Abstract
Introduction
There are important and understudied health differences among subgroups of Asian Americans. The authors examined differences in BMI percentile and body weight status among Asian American youth.
Methods
The authors conducted a retrospective cohort study using electronic health records in 2011–2020 from 2 integrated healthcare systems in California. Single-race, non-Latino White, and Asian American youth aged 2–19 years during the study period were included. Asian American subgroups included East, South, Southeast, and unidentified. Whites were the reference group. Study outcomes included age- and sex-specific BMI percentile and body weight status category (underweight, overweight or obesity, obesity). Series of 1-sample estimates for study outcomes were calculated by calendar year and biological ages.
Results
A total of 395,134 youth were included in the study (mean [SD] age at baseline of 8.26 [5.61] years; mean [SD] BMI percentile of 53.8 [30.3]), including 23,183 East Asians; 34,783 South Asians; and 34,738 Southeast Asians. Southeast Asians had the highest age-adjusted prevalence of obesity (2019 estimate: 13.3%) than East Asians (5.2%), South Asians (7.8%), and Whites (11.8%). South Asians had the highest prevalence of underweight (2019 estimate: 11.8%) than East Asians (5.5%), Southeast Asians (3.9%), and White (3.6%).
Conclusions
Substantial heterogeneity among Asian American youth was found in the study cohort. Asian American youth face distinct challenges of unhealthy weight statuses unique to their subgroups.
Keywords: Asian American, youth, obesity, underweight, heterogeneity
HIGHLIGHTS
-
•
BMI percentiles and weight status of Asian American youth are heterogeneous.
-
•
Southeast Asian youth had high prevalence of obesity and overweight.
-
•
South Asian youth had relatively high and increasing rates of underweight.
-
•
Asian American youth face distinct challenges in unhealthy weight statuses.
INTRODUCTION
Childhood obesity is associated with increased healthcare costs and long-term health risks.1,2 Approximately 1 in 5 U.S. children aged between 2 and 19 years had obesity according to the 2017–2020 National Health and Nutrition Examination Survey.3 By contrast, the estimated prevalence rate of children with underweight was consistently low, between 3.5% and 4.1% from 2001 to 2018.4
Asian Americans of all ethnicities, including multirace-ethnicity identities, accounted for 7.2% of the U.S. population in the 2020 Census, and single-race non-Latino Asians are expected to be the fastest growing racial or ethnic subgroup in the U.S.5 Overall, Asians have the lowest prevalence of childhood obesity.3,6,7 However, a review found that despite a lower average BMI than Whites, Asian American adults had higher prevalence of Type 2 diabetes, dyslipidemia, and hypertension.8 Lower BMI cutoffs for Asian adults have been recommended for body weight status and screening the risk of Type 2 diabetes, for example, the threshold for overweight may be 23 kg/m2 for all Asians or 24 kg/m2 for South Asians.9,10
Asian Americans consist of highly diverse subpopulations with distinct health risks and challenges.11, 12, 13, 14, 15 Asian Americans have been conventionally aggregated into a single race/ethnicity group in obesity studies. Heterogeneity in health among Asian American subgroups has been historically understudied, likely owing to unavailable data on ethnicities or the limited sample size or both.8 There is a limited but growing literature on the heterogeneity for the adult Asian American population.16, 17, 18, 19 Some studies noted the lowest obesity prevalence among Chinese American adults and the highest mean BMI among Filipino American adults.16,19 A prior study found that across all weight categories, Asian Americans had a higher prevalence of diabetes and prediabetes than White people, and within the Asian American population, South Asians and Filipino people had a higher diabetes prevalence than Chinese Americans.20 A scientific statement from the American Heart Association emphasized the importance of disaggregating data for Asian American subgroups owing to heterogeneity in the prevalence of Type 2 diabetes, atherosclerotic cardiovascular disease, and other risk factors.21
Knowledge of the heterogeneity among Asian American youth will be important reference for properly monitoring childhood obesity prevalence and prevention. This paper addresses the knowledge gap in understanding the heterogeneity in youth body weight status among Asian American youth. The state of California is home to a large Asian American population (approximately 6 million or 15% of the state population in the 2020 U.S. Census). Leveraging the detailed race and ethnicity information available in the electronic health records (EHRs) from 2 large regional integrated health systems in California—Kaiser Permanente Southern California and Northern California (referred to as KP in the remaining parts of this paper)—the authors conducted an exploratory analysis for the difference in youth body weight status and BMI percentile among Asian Americans. The authors aimed to contribute much needed detailed descriptive statistics data on Asian American youth’ health to the literature.
