Abstract
Background
Women experienced a larger decline in well-being than men did during the COVID-19 pandemic. This loss was greater for parents with childcare responsibilities living in Europe. However, little is known regarding the monetary value of health losses among Japanese workers with children during this time. This study filled this gap by attaching monetary values to poor self-assessed health (PSAH) due to a lower household income among middle-aged Japanese men and women.
Methods
This study used data on four waves from the Japan Household Panel Survey (JHPS) COVID-19 Special Survey conducted by Keio University to examine the impact of health conditions on life satisfaction among Japanese workers. It used the dichotomous variable PSAH to measure the value lost in moving from good, very good, or excellent health to fair or poor health. To select the explanatory variables for the estimation function measuring the impact of PSAH on life satisfaction, the determinants of PSAH were investigated using the random forest model. Considering the endogeneity between PSAH and life satisfaction, we used the two-stage residual inclusion approach with generalized residuals.
Results
The results show a significant difference in the monetary value of the loss of life satisfaction due to poor health between adults with children and adults without children. The results support the hypothesis that adults with children experience greater health losses than adults without children do. The health losses of adults with children were approximately 3.49 million Japanese yen (JPY) (7.3 times the average monthly household income), that is, 1.04 million JPY more than that of adults without children. The direct impact of PSAH and severe mental distress on life satisfaction was greater for adults with children than for adults without children.
Discussion
Adults with children were more likely to experience mental ill-health in the two lowest income classes; thus, the magnitude of the monetary value of the loss of well-being due to poor health during the pandemic increased.
Conclusions
Higher levels of mental health distress are associated with poorer health; therefore, attention must be paid to changes in income, sleep duration, and job insecurity among adults with children.
Keywords: Fixed-effects logit model, Health loss, Japan, Monetary valuation, Random forest, Two-stage residual inclusion
Introduction
Were middle-aged adults with children, who faced health risks during the COVID-19 pandemic, healthier and happier than those without children? The COVID-19 pandemic had uneven impacts according to gender and socioeconomic groups across countries. Women experienced a larger decline in well-being than did men during the pandemic [1–5]. In the UK [5] and Germany [6], both economic and health (psychological) crises decreased well-being, with the decline being greater for adults with childcare responsibilities than for non-parents. Furthermore, the decline in parents’ well-being in Germany was comparable to the impact on all individuals in the US and the UK [6].
In Japan, nationwide school closures during the early stage of the COVID-19 pandemic from March to May 2020 disadvantaged working adults with children, especially mothers. Female employees with minor children in the private sector had a higher probability of choosing to take temporary leave than male employees with minor children [7]. In addition, increased time spent on housework and childcare duties at home can affect workers’ quality of life [8]. Women over 30 years of age living with their families had more severe mental conditions than those who lived alone [9].
Studies have shown that decreased well-being is associated with poor health status caused by conflicts between family and work roles (work-family conflicts: WFC). By comparing data from three countries (the UK, Finland, and Japan), Chandola et al. [10] show that the poor mental health of working Japanese women was attributed, in part, to higher levels of WFC. Considering the disparity in time spent on housework and childcare among married couples in Japan, Tachibanaki and Takamatsu [11] show that a higher proportion of women’s income to household income was associated with a lower life satisfaction (LS) among married women. Most working Japanese women with multiple roles as employees and wives also shoulder the primary responsibility for household duties and, consequently, face high levels of WFC [12].
The COVID-19 pandemic aggravated career and family issues, and prioritized questions surrounding WFC [13]. Working mothers’ WFC, which causes ill health, remained high during this period in Argentina, Canada, and South Korea [14–16]. According to the 2021 Comprehensive Survey of Living Conditions in Japan, the proportion of working mothers with children younger than 18 years was a record high at 75.9%. The pandemic further exacerbated career and family issues; since working mothers spend significantly more time on housework and childcare duties than men, higher levels of psychological distress were observed in women in Japan. However, the effect of poor health on the LS of middle-aged adults with children during the COVID-19 pandemic remains unclear.
Satisfaction is less subject to short-term fluctuations and more cognitively oriented than well-being [17–19]; therefore, previous studies have used the Subjective Well-Being (SWB) valuation approach. This uses the implicit tradeoff between income and health status to estimate an individual’s willingness to pay for different health statuses, which estimates the income equivalent of changes in health status (from good to bad). The findings show that the main determinants of LS are age, gender [20, 21], chronic illness [22], chronic pain [23], 13 health conditions [24], health satisfaction [22, 25], household income [12, 20, 21, 26, 27], household work at high frequency [12], employment status, and social relationships [21].
Brown [20] and Kumagai [12] used equivalent household income to estimate average long-term health losses and applied it to attach a monetary value to the losses in normal times. Brown [20] reports long-term health losses of USD $41,654, which was 1.8 times the median annual equivalent household income (2010 baseline). Kumagai [12] assesses the health losses for women with multiple roles, such as employment and high-frequency domestic work, to be 1.47 times the real equivalent household income (USD $32,589.88, $1 USD = 105 Japanese yen (JPY), 2010 base), suggesting that to maintain the health of working women and avoid a decline in LS, it is necessary to eliminate high levels of WFC. These results indicate that it is crucial for husbands in Japan to share household work.
When exploring the effect of poor health on the LS of middle-aged adults with children during the COVID-19 pandemic, preventing mental health deterioration is an important factor. The objectives of the current study are twofold. One is to address the endogeneity among household income, health, and LS to evaluate the health losses of middle-aged people. The other is to discuss measures to prevent mental health deterioration in relation to health losses.
Therefore, in this study we used four-wave data from the JHPS COVID-19 Special Survey conducted by Keio University to examine the impact of declining household income on LS among Japanese workers aged 30–60 years through the health status of adults with and without children. We used data on poor self-assessed health (SAH) and LS to estimate the monetary values for workers’ health losses. Poor SAH (PSAH) is an important health indicator, and previous studies have examined the association between subjective health and socioeconomic status (SES), such as household income. A substantial proportion of disparities in health between SES levels can be attributed to differences in health behaviors, such as frequent drinking [28–36]. When measuring health losses, addressing potential omitted variable bias is a statistical challenge, because the positive relationship between SWB and health holds when using LS as the dependent variable in regressions [37–39].
Materials and methods
Study sample
This study applied the well-being valuation approach to attach monetary value to PSAH because of a lower standard of living during the COVID-19 pandemic. We used the dichotomous variable PSAH to measure the value lost in moving from good, very good, or excellent health to fair or poor health. Data were drawn from the JHPS COVID-19 Special Survey (Waves 1–4), conducted biannually by Keio University in Japan. The first survey was conducted from the end of May 2020 to the end of June 2020. The number of responses in Wave 1 was 3891, collected from respondents of the JHPS/KHPS 2020 conducted by Keio University in February 2020. The number of respondents in Waves 2–4 was 3244, 3681, and 3314, respectively.
The JHPS/KHPS is a unification of the KHPS and JHPS, which were originally separate but have many items in common, including those on the household structure, individual attributes, academic background, employment status, and economic conditions. The KHPS was first conducted in 2004 with approximately 7000 individuals from 4000 households, and new samples were added in 2007 and 2012. The JHPS was first conducted in 2009 with 4000 individuals, and a new sample was collected in 2019. Respondents were selected through a stratified two-stage random sampling using 24 regional and city classifications in Japan, with the number of survey subjects in each classification set according to their population size in the first stage of sampling. In the second stage, the participants were selected from basic resident registers based on designated numbers and sampling intervals.
Variables related to SWB
LS was used as a proxy for SWB. It was assessed using the question, “How satisfied are you with your life?” The responses ranged from 10 (completely satisfied) to 0 (completely dissatisfied) on an 11-point scale. In addition to the original variable ranging from 0 to 10, we used the quintile values of the original survey and created a five-point scale variable.
The PSAH was rated on a five-point scale with a question on current SAH, with values of 5, 4, 3, 2, and 1 assigned to “excellent,” “very good,” “good,” “fair,” or “poor,” respectively. We created a dichotomous variable of PSAH with a value of 1 if the SAH was fair or poor, and 0 otherwise.
