Abstract
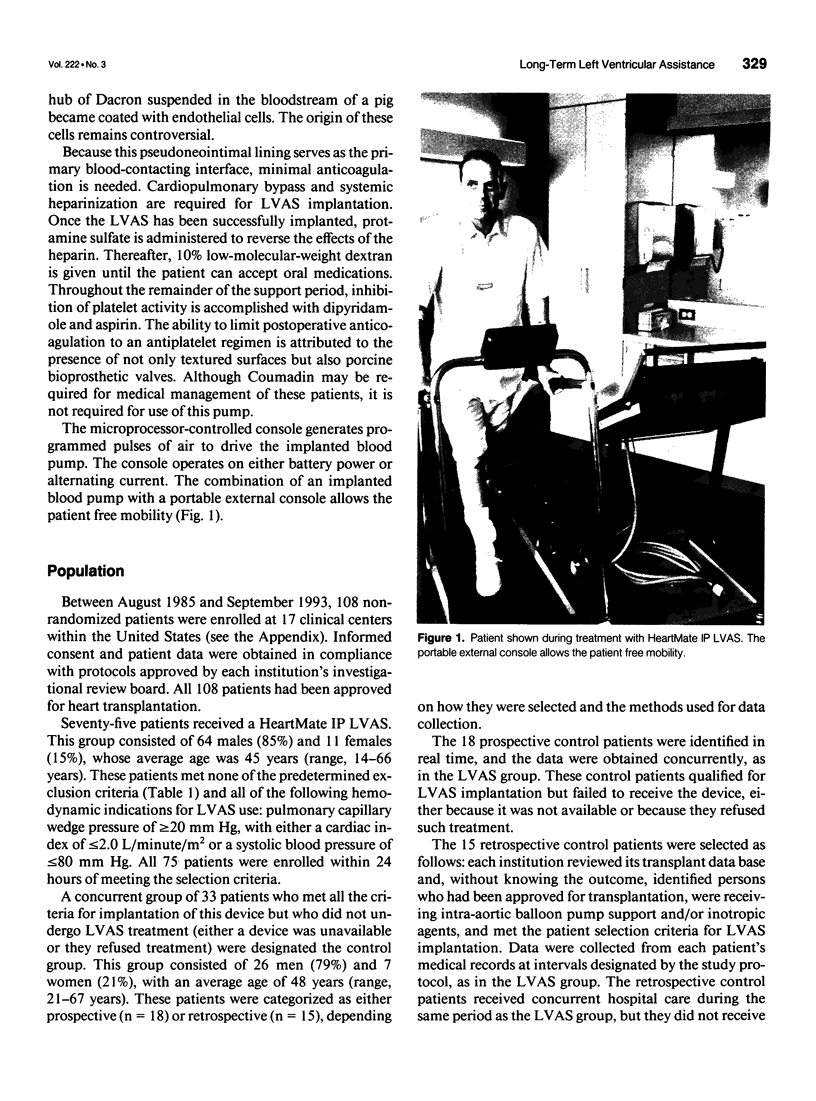
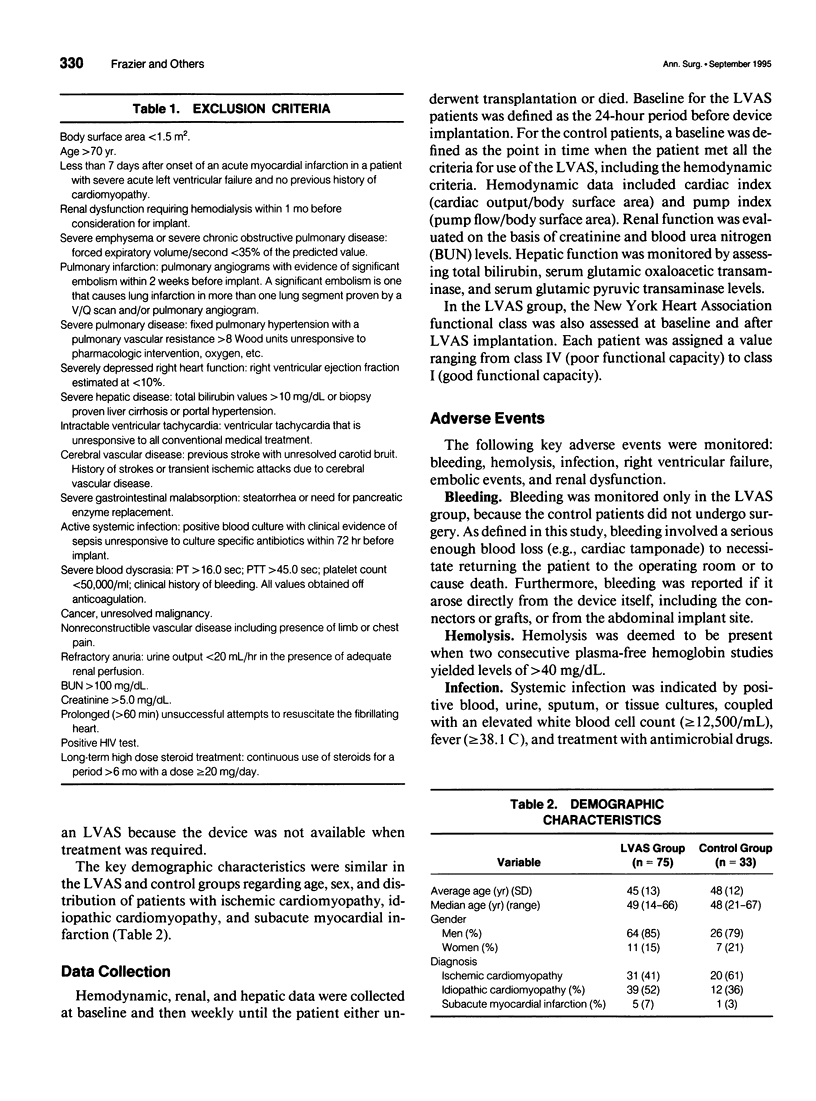
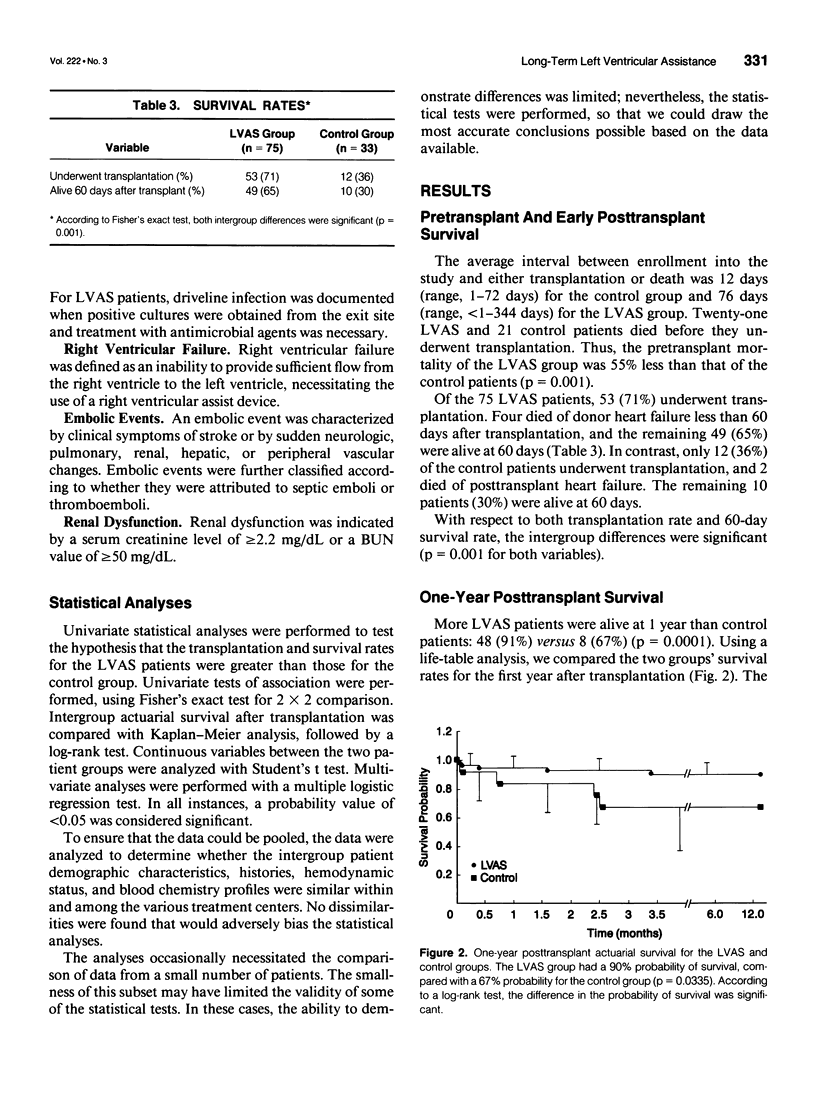
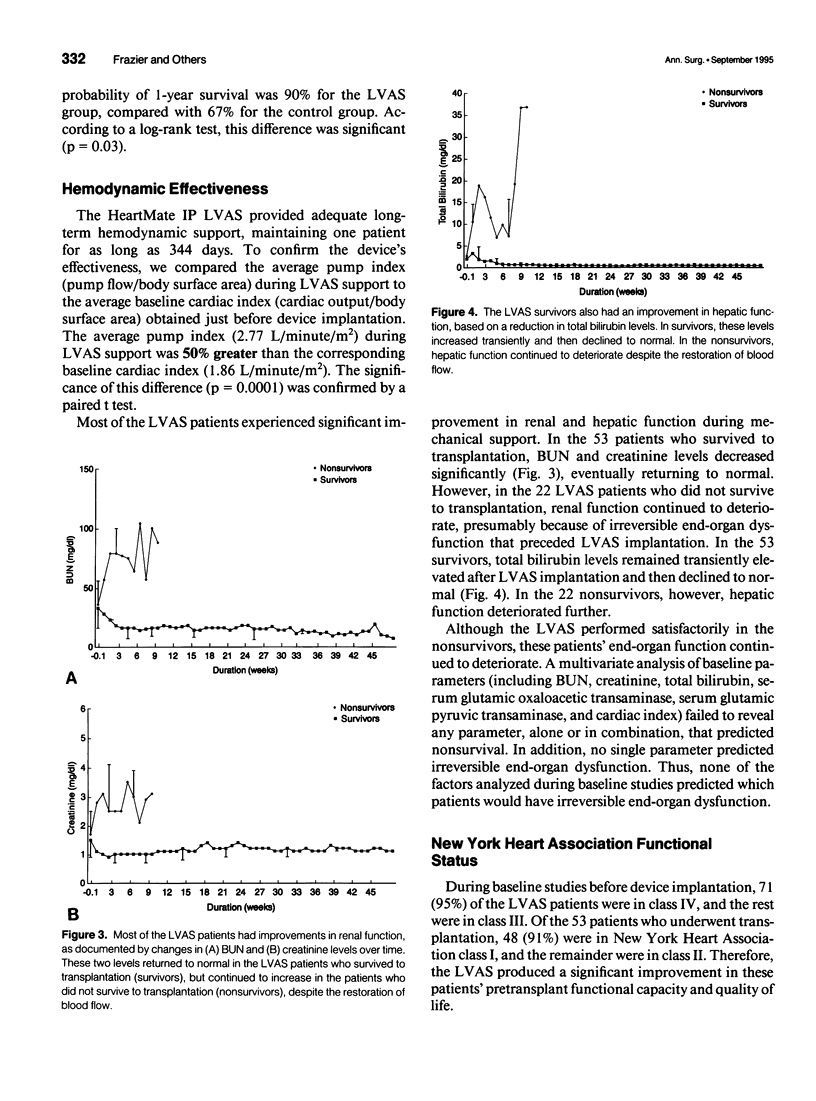
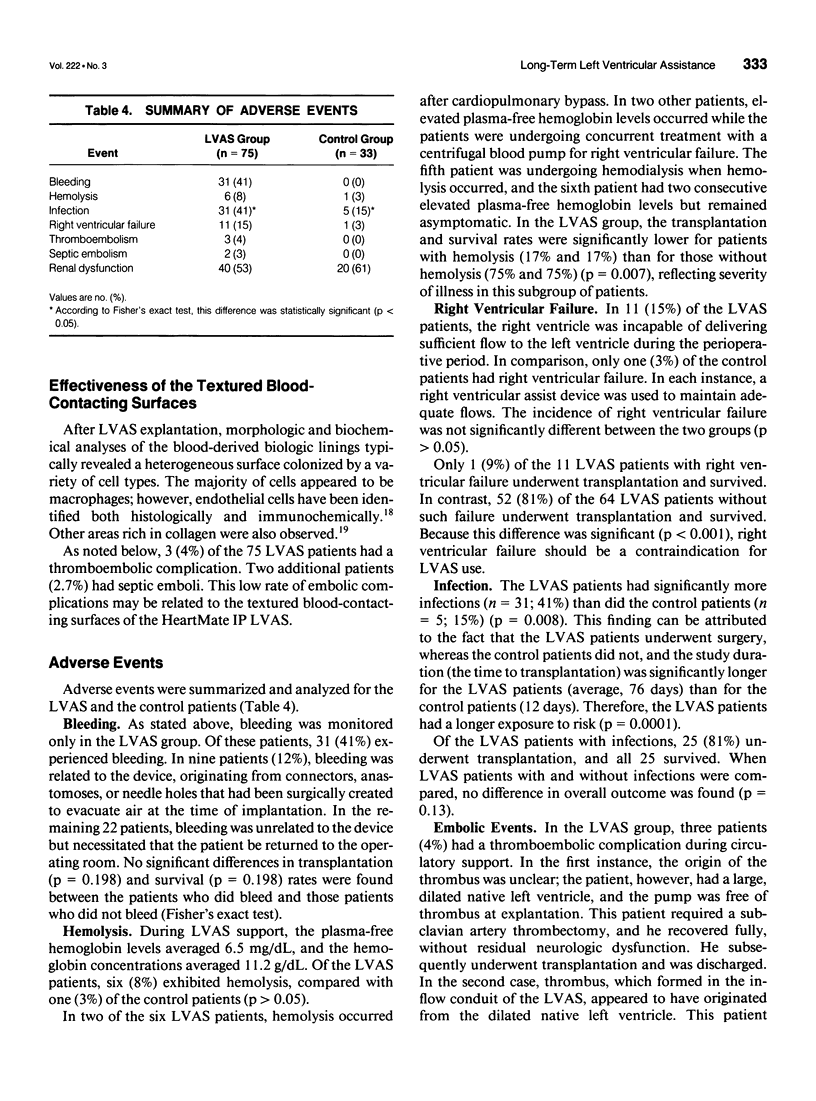
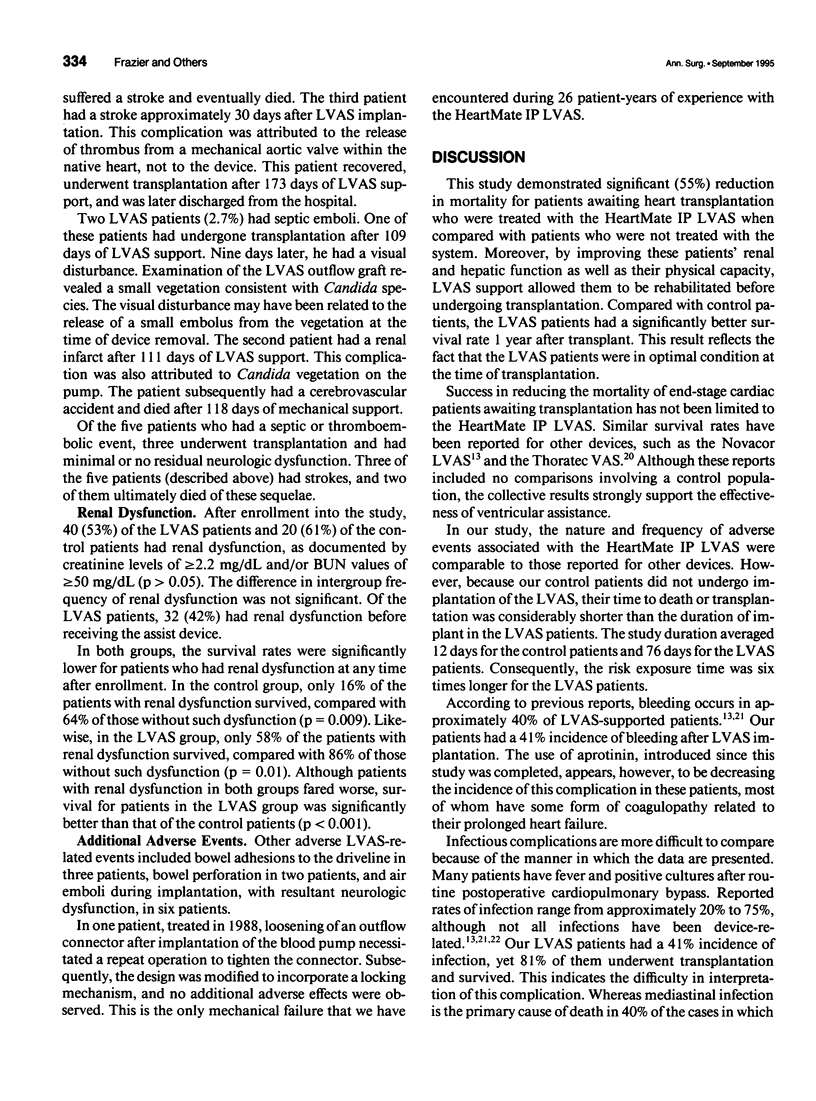
OBJECTIVE: This nonrandomized study using concurrent controls was performed to determine whether the HeartMate implantable pneumatic (IP) left ventricular assist system (LVAS) could provide sufficient hemodynamic support to allow rehabilitation of severely debilitated transplant candidates and to evaluate whether such support reduced mortality before and after transplantation. METHODS: Outcomes