METHODS
Study Sample
KP has a common EHR infrastructure to link hospitals, medical offices, pharmacies, and laboratories for medical practice and research with over 9.4 million patients, whose sociodemographic and health characteristics are comparable with those of the general California population.22,23 This analysis used a cohort of youth retrieved and assembled by a parent study.24 The use of data and research aims were approved by KP IRBs. In this study, a child entered the study cohort when the first BMI measurement was captured in EHR between the ages of 2 and 19 years and exited the study cohort when the age of a later measurement was above 19 years or the child no longer had KP healthcare coverage, all between 2011 and 2020. Other exclusion criteria were metastatic cancer diagnosis, pregnancy, bariatric surgery in the last 5 years of any measurement, and current palliative care.24 The authors included single-race non-Latino Asian American youth (in the remaining parts of this paper, the authors used Asian to refer exclusively to single-race non-Latino Asian American youth) and single-race non-Latino White youth (referred to as White in the remaining parts of this paper), which served as the reference group, similar to a prior study based on the same race and ethnicity criteria.20
The detailed ethnicity for Asians was based on members’ voluntary responses upon enrollment in KP or at outpatient visits. Asians with self-identified ethnicities were first partitioned into 3 subgroups by the regions of ancestries: East Asian (Chinese, Japanese, Korean, Okinawan, Taiwanese, and Tibetan), South Asian (Bangladeshi, Bhutanese, East Indian, Indian, Maldivian, Nepali, Pakistani, and Sri Lankan), and Southeast Asian (Bruneian, Burmese, Cambodian, Filipino, Hmong, Indonesian, Laotian, Malaysian, Mien, Singaporean, Timorese, Thai, and Vietnamese). Those classified as Asian but without more details were grouped as Asian unidentified.
Measures
Besides race and ethnicity, the authors retrieved biological sex, birth year, insurance status (commercial versus public options), census tract of residence based on the individual’s residential address, and poverty level of the census tracts. The outcomes were sex- and age-specific BMI percentile and weight status defined by the Centers for Disease Control and Prevention cutoffs for underweight (<5th percentile), healthy weight (5th–85th percentile), overweight or obesity (>85th percentile), and obesity (≥95th percentile). All outcomes were at the person-year level in the years when patients had outpatient visits, during which BMI and BMI percentile measures were recorded in the EHR. A very few records (<1%) with invalid BMI measures were not used. If a patient had more than 1 outpatient visit in a calendar year, the authors took the average of the multiple BMI percentile measures in that year and converted to weight status.
Statistical Analysis
The authors first calculated descriptive statistics for outcomes and sample characteristics by the study subgroups and then by sex. Next, the authors performed the temporal analysis between 2011 and 2020. In each calendar year and for each subgroup, the authors calculated the age-adjusted mean BMI percentile and prevalence rates of each unhealthy weight status by the Horvitz–Thompson estimator, in which sampling weights were applied to adjust the age distribution in the study sample to be equal to that of the general California youth population aged between 2 and 19 years in 2020. The temporal analysis for a study outcome consisted of 10 yearly point estimates between 2011 and 2020. The temporal analysis was also conducted for each sex separately. Finally, the authors conducted a by-age analysis for each study subgroup by pooling data from all calendar year. Chronological ages in the year of measurement were used as an integer-valued discrete explanatory variable between the ages of 2 and 19 years. For each of the 18 discrete ages and in each subgroup, the authors pooled all records with that age in any calendar year and calculated the sample mean BMI percentile and the sample proportions for each weight status. By-age analyses were always performed separately for each sex owing to the differing growth patterns between sex.
In all analyses, the parameters of interest included the mean BMI percentile, prevalence rate of obesity (ROB), prevalence rate of overweight or obesity (ROWOB), and prevalence rate of underweight (RUW). All statistical analyses were series of 1-sample point estimates and performed in R 4.3.2 and in 2024.
To preserve robust descriptive statistics results, the authors did not rely on any parametric or nonparametric modeling assumptions in this paper, such as specific shapes of trend and covariate effects. The authors used Wald’s pointwise 95% CI, that is, point estimate ± 1.96 times SE for parameters of interest. The difference in a common parameter of interest between 2 subgroups was tested using a conservative approach: if the 95% CIs of these 2 subgroups did not overlap, the between-group difference was significant at the p<0.05 level. However, owing to the large sample size, the lengths of all 95% CIs were short or very short, resulting in most between-group differences being statistically significant at the p<0.05 level.
