Abstract
Introduction
When the diagnosis of lumbar spinal stenosis is uncertain in the conventional psoas-relaxed position (PRP) MRI, upright MRI is a not widely available alternative. The aim of this study was to investigate whether a modified supine MRI position with legs straight and an adjustable pillow under the lumbar spine (EXT) could mimic the effect of standing.
Research question
We hypothesized that EXT would mimic upright MRI in stenosis severity.
Materials and methods
Forty patients (58 % male, mean age 57 years) underwent a 3T (65 %) or 1.5T MRI. For the levels L2-S1, central stenosis (Lee: 0–3), dural cross sectional area (DCSA: mm2); lateral recess stenosis (Bartinsky: 0–3), foraminal stenosis (Lee: 0–3) and lordosis angle (LA: L1-S1°) were measured in PRP and EXT by three radiologists. Cohen's kappa and Cronbach's alpha for intra/interrater reliability and Pearson's correlation coefficient between PRP and EXT were measured. P < 0.05 was used for statistical significance.
Results
At L4/L5 EXT showed increased narrowing in 40 % (central), 37.5 % (lateral), and 17.5 % (foraminal). DCSA decreased (P < 0.0001) and LA increased (P < 0.0001), with strong correlations and high reliability (P < 0.0001). Lateral recess stenosis increased significantly in EXT at L4/L5 (P = 0.014; K = 0.646). No significant difference was observed in foraminal stenosis (K = 0.488).
Discussion and conclusion
EXT increased lumbar lordosis to the normal standing range of approximately 50°, mimicking an upright MRI. A more realistic degree of central stenosis at all levels and of lateral recess stenosis at L4/L5 was shown. Foraminal stenosis did not increase.
Keywords: Lumbar spinal stenosis, Lumbar lateral recess stenosis, Lumbar foraminal stenosis, Upright MRI, Supine position MRI
Highlights
-
•
Extended MRI increased lumbar lordosis to mimic standing posture accurately.
-
•
The dural sac surface area decreased significantly in the extended position.
-
•
Central spinal stenosis worsened in 40 % of patients at the L4-L5 level.
-
•
Yellow ligament surface area increases in the extended position.
-
•
Extended position MRI helps detect posture-dependent spinal canal narrowing.
1. Introduction
PRP is the most popular MRI positioning for patients presenting with suspected lumbar spinal stenosis. PRP is comfortable, but several reports have shown that the degree of lumbar spinal, central (LSS) and foraminal stenosis (FoS) is underestimated due to the loss of lordosis along with the enlargement of the spinal canal (Hebelka et al., 2022; Kubosch et al., 2015). It follows that there is a risk of “underrating” the severity of LSS which seems to be a functionally dependent condition (Madsen et al., 2008). Furthermore, it could influence the treatment path of elderly and often overweight patients, who are frequently also suffering from symptomatic hip and knee degenerative disease. To achieve a more realistic imaging of the LSS, several alternatives have been investigated. These include the EXT with/without a pillow supporting the lumbar spine (Hansen et al., 2017), axial load devices to be applied in the supine PRP/EXT position (Fang et al., 2024) and upright MRI (Doktor et al., 2022; Charoensuk et al., 2023). The technical “add-ons” provide valuable information to increase the specificity of a diagnosis of spinal stenosis (Hebelka et al., 2022). However, axial load devices are impractical for obese patients, cause discomfort in the shoulders and knees and they are not widely used because of the cost. Similarly, upright MRI machines are low field (≤0.6T) with longer investigation times, up to 40 min for a standing scan, lower image resolution and not everywhere easily available. Furthermore, in many countries the examination with upright MRI is not reimbursed by public insurances. On the other hand, the EXT position requires no additional cost, it is easily applicable, and available. No studies have directly compared EXT to upright MRI or assessed its diagnostic accuracy.
The aim of this prospective, cross-sectional cohort study was to compare the imaging of patients with suspected lumbar spinal stenosis (LSS) in the PRP and in the EXT. This comparison was motivated by previous findings indicating no significant difference in DCSA between EXT and standing MRI. It was found in a study by Hansen et al. that supine MRI with a lumbar pillow can replicate the biomechanical changes seen in upright MRI such as reducing the canal dimensions and increasing the stenosis grade, offering an alternative to weight-bearing scans (upright MRI) (Hansen et al., 2017). The study further aimed to assess whether EXT could serve as a complementary or alternative imaging position to PRP in patients with suspected LSS and borderline findings.
