abdulbasit MO, Edun M, Aboderin G, Egbunu E. Exploring the efficacy of virtual reality-based rehabilitation in stroke: a narrative review of current evidence. Ann Med. (2023) 55:2285907. doi: 10.1080/07853890.2023.2285907, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J, Or CK, Chen T. Effectiveness of using virtual reality-supported exercise therapy for upper extremity motor rehabilitation in patients with stroke: systematic review and Meta-analysis of randomized controlled trials. J Med Internet Res. (2022) 24:e24111. doi: 10.2196/24111, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim M, Kaneko F. Virtual reality-based gait rehabilitation intervention for stroke individuals: a scoping review. J Exerc Rehabil. (2023) 19:95–104. doi: 10.12965/jer.2346114.057, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Liu F, Lin S, Yu L, Lin R. Effects of virtual reality rehabilitation training on cognitive function and activities of daily living of patients with poststroke cognitive impairment: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2022) 103:1422–35. doi: 10.1016/j.apmr.2022.03.012, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Finfgeld-Connett D. Generalizability and transferability of meta-synthesis research findings. J Adv Nurs. (2010) 66:246–54. doi: 10.1111/j.1365-2648.2009.05250.x, PMID: [DOI] [PubMed] [Google Scholar]
- 15.Spreij LA, Visser-Meily JMA, Sibbel J, Gosselt IK, Nijboer TCW. Feasibility and user-experience of virtual reality in neuropsychological assessment following stroke. Neuropsychol Rehabil. (2022) 32:499–519. doi: 10.1080/09602011.2020.1831935, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Isbel S, Holloway H, Greber C, Nguyen K, Frost J, Pearce C, et al. Virtual reality after stroke: identifying important characteristics when designing experiences to improve engagement in upper limb rehabilitation. Digit Health. (2024) 10:20552076241251634. doi: 10.1177/20552076241251634, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou Z, Li J, Wang H, Luan Z, du S, Wu N, et al. Experience of using a virtual reality rehabilitation management platform for breast cancer patients: a qualitative study. Support Care Cancer. (2023) 31:307. doi: 10.1007/s00520-023-07765-9, PMID: [DOI] [PubMed] [Google Scholar]
- 18.de Rooij IJM, van de Port IGL, Visser-Meily JMA, Meijer JWG. Virtual reality gait training versus non-virtual reality gait training for improving participation in subacute stroke survivors: study protocol of the ViRTAS randomized controlled trial. Trials. (2019) 20:89. doi: 10.1186/s13063-018-3165-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oh SY, Hwang SY, Chung ML, Lennie TA. A prediction model of rehabilitation motivation in middle-aged survivors of stroke in rehabilitation facilities in Korea. J Cardiovasc Nurs. (2020) 35:475–82. doi: 10.1097/JCN.0000000000000656 [DOI] [PubMed] [Google Scholar]
- 20.Chronister JA, Johnson EK, Berven NL. Measuring social support in rehabilitation. Disabil Rehabil. (2006) 28:75–84. doi: 10.1080/09638280500163695, PMID: [DOI] [PubMed] [Google Scholar]
- 21.AFK T, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. (2012) 27:181. doi: 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89. doi: 10.1016/j.jclinepi.2021.03.001, PMID: [DOI] [PubMed] [Google Scholar]
- 23.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. (2015) 13:179–87. doi: 10.1097/XEB.0000000000000062, PMID: [DOI] [PubMed] [Google Scholar]
- 24.Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol. (2014) 14:108. doi: 10.1186/1471-2288-14-108, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paquin K, Crawley J, Harris JE, Horton S. Survivors of chronic stroke – participant evaluations of commercial gaming for rehabilitation. Disabil Rehabil. (2016) 38:2144–52. doi: 10.3109/09638288.2015.1114155, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Krishnan S, Mandala MA, Wolf SL, Howard A, Kesar TM. Perceptions of stroke survivors regarding factors affecting adoption of technology and exergames for rehabilitation. PM and R. (2023) 15:1403–10. doi: 10.1002/pmrj.12963, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Celinder D, Peoples H. Stroke patients' experiences with Wii sports® during inpatient rehabilitation. Scand J Occup Ther. (2012) 19:457–63. doi: 10.3109/11038128.2012.655307, PMID: [DOI] [PubMed] [Google Scholar]
