Abstract
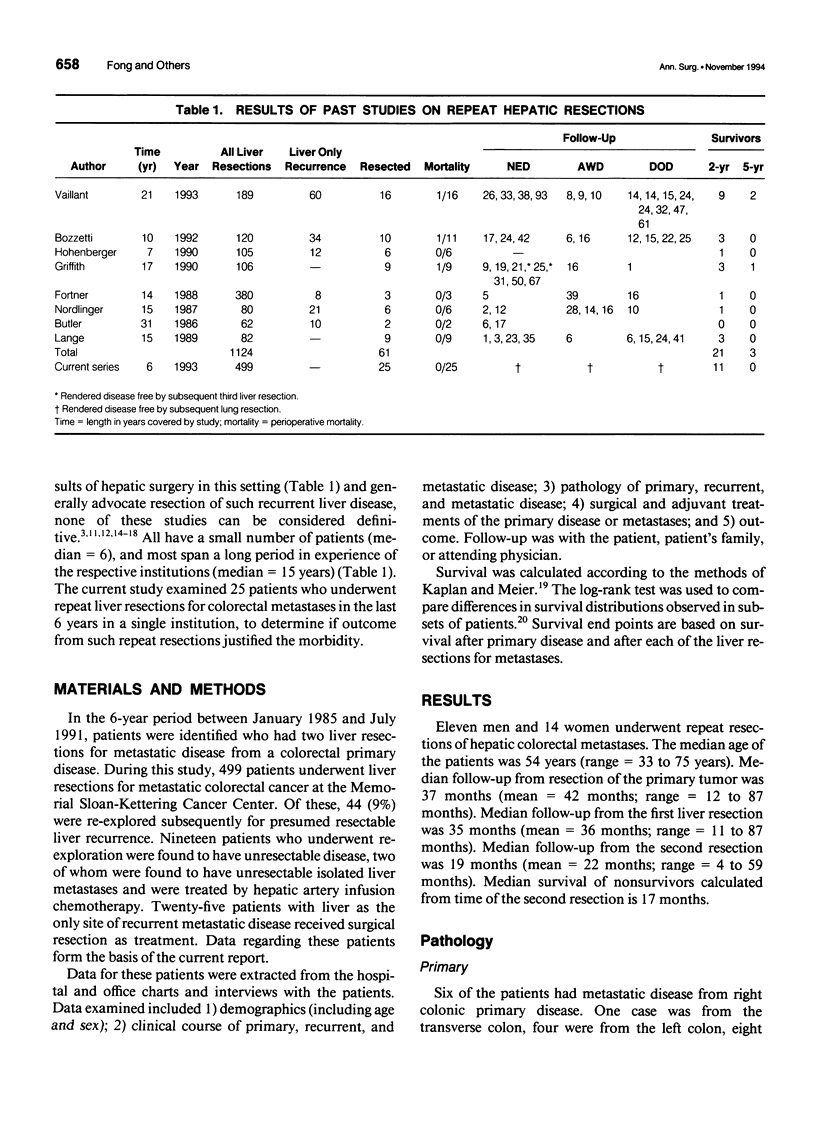
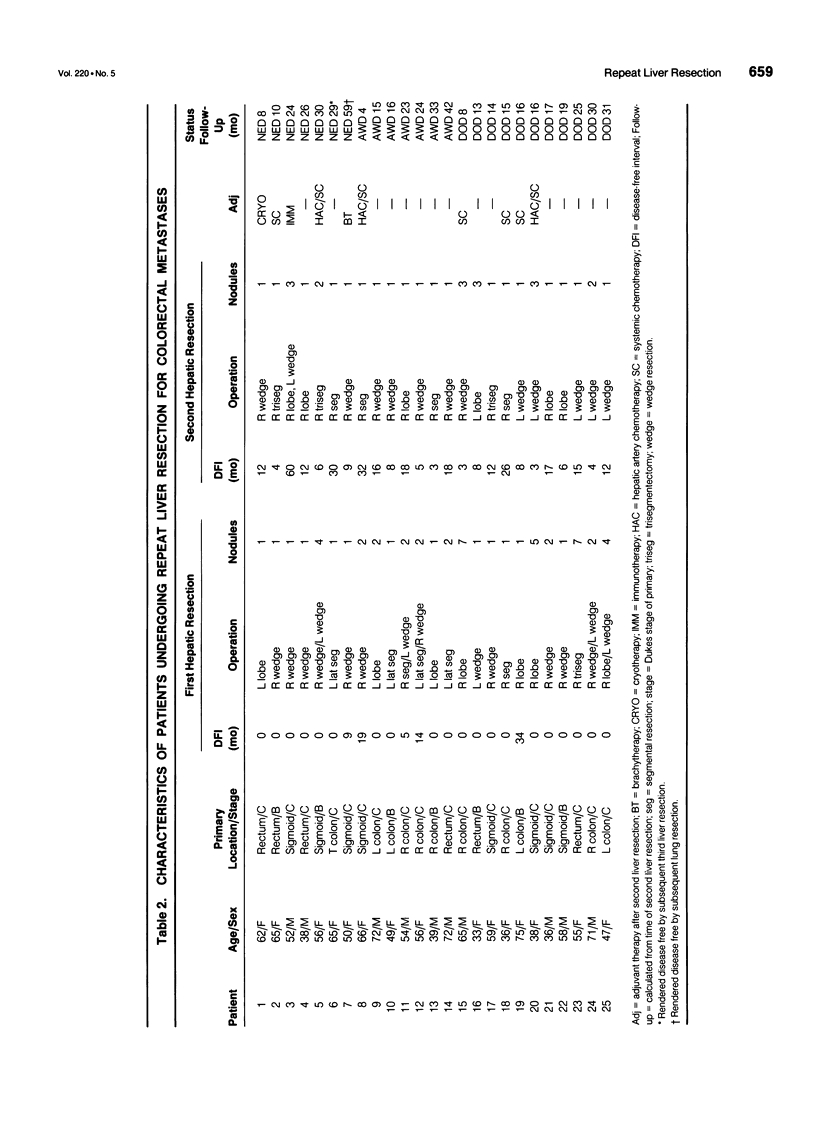
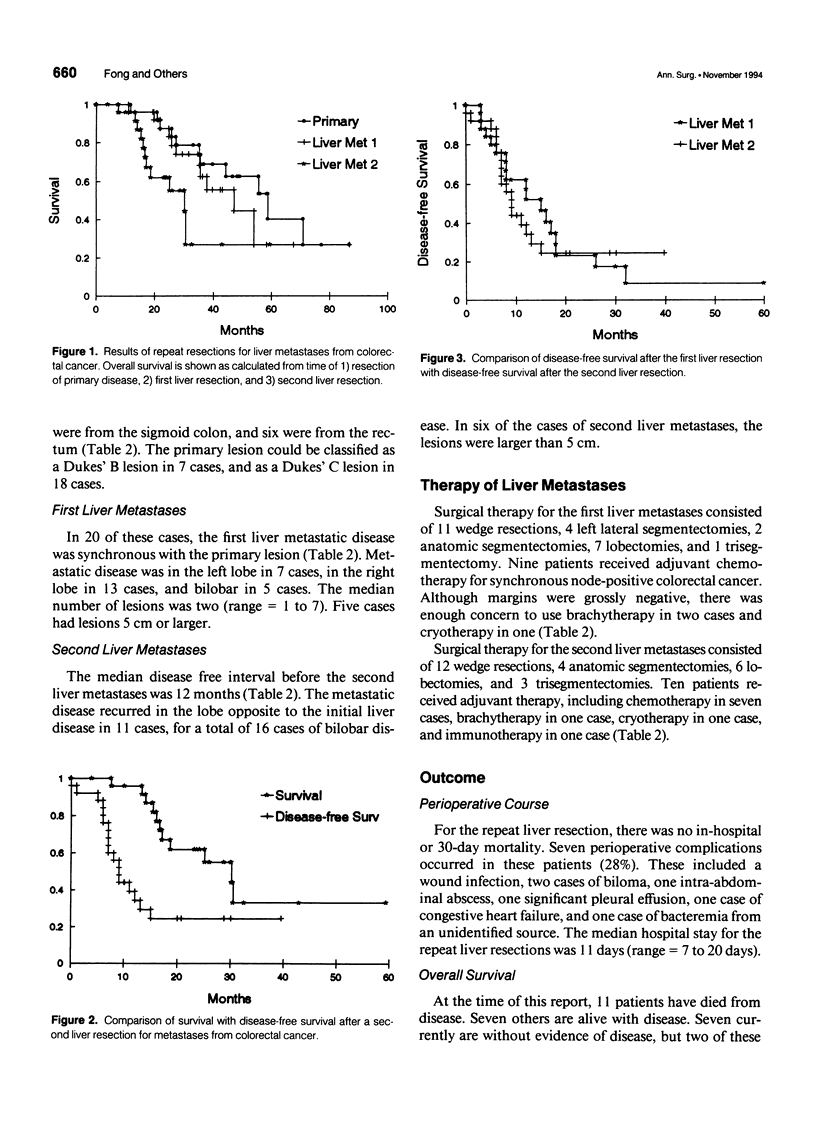
OBJECTIVE: The authors weighed the risks and benefits of repeat liver resections for colorectal metastatic disease. METHOD: In the 6-year period between January 1985 and June 1991, 499 patients underwent liver resections for colorectal metastases at the Memorial Sloan-Kettering Cancer Center. Of these, 25 patients had repeat surgical resections for isolated recurrent disease to the liver. The clinical data for these patients were reviewed. RESULTS: The median interval between the two resections was 11 months. There were no perioperative deaths, and the complication rate was 28%. Median follow-up after the second liver resection is 19 months, with median survival of 17 months for nonsurvivors. Although the median survival after the second resection is 30 months, 20 of the 25 patients have had recurrences with a median disease-free interval of only 9 months. No characteristic of primary or metastatic disease predicted outcome, including time between presentation of the primary and development of liver metastases, disease-free interval after the first liver resection, and bilobar liver involvement. CONCLUSIONS: Although repeat liver resections can be performed safely and improves survival, the likelihood of cure from such resection therapy is low. This likelihood of further recurrences encourage studies of adjuvant or alternative treatments of this population.
