Abstract
Human coronavirus NL63 (HCoV-NL63), a newly discovered coronavirus, has been associated with acute respiratory tract infections (ARI). Important questions pertaining to the contribution of HCoV-NL63 to ARI and its impact on public health remain. We reviewed HCoV-NL63 in specimens collected from 13 November 2002 to 31 December 2003 from the Stollery Children's Hospital on patients of <17 years of age to assess the role of this virus in ARI in children. Twenty-six of 1,240 specimens (2.1%) from seven outpatients and 19 inpatients aged 7 days to 9.5 years tested positive for HCoV-NL63 by reverse transcription-PCR. The majority of outpatients (86%) had upper respiratory tract infections, while the majority of inpatients (58%) had bronchiolitis. Peak HCoV-NL63 activity occurred in March. These results provide further evidence of the importance of HCoV-NL63 in ARI in children.
Acute respiratory illnesses (ARI) are a major health problem in people of all ages. They represent the leading cause of death from infectious disease in Canada and exert a great economic burden on the health care system (7). The viruses most frequently associated with respiratory tract infections include rhinoviruses, coronaviruses, influenza viruses, parainfluenza viruses, respiratory syncytial viruses (RSV), and adenoviruses. In children, RSV is the leading cause of ARI resulting in hospitalization (9, 13). More recently, human metapneumovirus virus (hMPV) has also been identified as an important respiratory pathogen in children (14). In 2004, a new human coronavirus (HCoV), NL63 (HCoV-NL63), was identified in clinical specimens from both infants and adults with ARI in The Netherlands (15). The virus was also identified in Canada, Australia, Belgium, China, and Japan, providing evidence for the worldwide distribution of HCoV-NL63 (1-4, 12, 15). Other HCoVs have been associated with respiratory illnesses (8). The most common, HCoV-229E and HCoV-OC43, are responsible for up 30% of the common cold syndrome in certain populations. Recently, a novel coronavirus, HCoV-severe acute respiratory syndrome, has been associated with severe atypical pneumonia and caused 774 deaths worldwide from November 2002 to July 2003 (16). Sequence analyses of the complete genome of HCoV-NL63 revealed that the virus is more closely related to HCoV-229E than to the other human coronaviruses (15). Preliminary data suggested that HCoV-NL63 may be an important respiratory tract pathogen in children, similarly to RSV and hMPV (2, 3, 5, 12, 15). In this study, we looked for HCoV-NL63 in patients with ARI to assess the impact of HCoV-NL63 infections on respiratory tract illnesses and to describe the clinical course of this illness in children.
MATERIALS AND METHODS
Specimens.
Detection of HCoV-NL63 was performed in nasopharyngeal (NP) aspirates or swabs that were submitted to the Provincial Laboratory for Public Health (Microbiology), northern Alberta, from 13 November 2002 to 31 December 2003 from the Stollery Children's Hospital outpatient clinics, emergency department, or inpatient wards from patients of <17 years of age for the detection of respiratory viruses. Respiratory viral tests were performed on specimens according to laboratory test algorithms; these tests included direct fluorescent antibody tests for RSV, parainfluenza virus, and influenza A and B viruses (Imagen; DakoCytomation Ltd.); rapid respiratory virus plate culturing; and traditional viral culturing. Specimens that tested negative for RSV, parainfluenza virus, influenza A and B viruses, and adenovirus were then tested for HCoV-NL63, unless the volumes of the specimens were inadequate. A small number of specimens that tested positive for human RSV (n = 39), hMPV (n = 42), or parainfluenza virus (n = 1) were also tested for HCoV-NL63. In the analysis of the monthly incidence of respiratory virus infection, specimens collected from the same patient with an identical virus isolated within a 10-day period were considered as duplicates.
Clinical data review and statistical analysis.
Inpatient and outpatient charts were reviewed for all children who tested positive for HCoV-NL63. The children's ages, genders, underlying medical conditions, symptoms, signs, and investigative results and details of the treatments offered were recorded. For hospitalized children, the durations and heights of fevers, need for oxygen, and durations of hospitalization were also recorded.