To measure the extent of WFC, we created an inverse variable representing the allocation of time between working hours and unpaid work hours at home [= 1/ (unpaid work hours / (working hours + unpaid work hours))]. Non-responses regarding working hours or unpaid work hours at home were excluded when measuring the extent of WFC.
The K6 is a six-item screening scale developed by Kessler et al. [40] to assess psychological distress. In this study, moderate or severe mental distress was identified using the K6 score. Respondents rated how frequently they had experienced the following six symptoms over the previous seven days: (a) feeling nervous, (b) feeling hopeless, (c) feeling restless or fidgety, (d) feeling so depressed that nothing could cheer you up, (e) feeling that everything was an effort, and (f) feeling worthless. Each item was rated using a five-point scale: 0 (“none of the time”), 1 (“a little of the time”), 2 (“some of the time”), 3 (“most of the time”), or 4 (“all the time”). Responses to the six items were summed to yield a K6 score between 0 and 24, with higher scores indicating a greater tendency toward mental illness. Prochaska et al. [41] used the receiver operating characteristic curve and identify a K6 score ≥ 5 as the optimal cut-off point indicative of moderate mental distress. A K6 score ≥ 13 indicated severe mental distress.
We focused on the change in job insecurity; secure to insecure. Following Wilson et al. [42], we used a single item to assess respondents’ job insecurity due to COVID-19. To create a single measure of job insecurity, we used a single question extracted from “how worried are you about the effect of a new coronavirus infection on losing your job or a family member’s job?” The binary variable of job insecurity took the value of 1 if the respondent selected ‘very likely’ and 0 otherwise. The other responses such as ‘not at all likely’ and ‘not too likely’ were classified under job security.
The JHPS does not provide the number of chronic diseases that affect individuals’ LS. However, the higher the number of chronic diseases, the lower the health satisfaction [43]. Therefore, we used a dummy variable for low health satisfaction as the proxy variable for the high number of chronic diseases. A dummy variable for low health satisfaction that took the value 1 if health satisfaction was less than 3, and 0 otherwise. Almost 6.5% of the sample was classified into low health satisfaction class. Nevertheless, Dolan et al. [44] argue that high satisfaction with health leads to a significant increase in the likelihood of preferring to live for a longer time in incomplete health. Considering this aspect, health satisfaction of those who have a chronic disease may be high.
Empirical strategy
First, we used the machine learning method, random forest (RF) model, to explore the determinants of PSAH during the COVID-19 pandemic. Second, we used the instrumental variable (IV) method to correct for a probable bias when measuring the relationship between PSAH and real household income. Third, we attached monetary value to health losses during the COVID-19 pandemic considering the following two health risks that working people faced during the pandemic: (1) the risk of serious illness caused by infection and risk to life resulting from a deteriorating health status and (2) a lower standard of living caused by a loss of income due to reduced working hours or a job loss.
RF model
The RF model has the advantage of dealing with missing values because partitioning can occur at any node, even if some independent variables are missing. As no functional form is assumed, few constraints are imposed on the choice of explanatory variables [45]. RF models can be used to predict binary variables and produce predictions without a significant bias [46]. They easily adapt to nonlinearities found in the data and do not estimate the coefficients of the explanatory variables in the same way as econometric models. Therefore, they tend to predict better than linear regression models do [47]. Researchers can use several explanatory variables to eliminate overtraining effects.
We split a nationally representative sample of middle-aged adults in Japan into two subsets: 50% of the data were used for training and 50% for validation. The sample of the regression tree was split when the RF model randomly selects certain explanatory variables from among all explanatory variables; RF uses entropy for split selection in classification cases. At each internal node of the decision tree, entropy (E) is given by Eq. (1):
| 1 |
Here, c is the number of unique classes, and pi is the prior probability for each class [47]. The RF estimate was computed with a minimum leaf size of 1 and 800, averaged over the results of 100 trees with no maximum depth (these are the defaults for RF). The model has 50 features.
Each tree was constructed using bootstrap sampling. Each bootstrap sample randomly removes approximately one-third of observations, which are referred to as out-of-bag (OOB) samples. For classification problems, the OOB error used for validation represents the classification error; the goal of RF model analysis was to explore the extent to which explanatory variables affect the dependent variable, and the effects were assessed using variable importance. It is difficult to rank the importance of factors in data analysis.
Supervised learning involves a multi-factor problem. Ranking factor importance involves assessing the impact of each factor on the response variable and creating quantitative measures to compare the factors [48, 49].
In general, variable importance was used to measure the magnitude of the prediction error when explanatory variables are randomly selected. The larger the prediction error, the greater the variable importance that can be evaluated. Variable importance is calculated by adding the improvement in the objective function given by the split criterion across all internal nodes of a tree and all trees in a forest. The variable importance scores are normalized divided by the maximum score [47].
The SWB valuation approach
The objective of the econometric analysis was to investigate how an individual’s LS was affected by poor health status. The key issue in this analysis was that the primary explanatory variable, PSAH, was not exogenous.
First, we used Eq. (2) to measure the relationship between PSAH and household income, which was converted into real income in 2020 prices by dividing it by the annual consumer price index (2020 = 100). We adopted the IV probit method to correct for probable bias in the estimated parameters. Second, considering the endogeneity between PSAH and LS, we used the two-stage residual inclusion (2SRI) approach [50] with generalized residuals. Terza et al. [50] added the generalized residual of the reduced-form equation to solve the endogeneity problem in discrete models.
The transformation into the standard natural logarithm accounts for the diminishing marginal effect of income on health. Additionally, LS may significantly correlate with certain omitted variables in the PSAH. This is because poor health is a predictor of life dissatisfaction, but reverse causality has not been established [51]. To correct for small amounts of endogeneity, we followed the 2SRI approach and added the generalized residuals of the reduced-form equation. To measure the value lost in moving from good, very good, or excellent health to fair or poor health, we used the dichotomous variable PSAH.
Equation (2) is as follows:
| 2 |
Here, if G is male, θ captures the direct effect of gender on PSAH; X is the vector of control variables such as age, severe or moderate mental distress, low health satisfaction, severity of COVID-19 symptoms (SCS), and time trend; Y denotes the real monthly household income in the past month (base year = 2020); Z represents IVs, and e is the error term. Dummy variables for single parent or spouseless, spouse’s non-work, and respondent’s non-work were used as IVs. Subscripts i and t indicate individuals and periods, respectively.
Under the assumption of ‘no defiers,’ IV estimation yields a parameter known as the Local Average Treatment Effect (LATE), which represents the average treatment effect for the specific subpopulation of ‘compliers’ [52]. Compliers are those whose treatment status is directly influenced by changes in the IVs. The ‘no defiers’ assumption means that individuals will not receive treatment if they are not encouraged by the IVs.
The satisfaction model can estimate the compensating income variation for the loss of well-being due to ill-health among middle-aged adults. The compensating income variation represents the monetary compensation required for unhealthy individuals to obtain the same level of life satisfaction as healthy individuals. Because the two health losses was mentioned in section “Materials and methods”, we used Eq. (3) to evaluate health losses in monetary terms, separately for adults with children and those without children. The hypothesis to be tested is whether adults with children incurred greater health losses than adults without children did: (exp [mean of real household income in the past month]−1) × (exp[−γ1/γ3]−1). The 2SRI approach with generalized residuals is considered to have the least bias when estimating the impact of changes in the PSAH [53].
Equation (3) is as follows:
| 3 |
where, if L is a work-centered lifestyle, κ captures the direct effect of lifestyle on LS; W is the vector of control variables such as age, severe or moderate mental distress, debt, and income insecurity, and ε is the error term.
This study tested the primary hypothesis on whether monetary compensation for the loss of well-being due to ill health among adults with children during the sample period is greater than that of adults without children. We also tested whether increased teleworking affects monetary compensation for the loss of well-being due to ill health among the same group (i.e., adults with children and adults without children).
