Abstract
The Roche COBAS AMPLICOR human immunodeficiency virus type 1 (HIV-1) Monitor (version 1.5) standard and ultrasensitive viral load assays often gave discordant results, with viral loads from the standard assay exceeding those from the ultrasensitive assay by more than 0.5 log10 for approximately 20% of specimens received. We began studies to determine the extent, magnitude, and reproducibility of the discordance between the assays and to discover and eliminate the cause of this discordance. Until then, we revised our standard operating procedure to include both standard and ultrasensitive testing on all specimens submitted for viral load determinations. Discordant results usually recurred on retesting. They were most prevalent for specimens with ultrasensitive viral loads of <1,000 and rare for specimens with viral loads of >10,000. Often, standard assay results exceeded those of the ultrasensitive assay by 50- to 100-fold. At higher viral loads, the difference between the standard and ultrasensitive assays persisted, but the percent difference was smaller and rarely caused discordance. The proportion of discordant results was significantly higher in specimens from pediatric patients than in specimens from adults. The ultrasensitive viral load determinations generally agreed with the results of the B-DNA (Bayer) viral load assays. If the plasma was transferred from the centrifuged plasma preparation tubes before freezing, standard and ultrasensitive results were concordant with each other and with values determined on plasma from lavender-topped EDTA tubes.
Human immunodeficiency virus (HIV) viral load determinations represent the standard of care in the initial assessment of HIV-infected persons and in the subsequent management of the disease (4, 11, 13). Spurious high viral loads may cause patients to be started unnecessarily on antiretroviral therapy. For the patient on therapy, such elevated results could prompt unnecessary repeat testing, HIV genotyping, or medication changes. Pregnant women could receive unnecessary caesarean sections. Providers may wrongly conclude that there is nonadherence to a prescribed antiretroviral regimen. Erroneous conclusions may be drawn if the patient is participating in a clinical trial. Thus, accuracy and reproducibility of the viral load results are important considerations. The Roche standard and ultrasensitive assays, available in manual and automated (COBAS) versions, are the most common tests for viral load quantification, and the Bayer Versant human immunodeficiency virus type 1 (HIV-1) RNA 3.0 (B-DNA) assay (Tarrytown, New York) is also widely used. The standard and ultrasensitive assays have been reported to correlate well both within versions and between versions 1.0 and 1.5 (2, 3, 5, 6), although at very low viral loads version 1.5 is the more sensitive (2, 9).
Our laboratory offered both (COBAS) standard and ultrasensitive assays (version 1.5) and performed the ordered test. When standard and ultrasensitive assays were performed with the same patient sample, the ultrasensitive result was less than 50 RNA copies/ml, while the standard result was 3,000. This discordance recurred on retesting the specimen. Determination of the HIV-1 viral loads for 20 pediatric patients by both standard and ultrasensitive methods revealed similar discordances in six of the results, with the standard results being higher. From July to December 2004, we revised our standard operating procedure to perform both standard and ultrasensitive assays on all plasma specimens submitted for viral load determination and began investigations to determine which result was correct and how to eliminate the problem.
(A preliminary version of these data was presented informally by E. C. Moore at the Pediatric AIDS Clinical Trials Group Winter Meeting, Baltimore, Md., 1 to 4 December 2004. Some information was also provided to Becton-Dickinson to allow them to alert other clients to the discrepancy and the techniques we developed to avoid it.)
MATERIALS AND METHODS
Patients.
Patient specimens used in the study were submitted to Detroit Medical Center (DMC) University Laboratories for viral load testing between July and December of 2004. Eighty percent of the patients came from the DMC adult HIV clinic (1,600 patients) or the pediatric clinic (about 90 patients). The remainder of the specimens were submitted by infectious-disease physicians or came from patients in our component hospitals or the high-risk-pregnancy clinic. This study was approved by the Human Subjects Committee of Wayne State University.
Specimen collection and transport.