2. Methods
2.1. Study design
Patients undergoing lumbar MRI for suspected spinal stenosis were included in the study. Exclusion criteria included: scoliosis, trauma and fractures, tumors, spondylolisthesis-where there was an apparent vertebral slip in PRP, previous lumbar spine surgery, and inability to tolerate the different positions.
The Institutional Review Board approved the study under number 317/2023.
2.2. MRI protocol
Positioning: The first examination was performed with conventional PRP, which is the routine scanning method according to the departmental protocols. A triangular foam cushion was placed under the patient's flexed knees (Fig. 1a). For the second examination in EXT, the knee cushion was removed, and a cushion was placed under the lumbar spine to maintain normal lumbar lordosis (Fig. 1b). Patient comfort is paramount to obtaining good images. EXT with firm cushion has been reported to be uncomfortable to painful (Hansen et al., 2017). Therefore, we used a pre-inflated pillow that could be deflated as required by the patient by gently pressing the valve (Fig. 1b). This option allowed for precise individual adjustment. Scan time for both positions was about 11 min.
Fig. 1.
RPR position (a) and Ext position (b) inflatable pillow (c).
2.3. Image acquisition
The standard image acquisition protocol is demonstrated in Table 1.
Table 1.
Standard image acquisition protocol in PRP and EXT.
| Position | Field Strength | Sequence | TR (ms) | TE (ms) | Matrix | FOV (cm) | Slice thickness (mm) |
|---|---|---|---|---|---|---|---|
| PRP & EXT | 1.5T | Sagittal T2 TSE | 2500 | 100 | 180 × 335 | 33 × 70 | 4 |
| PRP & EXT | 1.5T | Axial T2 TSE | 3000 | 120 | 212 × 150 | 20 × 30 | 3.8 |
| PRP & EXT | 3T | Sagittal T2 TSE | 3000 | 120 | 160 × 209 | 30 × 56 | 4 |
| PRP & EXT | 3T | Axial T2 TSE | 5441 | 114.5 | 200 × 133 | 20 × 35 | 4 |
Patients were randomized to the 1.5T (Ingenia, Philips Healthcare, USA) and 3T (Achieva, Philips Healthcare, USA) machines. The images were analyzed independently by three radiologists with different levels of experience (4, 13, and 20 years) twice at 6-week intervals using the PACS (Picture Archiving and Communication System) of the Department of Radiology.
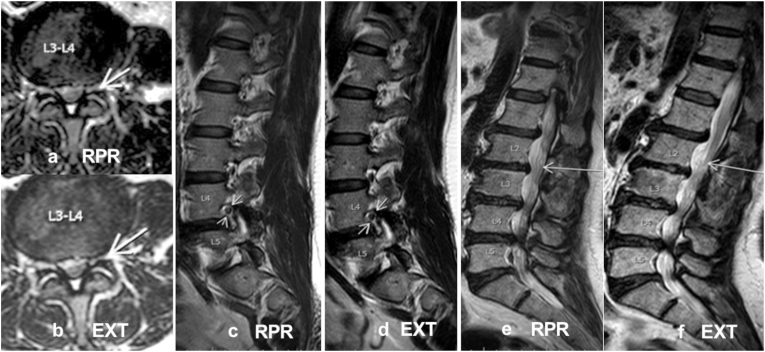
2.4. Data collection
Four levels were assessed for each patient, from L2/L3 to L5/S1, so there were 160 levels for all 40 patients. From a clinical point of view, the focus was particularly on the L4/L5 level, which is the most frequently stenotic level. The following parameters were assessed for each level for each patient in PRP and EXT positions: 1) The grades of central and lateral recess stenosis (LRS) were assessed on the axial T2 image using the methods of Lee (Lee et al., 2011) and Bartynski (Bartynski and Lin, 2003) respectively (Fig. 2c,d; 3 c,d; 4a,b). 2) The grade of foraminal stenosis (FoS) on sagittal T2 images using the grading system proposed by Lee (Lee et al., 2010) (Fig. 4c, d). 3) The dural cross-sectional area (DCSA) was digitally measured on axial T2 images using PACS software (Fig. 2c, d)4) Yellow ligament surface area (YLSA) was digitally measured using PACS software on axial T2 images (Fig. 3a, b). 5) Lordotic angle (LA) on sagittal T2 images (the angle between the superior endplate of L1 and the superior endplate of S1 (Fig. 2 a, b). 6) Presence and morphology of redundant nerve roots (RNR) according to the ASED classification proposed by Papavero et al. (2020) (Fig. 4e, f).
Fig. 2.
Sagittal (a,b) and axial (c,d) T2WI's: Changing the position from PRP to EXT increases the LA (a, b) and decreases the DCSA (c, d).
