Abstract
Background and Aim
Hemodialysis patients experience fatigue due to factors such as toxic compounds in the bloodstream, fluid, and electrolyte disorders. Despite resting, they still feel tired and report poor sleep quality. This study aimed to investigate the effect of foot reflexology massage on reducing fatigue and improving sleep quality in hemodialysis patients.
Methods
This quasi-experimental study was conducted on hemodialysis patients in southeastern Iran. Eligible patients were selected through purposive sampling and allocated to either the intervention group (n = 25) or the control group (n = 25). The intervention group received foot reflexology massage three times weekly for three weeks, while the control group received routine care. Data were collected using the Pittsburgh Sleep Quality Index (PSQI) and Piper Fatigue Scale at three time points: pre-intervention, immediately post-intervention, and two weeks after intervention.
Results
The findings showed that the mean score of sleep quality in the intervention group decreased from 16.23 before the intervention to 3.31 two weeks after the intervention (p < .001). Furthermore, the mean fatigue score in the intervention group decreased from 8.63 before the intervention to 3.11 two weeks after the intervention (p < .001).
Conclusion
The results of this study showed that foot reflexology can reduce fatigue and increase sleep quality in hemodialysis patients. As a simple, feasible, and non-invasive method without complications, reflexology can be used by nurses to reduce fatigue and increase sleep quality in HD patients.
Keywords: hemodialysis, sleep quality, fatigue, foot reflexology massage
Introduction
The human renal system is responsible for maintaining fluid homeostasis, eliminating metabolic waste products, and regulating blood pressure (Al Sharji et al., 2022). When the kidneys are unable to perform these functions over the long term, it results in chronic renal failure (CRF). Approximately 200,000 people worldwide are affected by CRF annually; in Iran alone, around 90,000 people are affected by this condition and the prevalence is increasing. If left untreated, chronic kidney failure quickly progresses to end-stage renal disease (ESRD). In this condition, patients lose a significant number of nephrons, rendering the kidneys unable to excrete metabolic waste and excess fluids, necessitating the use of an artificial blood purification system known as dialysis (Hendriks et al., 2020; Pourkhajoei et al., 2025).
Dialysis is used as a maintenance therapy to preserve homeostasis and stabilize internal conditions in patients with ESRD. There are two main types: (a) Hemodialysis (HD) and (b) Peritoneal dialysis (PD). In Iran, studies indicate that around 29,200 patients are undergoing hemodialysis, and these figures are expected to increase by 2030 (Kim et al., 2022; Oshvandi et al., 2021).
Although dialysis can be lifesaving, it cannot fully replace the normal functioning of healthy kidneys and is associated with various complications, particularly for patients with ESRD. Research suggests that dependence on HD machines, frequent treatment schedules, medication regimens, dietary restrictions, and changes in social roles can increase fatigue in patients. Fatigue is also strongly related to sleep disorders, so it can be expected that HD patients suffer from sleep disorders in addition to fatigue, which adversely affects their sleep quality (Ghanbari et al., 2022; Gregg et al., 2021).
Fatigue can have long-term negative effects and may eventually become life-threatening, making it essential to identify effective treatments as soon as possible. Several studies have introduced both pharmacological and non-pharmacological therapies to manage fatigue in HD patients. Pharmacological treatments often involve medication prescriptions, while non-pharmacological treatments, which fall under complementary and alternative medicine (CAM), include programs designed to support patients in their daily lives through activities such as yoga, acupressure, hypnosis, aromatherapy, and massage. Among these, massage therapy is one of the most widely used and popular CAM methods worldwide, especially among nurses (Çeçen & Lafcı, 2021; Ghasemi et al., 2021).
