Abstract
West Nile Virus (WNV) antibody development and persistence were investigated in blood donors who made WNV RNA-positive (viremic) donations in 2003. Plasma samples from the index donations and follow-up serum or plasma samples were tested for WNV immunoglobulin M (IgM), IgA, and IgG by using enzyme-linked immunosorbent assays. Antibody development was investigated with 154 samples collected from 84 donors 1 to 21 days after their RNA-positive, antibody-negative, index donation. WNV IgM and IgA were first detected on day 3, and all samples collected after day 9 were WNV IgM and IgA positive; WNV IgG was first detected on day 4, and all samples collected after day 16 were positive. Antibody persistence in this donor group (index donations antibody negative) was evaluated by using 128 samples collected from 89 donors on days 22 to 440 of follow-up; 88% of samples were WNV IgM positive, 86% were WNV IgA positive, and 100% were WNV IgG positive. In linear regression analysis, trendlines for WNV IgM and IgA reached the value discriminating positive from negative results at 218 days and 232 days of follow-up, respectively. Similar WNV IgM and IgA persistence trends characterized 27 donors whose index samples were positive for WNV IgM and IgA, as well as 14 donors whose index samples were positive for WNV IgG but negative for WNV IgM. These findings show that WNV IgG emerges after WNV IgM and IgA and that both WNV IgM and IgA typically persist for at least 6 months after infection. Thus, unlike some other flavivirus infections, WNV infection is not characterized by a relatively rapid disappearance of virus-specific IgA.
During the westward spread of West Nile Virus (WNV) across the United States, most cases in a given season occurred in geographic areas where the virus was newly introduced. However, infections continue to occur in states with large numbers of cases in prior seasons, albeit at lower levels (4). In these areas where WNV is now endemic, the diagnostic utility of WNV immunoglobulin M (IgM) detection has come into question; this concern is based mainly on the findings of Roehrig et al. (18), who showed that WNV IgM remained detectable in some WNV encephalitis patients for more than a year. Thus, for some patients from areas of endemicity, it may be difficult to determine whether a positive WNV IgM result reflects recent infection versus infection during the prior season.
Published findings for antibody responses to other flaviviruses suggest that WNV IgA detection may be a useful tool for distinguishing recent from past WNV infection. Virus-specific IgA appears quickly after infection by dengue viruses then falls to undetectable levels within a few months (6, 9, 22). Likewise, vaccine-induced yellow fever virus IgA disappears by about 80 days after vaccination (12). Preliminary findings consistent with these trends have been presented for WNV infection; Lanciotti (10) detected WNV IgA only between 11 and 50 days postinfection in most WNV-infected patients. However, systematic studies of WNV IgA production and persistence are lacking.
A unique opportunity for assessing WNV antibody development and persistence recently emerged from efforts to identify donations from WNV-infected blood donors and thus reduce the risk of transfusion-associated transmission of WNV (13). During the 2003 WNV season, blood collection agencies began measuring levels of WNV RNA in plasma by nucleic acid amplification test (NAT) screening, and viremic (i.e., WNV RNA-positive) donors were enrolled in follow-up studies designed to assess the length of the viremic period and document the antibody response to WNV (3). We report here findings on the emergence and persistence of the major classes (IgM, IgA, and IgG) of WNV antibodies during follow-up of blood donors who donated a confirmed WNV RNA-positive unit during the 2003 season.
MATERIALS AND METHODS
Blood donor specimens.
WNV RNA-positive blood donors were identified by NAT screening of donations made between June and November 2003 as previously described (3). Plasma from donations confirmed as WNV RNA-positive (hereafter referred to as the index donations), as well as plasma or serum specimens collected during follow-up visits, were supplied by Blood Systems Research Institute and American Red Cross Blood Services. Informed consent was obtained from all donors at the local blood donation site; protocols for NAT screening and follow-up were approved by local institutional review boards and the U.S. Food and Drug Administration.
WNV antibody assays.