Fig. 4.
Axial T2WI's (a,b), sagittal T2WI's (c,d,e,f): Changing the position from PRP to EXT reduces the diameter of the lateral recess (a, b) and the foramen (c, d) and increases the grading of the RNR (e,f).
Fig. 3.
Axial T2WI's: Changing the position from PRP to EXT increases the YLSA (a, b) and increases the severity of the central stenosis (c,d).
2.5. Statistical analysis
For variables containing grades, the mode of the three readings from the three readers was obtained. Numerical data parameters were compared between the PRP and EXT positions using a paired t-test, and results were presented as mean ± SD. For ordinal data (grades), a Wilcoxon signed-rank test was used to compare the change in grade between the two positions, and results were presented as the number of patients in each grade and the median for each position. Inter-reader and intra-reader reliability was assessed using Cohen's kappa for variables with grades. Pearson's correlation coefficient was used to assess correlations between numerical variables. Cronbach's alpha was used to assess the internal consistency of the variables. Data analysis was performed using SPSS 28.0 (IBM Corp., Armonk, NY, USA), and a significance level of P < 0.05 was considered statistically significant.
3. Results
This study included 40 patients (58 % males, mean age 57 years). Most examinations (65 %) were performed using an MRI 3T, while the rest with an MRI 1.5T. For each level from L2 to S1, the grade of central, lateral, and foraminal stenosis were measured in the PRP and EXT positions and compared accordingly.
3.1. Change of the lordotic angle
As expected, the LA increased in EXT significantly (P = 0.0001) from 43.78° ± 12.14° in PRP to 53.65° ± 12.14° in EXT. In a previous upright-MRI study the LA in PRP was 45.42° ± 9.75° and 51.11 ± 11.33° in standing position (Papavero et al., 2022). Thus, the EXT simulated the standing LA quite well (Table 2).
Table 2.
The change in the dural sac surface area (DCSA), the yellow ligament surface area (YLSA), and the lordotic angle between the PRP and EXT position at all levels.
| Position |
P Value | |||
|---|---|---|---|---|
| PRP mean ± SD | EXT mean ± SD | Mean difference (95 % CI) | ||
| DCSA (mm2) | ||||
| L2-L3 | 138.83 ± 48.72 | 135.83 ± 47.1 | −2.99 (−6.11–0.124) | 0.59 |
| L3-L4 | 113.58 ± 55.48 | 106.36 ± 55.31 | −7.22 (−10.15–−4.28) | <0.0001∗ |
| L4-L5 | 100.34 ± 67.18 | 93.78 ± 61.43 | −6.57 (−10.13–−3) | 0.001∗ |
| L5-S1 | 100.8 ± 60.49 | 93.93 ± 54.8 | −6.88 (−11.15–−2.6) | 0.002∗ |
| YLSA (mm2) | ||||
| L2-L3 | 95.08 ± 24.52 | 111.3 ± 26.2 | 16.23 (12.8–19.66) | <0.0001∗ |
| L3-L4 | 110.43 ± 26.192 | 125.15 ± 28.43 | 14.73 (11.98–17.47) | <0.0001∗ |
| L4-L5 | 126.93 ± 29.191 | 147.75 ± 31.35 | 20.83 (15.94–25.71) | <0.0001∗ |
| L5-S1 | 100.55 ± 24.15 | 115.58 ± 26.11 | 15.03 (11.19–18.86) | <0.0001∗ |
| Lordotic Angle (°) | 43.78 ± 12.14 | 53.65 ± 12.14 | 9.98 (8.003–11.95) | <0.0001∗ |
∗ significant increase (p <0.005).
3.2. Change in dural cross-sectional area and yellow ligament surface area
The DCSA decreased significantly at all levels except for L2/L3. And the yellow ligament showed buckling in its shape in EXT and significant increase in its surface area at all levels. (Table 2).
3.3. Change of the grade of central stenosis
A significant increase (P = 0.011) of the grade of LSS was observed in the EXT position only at the level of L4/L5 and a trend (P = 0.059) at the level L3/L4. (Table 3). Qualitatively, at least two readers rated an increase in severity of LSS of at least one grade in 16/40 patients (40 %).
Table 3.