Massage therapy has various types; with reflexology being the most common. Reflexology has a 4,000-year history, originating in China, and can play a significant role in alleviating complications experienced by hemodialysis patients. Reflexology specialists believe that feet serve as mirrors reflecting the entire body. Foot reflexology is essentially a human touch therapy that can be used anywhere and at any anytime, requiring no special equipment. It is non-invasive, and respects individuals’ privacy (Alinia-Najjar et al., 2020; Shahriari et al., 2021; Tedeschi, 2024). This therapeutic approach is based on the concept that specific points on the feet correspond to various organs and systems within the body. By applying pressure to these points—such as the arch of the foot—therapists aim to enhance energy circulation and improve organ functions, including kidney function. Additionally, pressure on the middle third of the foot is believed to stimulate the nervous system. This process involves opening ion channels in cell membranes and transmitting action potentials to the spinal cord, which in turn activates the parasympathetic nervous system and promotes the release of endogenous endorphins. Moreover, the energy wave created through the interaction between therapist and patient may help restore homeostasis. Therefore, reflexology could potentially influence sleep quality and reduce fatigue in hemodialysis patients, but further research is needed to confirm this relationship (Ghasemi et al., 2021; Raiesifar et al., 2021; Shahriari et al., 2021).
Numerous studies have investigated the effect of foot reflexology massage on symptoms such as fatigue and sleep quality in HD patients. Asltoghiri et al. demonstrated improvements in sleep disorders following reflexology massage (Asltoghiri & Ghodsi, 2012). Similarly, Lee et al. suggested that reflexology massage is a practical intervention for reducing fatigue and enhancing sleep quality (Lee et al., 2011). Although systematic reviews indicate that reflexology massage is safe and effective for managing insomnia, further studies are necessary to confirm this relationship (Yeung et al., 2012).
Reflexology massage, as one of the complementary and alternative medicine methods, has been widely used in recent decades. Nurses prefer this non-invasive technique, which has minimal side effects to improve the quality of nursing care (Lee et al., 2011; Yeung et al., 2012). However, decisions remain cautious due to insufficient studies (Samarehfekri et al., 2020). Therefore, the present study was conducted to examine the effect of foot reflexology massage on fatigue and sleep quality in HD patients.
Research Questions
What are the mean sleep quality scores in the intervention and control groups before, immediately, and two weeks after the intervention?
What are the mean fatigue scores in the intervention and control groups before, immediately, and two weeks after the intervention?
Methods
Study Design and Participants
This quasi-experimental study, conducted from October 2023 to March 2024, aimed to evaluate the effect of foot reflexology on sleep quality and fatigue in HD patients in southeastern Iran. Participants were selected by convenience sampling based on inclusion and exclusion criteria, and were allocated to either the control or the intervention group using purposive sampling. To control for potential bias, patients on even days of the week were assigned to the intervention group, while those on odd days were assigned to the control group. The study was double-blind with both participants and therapists unaware of group allocation to further minimize bias.
Based on a previous study (Shariati et al., 2012), the sample size was calculated to achieve 80% power at a 95% confidence level, indicating that 19 patients per group were needed (38 in total). Accounting for potential attrition, 25 patients were selected for each group, resulting in 50 patients in the final analysis.
Inclusion Criteria
Age at least 18 years (Azimpour et al., 2019).
Undergoing dialysis treatment for at least 3 months (Azimpour et al., 2019).
Receiving HD three times a week for four hours each session (Ghasemi et al., 2021).
No limb amputation or wounds at the site of the massage (Saedi et al., 2019).
No chronic and debilitating diseases such as cancer, chronic respiratory failure, heart failure, rheumatoid arthritis, or lupus erythematosus (Saedi et al., 2019).
No significant physical disability or mental disorder that impair self-care.
Exclusion Criteria
Missing more than two sessions of the interventions.
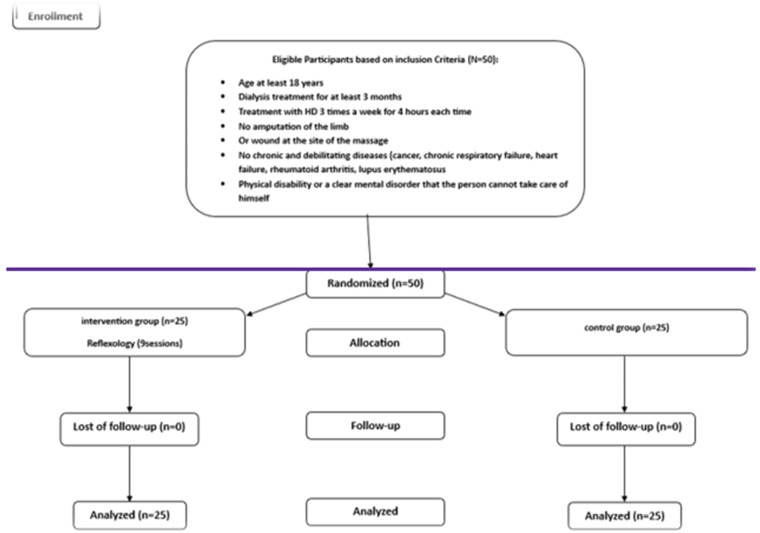
Using sleeping pills or sedatives (Ghanbari et al., 2022) (Figure 1).
