Abstract
OBJECTIVE: The authors determined an appropriate surgical treatment for liver metastases from colorectal cancers. Clinicopathologic features of metastatic lesions of colorectal cancers were studied. SUMMARY BACKGROUND DATA: Major hepatic resection is the usual procedure for treatment of hepatic metastases from colorectal cancers. METHODS: Forty consecutive patients who underwent hepatic resections were prospectively studied, for a total of 89 metastatic liver tumors. RESULTS: Metastatic tumor often extended along Glisson's capsule, including invasion to the portal vein (9 cases), the hepatic vein (3 cases), the bile duct (16 cases), and the nerve (6 cases). The main tumor had small satellite nodules in only one patient, and there were no microscopic deposits in the parenchyma, even within 10 mm from the metastatic tumors. Fibrous pseudocapsule formation was observed in 28 patients. DISCUSSION: The rarity of intrahepatic metastasis from metastatic tumor supports nonanatomic limited hepatic resection as the procedure of choice for metastatic colorectal cancer in the liver. The spread via Glisson's capsule should be taken into consideration for complete tumor clearance.
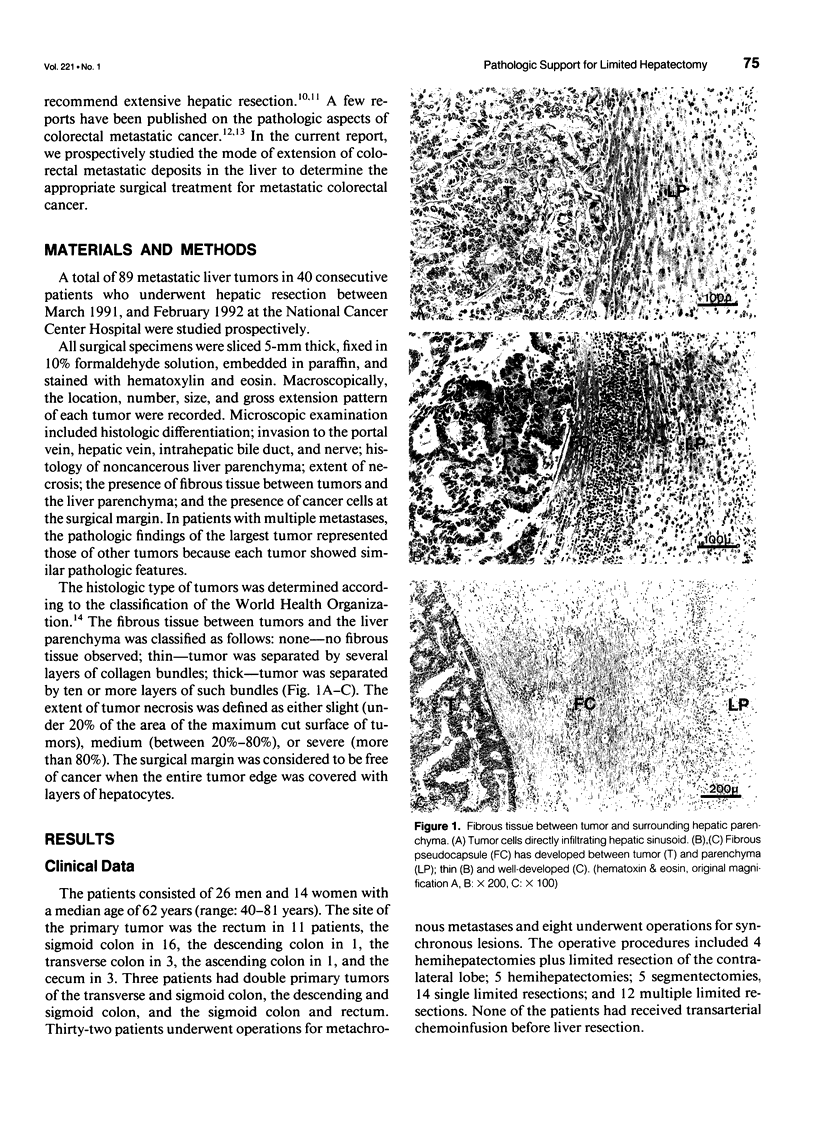
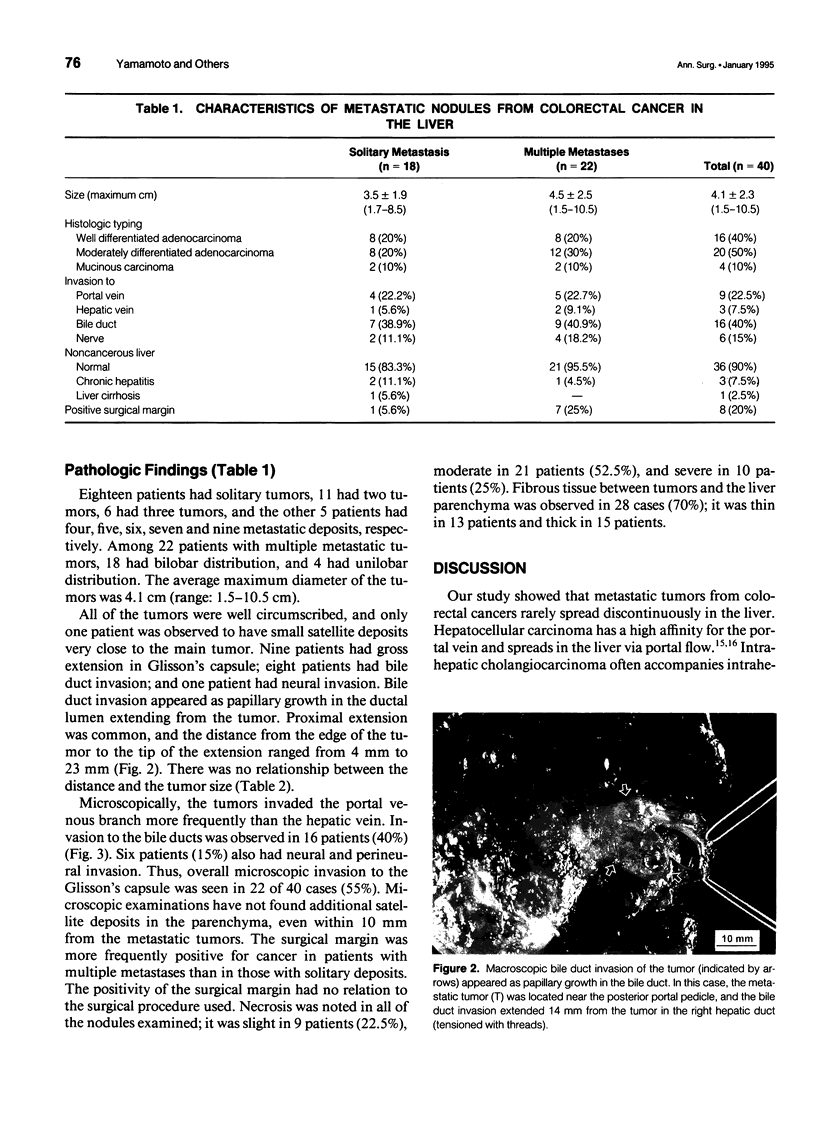
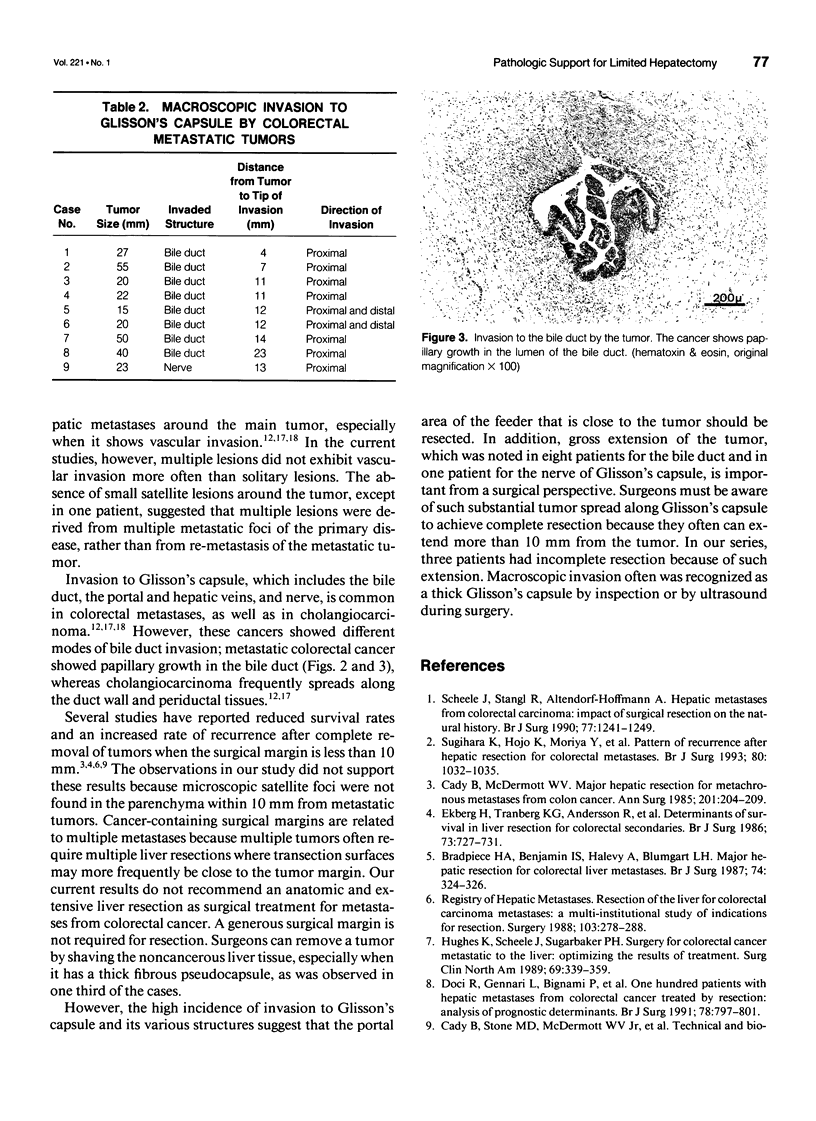
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bradpiece H. A., Benjamin I. S., Halevy A., Blumgart L. H. Major hepatic resection for colorectal liver metastases. Br J Surg. 1987 Apr;74(4):324–326. doi: 10.1002/bjs.1800740434. [DOI] [PubMed] [Google Scholar]