The change in the grade of central, lateral, and foraminal stenoses at four levels between the PRP and EXT.
| Grade |
P Value | ||||||
|---|---|---|---|---|---|---|---|
| 0 N(%) | 1 N(%) | 2 N(%) | 3 N(%) | Median Grade | |||
| Grade of central stenosis | |||||||
| L2-L3 | PRP/EXT | 30(75)/29(72.5) | 5(12.5)/5(12.5) | 5(12.5)/5(12.5) | 0/1(2.5) | 0/0 | 0.257 |
| L3-L4 | PRP/EXT | 19(47.5)/18(45) | 9(22.5)/8(20) | 8(20)/8(20) | 4(10)/4(10) | 1/1 | 0.059 |
| L4-L5 | PRP/EXT | 15(37.5)/13(32.5) | 8(20)7/17.5 | 4(10)/4(10) | 13(32.5)/16(40) | 1/1.5 | 0.011∗ |
| L5-S1 | PRP/EXT | 34(85)/34(85) | 4(10)/4(10) | 1(2.5)/0 | 1(2.5)/2(5) | 0/0 | 0.564 |
| Grade of Lateral stenosis | |||||||
| L2-L3 | PRP/EXT | 29(72.5)/27(67.5) | 10(25)/12(30) | 0/0 | 1(2.5)/1(2.5) | 0/0 | 0.564 |
| L3-L4 | PRP/EXT | 22(55)/17(42.5) | 8(20)/12(30) | 3(7.5)/3(7.5) | 7(17.5)/8(20) | 1/1 | 0.317 |
| L4-L5 | PRP/EXT | 14(35)/12(30) | 8(20)/8(20) | 4(10)/7(17.5) | 14(35)/13(32.5) | 0/1 | 0.014∗ |
| L5-S1 | PRP/EXT | 31(77.5)/31(77.5) | 6(15)/6(15) | 1(2.5)/1(2.5) | 2(5)/2(5) | 0/0 | 0.257 |
| Grade of foraminal stenosis | |||||||
| L2-L3 | PRP/EXT | 27(67.5)/26(65) | 10(25)/11(27.5) | 3(7.5)/3(7.5) | 0/0 | 0/0 | 0.564 |
| L3-L4 | PRP/EXT | 15(37.5)/16(40) | 16(40)/27(67.5) | 7(17.5)/6(15) | 2(5)/3(7.5) | 1/1 | 0.564 |
| L4-L5 | PRP/EXT | 8(20)/8(20) | 15(37.5)/13(32.5) | 12(30)/13(32.5) | 5(12.5)/6(15) | 1/1 | 0.763 |
| L5-S1 | PRP/EXT | 20(50)/23(57.5) | 11(27.5)/7(17.5) | 7(17.5)/8(20) | 2(5)/2(5) | 1/1 | 0.782 |
∗Significant increase (p <0.005).
3.4. Change of the grade of lateral recess stenosis
A significant increase in the grade of LRS was observed in the EXT position only at the level of L4-L5 (P = 0.014) (Table 3). In semiquantitative terms the severity of LRS increased in 15 % and 12.5 % at the levels L3/L4 and L4/L5, respectively. Qualitatively, at least two readers rated an increase in severity of LRS of at least one grade in 15/40 patients (37.5 %).
3.5. Change of the grade of foraminal stenosis
No significant increase in terms of classification severity was observed in the EXT position at all levels. Qualitatively, at least two readers rated an increase in severity of FoS of at least one grade in 7/40 patients (17.5 %), mostly at the L4/L5 level (Table 3).
3.6. Change of the RNR
No significant increase in terms of classification severity was observed in the EXT position at all levels. Qualitatively, at least two readers rated an increase in severity of RNR of at least one parameter in 7/40 patients (17.5 %), mostly at the L4/L5 level.
3.7. Reliability of the results
Regarding the grade of central stenosis in PRP and EXT, the kappa values showed substantial agreement between all readers. As for the grade of lateral stenosis, kappa showed substantial agreement between reader 1 vs 2 and reader 2 vs 3, whereas reader 1 vs 3 showed moderate agreement. For FoS, the Kappa analysis indicated moderate agreement between all readers in both positions. (Table 4).
Table 4.
Cohen's Kappa and Cronbach's Alpha values between the three readers for the types of stenosis at PRP and EXT position.
| Cohen's Kappa |
||||
|---|---|---|---|---|
| Type of stenosis | Reader 1 vs 2 | Reader 1 vs 3 | Reader 2 vs. 3 | Cronbach's α |
| Central RPR/EXT | 0.669/0.656 (Kubosch et al., 2015) | 0.725/0.707 (Kubosch et al., 2015) | 0.714/0.704 (Kubosch et al., 2015) | 0.967/0.971∗∗∗ |
| Lateral RPR/EXT | 0.637/0.613 (Kubosch et al., 2015) | 0.471/0.567 (Hebelka et al., 2022) | 0.654/0.646 (Kubosch et al., 2015) | 0.959/0.958∗∗∗ |
| Foraminal RPR/EXT | 0.488/0.535 (Hebelka et al., 2022) | 0.476/0.462 (Hebelka et al., 2022) | 0.600 (Kubosch et al., 2015)/0.517 (Hebelka et al., 2022) | 0.924/0.917∗∗∗ |
Cohen's Kappa (Hebelka et al., 2022): 0.4–0.6 moderate agreement (Kubosch et al., 2015), 0.6–0.8 substantial agreement (Madsen et al., 2008), ≥0.8 almost perfect agreement.