Figure 1.
Recruitment and Retention of Participants in the Study.
Data Collection Tools
In this study, data were collected using a three-part questionnaire, including 1) demographic information, 2) The Pittsburgh Sleep Quality Index (PSQI), and 3) The Piper Fatigue Scale.
Demographic Information Questionnaire
This questionnaire included age, sex, marital status, level of education, duration of kidney failure (months), and duration of dialysis (months) (Ghanbari et al., 2022).
Pittsburgh Sleep Quality Index (PSQI)
This questionnaire consists of 19 questions that examine seven domains of sleep: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. Each domain is scored from 0 (no problems during sleep) to 3 (severe problem during sleep). The sum of theses component scores yields a global PSQI score ranging from 0 to 21, with higher scores indicating poorer sleep quality. The validity of the questionnaire was 89.6% (Buysse et al., 1989). Its internal consistency (Cronbach's alpha) has been confirmed in previous studies, with values of .86 (Miladinia et al., 2017) and .88 (Raiesifar et al., 2021). In the current study, the reliability (internal consistency) was confirmed with a Cronbach's alpha coefficient of .89.
Piper Fatigue Scale
The Piper Fatigue Scale is a 23-item tool used to asses fatigue across four domains: behavior/intensity, emotional, sensory, and cognitive/mood. Questions 2 to 23 of the questionnaires are scored from 1 to 10, and the total mean score of this scale ranges from 1 to 10. Scores below 4 indicate mild fatigue, 4–6 indicate moderate fatigue, and above 6 signifies severe fatigue. The validity and reliability of the scale have been confirmed in studies in different patient populations. The Cronbach's alpha coefficient of the tool was .97 in Piper et al.'s study (Piper et al., 1998). In this study, the internal consistency was confirmed with a Cronbach's alpha of .97.
Data Collection and Intervention
Patients in the intervention group received three 16-min sessions per week for three consecutive weeks —each session involving 8 min of foot massage per foot (Izadpanah et al., 2018). During the sessions, the patient was placed in a semi-sitting position with their soles parallel to the reflexologist's chest, eyes closed, and relaxed. The reflexologist, who was of the same gender as the patient, performed massage on the solar plexus area, the pineal gland area in the upper inner part of the foot and the big toe. The protocol included 2 min of general massage on each foot, 5 min of reflexology massage on each leg, with 1-min rest in between. The control group did not receive any massage during the study. Data were collected before, immediately after, and two weeks after the intervention (follow-up).
Data Analysis
Data were analyzed using SPSS 22. Independent t-test (or Mann–Whitney U test), chi-squared test, or Fisher's exact test were used to compare baseline characteristics between the groups. Repeated measures ANOVA or the Friedman test was used to determine the mean difference in fatigue, and sleep quality between the two groups.
Ethical Considerations
This study was approved by the Ethics Committee of Kerman University of Medical Sciences (IR.KMU.REC.1402.228). Researchers explained research goals and protocol to the participants before their involvement. Those willing to participate in the study provided written informed consent.
Results
The mean age of the participants in the intervention group was 37.42 ± 11.43, while in the control group, it was38.87 ± 12.25. There was no significant difference in gender, education level, age, duration of chronic renal failure, and duration of HD between the two groups, and the two groups were identical in these characteristics (Table 1).
Table 1.