Plasma and serum specimens were tested for WNV IgM and WNV IgG by using U.S. Food and Drug Administration-cleared enzyme-linked immunosorbent assay (ELISA) kits manufactured by Focus Diagnostics (8); the assays were performed according to the instructions supplied in the package inserts. WNV IgA was measured by using an in-house alpha-capture ELISA modeled after the WNV IgM ELISA, differing from the WNV IgM ELISA in only three aspects. These differences were (i) the microtiter wells were coated with rabbit anti-human IgA, (ii) the enzyme substrate (tetramethylbenzidine) was obtained from a different vendor (enhanced K-blue; Neogen Corp., Lexington, KY), and (iii) the substrate incubation step was 30 min. An earlier study (17) showed the assay to be >95% sensitive with a panel of sera positive for WNV IgM and IgG, as well as a panel of sera positive in the WNV plaque reduction neutralization test; the assay was 100% specific with a panel of sera negative for WNV IgM and IgG, as well as a panel of sera from Los Angeles area blood donors collected in 1999. WNV IgM, IgG, and IgA results were expressed as sample/calibrator ratio (SCR; referred to as index in prior reports) (8, 17), calculated by dividing the absorbance value obtained for the donor sample by the absorbance value obtained for the calibrator serum included in all assay runs; a positive result was defined as SCRs of >1.10 for WNV IgM, >1.50 for WNV IgG, and >1.00 for WNV IgA. For the present study, values less than or equal to the indicated values were defined as negative. SCR values in all figures are presented using a logarithmic scale; all SCR values less than 0.12 were assigned a value of 0.11 for inclusion in figures.
Statistical analyses.
Differences among proportions were evaluated by using chi-square analysis. An ordinary least-squares linear model was used for regression analysis of WNV IgM and IgA persistence; the logarithms of SCR values were plotted as a function of days post index, and the resulting linear regression formulas were used to calculate the day post index associated with the SCR value discriminating positive from negative results (1.10 for WNV IgM and 1.00 for WNV IgA). The formula format (MedCalc Software, Mariakerke, Belgium) was: log Y = a + bX, where a represents the y intercept and b represents the slope of the log-transformed variable. The same model also provided a statistical test for the difference between the slopes. For all statistical analyses, a P value of <0.05 was considered statistically significant.
RESULTS
Distribution of index and follow-up samples.
A total of 282 follow-up samples were collected from 115 donors whose index donations were negative for WNV IgM, IgA, and IgG. These follow-up samples were segregated into two mutually exclusive groups based on the number of days since the index donation; 154 samples collected during the first 21 days of follow-up were used to assess WNV antibody development, and 128 samples collected >21 days post index were used to assess WNV antibody persistence. Day 21 of follow-up was selected as the segregating time point on the basis of published studies demonstrating seroconversion within 3 weeks of disease onset in essentially all WNV-infected patients (2, 14, 15, 23). Similarly, 50 follow-up samples were obtained from 29 donors whose index donations were already positive for WNV IgM and IgA (22 index donations were WNV IgG positive, seven were WNV IgG negative); 29 of the 50 follow-up specimens (from 27 donors) were collected >21 days post index and were used to evaluate WNV antibody persistence in this group. A third sample group contained 20 follow-up samples collected from 14 donors whose index donations were positive for WNV IgG but negative for WNV IgM; 12 of these 14 index donations were also negative for WNV IgA.
Development of WNV antibodies.
