Abstract
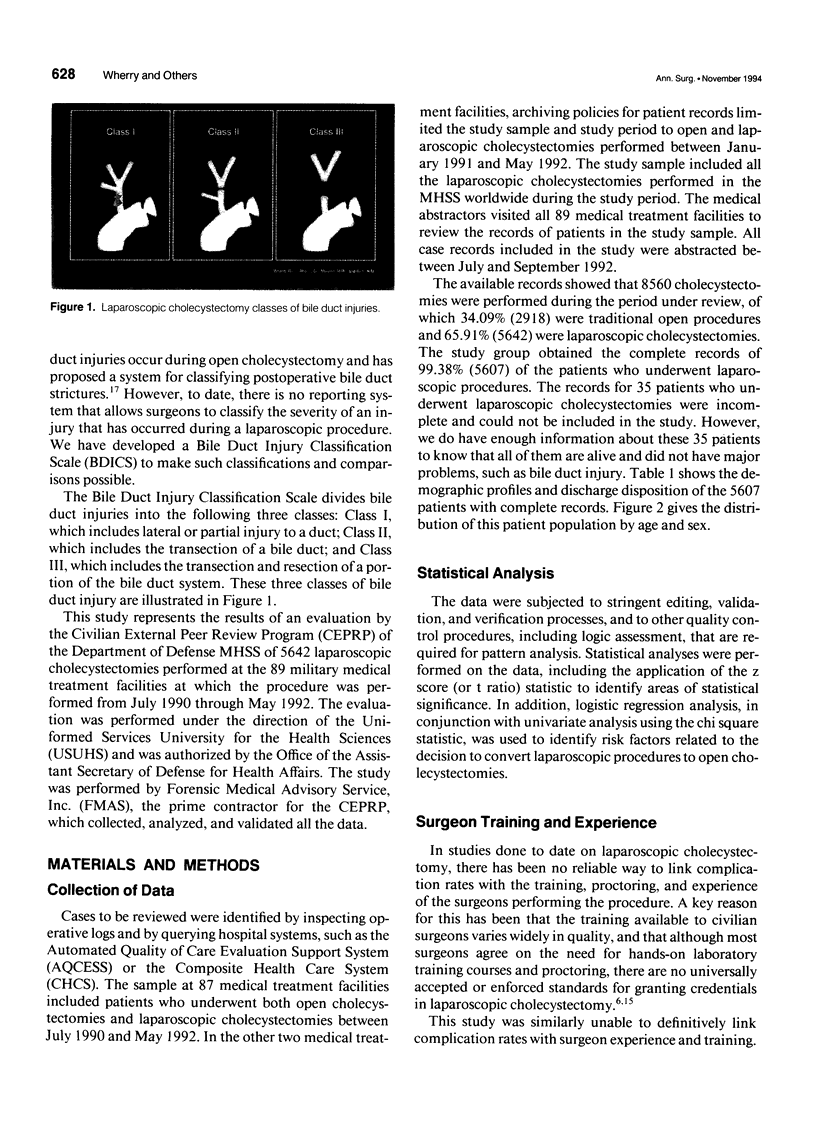
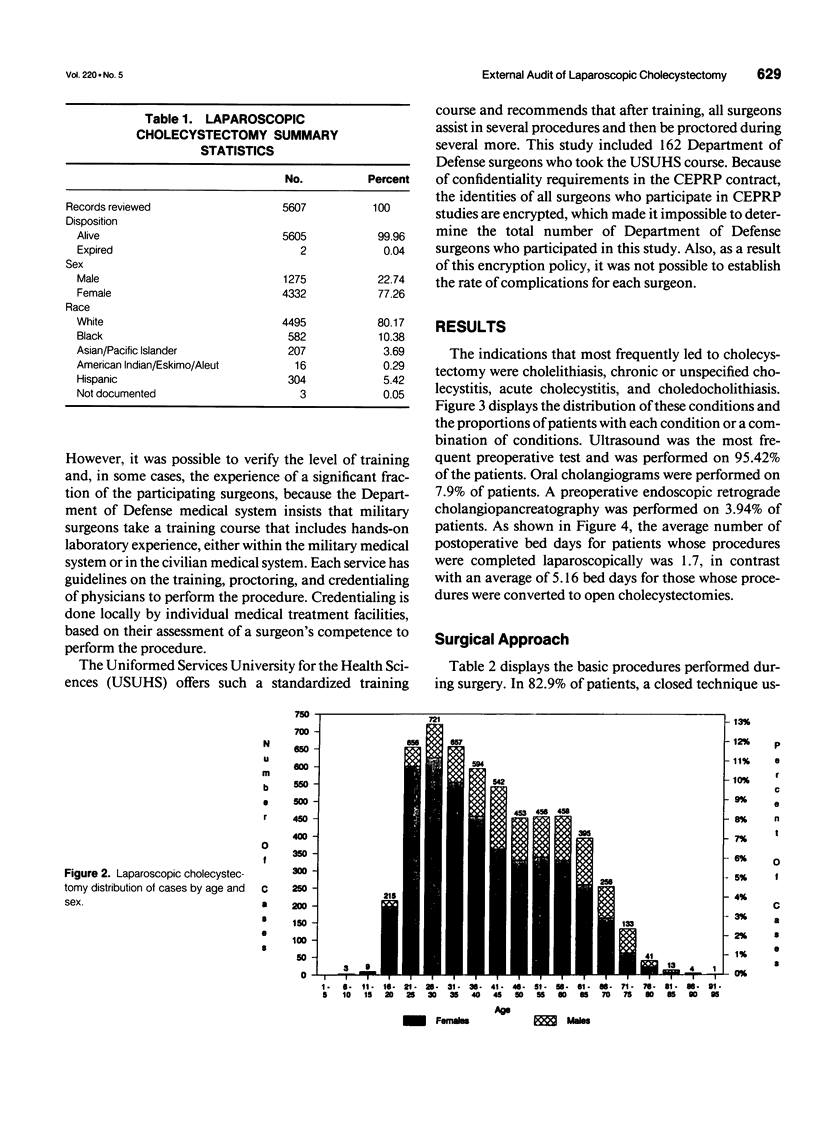
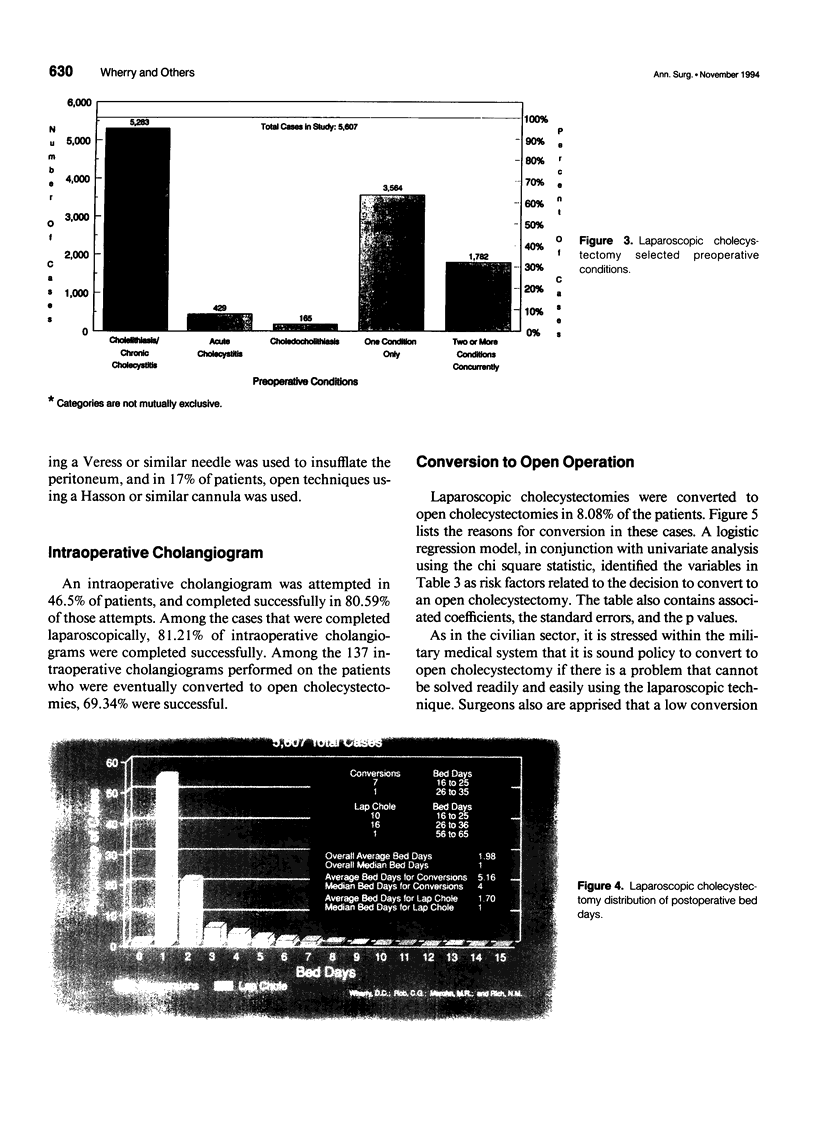
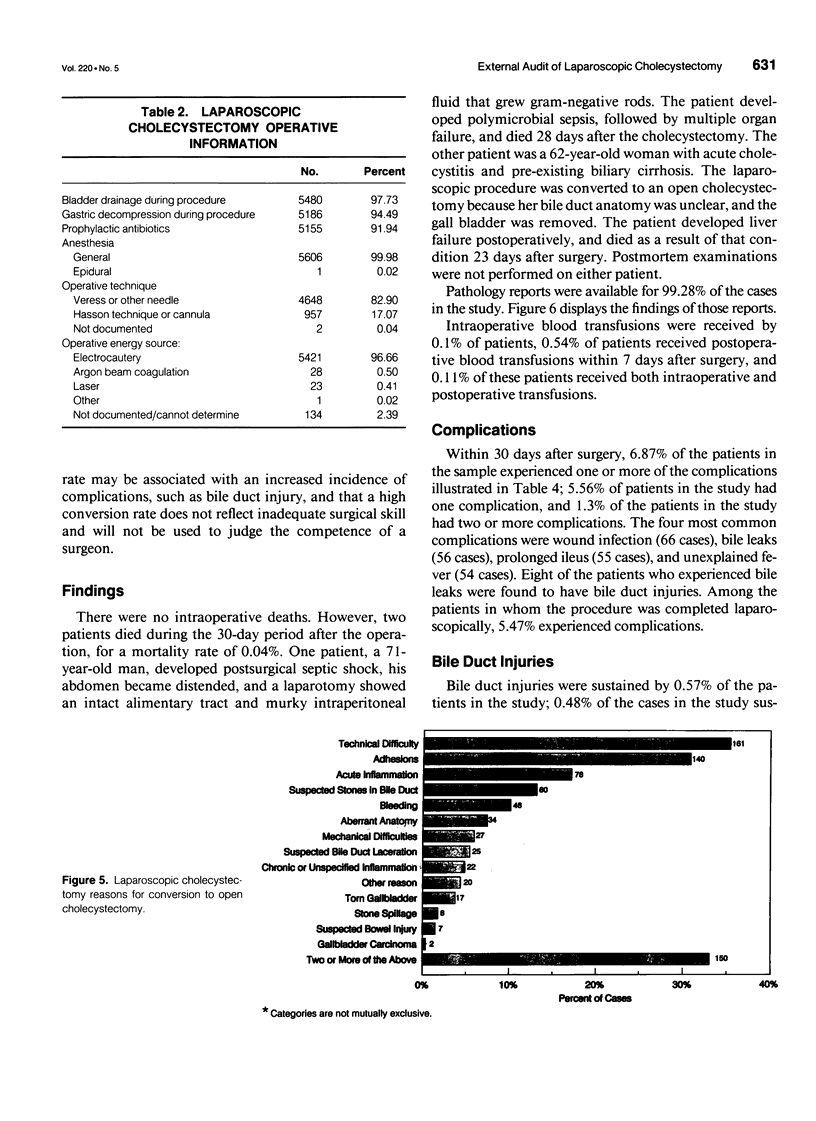
OBJECTIVE: This study provided an objective survey by an outside auditing group of a large, complete patient population undergoing laparoscopic cholecystectomies, determined the frequency of complications, especially bile duct injuries, and presented a system for classifying and comparing the severity of bile duct injuries. SUMMARY BACKGROUND DATA: This is the first study of laparoscopic cholecystectomy to encompass a large and complete patient population and to be based on objectively collected data rather than self-reported data. The Civilian External Peer Review Program (CEPRP) of the Department of Defense health care system conducted a retrospective study of 5642 patients who underwent laparoscopic cholecystectomies at 89 military medical treatment facilities from July 1990 through May 1992. METHODS: The study sample consisted of the complete records of 5607 (99.38%) of the 5642 laparoscopic cholecystectomy patients. RESULTS: Of the sample, 6.87% of patients experienced complications within 30 days of surgery, 0.57% sustained bile duct injuries, and 0.5% sustained bowel injuries. Among 5154 patients whose procedures were completed laparoscopically, 5.47% experienced complications. Laparoscopic