Description of Participants’ Demographic Information in Intervention and Control Groups.
| Group Variable |
Intervention | Control | Fisher's exact test | p value | ||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |||
| Sex | ||||||
| Female | 9 | 36 | 7 | 28 | 1.22 | .35 |
| Male | 16 | 64 | 18 | 72 | ||
| Marital Status | ||||||
| Single | 10 | 40 | 9 | 36 | 1.25 | .67 |
| Married | 14 | 56 | 15 | 60 | ||
| Divorced | 1 | 4 | 1 | 4 | ||
| Education Level | ||||||
| Illiterate | 5 | 20 | 6 | 24 | 1.76 | .68 |
| Upper secondary | 10 | 40 | 7 | 28 | ||
| Diploma | 6 | 24 | 7 | 28 | ||
| Academic | 4 | 16 | 5 | 20 | ||
| Mean | Standard deviation | Mean | Standard deviation | Independent t-test | p value | |
| Age | 37.42 | 11.43 | 38.87 | 12.25 | −0.22 | .83 |
| Duration of kidney failure (months) | 53.4 | 41.71 | 50.6 | 35.02 | −0.63 | .73 |
| Duration of dialysis (months) | 23.55 | 14.23 | 21.16 | 17.09 | −0.63 | .29 |
The results showed that the mean fatigue score in the intervention group decreased from 8.63 before the intervention to 3.11 two weeks after the intervention, which was statistically significant. Additionally, the mean fatigue score in the control group decreased from 7.94 before the intervention to 6.96 two weeks after the intervention, which was not statistically significant. Between-group comparisons indicated that the fatigue score significantly decreased in the intervention group after the intervention compared to the control group and this decrease remained evident up to two weeks after the intervention (Table 2).
Table 2.
Comparison of the Mean Fatigue Score at Different Times in the Intervention and Control Groups.
| Group Fatigue |
Intervention | Control | Mean difference | p value | ||
|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |||
| Before the intervention | 8.63 | 1.04 | 7.94 | 1.92 | 0.69 | .25 |
| Immediately after the intervention | 5.42 | 1.24 | 7.67 | 1.34 | 2.25 | <.001 |
| Two weeks after the intervention | 3.11 | 1.11 | 6.96 | 1.98 | 3.85 | <.001 |
| p value | <.001 | .11 | ||||
The mean sleep quality score in the intervention group decreased from 16.23 before the intervention to 3.31 two weeks after the intervention, which was statistically significant. In addition, the mean fatigue score in the control group decreased from 17.44 before the intervention to 6.56 two weeks after the intervention, which was not statistically significant. Between-group comparisons revealed that the sleep quality score significantly increased in the intervention group after the intervention compared to the control group and this increase persisted up to two weeks after the intervention (Table 3).
Table 3.
Comparison of the Mean Sleep Quality Score at Different Times in the Intervention and Control Groups.
| Group Sleep quality |
Intervention | Control | Mean difference | p value | ||
|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |||
| Before the intervention | 16.23 | 1.04 | 17.44 | 1.03 | 1.21 | .31 |
| Immediately after the intervention | 8.22 | 1.64 | 16.07 | 1.64 | 7.85 | <.001 |
| Two weeks after the intervention | 3.31 | 1.03 | 16.56 | 1.34 | 13.25 | <.001 |
| p value | <.001 | .12 | ||||
Discussion
The results of this study indicated a significant reduction in the mean fatigue score of the intervention group after the intervention, with this decrease persisting up to two weeks post-intervention. In contrast, the control group exhibited minimal change in the mean fatigue score before and after the intervention. Several previous studies support these findings: Kalani et al. found that aromatherapy with geranium and reflexology foot massage significantly reduced fatigue in HD patients (Kalani et al., 2023). Cecen et al. also found that hand and foot massages could reduce fatigue levels in HD patients in Turkey (Çeçen & Lafcı, 2021). Khamid et al. reported that foot massage, performed 2–3 times a week for 45 min each session, could reduce fatigue after HD sessions (Khamid & Rakhmawati, 2022).
Furthermore, systematic reviews by Nurinto et al. and Sahan et al. confirm that foot reflexology has a positive effect on reducing fatigue in HD patients (Nurinto et al., 2024; Şahan & Güler, 2023). In addition, Habibzadeh et al. found that reflexology massage reduced fatigue and improved sleep quality in HD patients; although, this study was limited to male participants and assessed outcomes two months after the intervention ended (Habibzadeh et al., 2020). Conversely, studies by Jones et al. and Otter et al. have reported increased fatigue or no significant change, indicating that the therapeutic role of reflexology remains controversial (Jones et al., 2013; Otter et al., 2010).