Cronbach's Alpha: ∗0.7–0.8 acceptable, ∗∗0.8–0.9 good, ∗∗∗ ≥0.9 excellent.
Cronbach's alpha analysis was conducted to determine internal consistency between readers in each grade and in both positions. Cronbach's alpha value indicates an excellent internal consistency between readers in all grades.
The high Pearson correlation coefficients for DCSA (PRP 0.961; EXT 0.956), YL (PRP 0.765; EXT 0.772) and LA (PRP 0.986; EXT 0.977) suggest excellent consistency among readers. (Table 5).
Table 5.
Pearson's correlation coefficient and Cronbach's Alpha values between three raters.
| Pearson's correlation coefficient |
Cronbach's Alpha | ||||||
|---|---|---|---|---|---|---|---|
| Rater 1 vs. 2 | P value | Rater 1 vs. 3 | P value | Rater 2 vs. 3 | P value | ||
| DCSA RPR | 0.914 | <0.0001 | 0.917 | <0.0001 | 0.916 | <0.0001 | 0.961∗ |
| DCSA EXT | 0.896 | <0.0001 | 0.883 | <0.0001 | 0.922 | <0.0001 | 0.956∗ |
| YLSA RPR | 0.455 | <0.0001 | 0.661 | <0.0001 | 0.437 | <0.0001 | 0.765∗∗ |
| YL SA EXT | 0.452 | <0.0001 | 0.641 | <0.0001 | 0.503 | <0.0001 | 0.772∗∗ |
| LA RPR | 0.948 | <0.0001 | 0.955 | <0.0001 | 0.974 | <0.0001 | 0.986∗ |
| LA EXT | 0.903 | <0.0001 | 0.951 | <0.0001 | 0.951 | <0.0001 | 0.977∗ |
p value <0.005 is significant.
Cronbach's Alpha: ∗ ≥0.9 excellent,∗∗ 0.7–0.8 acceptable.
Intra-rater reliability analysis was conducted for each reader; Pearson's correlation coefficient was used to determine intra-rater reliability, by assessing the correlation between two separate readings for each individual reader. All measured parameters demonstrated strong to excellent Pearson correlation coefficients, suggesting excellent intra-rater consistency.
The Cohen's Kappa analysis of central stenosis showed high intra-rater reliability, with Reader 3 showing excellent agreement, while Readers 2 and 1 demonstrated substantial agreement. Regarding lateral stenosis, agreement was more variable, with Reader 3 maintaining strong reliability, while Readers 2 and 1 showed moderate to substantial agreement. Regarding foraminal stenosis, it had the lowest intra-rater reliability, with Reader 3 showing substantial agreement, whereas Readers 2 and 1 exhibited only fair to moderate consistency.
A Bonferroni correction was applied in order to account for multiple comparisons across spinal levels and parameters. With 9 comparisons, the adjusted significance threshold was set at <0.0056. All comparisons remained statistically significant after correction, except for the DCSA measurement at the L2-L3 level (p = 0.59).
4. Discussion
Routine supine MRI often underestimates the severity of lumbar spinal canal stenosis due to the absence of gravitational effects, leading to discrepancies between imaging findings and patient symptoms. Studies, including those by Hong et al., Watanabe et al., Aaen et al., and Indrekvam et al. highlight the weak correlation between traditional MRI and clinical outcomes, emphasizing the need for alternative imaging techniques (Hong et al., 2015; Aaen et al., 2022; Watanabe et al., 2024; Indrekvam et al., 2023). Upright MRI or axial load devices have been shown to better assess LSS, detecting up to 85 % of changes missed by supine MRI (Madsen et al., 2008; Doktor et al., 2022). In a study by Madsen et al., the LA and YL thickness increased, while the DCSA decreased in the upright position (Madsen et al., 2008). Previous studies have also reported a stronger correlation between imaging findings and patient symptoms with the upright MRI (Tarantino et al., 2013). These methods provide a more accurate evaluation of spinal degeneration and stenosis, enhancing diagnostic accuracy and improving patient care, though they remain underutilized due to limited availability and lack of reimbursement in many areas.