Results
Descriptive analysis
Absence from work can have a direct impact on LS, as well as through PSAH; thus, those who took leave due to the spread of COVID-19 infection were excluded from the sample. The dropped sample percentage was 8.58% (268/3123) for adults with children and 5.37% (202/3760) for adults without children.
Table 1 summarizes the characteristics of the study sample aged between 30 and 60 years. Non-responses to SAH were excluded. We compare sample characteristics by dividing the sample into those who were able to work as usual during the sample period and those who increased telework.
Table 1.
Characteristics of the study sample
| Variables / samples | Adults with children | Adults without children | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (I) | (II) Those who increased telework (Telecommuting) | (III) | (IV) Those who increased telework (Telecommuting) | |||||||||
| N | Mean | SD | N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| Dependent variables | ||||||||||||
| Life satisfaction (LS) | 2520 | 6.008 | 2.167 | 329 | 6.240 | 2.222 | 3308 | 5.552 | 2.198 | 219 | 6.123 | 1.822 |
| Poor self-assessed health (PSAH) | 2525 | 0.062 | 0.242 | 330 | 0.058 | 0.233 | 3339 | 0.090 | 0.286 | 219 | 0.064 | 0.245 |
| Independent variables | ||||||||||||
| Age | 2525 | 43.295 | 6.970 | 330 | 42.479 | 6.520 | 3339 | 48.319 | 8.423 | 219 | 51.306 | 6.482 |
| Gender (male = 1) | 2525 | 0.467 | 0.499 | 330 | 0.209 | 0.407 | 3339 | 0.479 | 0.500 | 219 | 0.169 | 0.376 |
|
Dummy variable for severe COVID-19 symptom |
2525 | 0.028 | 0.165 | 330 | 0.018 | 0.134 | 3339 | 0.025 | 0.156 | 219 | 0.014 | 0.117 |
|
Dummy variable for low health satisfaction |
2525 | 0.054 | 0.226 | 330 | 0.061 | 0.239 | 3339 | 0.077 | 0.267 | 219 | 0.032 | 0.176 |
|
Real monthly household income during the past month (base year = 2020) |
2411 | 48.702 | 87.200 | 313 | 39.415 | 40.246 | 3087 | 46.705 | 98.439 | 197 | 39.719 | 24.148 |
|
Sleep duration on weekdays (average) |
2512 | 6.448 | 1.028 | 329 | 6.670 | 1.093 | 3317 | 6.314 | 1.041 | 218 | 6.278 | 0.922 |
|
Sleep duration on holidays (average) |
2467 | 7.182 | 1.129 | 325 | 7.395 | 1.081 | 3248 | 7.140 | 1.231 | 216 | 7.051 | 1.126 |
| Hours worked | 2070 | 33.249 | 17.575 | 200 | 29.225 | 16.819 | 2739 | 34.259 | 17.034 | 148 | 25.419 | 15.617 |
| Severe mental distress | 2525 | 0.087 | 0.282 | 330 | 0.088 | 0.284 | 3339 | 0.109 | 0.312 | 219 | 0.096 | 0.295 |
| Moderate mental distress | 2525 | 0.390 | 0.488 | 330 | 0.464 | 0.499 | 3339 | 0.391 | 0.488 | 219 | 0.447 | 0.498 |
|
Dummy variable for income insecurity |
2525 | 0.173 | 0.378 | 330 | 0.109 | 0.312 | 3339 | 0.174 | 0.379 | 219 | 0.146 | 0.354 |
|
Dummy variable for job insecurity |
2525 | 0.246 | 0.431 | 330 | 0.188 | 0.391 | 3339 | 0.257 | 0.437 | 219 | 0.224 | 0.418 |
| Dummy variable for income loss | 2525 | 0.138 | 0.345 | 330 | 0.139 | 0.347 | 3339 | 0.171 | 0.377 | 219 | 0.096 | 0.295 |
| Dummy variable for debt | 2525 | 0.129 | 0.335 | 330 | 0.115 | 0.320 | 3339 | 0.140 | 0.347 | 219 | 0.064 | 0.245 |
|
Dummy variable for dismissal or bankruptcy |
2525 | 0.032 | 0.175 | 330 | 0.024 | 0.154 | 3339 | 0.035 | 0.183 | 219 | 0.023 | 0.150 |
|
Dummy variable for work- centered lifestyle |
2525 | 0.713 | 0.453 | 330 | 0.409 | 0.492 | 3339 | 0.757 | 0.429 | 219 | 0.438 | 0.497 |
|
Dummy variable for work life between housework |
2525 | 0.141 | 0.348 | 330 | 0.203 | 0.403 | 3339 | 0.095 | 0.293 | 219 | 0.265 | 0.442 |
|
Dummy variable for respondent’s non-work |
2525 | 0.104 | 0.306 | 330 | 0.321 | 0.468 | 3339 | 0.098 | 0.298 | 219 | 0.251 | 0.435 |
|
Dummy variable for single parent or spouseless |
2525 | 0.063 | 0.242 | 330 | 0 | 0 | 3339 | 0.399 | 0.490 | 219 | 0 | 0 |
|
Dummy variable for spouse’s non-work |
2525 | 0.131 | 0.338 | 330 | 0 | 0 | 3339 | 0.066 | 0.248 | 219 | 0 | 0 |
|
Proxy variable of work- to-family conflict (WFC) |
1742 | 2.111 | 2.543 | 192 | 2.570 | 2.849 | 2129 | 1.805 | 1.814 | 136 | 2.833 | 3.166 |
Sources JHPS COVID-19 Special Survey, Waves 1–4
Non-responses to SAH and individuals on leave of absence from work are excluded
The number of PSAH respondents was 2855 for adults with children and 3558 for adults without children. The percentages of those who increased telework were 11.56% (= 330/2855) and 6.16% (= 219/3558) for adults with children and adults without children, respectively (Table 1). Proportions of women who increased telework for adults with children and adults without children were 79.1% and 83.1%, respectively.
Those who increased their telework were less likely than other middle-aged adults to have a work-centered lifestyle, at 40.9% and 43.8%, respectively, with relatively higher WFC averages of 2.570 and 2.833. The magnitude of WFC is inversely related to work-centered lifestyles, with fewer average weekly hours worked (29.22, 25.41) for those who increased teleworking.
Women generally experience greater pressure from high WFC, and differences in life dissatisfaction were observed between low and high levels of WFC. However, the association between a high WFC and life dissatisfaction tends to be overstated [54]. Therefore, researchers should control for time-invariant individual attributes in the analysis. Considering this, we present an overview of the descriptive statistics.
Adults without children who were able to work as usual during the sample period had the highest prevalence of severe mental health (0.109), low health satisfaction (0.077), the highest rate of job insecurity (0.257), and the lowest mean LS (5.552). By contrast, adults with children who increased their telework had the largest mean LS (6.240) and the lowest rate of job insecurity (0.188).
The distribution of responses to LS differed between middle-aged adults with children and those without children. As Table 1 shows, the mean LS was 6.240 for adults with children who increased teleworking and 6.008 for the other adults with children who were able to work as usual during the sample period. These values were higher than those for middle-aged people without children (teleworking = 6.123, work as usual = 5.552). Variations in LS correlated with PSAH prevalence. The prevalence of PSAH among middle-aged workers with children who increased teleworking was 0.058 and 0.062 for the other adults with children, which was lower than the scores among workers without children (teleworking = 0.090, work as usual = 0.064). The prevalence of PSAH among adults with children who increased their telework (0.058) was the lowest among middle-aged individuals. Interestingly, differences in LS and PSAH between middle-aged adults with children and those without children were not minor. However, causality tends to both directions: a high level of well-being certainly seems relevant for subsequent good health, with significant positive effects on health [55].
Responses on the intrahousehold time allocation decisions of those with children may have overreported the hours of household work [56]. Regardless, the aforementioned results allow us to consider the following: middle-aged women adjusted their working hours to allow time for childcare and household chores, whereas men tended not to increase telework and concentrated on market labor.