Primer sequences.
The primers used for amplification and sequencing were based on the published HCoV-NL63 genome sequence (AF371367) (15). Primers 730 (147-AGATGAGCAGATTGGTTATTGG-168) and 731 (491-GAAGAGTCTCGTGAGTTGTTAC-470), based on the sequence of the nucleocapsid gene, were designed using BEACON software and used for the diagnosis of HCoV-NL63. The primer set SS5852-5Pf-(5777) 5′-CTTTTGATAACGGTCACTATG-3′ and P4G1M-5-3Pr-(6616) 5′-CTCATTACATAAAACATCAAACGG-3′, described in the 2004 work of van der Hoek et al. and based on the sequence of the 1a gene, was used for confirmatory purposes and sequence analysis (15).
RT-PCR and sequence analysis.
Reverse transcription-PCR (RT-PCR) was performed as previously described (2). Briefly, viral RNA was extracted from original samples or tissue culture fluid using an RNeasy Mini kit (QIAGEN) or a QIAGEN QIAamp virus BioRobot MDx kit. Viral RNA was amplified in a one-step RT-PCR (QIAGEN) following the manufacturer's recommendations. In short, 5 μl of RNA was added to the RT-PCR mixture containing 2 μl QIAGEN OneStep RT-PCR enzyme mix, 10 μl of 5× QIAGEN OneStep RT-PCR buffer, 400 μM deoxynucleoside triphosphate, 0.6 μM of each primer, and 10 μl of Q solution in a final volume of 50 μl. The thermocycler conditions used were as follows: 50°C for 30 min for reverse transcription; 95°C for 15 min for the activation of the HotStart DNA polymerase; and then 50 cycles of 95°C for 30 sec, 50°C for 1 min, 72°C for 30 sec, followed by an extension of 10 min at 72°C. The PCR products were purified using a QIAquick PCR purification kit (QIAGEN) and sequenced on an ABI 377 sequencer by using a fluorescent dye-terminator kit (Applied Biosystems). The DNA sequences were assembled and analyzed with the SEQMAN, EDITSEQ, and MEGALIGN programs in the Lasergene program (DNASTAR, Madison, WI). Phylogenetic trees were generated by the neighbor-joining method using the MEGA2 program (10).
Nucleotide sequence database accession numbers.
The HCoV-NL63 sequences described in this paper have been deposited in GenBank under accession numbers DQ106888 to DQ106901. The nucleotide sequence database accession numbers for the following previously reported HCoV-NL63 isolates are in parentheses: the Dutch isolates (AY567487 to AY567494), the Australian isolates (AY746451 to AY746458), the Belgian isolates (AY758283 to AY758289), and the Canadian isolates (AY675541 to AY675553).
RESULTS
HcoV-NL63 detection and clinical data.
After removing 29 duplicate positive specimens, 581 specimens submitted during the study period had identifiable viruses, including 36 with adenovirus, 176 with influenza A virus, 30 with influenza B virus, 105 with parainfluenza virus, 217 with RSV, 9 with enterovirus, and 8 with herpes simplex virus. Of the 2,011 specimens that had tested negative with direct fluorescent antibody and culturing, 1,240 (61.7%) were available for the testing of HCoV-NL63, with the percent specimen tested per month ranging from 39.0% to 82.8%. HCoV-NL63 was detected in 26 of 1,240 NP specimens (2.1%). One of the 42 specimens that had tested positive for hMPV was also found to be positive for HCoV-NL63. The 39 specimens from which RSV had been detected and the 1 specimen that had tested positive for parainfluenza virus were negative for HCoV-NL63. Most of the HCoV-NL63 specimens were identified in February and March (7 and 12 specimens, respectively; 26.9% and 46.2%, respectively), and no HCoV-NL63 was found from August to November (Fig. 1). Patients with HCoV-NL63 were aged from 7 days to 9.5 years, with the majority being less than 1 year old (n = 17; 65.4%) (Table 1). The sex distribution was 65% (n = 17) male and 35% (n = 9) female (Table 1). HCoV-NL63 was detected in NP specimens from seven outpatients (five seen in the emergency department and two in an outpatient clinic, with two of these patients having repeat outpatient visits) and 19 inpatients (Table 1). The main symptoms on presentation were cough (n = 14; 54%), rhinitis (n = 8; 31%), and fever (n = 8; 31%).