In this paper, the authors focused on the practical significance of the between-group differences. The authors used the following references for practically significant or meaningful differences. In public health research, 1–2 percentage point differences or a 10% relative difference in the prevalence rate of unhealthy weight status is generally considered as practically meaningful and significant (e.g., the Healthy People 2030 initiative of the U.S. Department of Health and Human Services). Clinically, a 5-point difference in BMI percentile is considered a practically significant change at the individual pediatric patient level, but smaller differences can also be meaningful, particularly for children with obesity and overweight.25 From the public health perspective, a difference in 1–2 points in BMI percentile was reported as significant.24
RESULTS
Table 1 displays the characteristics of the entire cohort and by the study subgroups (White, all Asian, East Asian, South Asian, Southeast Asian, and Asian unidentified). A CONSORT diagram is presented in Appendix Figure 1 (available online). Details of specific ethnic subgroups (Chinses, Filipinos, Indians) are reported Appendix Table 1 (available online). The final study cohort comprised 395,134 youth, with a mean BMI percentile of 53.8 (SD=30.3) and an average age of 8.3 (SD=5.6) years at cohort entry. Most of this cohort had KP’s commercial insurance (92.5%) and resided in medium or large cities (82.0%). On average, 7.1% households in the census tracts of the study cohort’s residences were in poverty (SD=7.1%). At cohort entry, the cohort had 5.7% with underweight, 73.4% with normal weight, 12.0% with overweight, and 9.0% with obesity.
Table 1.
Characteristics of the Study Cohort of White and Asian American Youth
| Characteristics Mean (SD) or n (%) |
Total (N=395,134) |
White (n=210,662) |
Asian: all (n=184,472) |
East (n=23,183) |
South (n=20,837) |
Southeast (n=34,738) |
Asian unidentified (n=105,714) |
|---|---|---|---|---|---|---|---|
| Female | 194,631 (49.3) | 104,194 (49.5) | 90,437 (49.0) | 11,270 (48.6) | 9,867 (47.4) | 17,155 (49.4) | 52,145 (49.3) |
| Male | 200,503 (50.7) | 106,468 (50.5) | 94,035 (51.0) | 11,913 (51.4) | 10,970 (52.6) | 17,583 (50.6) | 53,569 (50.7) |
| Cohort entry | |||||||
| Age, year | 8.3 (5.6) | 8.6 (5.7) | 7.8 (5.5) | 7.1 (5.7) | 5.4 (4.8) | 7.5 (5.8) | 8.6 (5.3) |
| BMI percentile | 53.8 (30.3) | 56.7 (29.5) | 50.5 (30.9) | 47.0 (28.8) | 41.4 (31.7) | 53.2 (31.2) | 52.3 (30.8) |
| With obesity | 35,450 (9.0) | 20,497 (9.7) | 14,953 (8.1) | 945 (4.1) | 1,153 (5.5) | 3,608 (10.4) | 9,247 (8.7) |
| With overweight | 47,268 (12.0) | 27,473 (13.0) | 19,795 (10.7) | 1,986 (8.6) | 1,678 (8.1) | 4,098 (11.8) | 12,033 (11.4) |
| With normal weight | 289,838 (73.4) | 153,951 (73.1) | 135,887 (73.7) | 18,719 (80.7) | 14,983 (71.9) | 24,828 (71.5) | 77,357 (73.2) |
| With underweight | 22,578 (5.7) | 8,741 (4.1) | 13,837 (7.5) | 1,533 (6.6) | 3,023 (14.5) | 2,204 (6.3) | 7,077 (6.7) |
| Cohort exit | |||||||
| Age, year | 11.8 (5.7) | 12.3 (5.7) | 11.3 (5.6) | 10.8 (5.9) | 8.76 (5.5) | 11.1 (5.9) | 12.0 (5.4) |
| BMI percentile | 56.9 (30.4) | 59.3 (29.6) | 54.0 (31.0) | 51.0 (29.0) | 47.6 (32.7) | 58.2 (30.9) | 54.6 (30.8) |
| With obesity | 43,695 (11.1) | 25,728 (12.2) | 17,967 (9.7) | 1,248 (5.4) | 1,625 (7.8) | 4,681 (13.5) | 10,413 (9.9) |