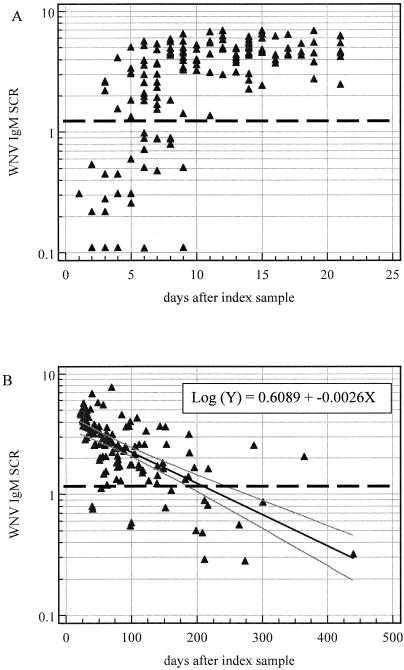
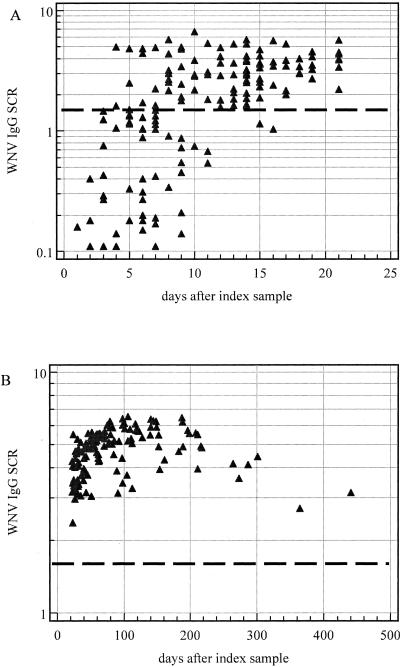
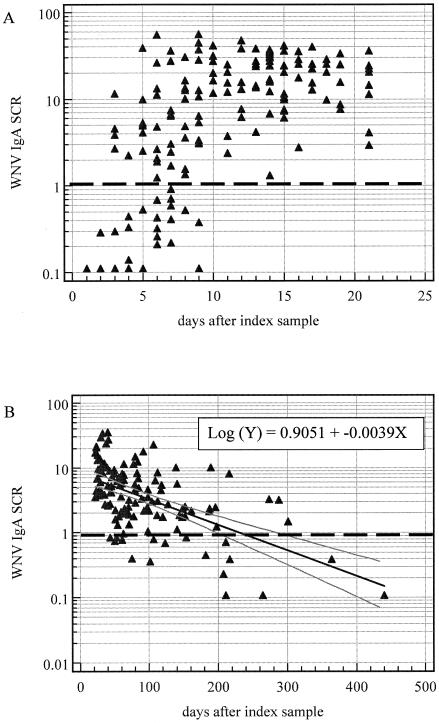
The timeline for development of WNV antibodies was evaluated by testing 154 samples collected from 84 donors during the first 21 days after donation of index plasma specimens negative for WNV antibodies. The results for WNV IgM, IgA, and IgG in these early follow-up samples are shown in panel A of Fig. 1 to 3, respectively. WNV IgM and IgA were first detected on day 3 post index, and all specimens collected after day 9 were positive for WNV IgM and IgA. WNV IgG was first detected on day 4 post index, and all specimens collected after day 16 were positive for WNV IgG. Thus, WNV IgA developed in parallel with WNV IgM, and WNV IgG developed later than both WNV IgM and IgA.
FIG. 1.
WNV IgM SCR values for follow-up samples from viremic blood donors whose index donations were negative for WNV antibodies. The dark dashed horizontal line in each panel indicates an SCR of 1.10, used to discriminate positive from negative results. (A) Samples collected on days 1 to 21 of follow-up. (B) Samples collected on days 22 to 440 of follow-up. The dark solid line represents the linear regression trend line, and the two lighter parallel lines represent the 95% confidence interval; the line formula is shown in the upper right-hand corner.
FIG. 3.
WNV IgG SCR values for follow-up samples from viremic blood donors whose index donations were negative for WNV antibodies. The dark dashed horizontal line in each panel indicates an SCR of 1.50, used to discriminate positive from negative results. (A) Samples collected on days 1 to 21 of follow-up. (B) Samples collected on days 22 to 440 of follow-up.
Persistence of WNV antibodies.
WNV antibody persistence in donors whose index donations were negative for WNV antibodies was assessed by measuring WNV IgM, IgA, and IgG in 128 samples collected >21 days post index from 89 donors. The distributions of SCR values are plotted as a function of days post index in panel B of Fig. 1 to 3. Overall, 88% of these samples were positive for WNV IgM (Fig. 1B), and 86% were positive for WNV IgA (Fig. 2B). As shown in the figures, samples collected >200 days after the index sample were more likely to be negative for WNV IgM or WNV IgA compared to samples collected <200 days post index. Linear regression analysis of the logarithm of SCR values versus days post index was used to approximate the day post index associated with the SCR discriminating positive from negative results; for WNV IgM this time point was day 218, and for WNV IgA it was day 232. Using this same model, the slope of the regression line for WNV IgA was statistically different from the slope for WNV IgM (P = 0.0054). All specimens collected >21 days post index were positive for WNV IgG, with maximal SCR values observed around day 100 of follow-up. A gradual decrease in IgG SCR values over time was observed for samples collected >200 days after the index donation (Fig. 3B); however, the small number of samples collected during this time frame precluded regression analysis of the time point associated with the IgG SCR discriminating positive from negative results.