Except as described for the individual experiments, blood was collected in plasma preparation tubes (PPT) by standard venipuncture and maintained at room temperature until centrifuged at 1,100 × g for 20 min within 4 h of collection. The PPT was then frozen at −20°C until the day of testing, when it was thawed at room temperature. The PPT is an evacuated plastic tube for the collection of venous blood. It contains dried K2EDTA as an anticoagulant. It also contains a proprietary gel material that, during centrifugation, allows the cellular elements to pass through and forms a barrier between the plasma and the cells. This technology permits transportation of the PPT without decanting the cell-free plasma. The tube is intended to prepare plasma for molecular diagnostic techniques such as PCR. Publications from Roche and Becton-Dickinson (7, 8) support freezing the PPT for the transport and storage of specimens intended for viral load determination. These handling techniques were validated for both standard and ultrasensitive assays in our laboratory in 2000 (see Discussion.)
Viral load testing.
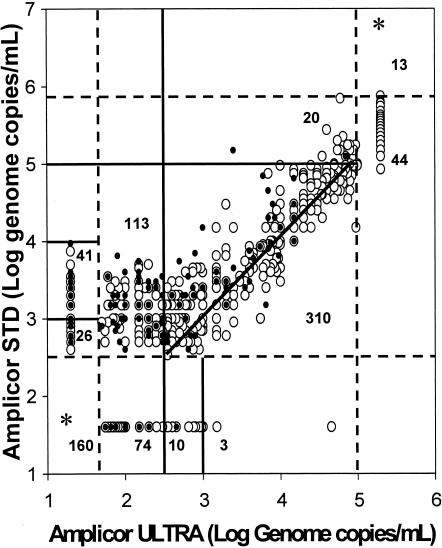
The Roche COBAS AMPLICOR HIV-1 Monitor (version 1.5) standard and ultrasensitive assays were carried out according to instructions on the package inserts. Standard and ultrasensitive assays are performed with the same kit but differ in sample preparation. The standard assay begins with untreated plasma, which is lysed, extracted, precipitated, and redissolved. A sample derived from 25 μl of plasma is used in the assay. For the ultrasensitive assay, plasma is ultracentrifuged to sediment the virus. The supernatant plasma is discarded, and the viral pellet is lysed, extracted, precipitated, and redissolved. A sample prepared from 250 μl of original plasma is assayed. The standard assay has a linear range from 400 to 750,000 RNA copies/ml, while the ultrasensitive assay is linear between 50 and 100,000 RNA copies/ml. The standard and ultrasensitive assays are capable of detecting virus below 400 and 50 genome copies per ml, respectively, but the results are nonlinear. The quantity present is reported as <400 or <50, with the designation (D) or (ND) appended to indicate whether viral nucleic acids were detected or not detected, respectively. The data presented in Fig. 1 were transformed to the base 10 logarithm (log10 HIV-1 RNA copies/ml).
FIG. 1.
Comparison of log10-transformed standard and ultrasensitive HIV-1 viral loads. The standard (STD) and ultrasensitive (ULTRA) results of 145 specimens from 96 pediatric patients (•) and 669 specimens from 572 adult patients (○) are plotted against one another. The solid diagonal line is the line of unity. Concordant results lie on this line or within 0.5 log10 of it. The dashed vertical lines at 1.70 (log10 of 50) and 5 (log10 of 100,000) indicate the limits of the linear range of the ultrasensitive assay, and the dashed horizontal lines at 2.60 (log10 of 400) and 5.88 (log10 of 750,000) show the limits of the linear range of the standard assay. A solid vertical line intersects the x axis at 2.60 and delineates the ultrasensitive results which are defined to be in agreement with the standard results of <400. The other internal lines are convenience lines; the numbers within the boxes they create indicate the number of results within these areas of the graph. The asterisks and adjacent numbers indicate the specimens above or below the limits of linearity of both assays.
Definition of discordant results.