procedures were converted to open cholecystectomies in 8.08% of cases. Intraoperative cholangiograms were attempted in 46.5% of cases and completed in 80.59% of those attempts. There were no intraoperative deaths; 0.04% of the patients died within 30 days of surgery. CONCLUSIONS: The frequency of complications found in this study is comparable to the frequency of complications reported in recent large civilian studies and earlier, smaller studies. The authors present a system for classifying bile duct injuries, which is designed to standardize references to such injuries and allow for accurate comparison of bile duct injuries in the future.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med. 1991 Apr 18;324(16):1073–1078. doi: 10.1056/NEJM199104183241601. [DOI] [PubMed] [Google Scholar]
- Airan M., Appel M., Berci G., Coburg A. J., Cohen M., Cuschieri A., Dent T., Duppler D., Easter D., Greene F. Retrospective and prospective multi-institutional laparoscopic cholecystectomy study organized by the Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 1992 Jul-Aug;6(4):169–178. doi: 10.1007/BF02210874. [DOI] [PubMed] [Google Scholar]
- Berci G., Sackier J. M. The Los Angeles experience with laparoscopic cholecystectomy. Am J Surg. 1991 Mar;161(3):382–384. doi: 10.1016/0002-9610(91)90602-a. [DOI] [PubMed] [Google Scholar]