Table 2 shows the differences in the number and percentage of middle-aged adults with PSAH who had severe COVID-19 symptoms at the time of the survey; among middle-aged adults with children who were severely ill with COVID-19, mothers were more likely to have PSAH, but fathers were not. Middle-aged men without children who were severely ill with COVID-19 tended to rate their health as poor, but this tendency did not apply to women without children. The JHPS COVID-19 Special Survey does not provide respondents’ medical history; therefore, it is difficult to explore the causal relationship from SCS to PSAH. There is no information on how many months have passed since the patients experienced SCS. However, the results in Table 2 suggest that middle-aged mothers and childless men were more likely to develop PSAH because of the SCS.
Table 2.
Prevalence of PSAH among middle-aged adults with severe COVID-19 symptoms
| Variables | Adults with children | Adults without children | ||||||
|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||||
| N | % | N | % | N | % | N | % | |
| Had or have SCS | 37 | 40 | 33 | 53 | ||||
| Perceived PSAH among SCS | 6 | 16.2 | 3 | 7.5 | 3 | 9.1 | 9 | 17.0 |
In the first survey, women’s prevalence of moderate mental distress was very high (0.456 = 0.281 + 0.175, Table 6). They may have experienced substantial WFC during the early stages of the pandemic. A systematic review of 43 studies suggested that symptoms of depression and anxiety worsened early in the pandemic, but responses to psychological stress after the first two months of the pandemic varied by population [57]. Thus, severe mental distress did not persist during the sample period; however, it is unclear what led to this population’s mental health recovery (Table 6).
Table 6.
Trends in moderate or serious mental ill-health
| K6/Wave | 1 | 2 | 3 | 4 | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| 5–8 | 446 | 0.268 | 343 | 0.239 | 419 | 0.238 | 345 | 0.222 | 1553 |
| (Women) | 258 | 0.281 | 192 | 0.242 | 226 | 0.235 | 196 | 0.229 | 872 |
| 9–12 | 260 | 0.156 | 196 | 0.137 | 286 | 0.163 | 246 | 0.158 | 988 |
| (Women) | 161 | 0.175 | 115 | 0.145 | 176 | 0.183 | 155 | 0.181 | 607 |
| 13–24 | 180 | 0.108 | 140 | 0.098 | 170 | 0.097 | 145 | 0.093 | 635 |
| (Women) | 124 | 0.135 | 87 | 0.110 | 105 | 0.109 | 83 | 0.097 | 399 |
| N | 1667 | 1434 | 1757 | 1555 | 6413 | ||||
| (Women) | 918 | 794 | 960 | 856 | 3528 | ||||
Non-responses to SAH and individuals on leave of absence from work are excluded.
Estimation results
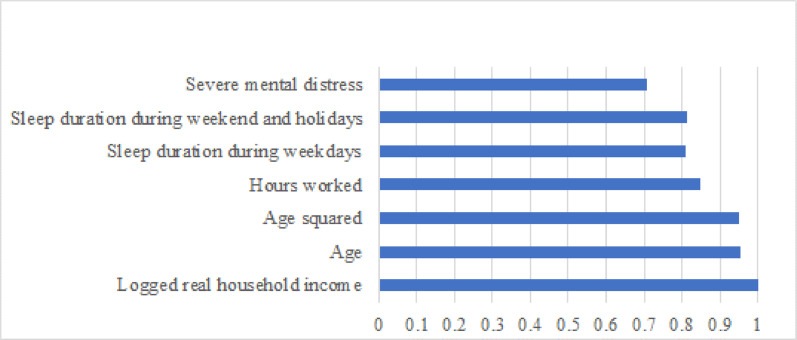
To select the explanatory variables for the estimation function measuring the impact of PSAH on LS, the determinants of PSAH were investigated using the RF model. The variables on the vertical axis in Fig. 1 rank the characteristics by their importance relative to the most important variable (at the bottom of the axis). For PSAH classification, the OOB error used for validation represents the classification error. The prediction accuracy of PSAH was good because the OOB error was 0.072. The eight variables of relative importance included logged real household income, low health satisfaction (the proxy variable of the high number of chronic diseases), age, age squared, hours worked, sleep duration on weekend and holidays, sleep duration on weekdays, and severe mental distress. A recent study by Foremny et al. [58] using RF model finds that low-income individuals have a higher probability of experiencing insomnia. Sleep duration is an important variable in perceiving poor health.
Fig. 1.
Determinants of PSAH
We can estimate two direct effects of the COVID-19 pandemic shock, severe COVID-19 symptoms and income loss, and an indirect effect, that of PSAH, on LS. Some middle-aged adults had PSAH due to severe COVID-19 symptoms. Our empirical strategy was a two-step approach. First, when estimating the PSAH function, we used three dummy variables representing a single parent or spouseless parent, spouse’s non-work, respondent’s non-work as IVs, which are related to real household income but not PSAH. Second, considering the endogeneity between the PSAH and LS, we used a 2SRI approach with generalized residuals.
Table 3 shows that all IVs had negative effects on real household income in the past month at the 1% level, and a dummy variable for having severe COVID-19 symptoms was significant at the 5% or 10% levels. All results of the weak instrument robust test (Anderson–Rubin test) for IV probit models indicated that the null hypothesis of a zero coefficient of correlation between the error terms of PSAH and real household income was not rejected. All the estimated models indicated a zero coefficient of correlation between the error terms (see Athrho in Table 3). The IV estimates are not substantially larger than the OLS estimates (Table 7), and the exclusion restrictions are plausibly satisfied in the LATE framework.
Table 3.
Results of IV probit model: determinants of health and household income
| Samples | Adults with children | Adults without children | ||
|---|---|---|---|---|
| Dependent variables | Poor self-assessed health (PSAH) | Logged real household income | Poor self-assessed health (PSAH) | Logged real household income |
| Variables | ||||
| Logged real household income | −0.297 | −0.257 | ||
| (0.301) | (0.255) | |||
| Gender (male = 1) | 0.0153 | 0.0399* | −0.00134 | 0.0613*** |
| (0.0919) | (0.0236) | (0.0755) | (0.0230) | |
| Age | 0.0102 | 0.00394** | 0.0142*** | −0.00235 |
| (0.00648) | (0.00153) | (0.00474) | (0.00146) | |
| Moderate or severe mental distress | 0.771*** | 0.00772 | 0.723*** | −0.100*** |
| (0.112) | (0.0234) | (0.0949) | (0.0254) | |
| Moderate mental distress at an early stage of the COVID-19 pandemic | −0.124 | −0.247*** | −0.639*** | 0.0468 |
| (0.177) | (0.0410) | (0.152) | (0.0460) | |
| Low health satisfaction | 1.650*** | −0.123*** | 1.715*** | −0.145*** |
| (0.137) | (0.0466) | (0.112) | (0.0436) | |
| Had or have severe COVID-19 symptom | −0.165 | −0.137** | 0.0703 | −0.121* |
| (0.235) | (0.0642) | (0.199) | (0.0735) | |
| Sleep duration on weekdays | −0.0284 | −0.0265** | ||
| (0.0348) | (0.0109) | |||
| Time trend | 0.0902 | 0.221*** | −0.533 | 0.985*** |
| (0.0830) | (0.0107) | (0.342) | (0.0630) | |
| Time trend squared | 0.116** | −0.156*** | ||
| (0.0588) | (0.0121) | |||
| IV: Single parent or spouseless | −0.520*** | −0.311*** | ||
| (0.0459) | (0.0253) | |||
| IV: Spouse’s non-work | −0.188*** | −0.212*** | ||
| (0.0342) | (0.0475) | |||
| IV: Respondent’s non-work | −0.129*** | |||
| (0.0342) | ||||
| Constant | −1.885* | 2.967*** | −1.182 | 2.674*** |
| (0.976) | (0.0740) | (0.730) | (0.128) | |
| lnσ2 | −0.611*** | −0.453*** | ||
| (0.0135) | (0.0124) | |||
| Athrho | 0.108 | 0.0687 | ||
| (0.174) | (0.169) | |||
| Weak instrument robust tests | AR test: chi2(3) = 5.02 | AR test: chi2(2) = 2.24 | ||
| Prob > chi2 = 0.1703 | Prob > chi2 = 0.3263 | |||
| N | 2724 | 2724 | 3263 | 3263 |
AR: Anderson–Rubin test. Standard errors in parentheses.