The results of the study indicated a statistical difference in the mean sleep quality score of the intervention group after the intervention. Even two weeks after the intervention ended, participants maintained higher mean sleep quality score compared to the control group, which showed no statistically significant difference in the mean sleep quality score before and after the intervention. Goktuna et al. found that three 15-min sessions of foot reflexology three times a week for three weeks can positively affect sleep in HD patients (Göktuna & Arslan, 2024). Ghanbari et al. also found that reflexology and Swedish massage significantly improved sleep quality in HD patients with restless leg syndrome (Ghanbari et al., 2022). Additionally, Edly highlighted that non-pharmacological methods such as cognitive-behavioral therapy, exercise, and reflexology can positively affect and improve sleep quality in HD patients (Edley, 2020).
Oshvandi et al. reported that foot massage with lavender and sweet orange oil had a positive impact on sleep quality and reduced restless leg syndrome in HD patients, indicating that foot massage can significantly increase sleep quality in this population (Oshvandi et al., 2021). Furthermore, Ajorpaz et al. emphasized that Thai massage performed three times a week for one month in 60-min sessions significantly improved sleep quality in HD patients (Mirbagher Ajorpaz et al., 2024). Siburian et al. also showed that three 20-min massages per week for three weeks could enhance sleep quality in HD patients (Siburian & Silaban, 2023). The results of this study are consistent with previous studies, and is in contrast with the study by Doner et al., which reported that massage intervention had no effect on sleep quality of patients (Döner et al., 2025).
Although numerous studies emphasize the positive impact of foot reflexology on fatigue and sleep quality in HD patients, it is also important to consider limitations that may affect the generalizability of these outcomes. Many studies feature small sample sizes, especially those restricted to male HD patients and often only conduct post-intervention assessments without long-term follow-up.
Limitations
One of the limitations of the present study is the reliance on self-reported questionnaires. Since respondents’ mental states and personality traits can affect their responses, it may affect the generalizability of the results. The impact of self-report questionnaires on the generalizability of findings is a well-recognized challenge in research, as individuals’ feelings, beliefs, and biases can skew results, potentially limiting the applicability of the findings beyond the specific sample.
Implication for Nursing Practice
Since hemodialysis patients commonly suffer from various complications, including fatigue and poor sleep quality, and are limited in their medication use due to their medical conditions, foot reflexology massage can be an effective interventional treatment that can reduce these complications to some extent in these patients. It is a simple, low-cost, and feasible treatment that can be easily taught and implemented by nurses.
Conclusion
Despite advancements in HD technology, complications such as fatigue and sleep disturbances continue to affect HD patients. Efforts using techniques such as reflexology aim to reduce these issues. Foot reflexology not only improves sleep quality but also reduces fatigue among HD patients. Teaching HD patients how to perform reflexology massage under the guidance of trained specialists and nurses can be an effective measure for these patients. Given its simplicity, low cost, and ease of teaching, foot reflexology can be readily incorporated into various healthcare settings to enhance patient care.
Supplemental Material
Supplemental material, sj-docx-1-son-10.1177_23779608251364099 for The Effect of Foot Reflexology Massage on Fatigue and Sleep Quality in Hemodialysis Patients by Raheleh Rajabi, Fatemeh Akhlaghi, Neda Asadi, Fatemeh Zamani Babgohari and Fatemeh Arabpoor in SAGE Open Nursing
Supplemental material, sj-docx-2-son-10.1177_23779608251364099 for The Effect of Foot Reflexology Massage on Fatigue and Sleep Quality in Hemodialysis Patients by Raheleh Rajabi, Fatemeh Akhlaghi, Neda Asadi, Fatemeh Zamani Babgohari and Fatemeh Arabpoor in SAGE Open Nursing
Acknowledgments
The authors thank the Nursing Research Center of Kerman University of Medical Sciences, Zarand, Iran.
Footnotes
ORCID iD: Neda Asadi https://orcid.org/0000-0001-7573-0452
Ethics Approval and Consent to Participate: This article is the result of the research project approved by the student research committee of Kerman University of Medical Sciences under the number IR ID. KMU. REC.1402.228 which was carried out with the financial support of the research and technology vice-chancellor of this university. It aligns with the suggested guidelines outlined in the Helsinki declaration of the World Medical Association, the Council for International Organizations of Medical Sciences (CIOMS), and the Belmont report.
