Abstract
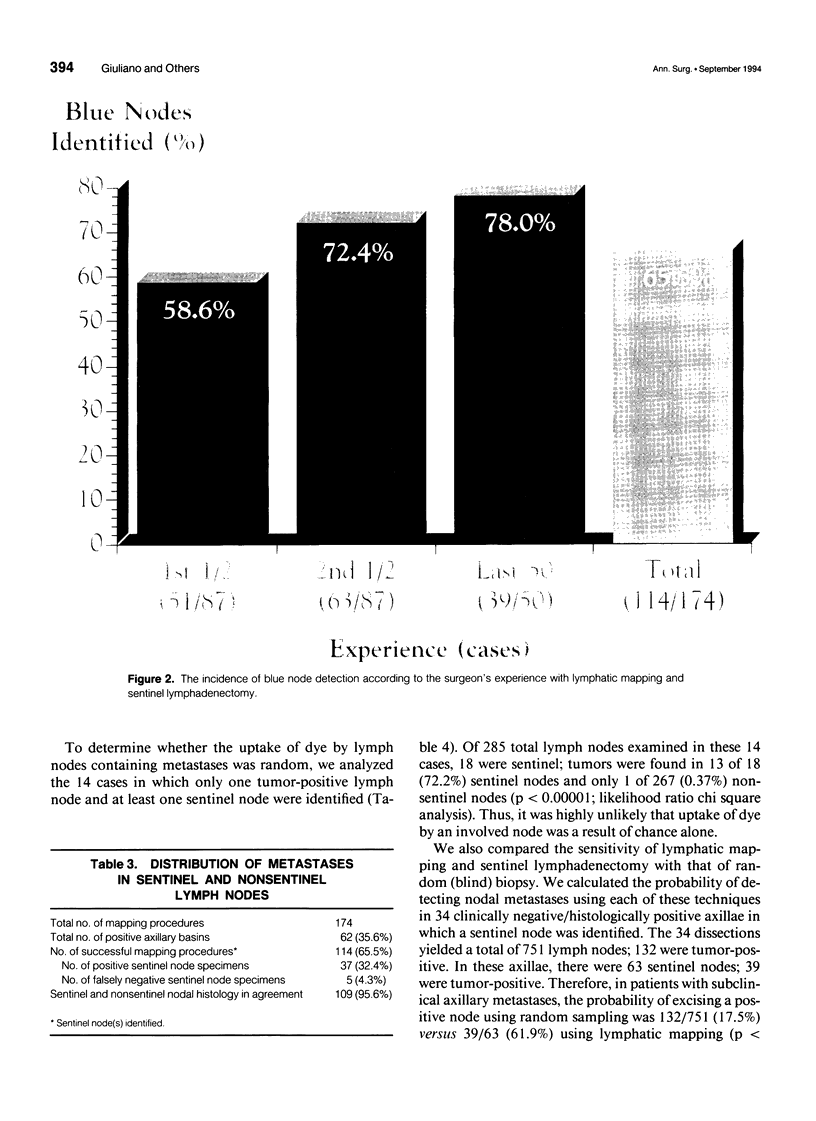
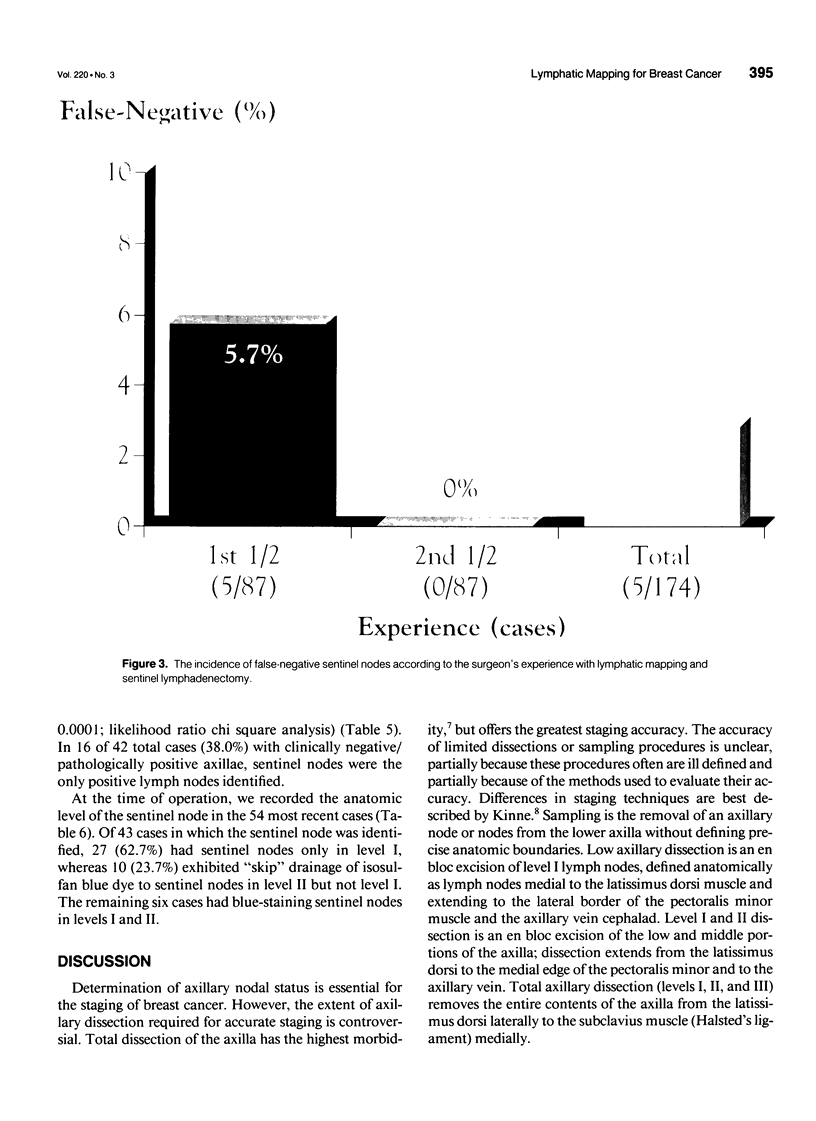
OBJECTIVE: The authors report the feasibility and accuracy of intraoperative lymphatic mapping with sentinel lymphadenectomy in patients with breast cancer. SUMMARY BACKGROUND DATA: Axillary lymph node dissection (ALND) for breast cancer generally is accepted for its staging and prognostic value, but the extent of dissection remains controversial. Blind lymph node sampling or level I dissection may miss some nodal metastases, but ALND may result in lymphedema. In melanoma, intraoperative lymph node mapping with sentinel lymphadenectomy is an effective and minimally invasive alternative to ALND for identifying nodes containing metastases. METHODS: One hundred seventy-four mapping procedures were performed using a vital dye injected at the primary breast cancer site. Axillary lymphatics were identified and followed to the first ("sentinel") node, which was selectively excised before ALND. RESULTS: Sentinel nodes were identified in 114 of 174 (65.5%) procedures and accurately predicted axillary nodal status in 109 of 114 (95.6%) cases. There was a definite learning curve, and all false-negative sentinel nodes occurred in the first part of the study; sentinel nodes identified in the last 87 procedures were 100% predictive. In 16 of 42 (38.0%) clinically negative/pathologically positive axillae, the sentinel node was the only tumor-involved lymph node identified. The anatomic location of the sentinel node was examined in the 54 most recent procedures; ten cases had only level II nodal metastases that could have been missed by sampling or low (level I) axillary dissection. CONCLUSIONS: This experience indicates that intraoperative lymphatic mapping can accurately identify the sentinel node--i.e., the axillary lymph node most likely to contain breast cancer metastases--in some patients. The technique could enhance staging accuracy and, with further refinements and experience, might alter the role of ALND.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ball A. B., Waters R., Fish S., Thomas J. M. Radical axillary dissection in the staging and treatment of breast cancer. Ann R Coll Surg Engl. 1992 Mar;74(2):126–129. [PMC free article] [PubMed] [Google Scholar]