Our study showed that EXT is an effective way to detect LSS. The combination of the decrease in DCSA and the increase in YLSA along with LA showed that this positioning increases sensitivity and specificity for LSS diagnosis. Kim et al. showed that YLSA is more sensitive than YL thickness (Kim et al., 2017).
Madsen et al. found that MRI with the patient in the supine position and legs straight gave similar results to upright MRI, regardless of axial loading (Madsen et al., 2008). The lumbar spine is more lordotic in an upright standing position than in other positions, that increases the LA and YLSA and reduces DCSA. This can contribute to canal stenosis. Hansen et al. found that LA increased by approximately 3.2° in upright, and by 12.8° when using the lumbar pillow in supine, compared to PRP. In addition, DCSA was significantly reduced both in standing and pillow-supine positions, compared to PRP, however, there was no significant difference in stenosis grading between upright and pillow-supine (Hansen et al., 2017). The results of our study indicated a significant decline in DCSA and a notable increase in LA in the EXT position, which is in concordance with the previous studies. It is easy to measure DCSA and LA in clinical practice. Papavero et al. found the lowest LA in the flexed position and the highest in the standing position (Papavero et al., 2022). People with stenosis often lean forward to ease pain, which reduces their natural lordosis. The EXT position makes LSS worse, causing pain during the scan. This was also noted by Hansen et al. (2017) We used an inflatable pillow to make the MRI more comfortable.
A statistically significant increase in the grade of LSS was observed in the EXT position only at the level of L4/L5, which is the most common level to be affected by degenerative changes, and a trend at the level L3/L4. However, using the Lee classification, at least two readers rated an increase in severity of LSS of at least one grade in 16/40 patients (40 %). This clearly demonstrates the relevance of the EXT-position-MRI in daily practice.
Lee and Schizas use morphological criteria, and not surface measurements, to assess central LSS. Two out of three readers rated an increase in central stenosis in 16/40 patients (40 %) (Charoensuk et al., 2023; Schizas et al., 2010).
In the EXT position, the YLSA increased at all levels, particularly at L4/L5, along with buckling, which worsened canal stenosis. The YL thickness increases with age, particularly at L4/L5 and it is important to distinguish between YL hypertrophy and buckling. Our study showed that buckling reduces the DCSA in the EXT position. This change was also seen in the MRI by Doktor et al. (2022) With advanced lumbar spine degenerative changes; the YL undergoes inward buckling rather than true hypertrophy, exacerbated by age-related fibrosis and increased collagen deposition, reducing elasticity and promoting canal narrowing during spinal extension (Yabe et al., 2024; Mihara et al., 2021).
L3/L4 and L4/L5 had the most pronounced increase in LRS. There is mixed evidence on how reliable MRI is for assessing nerve root problems and clinical symptoms. Some studies have found that MRI results can be unreliable. Two readers rated an increase in LRS in 15/40 patients (37.5 %).
Lee's MRI grading system for FoS correlates well with symptoms and intraoperative findings. EXT was not useful for detecting an increase in FoS (Lee et al., 2010). This may be because, unlike in upright MRI, there is no enlargement of the radicular arachnoid pocket due to gravity. Changes in foraminal morphology were seen in only 7/40 cases (17.5 %), mostly at the L4/L5 level. The moderate agreement between all readers is consistent with the observation by Speciale et al. that demonstrated poor to moderate inter and intra observer agreement for evaluation of foraminal stenosis in patients with symptomatic LSS (Speciale et al., 2002). In addition, a study by Banitalebi et al. and Doktor et al. found that there was only moderate inter observer agreement regarding facet joint osteoarthritic degenerative changes, which contributes significantly to foraminal stenosis (Banitalebi et al., 2022; Doktor et al., 2020). Banitalebi et al. found a moderate to substantial inter observer agreement for foraminal stenosis (0.42–0.77) which is in line with our findings (Banitalebi et al., 2022). Doktor et al. demonstrated that there was low inter observer agreement regarding positive degenerative pathologies between the supine and upright positions (Doktor et al., 2022). Yet, Cronbach's alpha analysis showed an excellent results indicating excellent internal consistency, these findings highlight the potential influence of subjective interpretation on these assessments. Alteration in foraminal geometry with advanced age and increased degeneration contributes to reduced foraminal height due to facet joint hypertrophy and osteophytes mainly in the lumbar spine's mechanically stressed zones like L4-L5 level (Al-Saeed et al., 2022).