FIG. 1.
Number of specimens and percentage positive for HCoV-NL63 per month.
TABLE 1.
Symptoms and medical history of patients infected with HCoV-NL63
| Patient group | Patient no. | Specimen no. | Sexa | Age (yr) | Medical historyb | ARI symptoms on presentation | Respiratory diagnosis |
|---|---|---|---|---|---|---|---|
| Outpatients | 1 | 452-03 | M | 0.18 | None | Paroxysmal cough | URTI |
| 2 | 315-03 | F | 6.33 | Prematurity (29 weeks gestational age), RAD | Bronchospasm, cough, fever, decreased intake | Exacerbation of RAD | |
| 3 | 306-03 | F | 0.07 | None | Cough, rhinitis | URTI | |
| 4 | 188-03 | M | 1.33 | None | Cough, rhinitis | URTI | |
| 5 | 457-03 | M | 0.09 | None | Vomiting, cough, rhinitis | URTI | |
| 6 | 368-03 | F | 0.07 | Prematurity (36 weeks gestational age) | Rhinitis, decreased feeding | URTI | |
| 7 | 305-03 | F | 0.34 | Prematurity (33 weeks gestational age), gastroschisis | Not recorded (tested at regular checkup) | URTI | |
| Inpatients with primary diagnoses of nonrespiratory problems | 8 | 377-03 | M | 0.93 | Congenital heart disease, prematurity (32 weeks gestational age), Down's syndrome | Bronchospasm while being ventilated following cardiac surgery | Bronchiolitis |
| 9 | 631-03 | M | 1.83 | Hemophilia | Rhinitis | URTI | |
| 10 | 500-03 | F | 0.33 | Short gut | Fever, desaturation | Bronchiolitis | |
| 11 | 372-03 | M | 2.0 | Global developmental delay, seizures, Arnold Chiari malformation | Cough, retching | URTI | |
| 12 | 301-03 | M | 0.67 | Congenital heart disease, aspiration, diaphragmatic eventration, pulmonary hypoplasia, global developmental delay | Fever, tachypnea | Bronchiolitis | |
| 13 | 435-03 | M | 0.33 | Congenital heart disease, cleft palate, hydronephrosis, diaphragmatic eventration, aspiration | Rhinitis | URTI, acute otitis media | |
| 14 | 303-03 | M | 8.9 | G6PD deficiency | Cough, pharyngitis | URTI | |
| Inpatients with primary diagnoses of respiratory problems | 15 | 581-03 | F | 0.58 | None | Fever, cough, tachypnea | Pneumonia with empyema due to pneumococcus |
| 16 | 410-03 | M | 0.10 | Drug withdrawal | Cough, rhinitis | Bronchiolitis | |
| 17 | 303-02 | F | 0.93 | None | Fever, rhinitis, tachypnea | Bronchiolitis, acute otitis media | |
| 18 | 446-03 | M | 0.67 | Laryngeal cyst | Stridor, fever | Laryngotracheobronchitis | |
| 19 | 309-03 | M | 1.42 | None | Cough, rhinitis | Bronchiolitis | |
| 20 | 460-03 | F | 1.08 | Prematurity (33 weeks gestational age), congenital heart disease, aspiration | Cough, fever | Bronchiolitis | |
| 21 | 257-03 | M | 0.09 | TEF (H type) | Cough, dyspnea | Bronchiolitis, acute otitis media | |
| 22 | 311-03 | M | 0.02 | None | Tachypnea, rhinitis | Bronchiolitis | |
| 23 | 394-03 | M | 5.42 | Dysfunctional cilia, global developmental delay | Cough, dyspnea | Bronchiolitis | |
| 24 | 415-03 | F | 0.14 | VACTERL syndrome, congenital heart disease | Cough, desaturations | Bronchiolitis | |
| 25 | 313-03 | M | 9.5 | RAD | Cough, pharyngitis, rash, wheeze | Exacerbation of RAD | |
| 26 | 316-03 | M | 0.5 | Prader-Willi syndrome, GERD, aspiration | Fever, tachypnea | Pneumoniac |
M, male; F, female.