| With overweight | 53,050 (13.4) | 29,909 (14.2) | 23,141 (12.5) | 2,401 (10.4) | 2,309 (11.1) | 4,877 (14.0) | 13,554 (12.8) |
| With normal weight | 278,473 (70.5) | 146,963 (69.8) | 131,510 (71.3) | 18,251 (78.7) | 14,463 (69.4) | 23,512 (67.7) | 75,284 (71.2) |
| With underweight | 19,916 (5.0) | 8,062 (3.8) | 11,854 (6.4) | 1,283 (5.5) | 2,440 (11.7) | 1,668 (4.8) | 6,463 (6.1) |
| Age in 2020, year | 14.5 (6.9) | 15.1 (6.92) | 13.8 (6.8) | 13.2 (7.30) | 10.7 (6.5) | 13.6 (7.2) | 14.6 (6.4) |
| Insurance: public options | 29,719 (7.5) | 16,694 (7.9) | 13,025 (7.1) | 1,847 (8.0) | 1,295 (6.2) | 3,954 (11.4) | 5,929 (5.6) |
| Insurance: commercial | 365,415 (92.5) | 193,968 (92.1) | 171,447 (92.9) | 21,336 (92.0) | 19,542 (93.8) | 30,784 (88.6) | 99,785 (94.4) |
| Residence | |||||||
| Large citiesa | 157,590 (39.9) | 83,128 (39.5) | 74,462 (40.4) | 9,582 (41.3) | 5,830 (28.0) | 15,967 (46.0) | 43,083 (40.8) |
| Medium citiesa | 166,327 (42.1) | 87,724 (41.6) | 78,603 (42.6) | 8,782 (37.9) | 12,160 (58.4) | 14,548 (41.9) | 43,113 (40.8) |
| Small citiesa | 71,217 (18.0) | 39,810 (18.9) | 31,407 (17.0) | 4,819 (20.8) | 2,847 (13.7) | 4,223 (12.2) | 19,518 (18.5) |
| % households in povertyb | 7.1 (7.1) | 7.0 (7.0) | 7.3 (7.2) | 6.1 (6.1) | 5.3 (5.2) | 9.3 (8.1) | 7.3 (7.4) |
Note: All N and n refer to the number of patients.
Large cities: population >400,000; medium cities: population between 100,000 and 400,000; small cities: population <100,000.
In the census tract of the residence.
Asians (n=184,472) were slightly younger (mean [SD]=7.8 [5.5] vs 8.6 [5.7]), had a lower mean BMI percentile (mean [SD]=50.5 [30.9] for Asians vs 56.7 [29.5] for Whites), had a higher RUW (7.5% vs 4.1%), and had lower ROB (8.1% vs 9.7%) and ROWOB (18.8% vs 22.7%) than Whites (n=210,662). Among Asian youth, South Asians were the youngest (mean [SD]=5.4 [4.8]), had the lowest mean BMI percentile (mean [SD]=41.4 [31.7]), and had the highest RUW (14.5%); Southeast Asian youth had the highest ROB (10.4%) and ROWOB (22.2%). Across all youth, slightly more females were in the normal weight category (75.2% female vs 71.6% male), whereas more males were in the obesity category (ROB: 10.5% male vs 7.4% female). Details of the by-sex descriptive statistics are reported in Appendix Table 2 (available online).
Figure 1 displays the temporal analysis results of the 4 study outcomes by subgroups (White, all Asian, East Asian, South Asian, and Southeast Asian). There were no notable changes over time in mean BMI percentile, ROB, and ROWOB in any study subgroup. Whites always had the highest mean BMI percentile, followed closely by Southeast Asians, but Southeast Asians had higher ROB and ROWOB than Whites. South Asians and East Asians consistently had notably lower mean BMI percentiles than the other subgroups. There was a slight increase in RUW in all other subgroups, except that South Asians had both a marked increase over time and the highest RUW in all times. All Asian subgroups had higher RUW than Whites (Figure 1).
Figure 1.
Age-adjusted temporal analysis between 2010 and 2020 for White and Asian American youth: mean BMI percentile (upper left), prevalence ROB (upper right), prevalence ROWOB (lower left), and prevalence RUW (lower right). Vertical bars are 95% CIs.
ROB, rate of obesity; ROWOB, rate of overweight or obesity; RUW, rate of underweight.