Full text
PDF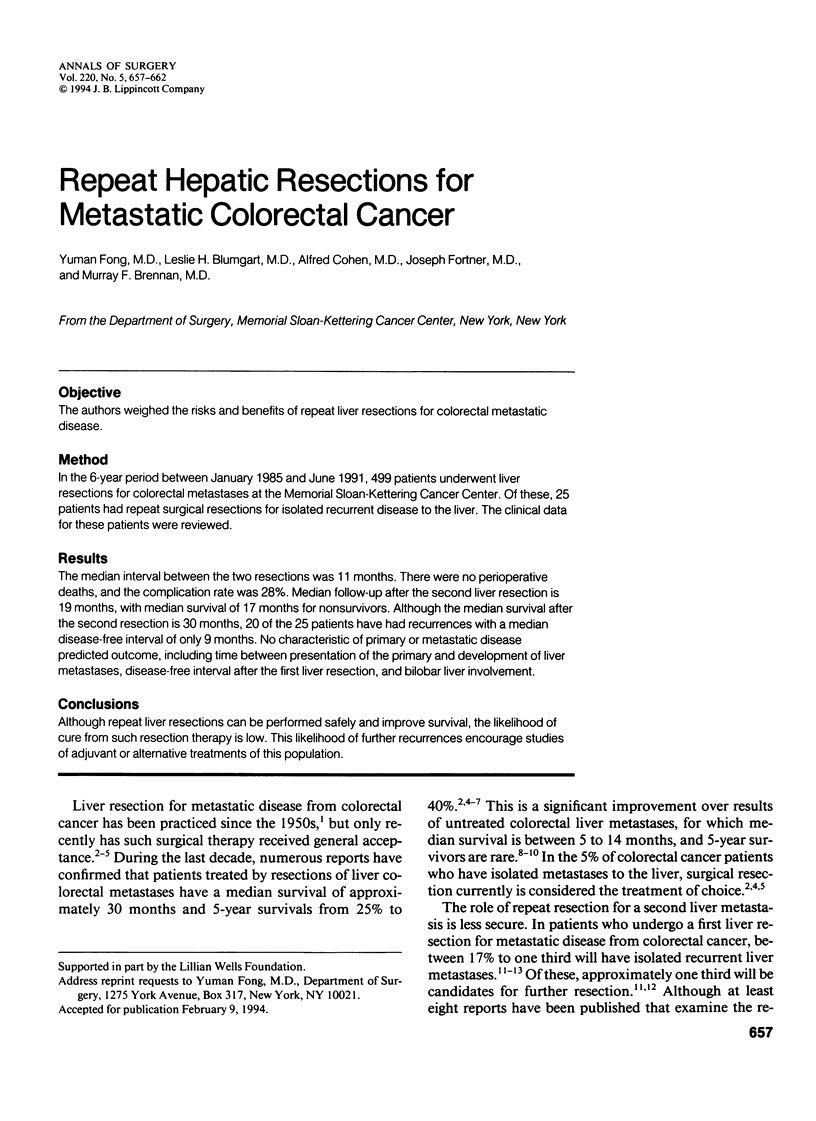
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abrams M. S., Lerner H. J. Survival of patients at Pennsylvania Hospital with hepatic metastases from carcinoma of the colon and rectum. Dis Colon Rectum. 1971 Nov-Dec;14(6):431–434. doi: 10.1007/BF02553467. [DOI] [PubMed] [Google Scholar]
- Bozzetti F., Bignami P., Montalto F., Doci R., Gennari L. Repeated hepatic resection for recurrent metastases from colorectal cancer. Br J Surg. 1992 Feb;79(2):146–148. doi: 10.1002/bjs.1800790216. [DOI] [PubMed] [Google Scholar]
- Bozzetti F., Doci R., Bignami P., Morabito A., Gennari L. Patterns of failure following surgical resection of colorectal cancer liver metastases. Rationale for a multimodal approach. Ann Surg. 1987 Mar;205(3):264–270. doi: 10.1097/00000658-198703000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler J., Attiyeh F. F., Daly J. M. Hepatic resection for metastases of the colon and rectum. Surg Gynecol Obstet. 1986 Feb;162(2):109–113. [PubMed] [Google Scholar]
- Cady B., McDermott W. V. Major hepatic resection for metachronous metastases from colon cancer. Ann Surg. 1985 Feb;201(2):204–209. doi: 10.1097/00000658-198502000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortner J. G. Recurrence of colorectal cancer after hepatic resection. Am J Surg. 1988 Mar;155(3):378–382. doi: 10.1016/s0002-9610(88)80086-2. [DOI] [PubMed] [Google Scholar]
- Fortner J. G., Silva J. S., Golbey R. B., Cox E. B., Maclean B. J. Multivariate analysis of a personal series of 247 consecutive patients with liver metastases from colorectal cancer. I. Treatment by hepatic resection. Ann Surg. 1984 Mar;199(3):306–316. doi: 10.1097/00000658-198403000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohenberger P., Schlag P., Schwarz V., Herfarth C. Tumor recurrence and options for further treatment after resection of liver metastases in patients with colorectal cancer. J Surg Oncol. 1990 Aug;44(4):245–251. doi: 10.1002/jso.2930440411. [DOI] [PubMed] [Google Scholar]
- Jaffe B. M., Donegan W. L., Watson F., Spratt J. S., Jr Factors influencing survival in patients with untreated hepatic metastases. Surg Gynecol Obstet. 1968 Jul;127(1):1–11. [PubMed] [Google Scholar]
