Abstract
Human infective endocarditis due to Streptococcus suis occurs infrequently. The case of a 43-year-old male who sustained life-threatening infective endocarditis is reported. Since growth of S. suis on commonly used sheep blood agar plates resembles viridans streptococci, diagnosis of S. suis constitutes a diagnostic pitfall. Identification was accomplished by using molecular methods.
CASE REPORT
An otherwise healthy 43-year-old male complained of malaise, fever, dyspnea, and upper back pain. He was treated with nonsteroidal drugs. Twelve days later, he was found to have severe orthopnea. Electrocardiography revealed sinus tachycardia and a complete left bundle branch block. Finally, due to acute respiratory insufficiency, the patient was admitted to the hospital of the Justus-Liebig University Giessen, Giessen, Germany, after emergency intubation. Transesophageal echocardiography revealed severe aortic regurgitation, huge aortic valve vegetations, and a ventricular septal defect located immediately left of the membranous septum. Blood cultures were taken, and intravenous antibiotic treatment with ceftazidime (two doses of 2 g each), rifampin (one dose of 600 mg), and vancomycin (two doses of 1 g each) was initiated (leukocytes/μl, 43,800; C-reactive protein, 189.7 mg/liter; body temperature, 38.5°C). The patient subsequently underwent emergency surgery consisting of aortic root debridement, aortic valve replacement with a 23-mm mechanical heart valve, and sealing of the ventricular septal defect by use of autologous pericardium. The perioperative and postoperative courses were uneventful. The patient was extubated 6 h after surgery, discharged home 10 days later, and prescribed a 6-week ambulatory intravenous antibiotic treatment. The 15-month follow-up was without complications: neither reinfection- nor valve-related events were noted, and clinical parameters were within normal ranges (leukocytes/μl, 8,300; C-reactive protein, <4 mg/liter; body temperature, 37°C). The patient resumed his job without restriction.
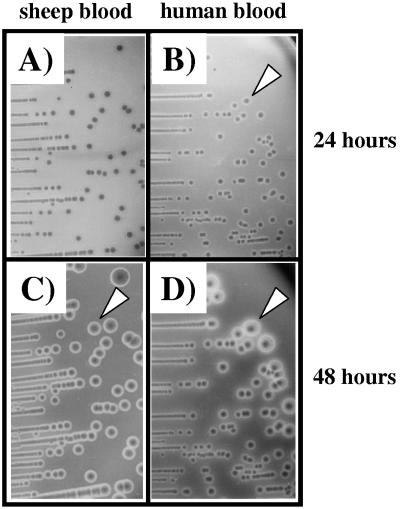
Both the inoculated blood cultures and the aortic valve revealed a pure culture of viridans streptococci after 24 h of cultivation on sheep blood agar plates in an atmosphere of 5% CO2. At 48 h, the bacterial colonies showed a very small zone of beta-hemolysis (Fig. 1). A commercial system for the phenotypic identification of gram-positive bacteria, the BBL Crystal gram-positive ID kit (Becton-Dickinson, Heidelberg, Germany), revealed Streptococcus bovis, which is a non-beta-hemolytic bacterium. To achieve taxonomic certainty, we amplified the 16S rRNA gene of this isolate with primers 63F (5′-CAG GCC TAA CAC ATG CAA GTC-3′) and 1220R (5′-TTG TAG CAC GTG TGT AGC CC-3′), and the nucleic acid sequence of the amplicon was determined with the DNA sequencing system MegaBACE 1000 (Molecular Dynamics, GE Healthcare, Uppsala, Sweden) by using the same primers. Sequence comparisons (GenBank database, National Center for Biotechnology Information, Bethesda, Md.) revealed the strain to be the closely related species Streptococcus suis, which was further confirmed by suilysin- and capsule-specific PCR (12, 20). Unfortunately, the BBL Crystal gram-positive ID kit did not identify S. suis, since this animal pathogen, apart from S. bovis, was not represented in its database, which is dominated by human pathogens (identification scheme manual; Becton-Dickinson). The MICs of the S. suis isolate for ceftazidime (0.25 μg/ml), rifampin (0.016 μg/ml), and vancomycin (0.75 μg/ml) were determined by using a commercially available epsilometer test (Etest; AB Biodisk, Solna, Sweden) as recommended by the vendor.