Discordant results were arbitrarily defined to be those in which the viral loads determined by the standard and ultrasensitive assays differed by more than 0.5 log10, or about 3.2-fold, although the actual difference was generally larger. We chose this number in part because it represents the difference that most clinicians assume is clinically significant (10). At high copy numbers, the assay variation is approximately 0.2 log10 (1, 10). Other authors have shown that the assay variation is larger at the lower ends of the linear ranges (6). The differences between the lower limits of the quantification ranges of the standard and ultrasensitive assays introduce unavoidable anomalies into the evaluation of discordance. A specimen with a standard result of 400 and an ultrasensitive result of <50 is discordant (minimum difference of eightfold). For a sample with a standard result of <400 and an ultrasensitive result of <50, concordance cannot be excluded. The difference in the detection limits may cause an unavoidable underestimate of discordance.
Statistical analysis.
Data were analyzed using SPSS for Windows v. 11.0 (SPSS, Inc., Chicago, Ill.). Fisher's exact tests were used to compare discordance rates in specimens from children versus rates in specimens from adults for each ultrasensitive range and for combined ranges.
RESULTS
Comparison of ultrasensitive and standard viral loads.
Viral load results from both standard and ultrasensitive assays were available for 1,265 specimens (including the 814 presented in Fig. 1). Of these, 230 (18.2%) were discordant. Two hundred eighteen discordant specimens were sent to our reference laboratory for repeat testing, and both standard and ultrasensitive results were received for 179 specimens. One hundred eleven specimens (62.0%) remained discordant, while 68 (38.0%) became concordant due to a decrease in standard results. The number of discordant specimens per run (22 specimens) varied between 0 and 13.
Figure 1 shows a plot of log10-transformed standard and ultrasensitive results from consecutive adult and pediatric patient specimens during the first 3 months of the study. These specimens are included in the 1,265 discussed above. One hundred forty-five specimens were included from 96 HIV-infected pediatric patients (only the first two specimens/patient are included), aged between 3 months and 17 years, including 38 females. The overall discordance rate was 49.0%; for the 135 specimens with ultrasensitive viral loads less than 10,000 RNA copies/ml, it was 51.9%. No pediatric specimen had an ultrasensitive viral load greater than 100,000 RNA copies/ml. Figure 1 also shows 669 results from 572 adult patients (five patients have three specimens each), ages 18 to 77, including 198 females. The overall discordance rate was 20.1%, and the rate among specimens with ultrasensitive viral loads of ≤10,000 RNA copies/ml was 25.3%. Fifty-seven adult specimens (9%) exceeded 100,000 RNA copies/ml. Even in concordant specimens, where the difference between the standard and ultrasensitive viral loads was <0.5 log, the viral load result determined by the standard assay was generally the higher.
The percentage of specimens with discordant results was higher from children than from adults. To determine whether the differences in percentage of discordant specimens were significant for children versus adults, the data from Fig. 1 were stratified by ultrasensitive viral load and are shown in Table 1. The difference in proportion of discordant specimens from children versus from adults is significant for all specimens and for those with viral loads of <1,000, both stratified and aggregated as shown in the table. For viral loads between 1,000 and 9,500, the proportion of discordant specimens is higher for children (22.2%) than for adults (11.1%); however, there are so few pediatric patients with viral loads in this range that we do not have adequate power to demonstrate that the pediatric and adult discordance rates differ significantly. Causes of the difference in discordance rates between children and adults are under investigation.
TABLE 1.