FIG. 2.
WNV IgA SCR values for follow-up samples from viremic blood donors whose index donations were negative for WNV antibodies. The dark dashed horizontal line in each panel indicates an SCR of 1.00, used to discriminate positive from negative results. (A) Samples collected on days 1 to 21 of follow-up. (B) Samples collected on days 22 to 440 of follow-up. The dark solid line represents the linear regression trend line, and the two lighter parallel lines represent the 95% confidence interval; the line formula is shown in the upper right-hand corner.
WNV antibody persistence was also investigated for 27 donors whose index donations were already positive for WNV IgM and IgA (i.e., markers of acute WNV infection); 29 samples collected 22 to 377 days post index were evaluated. The proportions of these specimens positive for WNV IgM or WNV IgA (both 83%) were not significantly different from the comparable proportions (88 and 86%, respectively) for samples from donors whose index donations were negative for WNV antibodies (Fig. 1B and 2B). All 29 follow-up samples were positive for WNV IgG.
Lastly, development, and persistence of WNV IgM and IgA antibodies were evaluated in a small group of 14 viremic donors (Table 1) whose index donations were positive for WNV IgG but not WNV IgM (12 of 14 index donations were also negative for WNV IgA). WNV IgM developed and persisted in nine donors along the same general timelines as demonstrated in Fig. 1; WNV IgA developed and persisted in all but one donor with the same general kinetics shown in Fig. 2. Likewise, WNV IgG SCR values were typically higher in follow-up samples than in the corresponding IgG-positive index samples.
TABLE 1.
Results for follow-up samples from donors whose index donations were positive for WNV-specific IgG but not WNV-specific IgM
| Donor | Day of follow-upa | WNV SCR
|
||
|---|---|---|---|---|
| IgM | IgA | IgG | ||
| A | 0 | 0.30 | 0.51 | 2.58 |
| 7 | 2.18 | 33.38 | 5.19 | |
| B | 0 | 0.49 | <0.10 | 2.07 |
| 12 | 4.22 | 14.05 | 5.06 | |
| 68 | 2.02 | 3.17 | 8.23 | |
| C | 0 | 0.77 | <0.10 | 1.57 |
| 9 | 0.82 | <0.10 | 1.71 | |
| 76 | 2.03 | 2.87 | 6.34 | |
| D | 0 | 0.26 | <0.10 | 2.89 |
| 6 | 6.16 | 17.26 | 5.06 | |
| E | 0 | 0.11 | 0.38 | 2.84 |
| 12 | 2.77 | 34.94 | 3.00 | |
| F | 0 | 0.07 | <0.10 | 1.88 |
| 5 | 0.28 | 0.59 | 3.83 | |
| 83 | 0.51 | 2.76 | 5.77 | |
| G | 0 | 0.15 | 0.23 | 1.59 |
| 15 | 2.83 | 8.89 | 3.44 | |
| 22 | 3.17 | 6.06 | 5.15 | |
| H | 0 | 0.12 | <0.10 | 1.93 |
| 44 | 1.73 | 8.34 | 3.26 | |
| I | 0 | 0.33 | <0.10 | 1.68 |
| 8 | 0.73 | 0.20 | 1.71 | |
| 11 | 3.37 | 4.65 | 2.75 | |
| J | 0 | 0.22 | <0.10 | 2.03 |
| 14 | 4.63 | 19.89 | 3.50 | |
| 93 | 1.55 | 3.09 | 6.55 | |
| K | 0 | 0.21 | <0.10 | 3.17 |
| 35 | 0.77 | 6.81 | 3.03 | |
| L | 0 | 0.41 | <0.10 | 4.11 |
| 199 | 0.56 | 0.86 | 4.77 | |
| M | 0 | 0.32 | 2.96 | 4.65 |
| 17 | 1.02 | 25.10 | 2.82 | |
| N | 0 | 0.65 | 4.86 | 5.99 |
| 21 | 0.81 | 5.13 | 7.39 | |
Follow-up day 0 = index donation.