FIG. 1.
S. suis isolate grown on sheep and human blood agar plates at 37°C in the presence of 5% CO2. After 24 h of incubation, small colonies are visible, which appear as alpha-hemolytic viridans streptococci on sheep blood agar plates (A) and as beta-hemolytic streptococci with a clear halo of hemolysis around the colonies on human blood agar plates (B). After prolonged incubation for 48 h, large colonies are visible with clear beta-hemolysis on both sheep (C) and human (D) blood agar plates. Hemolysis after prolonged incubation is more pronounced. Arrowheads indicate beta-hemolysis.
The rapid and destructive progression of the disease was obviously caused by a highly virulent strain of S. suis. A serotype-specific PCR indicated that the isolate was either an S. suis serotype 2 or an S. suis serotype 1/2 strain. This finding was achieved by detecting the capsular gene cps2J present in the capsular biosynthesis locus of S. suis serotypes 2 and 1/2 (20). To verify this data, serotyping of the S. suis isolate was also performed using a slide agglutination test method with rabbit antiserum, raised against the reference strains of S. suis (29). Agglutination identified the isolate clearly as belonging to serotype 2.
Discussion.
Streptococcus suis, a gram-positive, facultatively anaerobic coccus, is the causative agent of a wide range of clinical disease syndromes occurring mainly in swine and infrequently in humans. The clinical symptoms caused in swine include arthritis, meningitis, pneumonia, septicemia, endocarditis, abortions, and abscesses (12). In occupationally exposed persons, virulent strains of S. suis can cause purulent meningitis, septicemia, and endocarditis, which are commonly fulminant and often fatal (17, 21).
The most important virulence factor is the capsular polysaccharide of S. suis serotype 2 that is required for protection of the bacterium against phagocytosis (19). The predominant serotype causing infections in humans is serotype 2, with a few clinical cases being reported for serotypes 1 and 14 (20). Based on capsular antigens, 35 serotypes have been described but a substantial number of nontypeable strains exists (8, 29). Another virulence factor associated with high virulence in serotype 2 strains is the pore-forming hemolysin suilysin, which is present in approximately 70% of various serotypes of S. suis isolates (10, 12). It is a member of the family of thiol-activated, cholesterol-binding, and pore-forming cytolysins (12, 14). Although the knowledge of virulence factors of S. suis isolates is limited, additional potential candidate factors have been described (1, 6, 7, 10, 12, 23, 26, 28).
S. suis endocarditis in humans is a rare presentation worldwide, and only a few cases have been reported in the literature (3, 4, 9, 11, 15, 22, 24, 27). Infection with S. suis typically occurs via skin injuries, and in particular, farmers and workers involved in pork production are at risk. It is a known occupational disease occurring in people exposed to pigs or unprocessed pork (16). A detailed anamnesis of the patient disclosed that he was employed as a butcher in a slaughterhouse where only pigs were slaughtered. He occasionally removed abscesses from slaughtered pigs, and as a result, small skin lesions were inevitable during his work. Moreover, examination of his skin revealed that he suffered from very dry skin and fissured hands. A likely explanation for the fulminant and life-threatening disease was that an S. suis serotype 2 isolate derived from an infected pig entered the bloodstream of the patient via skin fissures or small lesions on his hands. Anamnestic reconstruction suggested that the microorganism disseminated very rapidly and destroyed his aortic valve and the ventricular septum within 10 to 14 days postinfection. The S. suis isolate was highly susceptible to the antibiotics used for treatment, and the patient responded very well and recovered rapidly after surgery.