G6PD, glucose-6-phosphate dehydrogenase; TEF, tracheoesophageal fistula; VACTERL, vertebral-anal-cardiac-tracheal-esophageal-renal-limb; GERD, gastroesophageal reflux disease.
Physician attributed pneumonia to aspiration.
Six of the seven outpatients with HCoV-NL63 infection had evidence of upper respiratory tract infections (URTI), and only one patient had a mild exacerbation of reactive airway disease (RAD) (Table 1). Three of these patients were born prematurely. Only the patient with RAD exacerbation had a documented temperature above 38.0°C. Chest radiography was performed only on the patient with RAD exacerbation, and the result was reported as normal. Medications were not prescribed for any of these patients. Of the 19 inpatients, 7 were admitted with primary diagnoses of nonrespiratory problems, and NP specimens were obtained according to our infection control protocol upon admission (n = 3) or during the admission (n = 5) when they showed symptoms of ARI (Table 1). Four of these seven patients had evidence of URTI, while only three had clinical or radiological evidence of bronchiolitis. Four of these seven patients could have acquired HCoV-NL63 nosocomially: patients #10 and #12 had been hospitalized for >14 days before the NP specimens were collected and HCoV-NL63 was detected, patient #8 had been in hospital for 4 days, and patient #11 had been discharged from hospital 11 days prior to the detection of the virus.
Twelve inpatients were admitted with primary diagnoses of respiratory problems (Table 1). Seven of these children had underlying pulmonary and/or cardiac disease. The durations of hospitalization for these patients ranged from 1 to 18 days, with a median of 3.0 days (Table 2). One child had a pneumococcal empyema (patient #15) and 1 had suspected aspiration pneumonia (patient #26), but the other 10 patients had clinical pictures compatible with viral ARI (bronchiolitis in 8 patients, laryngotracheobronchitis in 1 patient, and exacerbation of RAD in 1 patient). Excluding the child with the pneumococcal empyema, patients were either afebrile (n = 7) or had low-grade fever for 3 days or less (n = 4) (Table 2). Patient #18 had a laryngeal cyst and required intensive care unit (ICU) admission and ventilation because of exacerbation of stridor, while patient #8 was recovering from cardiac surgery in the ICU when HCoV-NL63 was detected, but none of the other patients required ICU admission. Treatments administered to patients included antibiotics (six patients), bronchodilators (eight patients), and corticosteroids (five patients). Nosocomial infection was possible in patients #22 and #24, as they had been discharged from hospital 7 and 9 days, respectively, prior to their admissions when HcoV-NL63 was identified. Patient #20 was the sibling of patient #4 (who remained as an outpatient), and their viruses were detected 4 days apart (Table 1). Patient #23 had a coinfection with hMPV. Patient #24 was discharged on oxygen after 18 days, despite not being on oxygen at the time of admission, but all other patients had uneventful recoveries.
TABLE 2.