- 28.Suai Li XZ, Liu M. Virtual reality rehabilitation experience in patients with motor dysfunction after ischemic stroke. Chin Nurs Manag. (2023) 23:744–8. doi: 10.3969/j.issn.1672-1756.2023.05.021 [DOI] [Google Scholar]
- 29.Lehmann I, Baer G, Schuster-Amft C. Experience of an upper limb training program with a non-immersive virtual reality system in patients after stroke: a qualitative study. Physiotherapy. (2020) 107:317–26. doi: 10.1016/j.physio.2017.03.001, PMID: [DOI] [PubMed] [Google Scholar]
- 30.Pallesen H, Andersen MB, Hansen GM, Lundquist CB, Brunner I. Patients' and health professionals' experiences of using virtual reality Technology for Upper Limb Training after stroke: a qualitative substudy. Rehabil Res Pract. (2018) 2018:1–11. doi: 10.1155/2018/4318678, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blazquez-Gonzalez P, Mirón-González R, Lendínez-Mesa A, Moro-Tejedor MN, Cobo-Sánchez JL, Mancebo-Salas N, et al. Efficacy of the therapeutic use of video games on the depressive state of stroke patients: protocol for systematic review and meta-analysis. PLoS One. (2022) 17:e0275740. doi: 10.1371/journal.pone.0275740, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Demeco A, Zola L, Frizziero A, Martini C, Palumbo A, Foresti R, et al. Immersive virtual reality in post-stroke rehabilitation: a systematic review. Sensors (Basel). (2023) 23:1712. doi: 10.3390/s23031712, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dias P, Silva R, Amorim P, Lains J, Roque E, Pereira ISF, et al. Using virtual reality to increase motivation in Poststroke rehabilitation. IEEE Comput Graph Appl. (2019) 39:64–70. doi: 10.1109/MCG.2018.2875630, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Li W, Zhu G, Lu Y, Wu J, Fu Z, Tang J, et al. The relationship between rehabilitation motivation and upper limb motor function in stroke patients. Front Neurol. (2024) 15:1390811. doi: 10.3389/fneur.2024.1390811, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moon KJ, Chung ML, Hwang SY. The perceived marital intimacy of spouses directly influences the rehabilitation motivation of hospitalized stroke survivors. Clin Nurs Res. (2021) 30:502–10. doi: 10.1177/1054773820924573, PMID: [DOI] [PubMed] [Google Scholar]
- 36.Ishida S, Harashima H, Miyano S, Kawama K. Effect of rehabilitation motivation on improving activities of daily living in subacute stroke patients. J Stroke Cerebrovasc Dis. (2023) 32:107385. doi: 10.1016/j.jstrokecerebrovasdis.2023.107385, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Singh H, Fakembe SP, Brown RK, Cameron JI, Nelson MLA, Kokorelias KM, et al. Stroke experiences and unmet needs of individuals of African descent living in high-income economy countries: a qualitative Meta-synthesis. J Racial Ethn Health Disparities. (2024) 11:2608–26. doi: 10.1007/s40615-023-01725-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seinfeld S, Bergstrom I, Pomes A, Arroyo-Palacios J, Vico F, Slater M, et al. Influence of music on anxiety induced by fear of heights in virtual reality. Front Psychol. (2015) 6:1969. doi: 10.3389/fpsyg.2015.01969, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McKay SM, Maki BE. Attitudes of older adults toward shooter video games: an initial study to select an acceptable game for training visual processing. Geron. (2010) 9:5–17. doi: 10.4017/gt.2010.09.01.001.00, PMID: [DOI] [PubMed] [Google Scholar]
- 40.Chandrasekaran R, Katthula V, Moustakas E. Too old for technology? Use of wearable healthcare devices by older adults and their willingness to share health data with providers. Health Informatics J. (2021) 27:14604582211058073. doi: 10.1177/14604582211058073, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Villada Castillo JF, Montoya Vega MF, Muñoz Cardona JE, Lopez D, Quiñones L, Henao Gallo OA, et al. Design of Virtual Reality Exergames for upper limb stroke rehabilitation following iterative design methods: usability study. JMIR Serious Games. (2024) 12:e48900. doi: 10.2196/48900, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bu X, Ng PHF, Tong Y, Chen PQ, Fan R, Tang Q, et al. A Mobile-based virtual