Since growth of S. suis on sheep blood agar plates commonly used in routine diagnostic laboratories resembles viridans streptococci, diagnosis of S. suis constitutes a diagnostic pitfall. First, approximately 30% of all S. suis isolates harbor no suilysin and are therefore not beta-hemolytic. These isolates show alpha-hemolysis. Second, lysis of erythrocytes by suilysin depends on the origin of the red blood cells used. Human erythrocytes are the most susceptible, followed by horse, sheep, cow, and pig erythrocytes (5). Almost all isolates of S. suis are alpha-hemolytic on sheep blood agar plates and develop beta-hemolysis, if at all, only after prolonged incubation (17). Since sheep blood is the commonly used blood with agar plates for diagnosis, S. suis isolates (despite suilysin expression) resemble viridans streptococci after 24 h of incubation. Inoculation of the most susceptible human blood agar plates showed that the S. suis isolate was beta-hemolytic after 24 h and that the hemolytic zone was more pronounced after a prolonged incubation of 48 h (Fig. 1). The presence of the suilysin gene was confirmed by employing a suilysin-specific PCR (12).
To confirm that the hemolytic activity observed was indeed due to suilysin of the S. suis isolate, the gene was heterologously expressed in the nonpathogenic gram-positive bacterium Listeria innocua. The entire gene was cloned into vector pSOG 34 (13) by using the primers sly-F SpeI (5′-CTC TCC TAA CTA GTT TTT AAT AGG-3′) and sly-R XhoI (5′-AGT TTC TCG AGA ATA GTG TTT AGC-3′) (recognition sites of restriction endonucleases are underlined). The suilysin gene was inserted into the unique SpeI and XhoI restriction sites of vector pSOG 34. The plasmid was transformed to generate the recombinant strain L. innocua(pSOG::sly) as described previously (18).
The expression levels of suilysin in S. suis and in the recombinant strain L. innocua(pSOG::sly) were monitored by using cytotoxic and hemolytic assays as described previously (2). The cytotoxic activity assay performed with Vero cells (African green monkey kidney cells) and the cell proliferation reagent WST-1, as recommended by the vendor (Roche Diagnostics, Mannheim, Germany), showed that bacterium-free supernatants of overnight cultures of S. suis and L. innocua(pSOG::sly) lysed the host cells within 3 hours. The hemolytic activity determined using human erythrocytes was 32 hemolytic U for both S. suis and L. innocua(pSOG::sly). The suilysin-negative strain L. innocua(pSOG) was neither hemolytic nor demonstrably cytotoxic.
We also detected suilysin in the supernatants of S. suis and L. innocua recombinant strains by employing a rabbit polyclonal antiserum raised against the conserved undecapeptide of listeriolysin, as specified previously (2). The polyclonal antiserum showed cross-reactivity with suilysin, and the toxin was detectable in the culture supernatants of both S. suis and L. innocua(pSOG::sly), with a calculated size of ∼55 kDa. The negative control strain L. innocua(pSOG) expressed no suilysin. Transfer of the gene encoding suilysin to a nonhemolytic L. innocua strain imparted both novel hemolytic and cytotoxic properties to the recombinant strain.
The destructive case of infective endocarditis with a fulminant course described here and similar cases caused by S. suis serotype 2 strains are very typical for acute endocarditis caused by bacteria of high virulence potential, such as Staphylococcus aureus, Streptococcus pyogenes, Streptococcus pneumoniae, Enterococcus species, or Enterobacteriaceae. Typical symptoms include high fever, leukocytosis, a high degree of aortic valve insufficiency, and generally a ventricular septal defect. Death occurs in several days to less than 6 weeks. On the other hand, viridans streptococci usually cause subacute or chronic endocarditis, a condition also called endocarditis lenta. Here the degree of valvular destruction may also be extensive, but infection occurs with a less acute onset of symptoms, with a low-grade fever, usually involving weeks to months, and with lower mortality (4, 25).
Since S. suis infection is a known occupational disease occurring in people with close contact to pigs or unprocessed pork, care to avoid generating skin lesions during meat processing procedures should be taken. The clear identification of S. suis as the causative agent of infective endocarditis enabled the appreciation of the infection as an occupational disease.
The data presented here endorse the use of molecular techniques in identifying unsuspected human, animal, and plant pathogens as well as environmental bacteria in clinical laboratories. Since animal, plant, and environmental bacteria are rarely included on commercial panels used for the identification of clinical isolates, only unusual properties and additional tests may reveal the true nature of the pathogen. With the growing rate of immunocompromised individuals and elderly populations, comprehensive and objective methods to monitor and identify atypical pathogens and their virulence potential are a matter of great consequence.