Clinical features and medical treatments for inpatients positive for HCoV-NL63
| Patient no. | No. of days
|
Temperature (°C)d | White blood cell count | Polymorphonucleocytes (%) | Bands (%) | Findings upon chest radiographe | ||
|---|---|---|---|---|---|---|---|---|
| Hospitalizeda | Feverb | Oxygenc | ||||||
| 15 | 10 | 2 | 5 | 40.1 | 26.8 | 58 | 39 | LC, PE |
| 16 | 4 | 0 | 0 | 37.6 | 12.1 | 28 | 0 | PHT |
| 17 | 2 | 1 | 0 | 38.7 | 11.1 | 71 | 0 | ND |
| 18 | NA | 1 | 7 | 38.7 | 11.9 | 82 | 0 | A, PE |
| 19 | 1 | 0 | 1 | 37.5 | ND | Normal | ||
| 20 | 12 | 3 | 7 | 39.6 | 11.1 | 52 | 14 | HI |
| 21 | 7f | 0 | 2 | 37.1 | 8.1 | 27 | 4 | PHT |
| 22 | 1 | 0 | 0 | ND | ND | PHT | ||
| 23 | 2 | 0 | 0 | 37.6 | 3.3 | 63 | 0 | ND |
| 24 | 18 | 0 | >18 | 37.4 | ND | HI | ||
| 25 | 1 | 0 | 0 | 36.8 | ND | HI, A | ||
| 26 | NA | 2 | NA | 38.4 | 4.8 | 30 | 31 | HI |
NA, not applicable, as admission was prolonged for investigations or surgery.
No. of days of fever while hospitalized.
No. of days of oxygen use while hospitalized.
Highest temperature recorded in hospital. ND, not done.
A, atelectasis; LC, lobar consolidation; PC, patchy consolidation; PE, pleural effusion; PHT, perihilar thickening.
Transferred from another hospital; nasopharyngeal specimen obtained upon admission.
Phylogenetic analysis.
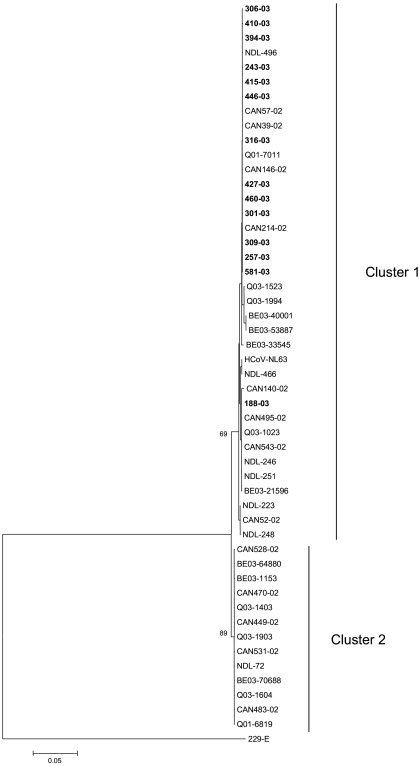
Nucleotide sequences were determined for nucleotides 5856 to 6280 of the 1a gene for 14 out of 26 positive specimens. Sequence comparison with published Dutch, Australian, Belgian, and previously characterized 2002 Canadian isolates showed that the 1a genes were relatively well conserved, with nucleic acid identities between specimens ranging from 97.2% to 100%. The phylogenetic tree of the HCoV-NL63 isolates showed the existence of two major groups or clusters, with the majority of isolates clustering in cluster 1 (Fig. 2). All the present Canadian isolates were found in cluster 1, whereas previously reported Canadian, Australian, Belgian, and Dutch isolates were found in both clusters. Nucleotide sequence comparison revealed five conserved nucleotide changes between isolates representative of clusters 1 and 2 (boxed in Fig. 3).
FIG. 2.
Phylogenetic analysis of HCoV-NL63 isolates. Nucleotide sequences were determined for nucleotides 5856 to 6280 of the 1a gene. The corresponding gene sequences from previously reported Dutch, Canadian, and Australian HCoV-NL63 isolates were also included. Phylogenetic analysis was performed using the neighbor-joining method of the MEGA2 program. The Dutch reference strain is indicated by HCoV-NL63, and the previous Dutch, Canadian, Belgian, and Australian isolates are indicated by NDL, CAN, BE03, and Q03, respectively, followed by the isolate number (e.g., NDL-246). The isolates presented in this study are in bold and indicated by the isolate number and the year (e.g., 140-02).