Competing Interests: The authors declare that they have no competing interests.
Authors’ Contributions: N. A, R.R, and F.A are the project manager who conceived and designed the project and supervised all phases of project including formative assessment, developing instrument, analysis and interpretation of data and drafting the article. F.Z and F.AR collected and analyzed the data and drafted the manuscript.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Material: The data are available upon request to the corresponding author after signing appropriate documents in line with ethical application and the decision of the Ethics Committee.
Supplemental Material: Supplemental material for this article is available online.
References
- Alinia-Najjar R., Bagheri-Nesami M., Shorofi S. A., Mousavinasab S. N., Saatchi K. (2020). The effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients hospitalized in the burn intensive care unit (ICU). Burns, 46(8), 1942–1951. 10.1016/j.burns.2020.04.035 [DOI] [PubMed] [Google Scholar]
- Al Sharji A., Alaloul F., Al Yazeedi B. (2022). Coping strategies in end-stage renal disease patients on hemodialysis in Oman: Optimistic, supportive, confrontive, and prayerful. Journal of Religion and Health, 61(3), 2072–2082. 10.1007/s10943-022-01579-5 [DOI] [PubMed] [Google Scholar]
- Asltoghiri M., Ghodsi Z. (2012). The effects of reflexology on sleep disorder in menopausal women. Procedia - Social and Behavioral Sciences, 31, 242–246. 10.1016/j.sbspro.2011.12.049 [DOI] [Google Scholar]
- Azimpour S., Hosseini H. S., Eftekhari A., Kazemi M. (2019). The effects of vibration and massage on severity of symptoms of restless leg syndrome and sleep quality in hemodialysis patients; a randomized cross-over clinical trial. Journal of Renal Injury Prevention, 8(2), 106–111. 10.15171/jrip.2019.20 [DOI] [Google Scholar]
- Buysse D. J., Reynolds C. F., 3rd, Monk T. H., Berman S. R., Kupfer D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Çeçen S., Lafcı D. (2021). The effect of hand and foot massage on fatigue in hemodialysis patients: A randomized controlled trial. Complementary Therapies in Clinical Practice, 43, 101344. 10.1016/j.ctcp.2021.101344 [DOI] [PubMed] [Google Scholar]
- Döner A., Taşci S., Bilgin A. (2025). The effect of massage, acupressure and reflexology on restless legs syndrome severity and sleep quality in patients receiving haemodialysis treatment: A systematic review and meta-analysis. Nursing Open, 12(2), e70135. 10.1002/nop2.70135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edley R. (2020). Can non-pharmacological interventions improve sleep quality for haemodialysis patients? Journal of Kidney Care, 5(1), 6–12. 10.12968/jokc.2020.5.1.6 [DOI] [Google Scholar]
- Ghanbari A., Shahrbabaki P. M., Dehghan M., Mardanparvar H., Abadi E. K. D., Emami A., Sarikhani-Khorrami E. (2022). Comparison of the effect of reflexology and Swedish massage on restless legs syndrome and sleep quality in patients undergoing hemodialysis: A randomized clinical trial. International Journal of Therapeutic Massage & Bodywork: Research, Education, & Practice, 15(2), 1–13. 10.3822/ijtmb.v15i2.705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghasemi M., Rejeh N., Bahrami T., Heravi-Karimooi M., Tadrisi S. D., Vaismoradi M. (2021). Aromatherapy massage vs. Foot reflexology on the severity of restless legs syndrome in female patients undergoing hemodialysis. Geriatrics (Basel), 6(4), 99. 10.3390/geriatrics6040099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Göktuna G., Arslan G. G. (2024). Effect of foot reflexology massage on sleep, anxiety and quality of life in hemodialysis patients: A single-blind, randomized, placebo-controlled trial. Explore (NY), 20(6), 103061. 10.1016/j.explore.2024.103061 [DOI] [PubMed] [Google Scholar]