RNR involvement was observed in cases of advanced stenosis, with changes in morphology and location between positions found only in 7/40 (17.5 %), mostly at the L4/L5 level. This may be due to the advanced stenosis in the PRP positions in a small cohort.
It is known from the literature that in lumbar spinal stenosis, MRI imaging does not necessarily correlate with symptoms. The combination of severe imaging with mild symptoms may justify conservative therapy or even a wait-and-see policy. On the other hand, clear symptoms without convincing imaging on PRP MRI often delay appropriate treatment. The EXT-MRI option is designed to address this discrepancy since it showed to increase the detection rate of lumbar central canal stenosis and is considered as an alternative to the upright MRI which is not readily available.
Limitations of our study included the small sample size of patients with stenosis. Future studies should include a larger number to provide robust results. In addition, comparison between the EXT and the upright position on a larger population is recommended to close the gap.
MRI scanner field strength (1.5T vs. 3T) can be a confounding factor in imaging, particularly when comparing results across different studies or when analyzing data longitudinally. To minimize this bias, the patients were scanned only once, and three radiologists analyzed the imaging twice.
5. Conclusion
The PRP/EXT modality detects central LSS in 40 % of borderline cases with posture-dependent symptoms or inconclusive results from a PRP-MRI. The EXT-MRI offers an acceptable level of comfort and ease of availability at a low cost, providing additional information that can influence clinical decisions.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: Prof F Kandziora
References
- Aaen J., Austevoll I.M., Hellum C., Storheim K., Myklebust T.Å., Banitalebi H., et al. vol. 31. Eur Spine J [Internet]; 2022. pp. 1391–1398. (Clinical and MRI Findings in Lumbar Spinal Stenosis: Baseline Data from the NORDSTEN Study). [DOI] [PubMed] [Google Scholar]
- Al-Saeed O., Joseph S., Khoumais N.A., Alkhawajah N.M., Al-Muhanna F.A., Al-Nemari, et al. MRI features of lumbar disc degeneration: prevalence and correlation with clinical findings. NeuroRadiol. J. 2022;35(Suppl. 2):19–27. doi: 10.1177/19714009221092891. [DOI] [Google Scholar]
- Banitalebi H., Espeland A., Anvar M., Hermansen E., Hellum C., Brox J.I., et al. Reliability of preoperative MRI findings in patients with lumbar spinal stenosis. BMC Musculoskelet Disord. 2022;23(1):1–9. doi: 10.1186/s12891-021-04949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartynski W.S., Lin L. Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR. 2003;24:348–360. [PMC free article] [PubMed] [Google Scholar]
- Charoensuk J., Laothamatas J., Sungkarat W., Worapruekjaru L., Hooncharoen B., Chousangsuntorn K. Axial loading during supine MRI for improved assessment of lumbar spine: comparison with standing MRI. Acta Radiol. 2023;64:217–227. doi: 10.1177/02841851211068148. [DOI] [PubMed] [Google Scholar]
- Doktor K., Jensen T.S., Christensen H.W., Fredberg U., Kindt M., Boyle E., et al. Degenerative findings in lumbar spine MRI: an inter-rater reliability study involving three raters. Chiropr. Man. Ther. 2020;28(1):1–10. doi: 10.1186/s12998-020-0297-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doktor K., Hartvigsen J., Hancock M., Christensen H.W., Fredberg U., Boyle E., Kindt M., Brix L., Jensen T.S. Reliability of reporting differences in degenerative MRI findings of the lumbar spine from the supine to the upright position. Skelet. Radiol. 2022;51:2141–2154. doi: 10.1007/s00256-022-04060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang X., Cui M., Wang Y., Liu L., Lv W., Ye H., Liu G. Effects of axial loading and positions on lumbar spinal stenosis: an MRI study using a new axial loading device. Skelet. Radiol. 2024 doi: 10.1007/s00256-024-04720-5. (online ahead of print) [DOI] [PubMed] [Google Scholar]
- Hansen B.B., Hansen P., Grindstedt J., Rasti Z., Bliddal H., Riis R.G.C., Boesen M. Conventional supine MRI with a lumbar pillow-an alternative to weight-bearing MRI for diagnosing spinal stenosis? A cross-sectional study. Spine. 2017;42:662–669. doi: 10.1097/BRS.0000000000001889. [DOI] [PubMed] [Google Scholar]