The authors used 2019 as an example year to review the details of temporal analysis. Whites had an average BMI percentile of 59.3 (95% CI=59.1, 59.5), the highest among all subgroups; an ROB of 11.8% (second highest); an ROWOB of 26.1% (highest); and an RUW of 3.6% (lowest). Southeast Asians were similar to Whites, with an average BMI percentile of 58.0 (95% CI=57.5, 58.4), an ROB of 13.3% (highest), an ROWOB of 27.0%, and an RUW of 3.9%. By contrast, East Asians had a notably lower mean BMI percentile of 50.6 (95% CI=50.1, 51.2), an ROB of 5.2%, an ROWOB of 15.4%, and an RUW of 5.5%. South Asians had the lowest mean BMI percentile of 47.0 (95% CI=46.4, 47.6), an ROB of 7.8%, an ROWOB of 18.6%, and a remarkably high RUW of 11.8% (highest).
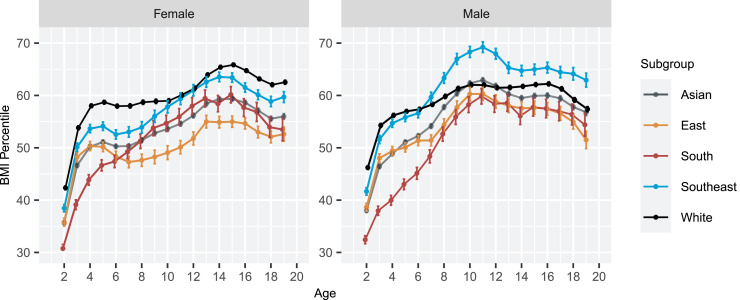
Figure 2 presents the by-age analysis for the mean BMI percentiles. Overall, males had lower mean BMI percentile than females in any subgroup. The mean BMI percentile increased rapidly in early ages in all subgroups, and the increase leveled off at different ages for each sex and subgroup. For males, Southeast Asians had a higher mean BMI percentile than East Asians and South Asians across all age levels and also had higher mean BMI percentile than Whites after the age of 8 years. For females, Southeast Asians were also higher in mean BMI percentile than East and South Asians. East Asians and South Asians had lower mean BMI percentiles than Whites for all sexes and age combinations. For example, among males aged 16 years, the mean BMI percentile for Southeast Asians was the highest (65.3, 95% CI=64.3, 66.3), above those of Whites (62.2, 95% CI=61.9, 62.6), East Asians (57.5, 95% CI=56.2, 58.7), and South Asians (57.5, 95% CI=55.8, 59.3). Among females aged 3 years, the average BMI percentiles were 48.3 (95% CI=47.4, 49.1), 39.1 (95% CI=38.2, 40.1), and 50.1 (95% CI=49.3, 50.9) for East, South, and Southeast Asians, respectively, all of whom had average BMI percentiles below those of Whites (53.9, 95% CI=53.5, 54.2).
Figure 2.
Estimated mean BMI percentiles for White and Asian American youth by chronological ages 2–19 years and sex. Vertical bars are 95% CIs.
Figure 3 shows the by-age estimates for ROB, ROWOB, and RUW. In all subgroups, the ROB and ROWOB increased in early ages before leveling off in slightly different ages for each subgroup and sex and generally around ages 8–10 years. Correspondingly, the RUW declined sharply in early ages and leveled off in later ages. There was a high level of heterogeneity in the prevalence of all unhealthy weight statuses among Asian subgroups. First, Southeast Asians consistently had a higher ROB and ROWOB than East Asians and South Asians in all sex–age combinations. Southeast Asian males had higher ROB and ROWOB than Whites in ages ≥6 years. Second, South Asians had consistently the highest RUW in all ages, whereas all other subgroups were similar to one another. Finally, East Asians had generally the lowest ROB and ROWOB in almost all ages except for the few youngest age years. For example, at age 10 years, 11.7% of East Asian males and 4.6% of East Asian females had obesity, 13.4% of South Asian males and 8.1% of South Asian females had obesity, and 25.4% of Southeast Asian males and 12.5% of Southeast Asian females had obesity. By contrast, at age 10 years, 3.2% of East Asian males and 5.3% of East Asian females were underweight, 8.5% of South Asian males and 7.8% of South Asian females were underweight, and only 3.3% of Southeast Asian males and 4.7% of Southeast Asian females were underweight.
Figure 3.
Estimated prevalence ROB, ROWOB, and RUW for White and Asian American youth by ages 2–19 years and sex. Vertical bars are 95% CIs. The differences in y-axis scales should be noted.
ROB, rate of obesity; ROWOB, rate of overweight or obesity; RUW, rate of underweight.
In all results except for a very few cases (e.g., ROWOB between Southeast Asians and Whites), none of the 95% CIs for the same parameter of interest overlapped, indicating that all between-group differences in 2019 were statistically significant at the p<0.05 level. Most between-group differences exceeded the practical significant cutoff (e.g., 5 points for BMI percentile and 1 percentage point for prevalence rates).