- Gregg L. P., Bossola M., Ostrosky-Frid M., Hedayati S. S. (2021). Fatigue in CKD: Epidemiology, pathophysiology, and treatment. Clinical Journal of the American Society of Nephrology, 16(9), 1445–1455. 10.2215/cjn.19891220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habibzadeh H., Wosoi Dalavan O., Alilu L., Wardle J., Khalkhali H., Nozad A. (2020). Effects of foot massage on severity of fatigue and quality of life in hemodialysis patients: A randomized controlled trial. International Journal of Community Based Nursing and Midwifery, 8(2), 92–102. 10.30476/ijcbnm.2020.81662.0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks F. K., Smeets J. S. J., Broers N. J. H., van Kranenburg J. M. X., van der Sande F. M., Kooman J. P., van Loon L. J. C. (2020). End-stage renal disease patients lose a substantial amount of amino acids during hemodialysis. The Journal of Nutrition, 150(5), 1160–1166. 10.1093/jn/nxaa010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izadpanah A. M., Hadavi M., Bahrami H. R. (2018). The effect of foot reflexology massage on fatigue severity in hemodialysis patients. Journal of Sabzevar University of Medical Sciences, 25(4), 581–590. https://doi.org/10.1590/1518-8345.6804.4023 [Google Scholar]
- Jones J., Thomson P., Irvine K., Leslie S. J. (2013). Is there a specific hemodynamic effect in reflexology? A systematic review of randomized controlled trials. The Journal of Alternative and Complementary Medicine, 19(4), 319–328. 10.1089/acm.2011.0854 [DOI] [PubMed] [Google Scholar]
- Kalani L., Kheirandish V., Bigdeli Shamloo M. B., Zanganeh M., Valiani M., Mojab F., Moazen J., Rashidi N. (2023). Comparing the effect of geranium aromatherapy and foot reflexology on fatigue and daily activities of patients undergoing hemodialysis: A randomized controlled trial. Trends in Medical Sciences, 2(4). 10.5812/tms-136136 [DOI] [Google Scholar]
- Khamid A., Rakhmawati A. (2022). The influence of feet reflexology and back massage on hemodialysis patients’ fatigue. KnE Life Sciences, 7(2), 677–686. 10.18502/kls.v7i2.10368 [DOI] [Google Scholar]
- Kim M., Seol J., Sato T., Fukamizu Y., Sakurai T., Okura T. (2022). Effect of 12-week intake of nicotinamide mononucleotide on sleep quality, fatigue, and physical performance in older Japanese adults: A randomized, double-blind placebo-controlled study. Nutrients, 14(4), 755. 10.3390/nu14040755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Han M., Chung Y., Kim J., Choi J. (2011). Effects of foot reflexology on fatigue, sleep and pain: A systematic review and meta-analysis. Journal of Korean Academy of Nursing, 41(6), 821–833. 10.4040/jkan.2011.41.6.821 [DOI] [PubMed] [Google Scholar]
- Miladinia M., Baraz S., Shariati A., Malehi A. S. (2017). Effects of slow-stroke back massage on symptom cluster in adult patients with acute leukemia: Supportive care in cancer nursing. Cancer Nursing, 40(1), 31–38. 10.1097/ncc.0000000000000353 [DOI] [PubMed] [Google Scholar]
- Mirbagher Ajorpaz N., Mohammadi M., Sadat Z., Rahemi Z., Mousavi S. M. S. (2024). The effect of Thai massage therapy on the quality of sleep in patients with hemodialysis; A randomized controlled trial. Journal of Clinical Care and Skills, 5(3), 117–123. 10.58209/jccs.5.3.117 [DOI] [Google Scholar]
- Nurinto H., Waluyo A., Yona S. (2024). The effectiveness of massage in reducing fatigue in hemodialysis patients: A systematic review. NurseLine Journal, 9(1), 45–56. 10.19184/nlj.v9i1.46611 [DOI] [Google Scholar]
- Oshvandi K., Mirzajani Letomi F., Soltanian A. R., Shamsizadeh M. (2021). The effects of foot massage on hemodialysis patients’ sleep quality and restless leg syndrome: A comparison of lavender and sweet orange essential oil topical application. Journal of Complementary and Integrative Medicine, 18(4), 843–850. 10.1515/jcim-2020-0121 [DOI] [PubMed] [Google Scholar]