Difference in percentage of discordant HIV viral load determinations from children versus from adults, stratified by ultrasensitive assay results
| Range of ultrasensitive viral loads (no. of RNA copies/ml) | Samples from adults
|
Samples from children
|
Significancea of difference in % of discordance | ||||
|---|---|---|---|---|---|---|---|
| No. in rangeb | No. discordant | % Discordant | No. in rangeb | No. discordant | % Discordant | ||
| <50† | 168** | 38 | 22.6 | 59** | 29 | 49.2 | <0.001 |
| 50-350† | 140** | 59 | 42.1 | 47** | 31 | 66.0 | 0.007 |
| 400-950† | 64** | 12 | 18.8 | 11** | 6 | 54.5 | 0.019 |
| 1,000-9,500 | 108** | 12 | 11.1 | 18 | 4 | 22.2 | 0.244 |
| >10,000 | 189 | 14 | 7.4 | 10 | 1 | 10.0 | 0.552 |
| All specimens | 669 | 135 | 20.2 | 145 | 71 | 34.5 | <0.001 |
| <1,000c | 372 | 109 | 29.3 | 117 | 66 | 56.4 | <0.001 |
Significance determined by Fisher's exact test.
**, includes specimens with results below the linear range of one or both of the assays.
Combined results from all specimens with ultrasensitive viral loads of <1,000 (rows marked with †).
B-DNA results.
When the problem with discordant results was first detected, we did not know whether the standard or ultrasensitive results (or neither) were correct. Fifty-six discordant specimens with adequate remaining plasma were sent to a reference laboratory for viral load determinations by the B-DNA technique. Of these, 49 were concordant with the ultrasensitive results (using the same 0.5 log10 definition applied to comparisons between standard and ultrasensitive results). Of seven (12.5%) specimens with discordance between ultrasensitive and B-DNA results, only three ultrasensitive results exceeded the B-DNA results by more than fivefold. No B-DNA viral load was higher than its corresponding ultrasensitive result. Thus, no B-DNA result could have been concordant with the standard result on the same specimen. This information suggests that the results of the ultrasensitive assay are generally reliable (data not shown). Additional B-DNA results are shown in Table 2.
TABLE 2.
Effect of plasma preparation method on HIV-1 viral loadsa
| Sample no. | No. of RNA copies/mlb
|
||||||
|---|---|---|---|---|---|---|---|
| EDTA tube (plasma aliquot frozen)
|
PPT (plasma aliquot frozen)
|
PPT (plasma frozen in situ)
|
|||||
| ULTRA | STD | B-DNA | ULTRA | STD | ULTRA | STD | |
| 1 | <50 (ND) | <400 (ND) | <75 | <50 (ND) | <400 (ND) | <50 (D) | <400 (D) |
| 2 | <50 (ND) | <400 (ND) | <75 | <50 (ND) | <400 (ND) | <50 (D) | 1,500 |
| 3 | <50 (ND) | <400 (ND) | <75 | <50 (D) | <400 (ND) | <50 (D) | 650 |
| 4 | <50 (ND) | <400 (ND) | <75 | <50 (ND) | <400 (ND) | <50 (ND) | 450 |
| 5 | <50 (ND) | <400 (ND) | <75 | <50 (D) | <400 (ND) | <50 (ND) | 1,000 |
| 6 | <50 (ND) | <400 (ND) | <75 | <50 (D) | <400 (ND) | <50 (D) | <400 (ND) |
| 7 | <50 (ND) | <400 (ND) | <75 | <50 (D) | <400 (ND) | 80 | 750 |
| 8 | <50 (ND) | <400 (ND) | <75 | <50 (D) | <400 (ND) | <50 (ND) | <400 (ND) |
| 9 | 15,000 | 20,000 | 10,000 | 25,000 | 35,000 | 20,000 | 70,000 |
| 10 | <50 (D) | <400 (ND) | <75 | <50 (D) | <400 (ND) | 65 | 3,500 |
| 11 | <50 (D) | <400 (ND) | <75 | <50 (D) | <400 (ND) | <50 (D) | <400 (ND) |
| 12 | <50 (D) | <400 (ND) | <75 | <50 (ND) | <400 (ND) | <50 (ND) | <400 (ND) |
| 13 | <50 (ND) | <400 (ND) | <75 | <50 (ND) | <400 (ND) | 600 | 5,500 |
Determined by the Roche standard (STD) and ultrasensitive (ULTRA) assays and the B-DNA assay.