FIG. 3.
Alignment of partial nucleotide sequences of the 1a gene of representative cluster 1 and 2 HCoV-NL63 strains. Only residues that differ from isolate HCoV-NL63 are shown. Identical nucleotides are represented by periods, and nucleotide positions are indicated at the ends of the lines. The five conserved changes between the cluster 1 and 2 isolates are boxed.
DISCUSSION
The prevalence of HCoV-NL63 in children and the morbidity associated with HCoV-NL63 infection are not well characterized. In this study, we have established that HCoV-NL63 circulated in infants and young children in Canada during 2002 and 2003. HCoV-NL63 was detected in 2.1% of specimens tested and was associated with both URTI and lower respiratory tract infections. These findings are similar to those of previous studies that reported detection rates ranging from 1.3% to 3.6% in various sample sets (1-6, 12, 15). In 2005, Esper et al. reported a higher positivity rate (8.8%), which could be due to the fact that they screened only children <5 years old or screened only when HCoV-NL63 was circulating (5).
Consistent with previous reports, HCoV-NL63 showed a seasonal distribution and was transmitted during the winter season, with predominance in February and March, in our study (1-5, 15). The prevalence of the virus in March 2003 might have been underestimated, since only 39.0% of the specimens that tested negative from that month were available for the screening of HCoV-NL63. The detection of HCoV-NL63 during the summer months, when 59.0% to 82.8% of the specimens were available for testing, suggests that low-level circulation of the virus occurs throughout the year.
The clinical symptoms associated with HCoV-NL63 were similar to those reported previously and are comparable to those observed in other viral respiratory infections with a predominance of bronchiolitis in hospitalized patients. However, prospective studies will be required to prove that HCoV-NL63 is a cause of ARI and to demonstrate the full spectrum of the disease. Our preliminary data suggest that, as with RSV, children of <12 months of age appear to be at increased risk for severe HCoV-NL63 infection. In this study, 65% of the HCoV-NL63-positive patients were <12 months of age, which is comparable to the 63% rate in a previous study (5). The role of maternal antibody in preventing or modifying infection remains to be determined, but five of the seven outpatients and 4 of the 19 inpatients were ≤2 months of age, suggesting that maternal antibody is not always present or, as with RSV, does not provide reliable protection in early infancy. Other human coronaviruses have been associated with severe disease in infants (11). Similar to what was found in previous reports (5, 6, 12), 69% of the children with HCoV-NL63 infection had underlying medical problems (especially prematurity and pulmonary and cardiac diseases). In contrast, other studies reported HCoV-NL63 infections mainly in previously well patients (1-4, 15). Differences in the populations under study could explain the variation observed in the incidence of HCoV-NL63 infection in patients with underlying medical problems. It is likely that infection with HCoV-NL63 is similar to those with RSV and hMPV and that infection is almost universal in early childhood, with recurrence, such that the virus can be detected from all age groups when the virus is circulating.
Previous phylogenetic analysis based on the 1a gene showed the presence of two distinct genetic clusters (1 and 2) (1, 2, 4, 15). The results show that all of the Canadian isolates presented in this paper clustered within cluster 1, whereas those of previous epidemics are found in both clusters. These findings indicate a shift in the predominant genotype over time, suggesting a temporal evolution of HCoV-NL63. However, additional studies are needed to confirm this hypothesis.
In conclusion, prospective, population-based studies will be required to provide a better understanding of the epidemiology and spectrum of illness caused by HCoV-NL63.