Acknowledgments
We thank Martina Leyerer and Sylvia Krämer for excellent technical assistance and Henk J. Wisselink (DLO-Institute for Animal Science and Health, Lelystad, The Netherlands) for serotyping the S. suis isolate.
This work was supported by grants from the Bundesministerium für Bildung und Forschung, Germany, within the framework of the National Genome Research Network (NGFN) (contract no. 01GS0401).
REFERENCES
- 1.Benga, L., R. Goethe, M. Rohde, and P. Valentin-Weigand. 2004. Non-encapsulated strains reveal novel insights in invasion and survival of Streptococcus suis in epithelial cells. Cell. Microbiol. 6:867-881. [DOI] [PubMed] [Google Scholar]
- 2.Darji, A., T. Chakraborty, K. Niebuhr, N. Tsonis, J. Wehland, and S. Weiss. 1995. Hyperexpression of listeriolysin in the nonpathogenic species Listeria innocua and high yield purification. J. Biotechnol. 43:205-212. [DOI] [PubMed] [Google Scholar]
- 3.Donsukal, K., C. Dejthevaporn, and R. Witoonpanich. 2003. Streptococcus suis infection: clinical features and diagnostic pitfalls. Southeast Asian J. Trop. Med. Public Health 34:154-158. [PubMed] [Google Scholar]
- 4.Fowler, V. G., W. M. Scheld, and A. S. Bayer. 2005. Endocarditis and intravascular infections, p. 975-1022. In G. L. Mandell, J. E. Bennett, and R. Dolin (ed.), Mandell, Douglas, and Bennett's principles and practice of infectious diseases, 6th ed. Elsevier Churchill Livingstone, Philadelphia, Pa.
- 5.Gottschalk, M., S. Lacouture, and J. D. Dubreuil. 1995. Characterization of Streptococcus suis capsular type 2 haemolysin. Microbiology 141:189-195. [DOI] [PubMed] [Google Scholar]
- 6.Gottschalk, M., and M. Segura. 2000. The pathogenesis of the meningitis caused by Streptococcus suis: the unresolved questions. Vet. Microbiol. 76:259-272. [DOI] [PubMed] [Google Scholar]
- 7.Haataja, S., K. Tikkanen, J. Liukkonen, C. Francois-Gerard, and J. Finne. 1993. Characterisation of a novel bacterial adhesion specificity of Streptococcus suis recognizing blood group P receptor oligosaccharides. J. Biol. Chem. 268:4311-4317. [PubMed] [Google Scholar]
- 8.Higgins, R., M. Gottschalk, M. Boudreau, A. Lebrun, and J. Henricson. 1995. Description of six new capsular types (28 through 34) of Streptococcus suis. J. Vet. Diagn. Investig. 7:405-406. [DOI] [PubMed] [Google Scholar]
- 9.Ho, A. K., K. S. Woo, K. K. Tse, and G. L. French. 1990. Infective endocarditis caused by Streptococcus suis serotype 2. J. Infect. 21:209-211. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs, A. A. C., P. L. W. Loeffen, A. J. G. van den Berg, and P. K. Storm. 1994. Identification, purification, and characterization of a thiol-activated hemolysin (suilysin) of Streptococcus suis. Infect. Immun. 62:1742-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kay, R., A. F. Cheng, and C. Y. Tse. 1995. Streptococcus suis infection in Hong Kong. QJM 88:39-47. [PubMed] [Google Scholar]
- 12.King, S. J., P. J. Heath, I. Luque, C. Tarradas, C. G. Dowson, and A. M. Whatmore. 2001. Distribution and genetic diversity of suilysin in Streptococcus suis isolated from different diseases of pigs and characterization of the genetic basis of suilysin absence. Infect. Immun. 69:7572-7582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otten, S. 2001. Characterization and identification of preferentially expressed intracellular genes of Listeria monocytogenes. Ph.D. thesis. Justus-Liebig-University Giessen, Giessen, Germany.