Detailed estimates and 95% CIs for all parameters of interest in the temporal analysis and by-age analysis and for Asian unidentified are included in Appendix Tables 3 and 4 (available online). Asians unidentified were similar to the aggregated Asians in all aspects, except that the mean age at cohort entry was a little older (8.6 vs 7.8 years).
DISCUSSION
To the author’s knowledge, this study is among the first to rigorously investigate BMI percentiles and prevalence of unhealthy weight statuses among Asian youth using a large study cohort and over a relatively long study period. The results add strong and detailed evidence to the literature to identify the unique challenges for each Asian subgroup. First, East Asians had low risks for all unhealthy weight statuses, which roughly aligned with the stereotypical impression for all aggregated Asians. Second, Southeast Asians were faced with a relatively high prevalence in childhood obesity and overweight, comparable with or slightly higher than those of Whites. Finally, South Asians were faced with the unique issue of underweight: their RUW was multiple-fold higher than those of other study subgroups and increased steadily. South Asians also had notably high within-group variation, that is, both RUW and ROB were high. The heterogeneity among Asian subgroup was not only statistically significant but also far exceeded the usual cutoffs for practically significant differences. For example, Southeast Asians had a mean BMI percentile 10–15 points higher than that of East Asians, whereas a 5-point difference is generally considered clinically significant.
Asian subgroups also showed distinct by-age relationship in all study outcomes. Future surveillance work may consider the empirical distribution of BMI percentile specific to these subgroups rather than focusing exclusively on the mean BMI percentiles or the Centers for Disease Control and Prevention official cutoffs owing to their large within-group heterogeneity.26, 27, 28 In particular, the underweight cutoff for South Asians needs more confirmatory study for its appropriateness. Southeast Asian youth already had remarkably high ROB and ROWOB using the current BMI percentile. The authors also observed consistent between-sex differences in all study subgroups, with males having higher mean BMI percentiles and higher ROB and ROWOB than females.29,30
Many prevention and intervention efforts for childhood obesity, such as improving food security and physical activity promotion, were not specific to Asians, largely owing to their overall low obesity prevalence.31 The results suggest that Southeast Asians need to be included or even emphasized in these efforts. Southeast Asians originated from the most diverse region of Asia in cultures, traditions, and languages, leading to distinct dietary habits, lifestyles, and norms. Recognizing these distinctions, culturally tailored programs should be developed to address the specific obesity issues among Southeast Asian youth.
The prevalence of underweight among South Asian youth is notable and has been rarely documented in the literature. This may be partly attributed to the distinct culture and practice in diet and lifestyle among South Asian families. The short- and long-term consequences of this elevated prevalence of underweight among South Asian youth need further investigations.
Limitations
KP members living in California cities may have characteristics (e.g., insurance plan, neighborhood poverty, urbanicity of residence) different from those of the general population. This potential sample selection bias may not be of concern because California has the highest population of Asians in the U.S., and Asian Americans predominantly live in metropolitan areas. Large-scale EHR data were the basis of this study and prior studies on obesity epidemiology.32,33 Using the EHR data for population health studies can suffer from the threat of encounter bias.34,35 The race and ethnicity information was based on voluntary responses of KP members, with a relatively low response rate (42.7%). However, the authors did not observe sizable differences in all analyses between Asian unidentified and the aggregated Asians, which suggested a lack of evidence for serious voluntary response bias with respect to the study interest. The authors were not able to study Pacific Islanders, Native Americans, and Alaska Natives owing to insufficient KP members in these race and ethnicity categories. Future studies are still needed to understand the health differences for these minority groups.
CONCLUSIONS
The authors found notable differences and unique challenges among Asian American youth. Southeast Asian youth had high prevalence of overweight and obesity, whereas South Asian youth had a remarkably high prevalence of underweight. Results of these analyses indicate that programs should be developed to eliminate these disparities.
Acknowledgments
ACKNOWLEDGMENTS
Funding: This study is supported by NIH/National Institute of Diabetes and Digestive and Kidney Diseases Grant 1R01DK123204 and KP internal fundings.
Declaration of interest: None.