- Benson E. A., Thorogood J. The effect of surgical technique on local recurrence rates following mastectomy. Eur J Surg Oncol. 1986 Sep;12(3):267–271. [PubMed] [Google Scholar]
- Boova R. S., Bonanni R., Rosato F. E. Patterns of axillary nodal involvement in breast cancer. Predictability of level one dissection. Ann Surg. 1982 Dec;196(6):642–644. doi: 10.1097/00000658-198212001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabanes P. A., Salmon R. J., Vilcoq J. R., Durand J. C., Fourquet A., Gautier C., Asselain B. Value of axillary dissection in addition to lumpectomy and radiotherapy in early breast cancer. The Breast Carcinoma Collaborative Group of the Institut Curie. Lancet. 1992 May 23;339(8804):1245–1248. doi: 10.1016/0140-6736(92)91591-u. [DOI] [PubMed] [Google Scholar]
- Davies G. C., Millis R. R., Hayward J. L. Assessment of axillary lymph node status. Ann Surg. 1980 Aug;192(2):148–151. doi: 10.1097/00000658-198008000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher B., Wolmark N., Bauer M., Redmond C., Gebhardt M. The accuracy of clinical nodal staging and of limited axillary dissection as a determinant of histologic nodal status in carcinoma of the breast. Surg Gynecol Obstet. 1981 Jun;152(6):765–772. [PubMed] [Google Scholar]
- Fisher C. J., Boyle S., Burke M., Price A. B. Intraoperative assessment of nodal status in the selection of patients with breast cancer for axillary clearance. Br J Surg. 1993 Apr;80(4):457–458. doi: 10.1002/bjs.1800800416. [DOI] [PubMed] [Google Scholar]
- Forrest A. P., Roberts M. M., Cant E., Shivas A. Simple mastectomy and pectoral node biopsy. Br J Surg. 1976 Aug;63(8):569–575. doi: 10.1002/bjs.1800630802. [DOI] [PubMed] [Google Scholar]
- Forrest A. P., Stewart H. J., Roberts M. M., Steele R. J. Simple mastectomy and axillary node sampling (pectoral node biopsy) in the management of primary breast cancer. Ann Surg. 1982 Sep;196(3):371–378. doi: 10.1097/00000658-198209000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graversen H. P., Blichert-Toft M., Andersen J. A., Zedeler K. Breast cancer: risk of axillary recurrence in node-negative patients following partial dissection of the axilla. Eur J Surg Oncol. 1988 Oct;14(5):407–412. [PubMed] [Google Scholar]
- Kinne D. W. Controversies in primary breast cancer management. Am J Surg. 1993 Nov;166(5):502–508. doi: 10.1016/s0002-9610(05)81144-4. [DOI] [PubMed] [Google Scholar]