- 14.Pamer, M. 2001. The family of thiol-activated, cholesterol-binding cytolysins. Toxicon 39:1681-1689. [DOI] [PubMed] [Google Scholar]
- 15.Peetermans, W. E., B. G. Moffie, and J. Thompson. 1989. Bacterial endocarditis caused by Streptococcus suis type 2. J. Infect. Dis. 159:595-596. [DOI] [PubMed] [Google Scholar]
- 16.Robertson, I. D., and D. K. Blackmore. 1989. Occupational exposure to Streptococcus suis type 2. Rev. Infect. Dis. 101:1102-1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruoff, K. L., R. A. Whiley, and D. Beighton. 2003. Streptococcus, p. 405-421. In P. R. Murray, E. J. Baron, M. A. Pfaller, J. H. Jorgenson, and R. H. Yolken (ed.), Manual of clinical microbiology, 8th ed. ASM Press, Washington, D.C.
- 18.Schäferkordt, S., E. Domann, and T. Chakraborty. 1998. Molecular approaches for the study of Listeria, p. 421-431. In P. Williams, J. Ketley, and G. Salmond (ed.), Bacterial pathogenesis: methods in microbiology, vol. 27. Academic Press, San Diego, Calif.
- 19.Smith, H. E., M. Damman, J. van der Velde, F. Wagenaar, H. J. Wisselink, N. Stockhofe-Zurwieden, and M. A. Smits. 1999. Identification and characterization of the cps locus of Streptococcus suis serotype 2: the capsule protects against phagocytosis and is an important virulence factor. Infect. Immun. 67:1750-1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith, H. E., V. Veenbergen, J. van der Velde, M. Damman, H. J. Wisselink, and M. A. Smits. 1999. The cps genes of Streptococcus suis serotypes 1, 2, and 9: development of rapid serotype-specific PCR assays. J. Clin. Microbiol. 37:3146-3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staats, J. J., I. Feder, O. Okwumabu, and M. M. Chengappa. 1997. Streptococcus suis: past and present. Vet. Res. Commun. 21:381-407. [DOI] [PubMed] [Google Scholar]
- 22.Tayoro, J., J. M. Besnier, P. Laudat, B. Cattier, and P. Choutet. 1996. Infective endocarditis due to Streptococcus suis serotype 2. Eur. J. Clin. Microbiol. Infect. Dis. 15:765-766. [DOI] [PubMed] [Google Scholar]
- 23.Tikkanen, K., S. Haataja, and J. Finne. 1996. The galactosyl-(α1-4)-galactose-binding adhesin of Streptococcus suis: occurrence in strains of different hemagglutination activities and induction of opsonic antibodies. Infect. Immun. 64:3659-3665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trottier, S., R. Higgins, G. Brochu, and M. Gottschalk. 1991. A case of human endocarditis due to Streptococcus suis in North America. Rev. Infect. Dis. 13:1251-1252. [DOI] [PubMed] [Google Scholar]
- 25.Truninger, K., C. H. Attenhofer Jost, B. Seifert, P. R. Vogt, F. Follath, A. Schaffner, and R. Jenni. 1999. Long term follow up of prosthetic valve endocarditis: what characteristics identify patients who were treated successfully with antibiotics alone? Heart 82:714-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vecht, U., H. J. Wisselink, M. L. Jellema, and H. E. Smith. 1991. Identification of two proteins associated with virulence of Streptococcus suis type 2. Infect. Immun. 59:3156-3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vilaichone, R. K., W. Vilaichone, P. Nunthapisud, and H. Wilde. 2002. Streptococcus suis infection in Thailand. J. Med. Assoc. Thail. 85(Suppl. 1):S109-S117. [PubMed] [Google Scholar]
- 28.Winterhoff, N., R. Goethe, P. Gruening, M. Rohde, H. Kalisz, H. E. Smith, and P. Valentin-Weigand. 2002. Identification and characterization of two temperature-induced surface-associated proteins of Streptococcus suis with high homologies to members of the arginine deiminase system of Streptococcus pyogenes. J. Bacteriol. 184:6768-6776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wisselink, H. J., H. E. Smith, N. Stockhofe-Zurwieden, K. Peperkamp, and U. Vecht. 2000. Distribution of capsular types and production of muraminidase-released protein (MRP) and extracellular factor (EF) of Streptococcus suis strains isolated from diseased pigs in seven European countries. Vet. Microbiol. 74:237-248. [DOI] [PubMed] [Google Scholar]