*** p < 0.01, ** p < 0.05, * p < 0.1
Table 7.
Results of OLS versus TSLS Estimation (2nd stage)
| Estimation method | Ordinary least squares | Two-stage least squares | ||
|---|---|---|---|---|
| Dependent variable | Poor self-assessed health (PSAH) | Poor self-assessed health (PSAH) | ||
| Variables / samples | Adults with children | Adults without children | Adults with children | Adults without children |
| Logged real household income | −0.0113 | −0.0195*** | −0.0337 | −0.0294 |
| (0.00727) | (0.00654) | (0.0311) | (0.0305) | |
| Gender (male = 1) | 0.00382 | −0.00550 | 0.00480 | −0.00521 |
| (0.00825) | (0.00862) | (0.00835) | (0.00866) | |
| Age | 0.000971 | 0.00143*** | 0.00107* | 0.00147*** |
| (0.000593) | (0.000520) | (0.000608) | (0.000530) | |
| Moderate or severe mental distress | 0.0598*** | 0.0811*** | 0.0597*** | 0.0800*** |
| (0.00911) | (0.00973) | (0.00911) | (0.0103) | |
| Moderate mental distress at an early stage of the COVID-19 pandemic | −0.0112 | −0.0836*** | −0.0169 | −0.0830*** |
| (0.0161) | (0.0176) | (0.0178) | (0.0177) | |
| Low health satisfaction | 0.461*** | 0.513*** | 0.458*** | 0.512*** |
| (0.0182) | (0.0167) | (0.0187) | (0.0173) | |
| Had or have severe COVID-19 symptom | −0.0245 | −0.00697 | −0.0272 | −0.00800 |
| (0.0251) | (0.0281) | (0.0253) | (0.0282) | |
| Sleep duration on weekdays | −0.00311 | −0.00339 | ||
| (0.00417) | (0.00425) | |||
| Time trend | 0.00451 | −0.0722*** | 0.00950 | −0.0622 |
| (0.00448) | (0.0250) | (0.00809) | (0.0390) | |
| Time trend squared | 0.0155*** | 0.0139** | ||
| (0.00474) | (0.00672) | |||
| Constant | −0.00510 | 0.106** | 0.0594 | 0.128 |
| (0.0351) | (0.0494) | (0.0938) | (0.0835) | |
| N | 2724 | 3263 | 2724 | 3263 |
Standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1
Both moderate or severe mental distress and low health satisfaction had positive effects on PSAH for adults with children and adults without children. Notably, for adults without children, a moderate mental illness at the beginning of the pandemic lowered the probability of PSAH. This implies health resilience for adults without children. The relationship between the age effect on PSAH and health resilience is unknown, but the age effect on PSAH was observed in adults without children and not in adults with children. The gender difference was small and not significant at the 5% level for PSAH. Comparing only those who did not increase telework, adults without children slept less on average on weekdays than those with children but worked longer hours. Many working women in their 40s and 50s in Japan work as non-regular employees with low wages, taking on a handful of household chores. Therefore, due to their multiple roles, weekday sleep duration was negatively associated with household income. Conversely, no such trend was observed among the adults without children who increased their teleworking. This group, 83% of which were women, worked the shortest hours at 25.4 h (Table 1). Experiencing SCS did not have an impact on PSAH.
Special benefits for all households (100 thousand JPY per household member) increased household income from September 2020 (Wave 2) to April 2021 (Wave 3). In FY2021, special benefits for households with children under 18 years old (100 thousand JPY per child) were provided to households with annual incomes of less than 9.6 million JPY, but not to adults without children. Consequently, the income of households without children decreased in September 2021 (Wave 4). The squared time trend term and the time trend explain these temporary income fluctuations within the sample period. The squared time trend for adults without children had a positive effect on PSAH. This explains the deterioration in health due to income decline during the second half of the sample period. The income-health relationship appears to be stronger for single parent or households without a spouse than for dual-earner households that account for the majority of adults with children.
Intra-household time allocation differs between households with and without children. Hence, we performed separate regression analyses for households with and without children. When the dependent variable is ordered, fixed-effects ordered logit (FEOL) models are useful for controlling unobserved time-invariant characteristics [59]. Individuals with the same LS scores over the sample period were excluded when estimating the FEOL models.
Two dependent variables (11-point scale variable and its five quantiles) were used for the FEOL model. Figure 2 shows the distribution of two dependent variables by presence of children. Adults with children tended to have higher LS values than adults without children. The distribution of the histograms on the 11-point scale for adults without children has three peaks at 3, 5, and 7.
Fig. 2.
Distribution of LS by presence of children
Table 4 presents the estimation results for the FEOL model. Neither the generalized residuals nor the interaction term between the generalized residuals and PSAH in the four equations were statistically significant at the 5% level. Therefore, the precise impact of PSAH on LS can be measured. However, for adults without children (11-point scale variable), logged real household income did not have a significant impact on LS, and the compensating variation of PSAH for this group could not be calculated. Therefore, we used a five-point scale variable to evaluate monetary compensation for the loss of well-being due to ill health. The age cubed was used to explain the bimodal nature of adults without children.
Table 4.
Results of FEOL estimation: 2SRI approach
| Dependent variable | Life satisfaction (5-point scale variable) | Life satisfaction (11-point scale variable) | ||
|---|---|---|---|---|
| Variables / samples | Adults with children | Adults without children | Adults with children | Adults without children |
| Gender (male = 1) | −0.0861 | 14.98*** | 0.0286 | 14.96*** |
| (0.640) | (0.927) | (0.591) | (0.916) | |
| Age cubed | −0.204*** | −0.223*** | ||
| (0.00858) | (0.00855) | |||
| Age squared | −0.00346** | 15.78*** | −0.00428*** | 17.24*** |
| (0.00138) | (0.663) | (0.00158) | (0.660) | |
| Logged real household income | 0.223** | 0.194** | 0.260*** | 0.118 |
| (0.0956) | (0.0954) | (0.0957) | (0.0901) | |
| Logged real household income × Telecommuting | 0.0374 | −0.0431 | −0.00460 | −0.0333 |
| (0.0805) | (0.0827) | (0.0702) | (0.0858) | |
| Severe mental distress | −1.631*** | −1.362*** | −1.504*** | −1.290*** |
| (0.363) | (0.321) | (0.308) | (0.291) | |
| Moderate mental distress | −0.626*** | −0.511*** | −0.654*** | −0.518*** |
| (0.172) | (0.164) | (0.170) | (0.155) | |
| Poor self-assessed health (PSAH) | −1.634** | −1.027** | −2.239*** | −1.186*** |
| (0.816) | (0.524) | (0.781) | (0.446) | |
| Generalized residual | 1.114* | 0.338 | 1.062 | 0.744* |
| (0.630) | (0.493) | (0.667) | (0.381) | |
| Generalized residual × Telecommuting | 3.284* | −0.599 | 2.320* | −0.419 |
| (1.860) | (1.278) | (1.385) | (1.273) | |
| PSAH × Generalized residual | −0.402 | 0.0891 | 0.0695 | −0.303 |
| (0.723) | (0.527) | (0.773) | (0.430) | |
| PSAH × Generalized residual × Telecommuting | −2.744 | 2.060 | −1.809 | 1.902 |
| (1.986) | (1.727) | (1.494) | (1.911) | |
| Work-centered lifestyle | −0.404* | −0.444* | ||
| (0.244) | (0.234) | |||
| Respondent’s non-work | 1.174*** | 0.987*** | ||
| (0.432) | (0.358) | |||
| Debt | −0.657*** | −0.647*** | ||
| (0.198) | (0.177) | |||
| Income insecurity | −0.247* | −0.334** | ||
| (0.149) | (0.144) | |||
| Spouse’s non-work | 0.720** | 0.784*** | ||
| (0.312) | −0.292 | |||
| N | 1719 | 2041 | 2047 | 2398 |
| N of panel units | 536 | 623 | 646 | 739 |
| Pseudo R-squared | 0.0729 | 0.0544 | 0.0793 | 0.0599 |
Robust standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1
Interestingly, different effects of health losses on LS were observed between adults with children and adults without children (Table 4). PSAH negatively affected the LS of adults with children at the 5% level; however, it did not have the same effect on the LS of adults without children. For adults with children, the compensating variation of PSAH was 7.3 times the real monthly household income (7.327 =−[−1.634/0.223]). This implies that 7.3 times the real monthly household income is required for adults with children to compensate for their loss of well-being due to poor health. For adults without children, the compensating variation of PSAH was 5.294 (=−[−1.027/0.194]), which is 27.7% lower than that for adults with children. The estimation results supported our hypothesis that monetary compensation for the loss of well-being due to ill health among adults with children during the sample period was greater than that of adults without children. Adults with children’s health losses were approximately 3.49 million JPY (349.0 = 7.327 × 476.3 thousand JPY), that is, 1.04 million JPY more than that of adults without children (245.0 = 5.294 × 462.9 thousand JPY).