- Cuschieri A., Dubois F., Mouiel J., Mouret P., Becker H., Buess G., Trede M., Troidl H. The European experience with laparoscopic cholecystectomy. Am J Surg. 1991 Mar;161(3):385–387. doi: 10.1016/0002-9610(91)90603-b. [DOI] [PubMed] [Google Scholar]
- Cuschieri A. Reflections on surgical training. Surg Endosc. 1993 Mar-Apr;7(2):73–74. doi: 10.1007/BF00704380. [DOI] [PubMed] [Google Scholar]
- Davidoff A. M., Pappas T. N., Murray E. A., Hilleren D. J., Johnson R. D., Baker M. E., Newman G. E., Cotton P. B., Meyers W. C. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992 Mar;215(3):196–202. doi: 10.1097/00000658-199203000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deziel D. J., Millikan K. W., Economou S. G., Doolas A., Ko S. T., Airan M. C. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993 Jan;165(1):9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- Forde K. A. Endosurgical training methods: is it surgical training that is out of control? Surg Endosc. 1993 Mar-Apr;7(2):71–72. doi: 10.1007/BF00704379. [DOI] [PubMed] [Google Scholar]
- Hunter J. G. Avoidance of bile duct injury during laparoscopic cholecystectomy. Am J Surg. 1991 Jul;162(1):71–76. doi: 10.1016/0002-9610(91)90207-t. [DOI] [PubMed] [Google Scholar]