- Hebelka H., Rydberg N., Hutchins J., Lagerstrand K., Brisby H. Axial loading during MRI induces lumbar foraminal area changes and has the potential to improve diagnostics of nerve root compromise. J. Clin. Med. 2022;11:2122. doi: 10.3390/jcm11082122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong J.H., Lee M.Y., Jung S.W., Lee S.Y. Does spinal stenosis correlate with MRI findings and pain, psychologic factor and quality of life? Korean J. Anesthesiol. 2015;68:481–487. doi: 10.4097/kjae.2015.68.5.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indrekvam K., Banerud I.F., Hermansen E., Austevoll I.M., Rekeland F., Guddal M.H., et al. The Norvegian degenerative spondylolisthesis and spinal stenosis (NORDSTEN) study: study overview, organization structure and population study. Eur. Spine J. 2023;32:4162–4173. doi: 10.1007/s00586-023-0782. [DOI] [PubMed] [Google Scholar]
- Kim Yu, Park J.Y., Kim D.H., Karm M.H., Lee Jy, Yoo J.I., Chon S.W., Suh J.H. The role of ligamentum flavum area as a morphological parameter of lumbar central spinal stenosis. Pain Physician. 2017;20:E419–E424. [PubMed] [Google Scholar]
- Kubosch D., Vicari M., Siller A., Strohm P.C., Kubosch E.J., Knoeller S., Henning J., Suedkamp N.P., Izadpanah K. The lumbar spine as a dynamic structure depicted in upright MRI. Medicine. 2015;94 doi: 10.1097/MD.0000000000001299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Lee J.W., Yeom J.S., Ki-Jeong, Hyun-Jib K., Soo K.C., Heung S.K. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010;194:1095–1098. doi: 10.2214/AFR.09.2772. [DOI] [PubMed] [Google Scholar]
- Lee G.Y., Lee J.W., Choi H.S., Oh K., Kang H.S. A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skelet. Radiol. 2011;40:1033–1039. doi: 10.1007/s00256-011-1102-x. [DOI] [PubMed] [Google Scholar]
- Madsen R., Jensen T.S., Pope M., Soerensen J.S., Bendix T. The effect of body position and axial load on spinal canal morphology. Spine. 2008;33:61–67. doi: 10.1097/BRS.0b013e31815e395f. [DOI] [PubMed] [Google Scholar]
- Mihara A., Nishida N., Jiang F., Ohgi J., Imago Y., Suzuki H., et al. Tensile test of human lumbar ligamentum flavum: age-related changes of stiffness. Appl. Sci. 2021;11(8):3337. doi: 10.3390/aap11083337. [DOI] [Google Scholar]
- Papavero L., Marques C.J., Lohmann J., Fitting T., Schawjinski K., Ali N., et al. Redundant nerve roots in lumbar spinal stenosis: Inter- and intra-rater reliability of an MRI-based classification. Neuroradiology. 2020;62:223–230. doi: 10.1007/s00234-019-02337-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papavero L., Ali N., Schawjinski K., Holtdirk A., Maas R., St Ebert. The prevalence of redundant nerve roots in standing positional MRI decreases by half in supine and almost to zero in flexed seated position: a retrospective cross-sectional cohort study. Neuroradiology. 2022;64:2191–2201. doi: 10.1007/s00234-022-03047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schizas C., Theumann N., Burn A., Tansey R., Wardlaw D., Smith F.W., et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine. 2010;35(21):1919–1924. doi: 10.1097/BRS.0b013e3181d359bd. [DOI] [PubMed] [Google Scholar]
- Speciale A.C., Pietrobon R., Urban C.W., Richardson W.J., Helms C.A., Major N., et al. Observer variability in assessing lumbar spinal stenosis severity on magnetic resonance imaging and its relation to cross-sectional spinal canal area. Spine. 2002;27(10):1082–1086. doi: 10.1097/00007632-200205150-00014. [DOI] [PubMed] [Google Scholar]
- Tarantino U., Fanucci E., Iundusi R., Celi M., Altobelli S., Gasbarra E., et al. Lumbar spine MRI in upright position for diagnosing acute and chronic low back pain: statistical analysis of morphological changes. J. Orthop. Traumatol. Off J Italian Soc. Orthop Traumatol. 2013;14(1):15–22. doi: 10.1007/s10195-012-0213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K., Otani K., Nikaido T., Kato K., Kobayashi H., Yabuki S., et al. Time course of asymptomatic stenosis in multiple lumbar stenosis – Five-year results of selective decompression of symptomatic levels. Medicina. 2024;60:636. doi: 10.3390/medicina60040636. 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabe Y., Ishikawa K., Kurosawa D., Murakami E., Aizawa T. Buckling of the ligmentum flavum in patients with lumbar spinal canal stenosis. Spine. 2024;49(17):E284–E290. doi: 10.1097/BRS.00000000000004941. [DOI] [PubMed] [Google Scholar]