In the two equations of the 5-point scale LS, neither the interaction term between telecommuting and logged real household income nor the interaction term between telecommuting and the generalized residuals were statistically significant at the 5% level. Therefore, we can consider that increased teleworking did not affect monetary compensation for the loss of well-being due to ill health and did not cause the endogeneity between health and LS.
The severity of health conditions substantially affects the corresponding compensating income variations, with an increase in this variation from moderate to severe conditions [60]. The FEOL model accounted for the severity of mental health status. The higher the severity of mental health, the greater the estimated coefficients on LS (Table 4). However, the JHPS COVID-19 Special Survey does not provide any information on the objective health status regarding SCS or whether COVID-19 symptoms were prolonged (long COVID-19), making it impossible to estimate the compensating variation for each severe symptom of COVID-19.
Mental health deterioration indirectly and directly affected both subjective poor health and LS (Tables 3 and 4). Indeed, severe mental distress negatively affected the LS of adults with children at the 5% level, and its effect was almost the same of PSAH. Random effects-ordered probit models were estimated to explore the determinants of worsening mental health. The dependent variable was mental ill-health, which took the value of 2 if the response was severe mental distress, 1 for moderate mental distress, and 0 otherwise.
Estimation results indicated that shorter sleep duration on weekdays, debt, and job insecurity had positive effects on mental ill-health (Table 5). For both adults with children and adults without children, telecommuting had no effects on mental ill-health. For adults with children, shorter sleep hours on weekdays and job insecurity due to the presence of children are likely to have a bidirectional effect. Therefore, it is necessary to consider health policies for the determinants of mental ill-health for adults with and without children. Adults with children were more likely to be mentally ill-health at the 1% level in the two lowest income classes, but there was no similar trend in adults without children.
Table 5.
Results of random effects-ordered probit model
| Dependent variable | Mental ill-health | |
|---|---|---|
| Variables | Adults with children | Adults without children |
| Gender (male = 1) | −0.441*** | −0.387*** |
| (0.119) | (0.115) | |
| Age | 0.0151* | −0.0368*** |
| (0.00848) | (0.00701) | |
| Low household income | 0.411*** | 0.410*** |
| (0.104) | (0.0910) | |
| Middle household income | 0.421*** | 0.0395 |
| (0.140) | (0.122) | |
| High household income | 0.264** | 0.172 |
| (0.112) | (0.108) | |
| Sleep duration on weekdays | −0.0972** | −0.122*** |
| (0.0474) | (0.0442) | |
| Debt | 0.582*** | 0.562*** |
| (0.132) | (0.122) | |
| Job insecurity | 0.725*** | 0.655*** |
| (0.121) | (0.107) | |
| Telecommuting | 0.186 | 0.211 |
| (0.136) | (0.184) | |
| Constant | 0.366 | −2.377*** |
| (0.521) | (0.468) | |
| σu2 | 2.385*** | 2.611*** |
| (0.300) | (0.285) | |
| N | 2841 | 3535 |
| N of panel units | 1148 | 1321 |
Standard errors in parentheses. *** p < 0.01, ** p < 0.05, * p < 0.1
Discussion
The compensating variation for loss of wellbeing due to poor health among adults with children is 7.3 times the real monthly household income, while that of childless adults is 5.3 times the real monthly household income. What causes this difference in the monetary value of the loss of well-being due to poor health between adults with children and adults without children?
We consider the influencing factors based on the two estimation results. The direct impact of PSAH and severe mental distress on LS was greater for adults with children than for adults without children (Table 4). Adults with children were more likely to have poor mental health in the two lowest income classes (Table 5). Early into the pandemic, childcare anxiety increased substantially among mothers living in seven prefectures with high infection rates [61]. Nevertheless, there was a reduction in the number of patients with acute medical illnesses because of fear of contagion. The reduced per capita healthcare costs of preschool children were greater among prefectures taking specific precautions [62].
These changes further exacerbated healthy parent–child relationships, and most of the differences in the monetary value of the loss of well-being are explained by the intergenerational transmission of well-being. Powdthavee and Vignoles [63] used a multilevel multivariate response model that allows for both the child’s LS and parents’ mental distress to be estimated simultaneously in a single equation; they show that a child’s LS is associated with a lower level of their father’s distress a year later, regardless of the gender of the child.
Considering that the higher levels of paternal and maternal distress were significantly associated with lower levels of LS in the child, the association between parental stress and children’s LS is primarily due to either distress-to-distress contagion, transmission via parent–child interaction, or both [63].
As the JHPS COVID-19 Special Survey does not provide any information on a child’s LS, the age of the youngest child, or the number of children, we cannot discuss the specific intergenerational transmission of well-being based on the results of this study. Increased teleworking did not affect monetary compensation for the loss of well-being due to ill health. However, it is not clear from the data in this study whether intergenerational relationships within families increased the magnitude of the monetary value of the loss of well-being due to ill health during the pandemic.
One of the limitations of this study is the lack of information on the SCS when exploring the compensation variation classified by SCS. Future studies should use detailed information on COVID-19 symptoms to provide monetary value for moderate-to-severe conditions. Another limitation is that the JHPS does not provide the number of chronic diseases that affect individuals’ LS. Therefore, we used a dummy variable for low health satisfaction as the proxy variable for the high number of chronic diseases.
Nevertheless, the strength of this study lies in demonstrating that the loss of well-being attributable to health deterioration through a lower income and lifestyle changes was much greater than that attributable to the SCS. The cost of death in the US as of July 2, 2020, was estimated over $1.4 trillion [64], and the value of reducing the risk of fatality from COVID-19 infection was twice as high as the risk of lung disease and cancer from air pollution [65]. Despite the focus on these, the compensatory variation in ill health among middle-aged adults may have been underestimated.
To prevent the deterioration of subjective health among adults with children, quantifying the impact of changes in their work and living environments on their health is critical. Lower income, shorter sleep duration on weekdays, and job insecurity are associated with PSAH through mental ill-health; thus, attention should be paid to changes in income, sleep duration, and job insecurity.
Using the German Socio-Economic Panel (2002–2020), Mikucka et al. [66] show that the long-term effects of job insecurity tend to have lasting effects on health. From a similar perspective, the accumulated adverse health effects during the COVID-19 pandemic may have long-term consequences. However, the data in this study were collected over a short period of two years, and we cannot analyze the accumulated results of negative health effects.