- Kissin M. W., Thompson E. M., Price A. B., Slavin G., Kark A. E. The inadequacy of axillary sampling in breast cancer. Lancet. 1982 May 29;1(8283):1210–1212. doi: 10.1016/s0140-6736(82)92337-6. [DOI] [PubMed] [Google Scholar]
- Kitchen P. R., McLennan R., Mursell A. Node-positive breast cancer: a comparison of clinical and pathological findings and assessment of axillary clearance. Aust N Z J Surg. 1980 Dec;50(6):580–583. doi: 10.1111/j.1445-2197.1980.tb04200.x. [DOI] [PubMed] [Google Scholar]
- Kjaergaard J., Blichert-Toft M., Andersen J. A., Rank F., Pedersen B. V. Probability of false negative nodal staging in conjunction with partial axillary dissection in breast cancer. Br J Surg. 1985 May;72(5):365–367. doi: 10.1002/bjs.1800720511. [DOI] [PubMed] [Google Scholar]
- Mathiesen O., Carl J., Bonderup O., Panduro J. Axillary sampling and the risk of erroneous staging of breast cancer. An analysis of 960 consecutive patients. Acta Oncol. 1990;29(6):721–725. doi: 10.3109/02841869009092990. [DOI] [PubMed] [Google Scholar]
- Moffat F. L., Jr, Senofsky G. M., Davis K., Clark K. C., Robinson D. S., Ketcham A. S. Axillary node dissection for early breast cancer: some is good, but all is better. J Surg Oncol. 1992 Sep;51(1):8–13. doi: 10.1002/jso.2930510105. [DOI] [PubMed] [Google Scholar]
- Morton D. L., Wen D. R., Wong J. H., Economou J. S., Cagle L. A., Storm F. K., Foshag L. J., Cochran A. J. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992 Apr;127(4):392–399. doi: 10.1001/archsurg.1992.01420040034005. [DOI] [PubMed] [Google Scholar]
- Musumeci R., Tesoro-Tess J. D., Costa A., Veronesi U. Indirect lymphography of the breast with iotasul: a vanishing hope? Lymphology. 1984 Dec;17(4):118–123. [PubMed] [Google Scholar]
- Nieweg O. E., Kim E. E., Wong W. H., Broussard W. F., Singletary S. E., Hortobagyi G. N., Tilbury R. S. Positron emission tomography with fluorine-18-deoxyglucose in the detection and staging of breast cancer. Cancer. 1993 Jun 15;71(12):3920–3925. doi: 10.1002/1097-0142(19930615)71:12<3920::aid-cncr2820711220>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Pigott J., Nichols R., Maddox W. A., Balch C. M. Metastases to the upper levels of the axillary nodes in carcinoma of the breast and its implications for nodal sampling procedures. Surg Gynecol Obstet. 1984 Mar;158(3):255–259. [PubMed] [Google Scholar]