reality speech rehabilitation app for patients with aphasia after stroke: development and pilot usability study. JMIR Serious Games. (2022) 10:e30196. doi: 10.2196/30196, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Desai K, Prabhakaran B, Ifejika N, Annaswamy TM. Personalized 3D exergames for in-home rehabilitation after stroke: a pilot study. Disabil Rehabil Assist Technol. (2023) 18:704–13. doi: 10.1080/17483107.2021.1913518, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Zhou P, Li W, Zhao J, Chen S, Chen Y, Shen X, et al. Modulated effectiveness of rehabilitation motivation by reward strategies combined with tDCS in stroke: study protocol for a randomized controlled trial. Front Neurol. (2023) 14:1200741. doi: 10.3389/fneur.2023.1200741, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin S, Wang C, Wang Q, Xie S, Tu Q, Zhang H, et al. The experience of stroke survivors and caregivers during hospital-to-home transitional care: a qualitative longitudinal study. Int J Nurs Stud. (2022) 130:104213. doi: 10.1016/j.ijnurstu.2022.104213, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Ahmad Ainuddin H, Romli MH, Hamid TA, SF Salim M, Mackenzie L. An exploratory qualitative study with older Malaysian stroke survivors, caregivers, and healthcare practitioners about falls and rehabilitation for falls after stroke. Front Public Health. (2021) 9:611814. doi: 10.3389/fpubh.2021.611814, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tornbom K, Danielsson A. Experiences of treadmill walking with non-immersive virtual reality after stroke or acquired brain injury - A qualitative study. PLOS ONE, (2018). 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gustavsson M, Kjörk EK, Erhardsson M, Murphy MA. Virtual reality gaming in rehabilitation after stroke - user experiences and perceptions. Disabil Rehabil (2022) 44, 6759–6765. [DOI] [PubMed] [Google Scholar]
- 49.Thomson K, Pollock A, Bugge C, Brady MC. Commercial gaming devices for stroke upper limb rehabilitation: The stroke survivor experience. J Rehabil Assist Technol Eng. (2020) 7:2055668320915381. doi: 10.1177/2055668320915381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moan ME, Vonstad EK, Su X, Vereijken B, Solbjør M, Skjæret-Maroni N. Experiences of Stroke Survivors and Clinicians With a Fully Immersive Virtual Reality Treadmill Exergame for Stroke Rehabilitation: A Qualitative Pilot Study. Frontiers in Aging Neurosci. (2021). 13:735251. doi: 10.3389/fnagi.2021.735251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amaya A, Woolf C, Devane N, Galliers J, Talbot R, Wilson S, et al. Receiving aphasia intervention in a virtual environment: the participants’ perspective. Aphasiology (2018). 32:538–558. [Google Scholar]
- 52.Chen Y, Chen Y, Zheng K, Dodakian K, See J, Zhou R, et al. A qualitative study on user acceptance of a home-based stroke telerehabilitation system. TOPICS IN STROKE REHABILITATION, 2020. 27:81–92. doi: 10.1080/10749357.2019.1683792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wingham J, Adie K, Turner D, Schofield C, Pritchard C. Participant and caregiver experience of the Nintendo Wii Sports™ after stroke: qualitative study of the trial of Wii™ in stroke (TWIST). Clin Rehabil. (2015) 29:295‐305. doi: 10.1177/0269215514542638 [DOI] [PubMed] [Google Scholar]
- 54.Demers M, Chan Chun Kong D, Levin MF. Feasibility of incorporating functionally relevant virtual rehabilitation in sub-acute stroke care: perception of patients and clinicians Disabil Rehabil Assist Technol. (2019). 14:361–367. doi: 10.1080/17483107.2018.1449019 [DOI] [PubMed] [Google Scholar]
- 55.Kilbride C, Butcher T, Warland A, Ryan J, Scott DJM, Cassidy E, et al. Rehabilitation via HOMe-Based gaming exercise for the Upper limb post Stroke (RHOMBUS): a qualitative analysis of participants\u0027 experience. BMJ Open. (2024) 14:e075821. doi: 10.1136/bmjopen-2023-075821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lo SHS, Chau JPC, Choi KC, Butt L, Lau AYL, Lee VWY, et al. Stroke survivor and caregiver experiences of virtual reality gaming to promote social participation: A qualitative study. PLoS One. (2024) 19:e0315826. doi: 10.1371/journal.pone.0315826 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.