DISCUSSION
The identification of WNV-infected blood donors by NAT screening has led to the collection of an invaluable specimen panel for studying the natural history of WNV antibody production and persistence. WNV viremia begins within a few days of infection and is short-lived (2, 5, 11, 19, 20), thus serving as a clear indicator of recent infection. Models based on viral doubling time and the viral load of the index donation suggest that the time between an infectious mosquito bite and donation of the index specimen averages about 8 days (1). The timeline of antibody production and persistence based on days since donation of the index sample thus appears to be a good approximation of the timeline based on days since infection. However, further validation of the assumptions underlying the models for extrapolating the day of infection is needed before timelines of antibody production and persistence can be expressed as days since infection (1).
WNV antibody development was investigated by using follow-up serum or plasma samples from donors whose index plasma specimens were positive for WNV RNA but negative for the three major isotypes of WNV antibodies (IgM, IgG, and IgA). The patterns of WNV IgM and IgG emergence were consistent with published findings (2, 14, 15, 23) demonstrating that WNV IgM is typically detected a few days before IgG. Our results extend these findings by showing that WNV IgA appears at about the same time as WNV IgM, and before WNV IgG, and are consistent with published data (6, 9, 22) demonstrating early detection of virus-specific IgA in other flavivirus infections.
Follow-up samples from this same donor group (antibody-negative index donations) were used to evaluate persistence of WNV antibody isotypes. WNV IgM was remarkably persistent during the follow-up period, particularly during the first 200 days of follow-up. Linear regression analysis indicated that, at least among this study group and under our assay conditions, reversion from a positive to negative WNV IgM result should be expected around day 218 of follow-up. Evaluation of more follow-up samples collected >200 days post index is needed to test this hypothesis.
Our WNV IgM persistence findings are consistent with those of Roehrig et al. (18), who found that the vast majority of samples collected from WNV encephalitis patients between days 50 and 250 of follow-up were positive for WNV IgM. In contrast, our findings differ from those of Tardei et al. (23), who found that ca. 45% of samples collected from WNV-infected patients at 60 to 100 days of follow-up were negative for WNV IgM. Indeed, our current findings contrast with our own previous results (16) demonstrating WNV IgM seroreversion in 54% of WNV patients with two samples collected 60 to 111 days apart. Our earlier study was limited by lack of information of the date of clinical presentation and date of onset; further, the WNV IgM ELISA used at the time utilized native WNV antigen, serum at a fourfold higher dilution, and a higher SCR to discriminate positive from negative results. Unfortunately, the WNV IgM-negative samples from the earlier study were not available for comparative evaluation using the current WNV IgM assay format.
Like WNV IgM, WNV IgA was remarkably persistent over time, particularly during the first 200 days of follow-up. Thus, WNV IgA detection does not appear to be a useful adjunct to WNV IgM detection for identifying very recent WNV infection. Indeed, linear regression analysis indicated that WNV IgA persistence is similar to that of WNV IgM, with seroreversion expected at about 232 days of follow-up. These findings are consistent with published findings of long-term persistence of IgA directed to other flaviviruses. Han et al. (7) detected IgA to Japanese encephalitis virus in three of six infected children 145 days after disease onset; similarly, Summers et al. (21) detected IgA to dengue-2 in six of nine vaccinated volunteers at 6 months of follow-up. Our results differ, however, from findings reported by other groups studying immune responses to flaviviruses. Two groups (9, 22) reported that IgA recognizing dengue viruses fell to undetectable levels within a few months of infection, and a third group (12) found that yellow fever IgA was not detectable by 80 days post vaccination. Further, our findings differ from those of Lanciotti et al. (10), who have presented preliminary data indicating that WNV IgA is rarely detected in samples collected from WNV-infected patients >50 days after onset. It remains unclear if this discrepancy reflects differences in assay sensitivities, study groups, and/or other parameters.
The dynamic range of WNV IgA SCR values was much broader compared to WNV IgM and IgG SCR values, with many samples exhibiting WNV IgA values >10.00. This phenomenon reflected procedural differences unique to the WNV IgA ELISA; enzyme substrate was purchased from a different vendor, and a longer substrate incubation time was used (17). These higher WNV IgA SCR values, coupled with stronger variance, most likely contributed to the more pronounced negative slope calculated for WNV IgA versus WNV IgM in the regression model. The point meriting emphasis from the model, however, is that the timeframes for WNV IgM and WNV IgA seroreversion appear to be similar.