- Otter S., Church A., Murray A., Lucas J., Creasey N., Woodhouse J., Grant R., Cooper H. (2010). The effects of reflexology in reducing the symptoms of fatigue in people with rheumatoid arthritis: A preliminary study. The Journal of Alternative and Complementary Medicine, 16(12), 1251–1252. 10.1089/acm.2010.0557 [DOI] [PubMed] [Google Scholar]
- Piper B. F., Dibble S. L., Dodd M. J., Weiss M. C., Slaughter R. E., Paul S. M. (1998). The revised Piper Fatigue Scale: Psychometric evaluation in women with breast cancer. Oncology Nursing Forum, 25(4), 677–684. https://doi.org/10.1037/t18854-000 [PubMed] [Google Scholar]
- Pourkhajoei S., Goudarzi R., Amiresmaeili M., Nakhaee N., Yazdi-Feyzabadi V. (2025). Estimation of economic burden of high salt intake in cardiovascular disease attributed to hypertension in Iran. Cost Effectiveness and Resource Allocation, 23(21). 10.1186/s12962-025-00631-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raiesifar Z., Molavynejad S., Raiesifar A., Maraghi E., Vaismoradi M., Helalat A. (2021). The effect of slow-stroke back massage on fatigue and sleep quality in hemodialysis patients: A clinical trial study. Journal of Hayat, 27(1), 59–71. https://doi.org/10.18502/hayat.v27i1 [Google Scholar]
- Saedi F., Barkhordari-Sharifabad M., Javadi-Estahbanati M., Fallahzadeh H. (2019). Sexual function, social isolation, loneliness and self-esteem in patients undergoing hemodialysis. Sexuality and Disability, 37(3), 401–413. 10.1007/s11195-019-09575-6 [DOI] [Google Scholar]
- Şahan S., Güler S. (2023). The effect of foot reflexology on fatigue in hemodialysis patients: A meta-analysis study. Revista Latino-Americana de Enfermagem, 31, e4022. https://doi.org/10.1590/1518-8345.6804.4022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samarehfekri A., Dehghan M., Arab M., Ebadzadeh M. R. (2020). Effect of foot reflexology on pain, fatigue, and quality of sleep after kidney transplantation surgery: A parallel randomized controlled trial. Evidence-Based Complementary and Alternative Medicine, 2020(1), 5095071. 10.1155/2020/5095071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahriari A., Sarani H., Sheikh S., Arbabisarjou A. (2021). The effect of foot reflexology massage on pruritus in hemodialysis patients. Journal of Education and Health Promotion, 10(1), 81. 10.4103/jehp.jehp_494_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariati A., Jahani S., Hooshmand M., Khalili N. (2012). The effect of acupressure on sleep quality in hemodialysis patients. Complementary Therapies in Medicine, 20(6), 417–423. 10.1016/j.ctim.2012.08.001 [DOI] [PubMed] [Google Scholar]
- Siburian C., Silaban N. (2023). The effect of foot massage with oil aromatherapy on hemodialysis patients’ sleep quality. Jurnal Aisyah: Jurnal Ilmu Kesehatan, 8(1), 33–38. https://doi.org/10.30604/jika.v8i1.1398 [Google Scholar]
- Tedeschi R. (2024). Exploring the efficacy of plantar reflexology as a complementary approach for headache management: A comprehensive review. International Journal of Therapeutic Massage & Bodywork, 17(3), 31–40. https://doi.org/10.3822/ijtmb.v17i3.971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung W.-F., Chung K.-F., Poon M. M.-K., Ho F. Y.-Y., Zhang S.-P., Zhang Z.-J., Ziea E. T.-C., Wong V. T. (2012). Acupressure, reflexology, and auricular acupressure for insomnia: A systematic review of randomized controlled trials. Sleep Medicine, 13(8), 971–984. 10.1016/j.sleep.2012.06.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-son-10.1177_23779608251364099 for The Effect of Foot Reflexology Massage on Fatigue and Sleep Quality in Hemodialysis Patients by Raheleh Rajabi, Fatemeh Akhlaghi, Neda Asadi, Fatemeh Zamani Babgohari and Fatemeh Arabpoor in SAGE Open Nursing
Supplemental material, sj-docx-2-son-10.1177_23779608251364099 for The Effect of Foot Reflexology Massage on Fatigue and Sleep Quality in Hemodialysis Patients by Raheleh Rajabi, Fatemeh Akhlaghi, Neda Asadi, Fatemeh Zamani Babgohari and Fatemeh Arabpoor in SAGE Open Nursing