Conclusion
The present study showed a significant difference in the monetary value of the loss of well-being due to poor health between adults with children and adults without children during the sample period. To compensate for the loss of well-being due to poor health, adults with children were required to earn 7.3 times their monthly household income. By contrast, the compensating variation among adults without children was approximately 5.3 times their monthly household income. The deterioration of a healthy parent–child relationship during the sample period increased the monetary value of the loss of well-being. As higher levels of mental health distress are associated with poorer health, attention must be paid to changes in income, sleep duration, and job insecurity among adults with children. We should not underestimate the negative impacts of ill-health among adults with children during shocks such as the COVID-19 pandemic.
Acknowledgements
We are thankful for the helpful comments by Prof. Takashi Oshio on an early version of our manuscript.
Abbreviations
- FEOL
Fixed-effects ordered logit
- IV
Instrumental variable
- JHPS
Japan Household Panel Survey
- LS
Life satisfaction
- OOB
Out-of-bag
- RF
Random forest
- SAH
Self-assessed health
- PSAH
Poor self-assessed health
- SCS
Severity of COVID-19 symptoms
- SES
Socioeconomic status
- SWB
Subjective well-being
- WFC
Work-family conflicts
- 2SRI
Two-stage residual inclusion
Appendix
Author contributions
NK: Writing– original draft, Formal analysis, Conceptualization. TA and MJ: Writing– review.
Funding
We appreciate the research grant from Murata Science and Education Foundation to our study project “Economic Evaluation of Health Losses Accounting for Two Major Risks during Infectious Disease Outbreaks.”
Data availability
The datasets used in this study are owned by Panel Data Research Center at Keio University and cannot be shared publicly. However, the datasets can be accessed at no cost, under the Usage Agreement. The PDRC at Keio University provides microdata for nonprofit and academic purposes only. Qualifications and requirements for usage, and procedures for requesting and using the data are shown in the following website: https://www.pdrc.keio.ac.jp/en/paneldata/howto/.
Declarations
Ethics approval and consent to participate
The present study falls under (1) to (3) below. In medical research in Japan, the Ethical Guidelines for Life Sciences and Medical Research Involving Human Subjects (2021), which are the standard ethical guidelines based on the Declaration of Helsinki, have been established. It defines research that meets the following conditions as not subject to the ethical guidelines. (1) Samples and information that have established academic value, are widely used for research purposes, and are generally available to the public. (2) Existing information that does not fall under the category of information on individuals. (3) Anonymized processed information that has already been created.
Consent for publication
Not applicable.
Generative AI and AI-assisted technologies in the writing process
None.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Adams-Prassl A, Boneva T, Golin M, Rauh C. The impact of the coronavirus lockdown on mental health: evidence from the united States. Econ Policy. 2022;37:139–55. 10.1093/epolic/eiac002. [Google Scholar]
- 2.Davillas A, Jones AM. The first wave of the COVID-19 pandemic and its impact on socioeconomic inequality in psychological distress in the UK. Health Econ. 2021;30:1668–83. 10.1002/hec.4275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao X, Davillas A, Jones AM. The Covid-19 pandemic and its impact on socioeconomic inequality in psychological distress in the united kingdom: an update. Health Econ. 2022;31:912–20. 10.1002/hec.4480. [DOI] [PubMed] [Google Scholar]
- 4.Pedraza P, Marin G, Kea T. Life dissatisfaction and anxiety in COVID-19 pandemic. MUNI econ working Paper, No. 2020-03. MUNI ECON WP. 2020;(3). 10.5817/WP_MUNI_ECON_2020-03
- 5.Etheridge B, Spantig L. The gender gap in mental well-being at the onset of the Covid-19 pandemic: evidence from the UK. Eur Econ Rev. 2022;145:104114. 10.1016/j.euroecorev.2022.104114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huebener M, Waights S, Spiess CK, Siegel NA, Wagner GG. Parental well-being in times of Covid-19 in Germany. Rev Econ Househ. 2021;19:91–122. 10.1007/s11150-020-09529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yanfei Z. How women bear the Brunt of COVID-19’s damages on work (continued): the gender gap in employment recovery. Jpn Lab Issues. 2021;5:2–10. [Google Scholar]
- 8.Sakuragi T, Tanaka R, Tsuji M, Tateishi S, Hino A, Ogami A, et al. Gender differences in housework and childcare among Japanese workers during the COVID-19 pandemic. J Occup Health. 2022;64:e12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanata T, Takeda K, Fujii T, Iwata R, Hiyoshi F, Iijima Y, et al. Gender differences and mental distress during COVID-19: a cross-sectional study in Japan. BMC Psychiatry. 2024;24:776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandola T, Martikainen P, Bartley M, Lahelma E, Marmot M, Michikazu S, et al. Does conflict between home and work explain the effect of multiple roles on mental health? A comparative study of finland, japan, and the UK. Int J Epidemiol. 2004;33:884–93. 10.1093/ije/dyh155. [DOI] [PubMed] [Google Scholar]
- 11.Tachibanaki T, Takamatsu R. Statistical analysis on perceived happiness (Kofukukan no Toukei Bunseki). Japan: Iwanamishoten; 2018. (in Japanese). [Google Scholar]
- 12.Kumagai N. Valuation of health losses of women with multiple roles using a well-being valuation approach: evidence from Japan. PLoS ONE. 2021;16:e0251468. 10.1371/journal.pone.0251468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldin C. Career & family: women’s Century-Long journey toward equity. Princeton University Press; 2021. [Google Scholar]
- 14.Trógolo MA, Moretti LS, Medrano LA. A nationwide cross-sectional study of workers’ mental health during the COVID-19 pandemic: impact of changes in working conditions, financial hardships, psychological detachment from work and work-family interface. BMC Psychol. 2022;10:73. 10.1186/s40359-022-00783-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jung G, Ha JS, Seong M, Song JH. The effects of depression and fear in dual-income parents on work-family conflict during the COVID-19 pandemic. Sage Open. 2023;13:21582440231157662. 10.1177/21582440231157662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bilodeau J, Quesnel-Vallée A, Poder T. Work stressors, work-family conflict, parents’ depressive symptoms and perceived parental concern for their children’s mental health during COVID-19 in canada: a cross-sectional analysis. BMC Public Health. 2023;23:2181. 10.1186/s12889-023-17037-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michalos AC. Satisfaction and happiness. Soc Indic Res. 1980;8:385–422. 10.1007/BF00461152. [Google Scholar]
- 18.Meadow HL, Mentzer JT, Rahtz DR, Sirgy MJ. A life satisfaction measure based on judgment theory. Soc Indic Res. 1992;26:23–59. 10.1007/BF00303824. [Google Scholar]
- 19.Crooker KJ, Near JP. Happiness and satisfaction: Measures of affect or cognition? Soc Indic Res. 1998;44:195–224. 10.1023/A:1006820710885. [Google Scholar]
- 20.Brown TT. The subjective well-being method of valuation: an application to general health status. Health Serv Res. 2015;50:1996–2018. 10.1111/1475-6773.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howley P. Less money or better health? Evaluating individual’s willingness to make trade-offs using life satisfaction data. J Econ Behav Organ. 2017;135:53–65. 10.1016/j.jebo.2017.01.010. [Google Scholar]
- 22.Ferrer-i-Carbonell A, van Praag BMS. The subjective costs of health losses due to chronic diseases. An alternative model for monetary appraisal. Health Econ. 2002;11:709–22. 10.1002/hec.696. [DOI] [PubMed] [Google Scholar]
- 23.McNamee P, Mendolia S. The effect of chronic pain on life satisfaction: evidence from Australian data. Soc Sci Med. 2014;121:65–73. 10.1016/j.socscimed.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 24.Powdthavee N, van den Berg B. Putting different price tags on the same health condition: re-evaluating the well-being valuation approach. J Health Econ. 2011;30:1032–43. 10.1016/j.jhealeco.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 25.van Praag B, Ferrer-i-Carbonell A. Happiness quantified: a satisfaction calculus approach. Oxford University Press; 2004. [Google Scholar]