For details of specimen handling, see Results. Bold type indicates discordant results. ND, no viral RNA detected. D, viral RNA detected but below the linear range of the assay.
Effect of handling of PPT on viral load results.
Several factors made us suspect that freezing PPT might cause the discordant results. Among these were the nearly contemporaneous reports that the PPT could not be used for certain hepatitis assays, a suggestion from Cheryl Jennings of Rush Medical Center and the Viral Quality Assurance Laboratory, and information from Roche that they could reproduce our discrepant results with our specimens but not with those from a collaborating laboratory. To test our hypothesis, we drew two blood specimens each from 13 patients for viral load testing: one specimen for testing with an EDTA tube and one for testing with a PPT. Within 2 h of collection, the EDTA specimen was centrifuged for 20 min at 1,100 × g. The plasma was frozen in two aliquots, one of which was sent to a reference laboratory for B-DNA testing. The PPT was centrifuged according to our usual protocol. Plasma (850 μl) was removed and frozen in a transfer tube; the remainder was frozen in situ in the PPT. On the day of testing, each of the three specimens was thawed at room temperature and tested by the standard and ultrasensitive assays. The results are shown in Table 2. Columns 2 to 4 show the results obtained with plasma from the lavender-topped EDTA tube, including the B-DNA results. Columns 5 and 6 show the results from the plasma aliquot frozen in a transfer tube after removal from the centrifuged PPT. The results from the PPT plasma frozen in the aliquot tube are concordant with each other, with the B-DNA results, and with the lavender-topped EDTA results. Twelve of the 13 specimens exhibited viral loads below the linear range of all assays. Columns 7 and 8 show the standard and ultrasensitive results obtained from the plasma frozen in situ in the PPT. Eight of the 13 viral loads determined from plasma frozen in the PPT were discordant (denoted by bold type). For seven of these results, the standard viral load increased from <400 (none detected) to between 450 and 3,500 RNA copies/ml. In addition, three specimens with ultrasensitive results below the linear range in the first two test conditions were elevated to within the linear range (65, 80, and 600 RNA copies/ml) after being frozen in situ. Sample no. 13 had results of 600 and 5,500 RNA copies/ml in the ultrasensitive and standard assays, respectively, when assays were performed on plasma frozen in situ; the other assays done with this specimen detected no viral RNAs. Freezing patient plasma in situ in PPT can cause elevations in both the standard and ultrasensitive viral loads determined for that plasma. Increases in viral loads caused by freezing plasma in PPT are more numerous and larger in the standard assay, but the change in ultrasensitive results may also be clinically relevant.
DISCUSSION
Freezing plasma samples in the PPT in which they are collected elevates artifactually the results of the standard viral load assay but has less effect on the ultrasensitive results. At low viral loads, the standard results may exceed the ultrasensitive results by 100-fold or more. Overall, about 18% of the specimens received during this study were discordant, and specimens from children had a significantly higher rate of discordant results than those from adults. We do not know why only some specimens were discordant or why pediatric patients differed significantly from the adult patients in the proportion of discordant specimens. These questions are under investigation.
Whatever unknown factors contribute to the discordant results, the discrepancies can be eliminated if plasma specimens collected in PPT are transferred to a second tube after centrifugation but prior to freezing. We assume that freezing the PPT releases nonparticulate HIV-1 genetic material from cells in or below the separator gel into the overlying plasma. Since the viral load assay employs reverse transcriptase PCR technology, it can amplify any virus-specific template, either DNA or RNA, that may be present. A recent study by the Viral Quality Assurance Laboratory (NO1-AI-85354) determined that a single copy of HIV-1-specific proviral DNA could increase the detected viral load by 100 to 200 RNA copies (Cheryl Jennings [Rush Medical Center], personal communication).