- Rosen P. P., Lesser M. L., Kinne D. W., Beattie E. J. Discontinuous or "skip" metastases in breast carcinoma. Analysis of 1228 axillary dissections. Ann Surg. 1983 Mar;197(3):276–283. doi: 10.1097/00000658-198303000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacre R. A. Clinical evaluation of axillar lymph nodes compared to surgical and pathological findings. Eur J Surg Oncol. 1986 Jun;12(2):169–173. [PubMed] [Google Scholar]
- Senofsky G. M., Moffat F. L., Jr, Davis K., Masri M. M., Clark K. C., Robinson D. S., Sabates B., Ketcham A. S. Total axillary lymphadenectomy in the management of breast cancer. Arch Surg. 1991 Nov;126(11):1336–1342. doi: 10.1001/archsurg.1991.01410350026004. [DOI] [PubMed] [Google Scholar]
- Shaw J. H., Rumball E. M. Complications and local recurrence following lymphadenectomy. Br J Surg. 1990 Jul;77(7):760–764. doi: 10.1002/bjs.1800770715. [DOI] [PubMed] [Google Scholar]
- Smith J. A., 3rd, Gamez-Araujo J. J., Gallager H. S., White E. C., McBride C. M. Carcinoma of the breast: analysis of total lymph node involvement versus level of metastasis. Cancer. 1977 Feb;39(2):527–532. doi: 10.1002/1097-0142(197702)39:2<527::aid-cncr2820390221>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Steele R. J., Forrest A. P., Gibson T., Stewart H. J., Chetty U. The efficacy of lower axillary sampling in obtaining lymph node status in breast cancer: a controlled randomized trial. Br J Surg. 1985 May;72(5):368–369. doi: 10.1002/bjs.1800720512. [DOI] [PubMed] [Google Scholar]
- Veronesi U., Luini A., Galimberti V., Marchini S., Sacchini V., Rilke F. Extent of metastatic axillary involvement in 1446 cases of breast cancer. Eur J Surg Oncol. 1990 Apr;16(2):127–133. [PubMed] [Google Scholar]
- Veronesi U., Rilke F., Luini A., Sacchini V., Galimberti V., Campa T., Dei Bei E., Greco M., Magni A., Merson M. Distribution of axillary node metastases by level of invasion. An analysis of 539 cases. Cancer. 1987 Feb 15;59(4):682–687. doi: 10.1002/1097-0142(19870215)59:4<682::aid-cncr2820590403>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Wilking N., Rutqvist L. E., Carstensen J., Mattsson A., Skoog L. Prognostic significance of axillary nodal status in primary breast cancer in relation to the number of resected nodes. Stockholm Breast Cancer Study Group. Acta Oncol. 1992;31(1):29–35. doi: 10.3109/02841869209088261. [DOI] [PubMed] [Google Scholar]