- 26.Ásgeirsdóttir TL, Birgisdottir KH, Ólafsdóttir T, Olafsson SP. A compensating income variation approach to valuing 34 health conditions in Iceland. Econ Hum Biol. 2017;27:167–83. 10.1016/j.ehb.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Ólafsdóttir T, Ásgeirsdóttir TL, Norton EC. Valuing pain using the subjective well-being method. Econ Hum Biol. 2020;37:100827. 10.1016/j.ehb.2019.100827. [DOI] [PubMed] [Google Scholar]
- 28.Kucharska-Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population-based data from the united States and Finland. Ann Epidemiol. 2011;21:572–9. 10.1016/j.annepidem.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mosquera PA, San Sebastian M, Waenerlund AK, Ivarsson A, Weinehall L, Gustafsson PE. Income-related inequalities in cardiovascular disease from mid-life to old age in a Northern Swedish cohort: a decomposition analysis. Soc Sci Med. 2016;149:135–44. 10.1016/j.socscimed.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 30.Adler NE, Rehkopf DH. U.S. Disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235– 52. 10.1146/annurev.publhealth.29.020907.090852 [DOI] [PubMed] [Google Scholar]
- 31.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mackenbach JP, Valverde JR, Bopp M, Brønnum-Hansen H, Deboosere P, Kalediene R, et al. Determinants of inequalities in life expectancy: an international comparative study of eight risk factors. Lancet Public Health. 2019;4:e529–37. 10.1016/S2468-2667(19)30147-1. [DOI] [PubMed] [Google Scholar]
- 33.Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36:349–70. 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petrovic D, de Mestral C, Bochud M, Bartley M, Kivimäki M, Vineis P, et al. The contribution of health behaviors to socioeconomic inequalities in health: a systematic review. Prev Med. 2018;113:15–31. 10.1016/j.ypmed.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, Kivimäki M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLOS Med. 2011;8:e1000419. 10.1371/journal.pmed.1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu KQ, Aw JYH, Payne CF. Inequalities in mortality in the Asia-Pacific: a cross-national comparison of socioeconomic gradients. J Gerontol B Psychol Sci Soc Sci. 2024;79:gbad193. 10.1093/geronb/gbad193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dolan P, Kahneman D. Interpretations of utility and their implications for the valuation of health. Econ J. 2008;118:215– 34. 10.1111/j.1468-0297.2007.02110.x [Google Scholar]
- 38.Dolan P, Peasgood T, White M. Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being. J Econ Psychol. 2008;29:94–122. 10.1016/j.joep.2007.09.001. [Google Scholar]
- 39.Easterlin RA. Explaining happiness. Proc Natl Acad Sci U S A. 2003;100:11176–83. 10.1073/pnas.1633144100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–76. 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 41.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21:88–97. 10.1002/mpr.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62(9):686–91. 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 43.Yoon K, Lee M. Factors influencing the health satisfaction of users of public health and medical institutions in South Korea. Front Public Health. 2022;10:1079347. 10.3389/fpubh.2022.1079347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dolan P, Kavetsos G, Tsuchiya A. Sick but satisfied: the impact of life and health satisfaction on choice between health scenarios. J Health Econ. 2013;32:708–14. 10.1016/j.jhealeco.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breiman L. Random forests. Mach Learn. 2001;45:5–32. 10.1023/A:1010933404324. [Google Scholar]
- 46.Ellis K, Kerr J, Godbole S, Lanckriet G, Wing D, Marshall S. A random forest classifier for the prediction of energy expenditure and type of physical activity from wrist and hip accelerometers. Physiol Meas. 2014;35:2191–203. 10.1088/0967-3334/35/11/2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schonlau M, Zou RY. The random forest algorithm for statistical learning. Stata J. 2020;20:3–29. 10.1177/1536867X20909688. [Google Scholar]
- 48.Zhang C, Ding Y, Peng Q. Who determines united States healthcare out-of-pocket costs? Factor ranking and selection using ensemble learning. Health Inf Sci Syst. 2021;9:22. 10.1007/s13755-021-00153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumagai N, Jakovljević M. Random forest model used to predict the medical out-of-pocket costs of hypertensive patients. Front Public Health. 2024;12:1382354. 10.3389/fpubh.2024.1382354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. J Health Econ. 2008;27:531–43. 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gana K, Bailly N, Saada Y, Joulain M, Trouillet R, Hervé C, et al. Relationship between life satisfaction and physical health in older adults: a longitudinal test of cross-lagged and simultaneous effects. Health Psychol. 2013;32:896–904. 10.1037/a0031656. [DOI] [PubMed] [Google Scholar]
- 52.Imbens GW, Angrist JD. Identification and estimation of local average treatment effects. Econometrica. 1994;62(2):467–75. 10.2307/2951620. [Google Scholar]
- 53.Basu A, Coe NB, Chapman CG. 2SLS versus 2SRI: appropriate methods for rare outcomes and/or rare exposures. Health Econ. 2018;27:937–55. 10.1002/hec.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oshio T, Inoue A, Tsutsumi A. Does work-to-family conflict really matter for health? Cross-sectional, prospective cohort and fixed-effects analyses. Soc Sci Med. 2017;175:36–42. 10.1016/j.socscimed.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 55.Binder M, Coad A. I’m afraid I have bad news for you… estimating the impact of different health impairments on subjective well-being. Soc Sci Med. 2013;87:155–67. 10.1016/j.socscimed.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 56.Kohara M. Determining intrahousehold time allocation for workers with children (Kodomo Noiru Roudousha no Kakeinai Jikanhaibun no Kettei). Jpn J Lab Stud. 2019;707:47–59. (in Japanese). [Google Scholar]
- 57.Salanti G, Peter N, Tonia T, Holloway A, White IR, Darwish L, et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: a systematic review and dose–response meta-analysis. Ann Intern Med. 2022;175:1560–71. 10.7326/M22-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Foremny D, Sorribas-Navarro P, Vall Castelló J. Income insecurity and mental health in pandemic times. Econ Hum Biol. 2024;53:101351. 10.1016/j.ehb.2024.101351. [DOI] [PubMed] [Google Scholar]
- 59.Baetschmann G, Ballantyne A, Staub KE, Winkelmann R. Feologit: a new command for fitting fixed-effects ordered logit models. Stata J. 2020;20:253–75. 10.1177/1536867X20930984. [Google Scholar]
- 60.Baldursdottir K, Asgeirsdottir TL, Olafsdottir T. How sensitive is the compensating income variation to severity and adaptation? Econ Hum Biol. 2023;49:101213. 10.1016/j.ehb.2022.101213. [DOI] [PubMed] [Google Scholar]
- 61.Takaku R, Yokoyama I. What the COVID-19 school closure left in its wake: evidence from a regression discontinuity analysis in Japan. J Public Econ. 2021;195:104364. 10.1016/j.jpubeco.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kumagai N. The impact of the COVID-19 pandemic on physician visits in Japan. Front Public Health. 2021;9:743371. 10.3389/fpubh.2021.743371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Powdthavee N, Vignoles A. Mental health of parents and life satisfaction of children: a within-family analysis of intergenerational transmission of well-being. Soc Indic Res. 2008;88:397–422. 10.1007/s11205-007-9223-2. [Google Scholar]
- 64.Viscusi WK. Pricing the global health risks of the COVID-19 pandemic. J Risk Uncertain. 2020;61:101–28. 10.1007/s11166-020-09337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hammitt JK. Valuing mortality risk in the time of COVID-19. J Risk Uncertain. 2020;61:129–54. 10.1007/s11166-020-09338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mikucka M, Arránz Becker O, Worl C. Short- and long-term health effects of job insecurity. Fixed effects panel analysis of German data. Scand J Work Environ Health. 2025;51(2):68–76. 10.5271/sjweh.4206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used in this study are owned by Panel Data Research Center at Keio University and cannot be shared publicly. However, the datasets can be accessed at no cost, under the Usage Agreement. The PDRC at Keio University provides microdata for nonprofit and academic purposes only. Qualifications and requirements for usage, and procedures for requesting and using the data are shown in the following website: https://www.pdrc.keio.ac.jp/en/paneldata/howto/.