CRediT AUTHOR STATEMENT
Darcy M. Van Deventer: Software, Formal analysis, Writing - original draft, Writing - review & editing. Margo A. Sidell: Methodology, Data curation, Validation, Investigation, Writing - review & editing. Catherine Lee: Methodology, Data curation, Investigation, Writing - review & editing. Deborah R. Young: Investigation, Writing - review & editing, Supervision. Monique M. Hedderson: Investigation, Writing - review & editing, Supervision. Deborah A. Cohen: Investigation, Writing - review & editing. Emily F. Liu: Data curation, Writing - review & editing. Lee J. Barton: Data curation, Writing - review & editing. Galina Inzhakova: Resources, Project administration, Writing - review & editing. Bing Han: Methodology, Formal analysis, Validation, Investigation, Writing - original draft, Writing - review & editing, Supervision.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2025. 100381.
Appendix. Supplementary materials
REFERENCES
- 1.Barton M. Childhood obesity: a life-long health risk. Acta Pharmacol Sin. 2012;33(2):189–193. doi: 10.1038/aps.2011.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward Z.J., Bleich S.N., Long M.W., Gortmaker SL. Association of body mass index with health care expenditures in the United States by age and sex. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0247307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stierman B., Afful J., Carroll M.D., et al. 2020 Prepandemic Data Files—Development of Files and Prevalence Estimates for Selected Health Outcomes. 2021. National health and nutrition examination survey 2017.https://www.ncbi.nlm.nih.gov/books/NBK606854/ Accessed August 4, 2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fryar C.D., Carroll M., Ogden C. Prevalence of underweight among children and adolescents aged 2–19 years: United States, 1963–1965 through 2013–2014. Health E-Stats. 2018 https://www.cdc.gov/nchs/data/hestat/underweight-child-17-18/underweight-child.htm Accessed August 4, 2025. [Google Scholar]
- 5.Budiman A., Cilluffo A., Ruiz NG. Pew Research Center; Washington, DC: 2019. Key Facts About Asian Origin Groups in the U.S.https://www.pewresearch.org/short-reads/2025/05/01/key-facts-about-asians-in-the-us/#:∼:text=Four%2Din%2Dfive%20U.S.%20Asians,likely%20to%20identify%20as%20multiracial Accessed August 4, 2025. [Google Scholar]
- 6.Kirby J.B., Liang L., Chen H.J., Wang Y. Race, place, and obesity: the complex relationships among community racial/ethnic composition, individual race/ethnicity, and obesity in the United States. Am J Public Health. 2012;102(8):1572–1578. doi: 10.2105/AJPH.2011.300452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr. 2011;2(1):23–31. doi: 10.3945/an.110.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Z., Daniel S., Fujioka K., Umashanker D. Obesity among Asian American people in the United States: a review. Obesity (Silver Spring) 2023;31(2):316–328. doi: 10.1002/oby.23639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu W.C., Araneta M.R.G., Kanaya A.M., Chiang J.L., Fujimoto W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care. 2015;38(1):150–158. doi: 10.2337/dc14-2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Araneta M.R.G., Kanaya A.M., Hsu W.C., et al. Optimum BMI cut points to screen Asian Americans for type 2 diabetes. Diabetes Care. 2015;38(5):814–820. doi: 10.2337/dc14-2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gee G.C., Ponce N. Associations between racial discrimination, limited English proficiency, and health-related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100(5):888–895. doi: 10.2105/AJPH.2009.178012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holland A.T., Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22(6):397–405. doi: 10.1016/j.annepidem.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu W., Diep C.S., McKyer LJ. Risk factors for childhood obesity among Asian Americans: a systematic review of literature and recommendations for health care research. J Health Care Poor Underserved. 2015;26(2 Suppl):171–190. doi: 10.1353/hpu.2015.0056. [DOI] [PubMed] [Google Scholar]
- 14.Gee G.C., Ro A., Gavin A., Takeuchi DT. Disentangling the effects of racial and weight discrimination on body mass index and obesity among Asian Americans. Am J Public Health. 2008;98(3):493–500. doi: 10.2105/AJPH.2007.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elsamadony A., Yates K.F., Sweat V., et al. Asian adolescents with excess weight are at higher risk for insulin resistance than Non-Asian Peers. Obesity (Silver Spring) 2017;25(11):1974–1979. doi: 10.1002/oby.22003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah N.S., Luncheon C., Kandula N.R., et al. Heterogeneity in obesity prevalence among Asian American adults. Ann Intern Med. 2022;175(11):1493–1500. doi: 10.7326/M22-0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gong S., Wang K., Li Y., Alamian A. Geographic differences in obesity prevalence and its risk factors among Asian Americans: findings from the 2013–2014 California Health Interview Survey. Sci Rep. 2018;8(1) doi: 10.1038/s41598-018-29906-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang E.J., Wong E.C., Dixit A.A., Fortmann S.P., Linde R.B., Palaniappan LP. Type 2 diabetes: identifying high risk Asian American subgroups in a clinical population. Diabetes Res Clin Pract. 