- Cady B., McDermott W. V. Major hepatic resection for metachronous metastases from colon cancer. Ann Surg. 1985 Feb;201(2):204–209. doi: 10.1097/00000658-198502000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cady B., Stone M. D., McDermott W. V., Jr, Jenkins R. L., Bothe A., Jr, Lavin P. T., Lovett E. J., Steele G. D., Jr Technical and biological factors in disease-free survival after hepatic resection for colorectal cancer metastases. Arch Surg. 1992 May;127(5):561–569. doi: 10.1001/archsurg.1992.01420050085011. [DOI] [PubMed] [Google Scholar]
- Doci R., Gennari L., Bignami P., Montalto F., Morabito A., Bozzetti F. One hundred patients with hepatic metastases from colorectal cancer treated by resection: analysis of prognostic determinants. Br J Surg. 1991 Jul;78(7):797–801. doi: 10.1002/bjs.1800780711. [DOI] [PubMed] [Google Scholar]
- Ekberg H., Tranberg K. G., Andersson R., Lundstedt C., Hägerstrand I., Ranstam J., Bengmark S. Determinants of survival in liver resection for colorectal secondaries. Br J Surg. 1986 Sep;73(9):727–731. doi: 10.1002/bjs.1800730917. [DOI] [PubMed] [Google Scholar]
- Hughes K., Scheele J., Sugarbaker P. H. Surgery for colorectal cancer metastatic to the liver. Optimizing the results of treatment. Surg Clin North Am. 1989 Apr;69(2):339–359. doi: 10.1016/s0039-6109(16)44790-0. [DOI] [PubMed] [Google Scholar]