Not surprisingly, all follow-up samples collected >21 days post index were positive for WNV IgG. SCR values peaked around day 100 of follow-up and appeared to plateau for the next 100 days. The small number of samples collected >200 days post index showed a trend toward decreasing IgG SCR values over time; additional studies with more specimens collected many months or years after infection are required to accurately assess WNV IgG persistence.
In support of findings from the 2002 WNV season in the United States (24), some index donations contained both WNV RNA and WNV antibodies indicative of recent infection (i.e., IgM and IgA). This observation thus suggests that detection of WNV IgM and IgA cannot be taken as evidence that the viremic period has ended. Detailed studies of the timeline of WNV viremia in blood donors, relative to the evolution of serological markers, are needed.
Index donations from a small group of viremic blood donors were positive for WNV IgG but negative for WNV IgM. The explanation for this unusual antibody pattern in viremic individuals remains unclear; the IgG positive result may reflect prior natural exposure to WNV or another flavivirus, prior vaccination to a flavivirus, or a false-positive result. Likewise, the limited availability of follow-up samples and the long time intervals between samples make some of the follow-up results difficult to interpret. However, the majority of these donors showed a further increase in WNV IgG SCR values and exhibited WNV IgM and IgA development and persistence patterns similar to those observed for other viremic donors; these findings thus indicate a competent acute immune response to WNV infection in these donors. Further studies are needed to characterize this unusual subset of viremic donors.
Acknowledgments
We thank all personnel at local blood centers who participated in the recruitment of donors for follow-up studies and collected index and follow-up specimens. Jane Filamor, Rabinderjot Sahni, Irina Walsh, Nelly Gefter, and Simon Ng provided expert technical assistance, and Jose Matud supplied valuable statistical advice.
REFERENCES
- 1.Busch, M. P., and S. L. Stramer. 2005. Viremia and antibody studies in WNV-infected blood donors. Centers for Disease Control and Prevention, Atlanta, Ga. [Online.] www.cdc.gov/ncidod/dvbid/westnile/conf/February_2005.htm.
- 2.Centers for Disease Control and Prevention. 2002. Laboratory-acquired West Nile Virus infections—United States, 2002. Morb. Mortal. Wkly. Rep. 51:1133-1135. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2004. Update: West Nile virus screening of blood donations and transfusion-associated transmission—United States, 2003. Morb. Mortal. Wkly. Rep. 53:281-284. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2004. 2004 West Nile virus activity in the United States. Centers for Disease Control and Prevention, Atlanta, Ga. [Online.] http://www.cdc.gov/ncdod/cvbid/westnile/surv&controlCaseCOntrol_detailed.htm.
- 5.Gordon, S. M., and C. M. Isada. 2003. West Nile fever: lessons from the 2002 season. Cleveland Clin. J. Med. 70:449-454. [DOI] [PubMed] [Google Scholar]
- 6.Groen, J., J. Velzing, C. Copra, E. Balentien, V. Deubel, V. Vorndam, and A. D. Osterhaus. 1999. Diagnostic value of dengue virus-specific IgA and IgM serum antibody detection. Microbes Infect. 1:1085-1090. [DOI] [PubMed] [Google Scholar]
- 7.Han, X. Y., Q. W. Ren, Z. Y. Yu, and T. F. Tsai. 1988. Serum and cerebrospinal fluid immunoglobulins M, A, and G in Japanese encephalitis. J. Clin. Microbiol. 26:976-978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hogrefe, W. R., R. Moore, M. Lape-Nixon, M. Wagner, and H. E. Prince. 2004. The performance of West Nile Virus recombinant (preM/E)-based IgG and IgM ELISA for the detection of West Nile Virus and other flavivirus antibodies. J. Clin. Microbiol. 42:4641-4648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koraka, P., C. Suharti, T. E. Setiati, A. T. A. Mairuhu, E. Van Gorp, C. E. Hack, M. Juffrie, J. Sutaryo, G. M. Van Der Meer, J. Groen, and A. D. M. E. Osterhaus. 2001. Kinetics of dengue virus-specific serum immunoglobulin classess and subclasses correlate with clinical outcome of infection. J. Clin. Microbiol. 39:4332-4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lanciotti, R. S. 2004. Current laboratory protocols for West Nile Virus. Centers for Disease Control and Prevention, Atlanta, Ga. [Online.] www.cdc.gov/ncidod/dvbid/westnile/conf/February_2004.htm.