For the standard assay, nucleic acids are extracted directly from plasma samples, so any contaminating genetic material would be amplified. For the ultrasensitive assay, virions are sedimented from the plasma prior to nucleic acid extraction, apparently leaving the contaminating material in the supernatant fluid, which is discarded. If the amount of HIV genetic material released into the plasma were especially large, the viral load determined by the ultrasensitive assay could be falsely elevated by free HIV genetic material remaining in the small amount of plasma contaminating the viral pellet. This hypothesis may explain the higher ultrasensitive viral load results shown in Table 2, column 7 (frozen in the PPT) compared to column 5 (frozen in a transfer tube) and to the B-DNA results in column 4. It also could explain why 12.5% of the B-DNA results obtained for discordant specimens were also discordant with the ultrasensitive results. Thus, freezing plasma in the PPT is not acceptable, even if the ultrasensitive HIV-1 viral load assay is planned. Other results, not presented here, suggest that if specimens in PPT are markedly delayed in transit or otherwise mishandled, the standard assay results are similarly compromised relative to those of the ultrasensitive assay. With the agreement of our physicians, we have discontinued the standard assay and offer only the ultrasensitive assay.
One published paper (12), one recent poster (R. Murphy, B. Berzins, A. Leake, M. Till, V. Stosor, J. Stanton, and F. Palella, 12th Conference on Retroviruses and Opportunistic Infections, Boston, Mass., no. 738, 22 to 25 February 2005), and anecdotal reports indicate that others have noted the discrepancy between results obtained in EDTA and PPT but did not determine the cause. Our laboratory had some previous indications that viral load determinations were not accurate: failure to amplify viral RNA in the HIV genotyping assay sometimes occurred despite detected viral loads ranging from 1,000 to 5,000 copies/ml. Since we changed our specimen processing protocol for the viral load determinations, these genotyping failures no longer occur.
Previous papers showing that viral loads were not affected by freezing the PPT (7, 8) made PPT the collection method of choice for many laboratories. Since PPT became available prior to highly active antiretroviral therapy, most specimens used in the original validations (7, 8), and in our own as well, had viral loads greater than 10,000 genome copies per ml. The numeric difference between the discordant standard and ultrasensitive viral loads usually ranged from 350 to 10,000 RNA copies/ml. Only when highly effective antiretroviral therapy substantially reduced the viral load did a discrepancy of several hundred or even several thousand RNA copies/ml become meaningful.
Acknowledgments
We thank the technologists of the DMC University Laboratories Molecular Microbiology Laboratory for their patience, understanding, and support during the months of duplicate testing required until we eliminated the cause of the discrepant results. We thank Michael Kruger for performing the statistical analysis.
Roche Molecular Diagnostics paid for all duplicate testing without restriction on test type or location.
REFERENCES
- 1.Brambilla, D., P. S. Reichelderfer, J. W. Bremer, D. E. Shapiro, R. C. Hershow, D. A. Katzenstein, S. M. Hammer, B. Jackson, A. C. Collier, R. S. Sperling, M. G. Fowler, R. W. Coombs, et al. 1999. The contribution of assay variation and biological variation to the total variability of plasma HIV-1 RNA measurements. AIDS 13:2269-2279. [DOI] [PubMed] [Google Scholar]