REFERENCES
- 1.Arden, K. E., M. D. Nissen, T. P. Sloots, and I. M. Mackay. 2005. New human coronavirus, HCoV-NL63, associated with severe lower respiratory tract disease in Australia. J. Med. Virol. 75:455-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bastien, N., K. Anderson, L. Hart, P. Van Caeseele, K. Brandt, D. Milley, T. Hatchette, E. C. Weiss, and Y. Li. 2005. Human coronavirus NL63 infection in Canada. J. Infect. Dis. 191:503-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiu, S. S., K. H. Chan, K. W. Chu, S. W. Kwan, Y. Guan, L. L. Poon, and J. S. Peiris. 2005. Human coronavirus NL63 infection and other coronavirus infections in children hospitalized with acute respiratory disease in Hong Kong, China. Clin. Infect. Dis. 40:1721-1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebihara, T., R. Endo, X. Ma, N. Ishiguro, and H. Kikuta. 2005. Detection of human coronavirus NL63 in young children with bronchiolitis. J. Med. Virol. 75:463-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esper, F., C. Weibel, D. Ferguson, M. L. Landry, and J. S. Kahn. 2005. Evidence of a novel human coronavirus that is associated with respiratory tract disease in infants and young children. J. Infect. Dis. 191:492-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fouchier, R. A., N. G. Hartwig, T. M. Bestebroer, B. Niemeyer, J. C. de Jong, J. H. Simon, and A. D. Osterhaus. 2004. A previously undescribed coronavirus associated with respiratory disease in humans. Proc. Natl. Acad. Sci. USA 101:6212-6216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health Canada. Editorial Board of Respiratory Disease in Canada. 2001. Respiratory disease in Canada. [Online.] http://www.phac-aspc.gc.ca/publicat/rdc-mrc01/index.html.
- 8.Holmes, K. V. 2001. Coronavirus, p. 1187-1204. In D. M. Knipe and M. D. Howley (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams and Wilkins, Philadelphia, Pa. [Google Scholar]
- 9.Kim, H. W., J. O. Arrobio, C. D. Brandt, B. C. Jeffries, G. Pyles, J. L. Reid, R. M. Chanock, and R. H. Parrott. 1973. Epidemiology of respiratory syncytial virus infection in Washington, D.C. I. Importance of the virus in different respiratory tract disease syndromes and temporal distribution of infection. Am. J. Epidemiol. 98:216-225. [DOI] [PubMed] [Google Scholar]
- 10.Kumar, S., K. Tamura, I. B. Jakobsen, and M. Nei. 2001. MEGA2: molecular evolutionary genetics analysis software. Bioinformatics 17:1244-1245. [DOI] [PubMed] [Google Scholar]
- 11.McIntosh, K., R. K. Chao, H. E. Krause, R. Wasil, H. E. Mocega, and M. A. Mufson. 1974. Coronavirus infection in acute lower respiratory tract disease of infants. J. Infect. Dis. 130:502-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moes, E., L. Vijgen, E. Keyaerts, K. Zlateva, S. Li, P. Maes, K. Pyrc, B. Berkhout, L. Van Der Hoek, and M. Van Ranst. 2005. A novel pancoronavirus RT-PCR assay: frequent detection of human coronavirus NL63 in children hospitalized with respiratory tract infections in Belgium. BMC Infect. Dis. 5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monto, A. S. 2002. Epidemiology of viral respiratory infections. Am. J. Med. 112(Suppl. 6A):4S-12S. [DOI] [PubMed] [Google Scholar]
- 14.van den Hoogen, B. G., J. C. de Jong, J. Groen, T. Kuiken, R. de Groot, R. A. Fouchier, and A. D. Osterhaus. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 7:719-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Hoek, L., K. Pyrc, M. F. Jebbink, W. Vermeulen-Oost, R. J. Berkhout, K. C. Wolthers, P. M. Wertheim-Van Dillen, J. Kaandorp, J. Spaargaren, and B. Berkhout. 2004. Identification of a new human coronavirus. Nat. Med. 10:368-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.W.H.O. Communicable Disease Surveillance and Response (CSR). 2003. Summary of probable SARS cases with onset of illness from November 1 2002 to July 31 2003. [Online.] http://www.who.int/csr/sars/country/table2004_04_21/en/.