- Iwatsuki S., Shaw B. W., Jr, Starzl T. E. Experience with 150 liver resections. Ann Surg. 1983 Mar;197(3):247–253. doi: 10.1097/00000658-198303000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makuuchi M., Hasegawa H., Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet. 1985 Oct;161(4):346–350. [PubMed] [Google Scholar]
- Nakajima T., Kondo Y., Miyazaki M., Okui K. A histopathologic study of 102 cases of intrahepatic cholangiocarcinoma: histologic classification and modes of spreading. Hum Pathol. 1988 Oct;19(10):1228–1234. doi: 10.1016/s0046-8177(88)80156-4. [DOI] [PubMed] [Google Scholar]
- Nakamura S., Yokoi Y., Suzuki S., Baba S., Muro H. Results of extensive surgery for liver metastases in colorectal carcinoma. Br J Surg. 1992 Jan;79(1):35–38. doi: 10.1002/bjs.1800790112. [DOI] [PubMed] [Google Scholar]
- Scheele J., Stangl R., Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg. 1990 Nov;77(11):1241–1246. doi: 10.1002/bjs.1800771115. [DOI] [PubMed] [Google Scholar]
- Sugihara K., Hojo K., Moriya Y., Yamasaki S., Kosuge T., Takayama T. Pattern of recurrence after hepatic resection for colorectal metastases. Br J Surg. 1993 Aug;80(8):1032–1035. doi: 10.1002/bjs.1800800837. [DOI] [PubMed] [Google Scholar]
- Weinbren K., Mutum S. S. Pathological aspects of cholangiocarcinoma. J Pathol. 1983 Feb;139(2):217–238. doi: 10.1002/path.1711390210. [DOI] [PubMed] [Google Scholar]
- Yamamoto J., Kosuge T., Takayama T., Shimada K., Makuuchi M., Yoshida J., Sakamoto M., Hirohashi S., Yamasaki S., Hasegawa H. Surgical treatment of intrahepatic cholangiocarcinoma: four patients surviving more than five years. Surgery. 1992 Jun;111(6):617–622. [PubMed] [Google Scholar]