- 2.Brambilla, D. J., C. Jennings, R. Morack, S. Granger, and J. W. Bremer. 2004. Comparison of the sensitivities of the version 1.5 and version 1.0 ultrasensitive Roche AMPLICOR HIV-1 MONITOR kits at low concentrations of human immunodeficiency virus RNA. J. Clin. Microbiol. 42:2819-2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brambilla, D. J., S. Granger, C. Jennings, and J. W. Bremer. 2001. Multisite comparison of reproducibility and recovery from the standard and ultrasensitive Roche AMPLICOR HIV-1 MONITOR assays. J. Clin. Microbiol. 39:1121-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coombs, R. W., S. L. Welles, C. Hooper, P. S. Reichelderfer, R. T. D'Aquila, A. J. Japour, V. A. Johnson, D. R. Kuritzkes, D. D. Richman, S. Kwok, J. Todd, J. B. Jackson, V. DeGruttola, C. S. Crumpacker, J. Kahn, et al. 1996. Association of plasma human immunodeficiency virus type 1 RNA level with risk of clinical progression in patients with advanced infection. J. Infect. Dis. 174:704-712. [DOI] [PubMed] [Google Scholar]
- 5.Erali, M., and D. R. Hillyard. 1999. Evaluation of the ultrasensitive Roche Amplicor HIV-1 Monitor assay for quantitation of human immunodeficiency virus type 1 RNA. J. Clin. Microbiol. 37:792-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill, C. E., A. M. Green, J. Ingersoll, K. A. Easley, F. S. Nolte, and A. M. Caliendo. 2004. Assessment of agreement between the AMPLICOR HIV-1 MONITOR test versions 1.0 and 1.5. J. Clin. Microbiol. 42:286-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holodniy, M., L. Mole, B. Yen-Lieberman, D. Margolis, C. Starkey, R. Carroll, T. Spahlinger, J. Todd, and J. B. Jackson. 1995. Comparative stabilities of quantitative human immunodeficiency virus RNA in plasma from samples collected in VACUTAINER CPT, VACUTAINER PPT, and standard VACUTAINER tubes. J. Clin. Microbiol. 33:1562-1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holodniy, M., L. Rainen, S. Herman, and B. Yen-Lieberman. 2000. Stability of plasma human immunodeficiency virus viral load in VACUTAINER PPT plasma preparation tubes during overnight shipment. J. Clin. Microbiol. 38:323-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson, L. B., E. Piwowar-Manning, L. Johnson-Lewis, R. Bassett, L. M. Demeter, and D. Brambilla. 2004. Comparisons of versions 1.0 and 1.5 of the UltraSensitive AMPLICOR HIV-1 MONITOR test for subjects with low viral load. J. Clin. Microbiol. 42:2774-2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NCCLS. 2003. Quantitative molecular methods for infectious diseases, p. 19-20. Approved standard MM6-A (ISBN 1-56238-508.9). NCCLS, Wayne, Pa.
- 11.O'Brien, W. A., P. M. Hartigan, D. Martin, J. Esinhart, A. Hill, S. Benoit, M. Rubin, M. S. Simberkoff, and J. D. Hamilton. 1996. Changes in plasma HIV-1 RNA and CD4+ lymphocyte counts and the risk of progression to AIDS. N. Engl. J. Med. 334:426-431. [DOI] [PubMed] [Google Scholar]
- 12.Squires, K., A. Lazzarin, J. M. Gatell, W. G. Powderly, V. Pokrovskiy, J.-F. Delfaissy, J. Jemsek, A. Rivero, W. Rozenbaum, S. Schrader, M. Sension, A. Vibhagool, A. Thiry, and M. Giordano. 2004. Comparison of once-daily atazanavir with efavirenz, each in combination with fixed-dose zidovudine and lamivudine, as initial therapy for patients infected with HIV. AIDS 36:1011-1019. [DOI] [PubMed] [Google Scholar]
- 13.Welles, S. L., J. B. Jackson, B. Yen-Lieberman, L. Demeter, A. J. Japour, L. M. Smeaton, V. A. Johnson, D. R. Kuritzkes, R. T. D'Aquila, P. A. Reichelderfer, D. D. Richman, R. Reichman, M. Fischl, R. Dolin, R. W. Coombs, J. O. Kahn, C. McLaren, J. Todd, S. Kwok, C. S. Crumpacker, et al. 1996. Prognostic value of plasma HIV-1 RNA levels in patients with advanced HIV-1 disease and with little or no zidovudine therapy. J. Infect. Dis. 174:696-703. [DOI] [PubMed] [Google Scholar]