- 11.Marfin, A. A., and D. J. Gubler. 2001. West Nile encephalitis: an emerging disease in the United States. Clin. Infect. Dis. 33:1713-1719. [DOI] [PubMed] [Google Scholar]
- 12.Monath, T. P. 1971. Neutralizing antibody response in the major immunoglobulin classes to yellow fever 17D vaccination of humans. Am. J. Epidemiol. 93:122-129. [DOI] [PubMed] [Google Scholar]
- 13.Pealer, L. N., A. A. Marfin, L. R. Petersen, R. S. Lanciotti, P. L. Page, S. L. Stramer, M. G. Stobierski, K. Signs, B. Newman, H. Kapoor, J. L. Goodman, and M. E. Chamberland. 2003. Transmission of West Nile virus through blood transfusion in the United States in 2002. N. Engl. J. Med. 349:1236-1245. [DOI] [PubMed] [Google Scholar]
- 14.Petersen, L. R., and A. A. Marfin. 2002. West Nile Virus: a primer for the clinician. Ann. Int. Med. 137:173-179. [DOI] [PubMed] [Google Scholar]
- 15.Petersen, L. R., J. T. Roehrig, and J. M. Hughes. 2002. West Nile virus encephalitis. N. Engl. J. Med. 347:1225-1226. [DOI] [PubMed] [Google Scholar]
- 16.Prince, H. E., and W. R. Hogrefe. 2003. Detection of West Nile Virus (WNV)-specific immunoglobulin M in a reference laboratory setting during the 2002 WNV season in the United States. Clin. Diagn. Lab. Immunol. 10:764-768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prince, H. E., and M. Lape-Nixon. 2005. Evaluation of a West Nile virus immunoglobulin A (WNV IgA) capture enzyme-linked immunosorbent assay (ELISA). Clin. Diagn. Lab. Immunol. 12:231-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roehrig, J. T., D. Nash, B. Maldin, A. Labowitz, D. A. Martin, R. S. Lanciotti, and G. L. Campbell. 2003. Persistence of virus-reactive serum immunoglobulin M antibody in confirmed West Nile Virus encephalitis cases. Emerg. Infect. Dis. 9:376-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampathkumar, P. 2003. West Nile virus: epidemiology, clinical presentation, diagnosis, and prevention. Mayo Clin. Proc. 78:1137-1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Solomon, T., M. H. Ooi, D. W. C. Beasley, and M. Mallewa. 2003. West Nile encephalitis. Br. J. Med. 326:865-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Summers, P. L., K. H. Eckels, J. M. Dalrymple, R. M. Scott, and V. A. Boyd. 1984. Antibody response to Dengue-2 vaccine measured by two different radioimmunoassay methods. J. Clin. Microbiol. 19:651-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Talarmin, A., B. Labeau, J. Lelarge, and J.-L. Sarthou. 1998. Immunoglobulin A-specific capture enzyme-linked immunosorbent assay for diagnosis of Dengue Fever. J. Clin. Microbiol. 36:1189-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tardei, G., S. Ruta, V. Chitu, C. Rossi, T. F. Tsai, and C. Cernescu. 2000. Evaluation of immunoglobulin M (IgM) and IgG enzyme immunoassays in serologic diagnosis of West Nile virus infection. J. Clin. Microbiol. 38:2232-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tobler, L. H., C. Bianco, S. A. Glynn, G. B. Schreiber, B. J. Dille, H. E. Prince, R. S. Lanciotti, J. M. Linnen, J. Gallarda, V. Shyamala, D. Smith, S. H. Kleinman, and M. P. Busch. 2005. Detection of West Nile Virus (WNV) RNA and antibody in frozen plasma components from a voluntary market withdrawal during the 2002 peak epidemic. Transfusion 45:480-486. [DOI] [PubMed] [Google Scholar]