- McSherry C. K., Glenn F. The incidence and causes of death following surgery for nonmalignant biliary tract disease. Ann Surg. 1980 Mar;191(3):271–275. doi: 10.1097/00000658-198003000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen D. O. Laparoscopic cholecystectomy. Am J Surg. 1991 Mar;161(3):339–344. doi: 10.1016/0002-9610(91)90592-2. [DOI] [PubMed] [Google Scholar]
- Orlando R., 3rd, Russell J. C., Lynch J., Mattie A. Laparoscopic cholecystectomy. A statewide experience. The Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1993 May;128(5):494–499. doi: 10.1001/archsurg.1993.01420170024002. [DOI] [PubMed] [Google Scholar]
- Peters J. H., Ellison E. C., Innes J. T., Liss J. L., Nichols K. E., Lomano J. M., Roby S. R., Front M. E., Carey L. C. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991 Jan;213(1):3–12. doi: 10.1097/00000658-199101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postgraduate course on interventional laparoscopy. 1990 Clinical Congress of the American College of Surgeons. October 1990. Am J Surg. 1991 Mar;161(3):323–409. [PubMed] [Google Scholar]
- Schirmer B. D., Edge S. B., Dix J., Hyser M. J., Hanks J. B., Jones R. S. Laparoscopic cholecystectomy. Treatment of choice for symptomatic cholelithiasis. Ann Surg. 1991 Jun;213(6):665–677. doi: 10.1097/00000658-199106000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott T. R., Zucker K. A., Bailey R. W. Laparoscopic cholecystectomy: a review of 12,397 patients. Surg Laparosc Endosc. 1992 Sep;2(3):191–198. [PubMed] [Google Scholar]