- Kemeny N., Schneider A. Regional treatment of hepatic metastases and hepatocellular carcinoma. Curr Probl Cancer. 1989 Jul-Aug;13(4):197–283. doi: 10.1016/0147-0272(89)90007-x. [DOI] [PubMed] [Google Scholar]
- Lange J. F., Leese T., Castaing D., Bismuth H. Repeat hepatectomy for recurrent malignant tumors of the liver. Surg Gynecol Obstet. 1989 Aug;169(2):119–126. [PubMed] [Google Scholar]
- Nordlinger B., Quilichini M. A., Parc R., Hannoun L., Delva E., Huguet C. Hepatic resection for colorectal liver metastases. Influence on survival of preoperative factors and surgery for recurrences in 80 patients. Ann Surg. 1987 Mar;205(3):256–263. doi: 10.1097/00000658-198703000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PESTANA C., REITEMEIER R. J., MOERTEL C. G., JUDD E. S., DOCKERTY M. B. THE NATURAL HISTORY OF CARCINOMA OF THE COLON AND RECTUM. Am J Surg. 1964 Dec;108:826–829. doi: 10.1016/0002-9610(64)90041-8. [DOI] [PubMed] [Google Scholar]
- Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of indications for resection. Registry of Hepatic Metastases. Surgery. 1988 Mar;103(3):278–288. [PMC free article] [PubMed] [Google Scholar]
- Scheele J., Stangl R., Altendorf-Hofmann A., Gall F. P. Indicators of prognosis after hepatic resection for colorectal secondaries. Surgery. 1991 Jul;110(1):13–29. [PubMed] [Google Scholar]
- Scheele J., Stangl R., Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg. 1990 Nov;77(11):1241–1246. doi: 10.1002/bjs.1800771115. [DOI] [PubMed] [Google Scholar]
- Vaillant J. C., Balladur P., Nordlinger B., Karaitianos I., Hannoun L., Huguet C., Parc R. Repeat liver resection for recurrent colorectal metastases. Br J Surg. 1993 Mar;80(3):340–344. doi: 10.1002/bjs.1800800324. [DOI] [PubMed] [Google Scholar]
- WOODINGTON G. F., WAUGH J. M. Results of resection of metastatic tumors of the liver. Am J Surg. 1963 Jan;105:24–29. doi: 10.1016/0002-9610(63)90263-0. [DOI] [PubMed] [Google Scholar]
- Wilson S. M., Adson M. A. Surgical treatment of hepatic metastases from colorectal cancers. Arch Surg. 1976 Apr;111(4):330–334. doi: 10.1001/archsurg.1976.01360220026004. [DOI] [PubMed] [Google Scholar]
- Wood C. B., Gillis C. R., Blumgart L. H. A retrospective study of the natural history of patients with liver metastases from colorectal cancer. Clin Oncol. 1976 Sep;2(3):285–288. [PubMed] [Google Scholar]