2011;93(2):248–254. doi: 10.1016/j.diabres.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Staimez L.R., Weber M.B., Narayan K.M.V., Oza-Frank R. A systematic review of overweight, obesity, and type 2 diabetes among Asian American subgroups. Curr Diabetes Rev. 2013;9(4):312–331. doi: 10.2174/15733998113099990061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vicks W.S., Lo J.C., Guo L., et al. Prevalence of prediabetes and diabetes vary by ethnicity among U.S. Asian adults at healthy weight, overweight, and obesity ranges: an electronic health record study. BMC Public Health. 2022;22(1):1954. doi: 10.1186/s12889-022-14362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwan T.W., Wong S.S., Hong Y., et al. Epidemiology of diabetes and atherosclerotic cardiovascular disease among Asian American adults: implications, management, and future directions: a scientific statement from the American Heart Association. Circulation. 2023;148(1):74–94. doi: 10.1161/CIR.0000000000001145. [DOI] [PubMed] [Google Scholar]
- 22.Koebnick C., Langer-Gould A.M., Gould M.K., et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with U.S. Census Bureau data. Permanente J. 2012;16(3):37–41. doi: 10.7812/TPP/12-031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gordon NP. Kaiser Permanente Division of Research; Oakland, CA: 2015. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: statistics from the 2011 California Health Interview Survey. [Google Scholar]
- 24.Young D.R., Hedderson M.M., Sidell M.A., et al. City-level sugar-sweetened beverage taxes and youth body mass index percentile. JAMA Netw Open. 2024;7(7) doi: 10.1001/jamanetworkopen.2024.24822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barlow S.E., Hampl SE. Extended bmi-for-age growth charts: putting them to use. Pediatrics. 2023;152(3) doi: 10.1542/peds.2023-062815. [DOI] [PubMed] [Google Scholar]
- 26.Han B., Lim N. Estimating conditional proportion curves by regression residuals. Stat Med. 2010;29(13):1443–1454. doi: 10.1002/sim.3889. [DOI] [PubMed] [Google Scholar]
- 27.Swierad E., Huang TT-K, Ballard E., Flórez K., Li S. Developing a socioculturally nuanced systems model of childhood obesity in Manhattan’s Chinese American community via group model building. J Obes. 2020;2020(1) doi: 10.1155/2020/4819143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quader Z.S., Gazmararian J.A., McCullough LE. Obesity and understudied minority children: existing challenges and opportunities in epidemiology. BMC Pediatr. 2019;19(1):103. doi: 10.1186/s12887-019-1484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah B., Tombeau Cost K., Fuller A., Birken C.S., Anderson L.N. Sex and gender differences in childhood obesity: contributing to the research agenda. BMJ Nutr Prev Health. 2020;3(2):387–390. doi: 10.1136/bmjnph-2020-000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwon S., Wang-Schweig M., Kandula NR. Body composition, physical activity, and convenience food consumption among Asian American youth: 2011–2018 NHANES. Int J Environ Res Public Health. 2020;17(17):6187. doi: 10.3390/ijerph17176187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Min J., Goodale H., Xue H., Brey R., Wang Y. Racial-ethnic disparities in obesity and biological, behavioral, and sociocultural influences in the United States: a systematic review. Adv Nutr. 2021;12(4):1137–1148. doi: 10.1093/advances/nmaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu A.J., Aris I.M., Hivert M.F., et al. Association of changes in obesity prevalence with the COVID-19 pandemic in youth in Massachusetts. JAMA Pediatr. 2022;176(2):198–201. doi: 10.1001/jamapediatrics.2021.5095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woolford S.J., Sidell M., Li X., et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA. 2021;326(14):1434–1436. doi: 10.1001/jama.2021.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldstein B.A., Bhavsar N.A., Phelan M., Pencina MJ. Controlling for informed presence bias due to the number of health encounters in an electronic health record. Am J Epidemiol. 2016;184(11):847–855. doi: 10.1093/aje/kww112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldstein B.A., Phelan M., Pagidipati N.J., Peskoe SB. How and when informative visit processes can bias inference when using electronic health records data for clinical research. J Am Med Inform Assoc. 2019;26(12):1609–1617. doi: 10.1093/jamia/ocz148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.