of 75 LVAS patients were compared with outcomes of 33 control patients (not treated with an LVAS) at 17 centers in the United States. All patients were transplant candidates who met the following hemodynamic criteria: pulmonary capillary wedge pressure > or = 20 mm Hg with a systolic blood pressure < or = 80 mm Hg or a cardiac index < or = 2.0 L/minute/m2. In addition, none of the patients met predetermined exclusion criteria. RESULTS: More LVAS patients than control patients survived to transplantation: 53 (71%) versus 12 (36%) (p = 0.001); and more LVAS patients were alive at 1 year: 48 (91%) versus 8 (67%) (p = 0.0001). The time to transplantation was longer in the group supported with the LVAS (average, 76 days; range, < 1-344 days) than in the control group (average, 12 days; range, 1-72 days). In the LVAS group, the average pump index (2.77 L/minute/m2) throughout support was 50% greater than the corresponding cardiac index (1.86 L/minute/m2) at implantation (p = 0.0001). In addition, 58% of LVAS patients with renal dysfunction survived, compared with 16% of the control patients (p < 0.001). CONCLUSIONS: The LVAS provided adequate hemodynamic support and was effective in rehabilitating patients based on improved renal, hepatic, and physical capacity assessments over time. In the LVAS group, pretransplant mortality decreased by 55%, and the probability of surviving 1 year after transplant was significantly greater than in the control group (90% vs. 67%, p = 0.03). Thus, the HeartMate IP LVAS proved safe and effective as a bridge to transplant and decreased the risk of death for patients waiting for transplantation.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Champsaur G., Ninet J., Vigneron M., Cochet P., Neidecker J., Boissonnat P. Use of the Abiomed BVS System 5000 as a bridge to cardiac transplantation. J Thorac Cardiovasc Surg. 1990 Jul;100(1):122–128. [PubMed] [Google Scholar]
- Dasse K. A., Chipman S. D., Sherman C. N., Levine A. H., Frazier O. H. Clinical experience with textured blood contacting surfaces in ventricular assist devices. ASAIO Trans. 1987 Jul-Sep;33(3):418–425. [PubMed] [Google Scholar]
- DeVries W. C., Anderson J. L., Joyce L. D., Anderson F. L., Hammond E. H., Jarvik R. K., Kolff W. J. Clinical use of the total artificial heart. N Engl J Med. 1984 Feb 2;310(5):273–278. doi: 10.1056/NEJM198402023100501. [DOI] [PubMed] [Google Scholar]
- Didisheim P., Olsen D. B., Farrar D. J., Portner P. M., Griffith B. P., Pennington D. G., Joist J. H., Schoen F. J., Gristina A. G., Anderson J. M. Infections and thromboembolism with implantable cardiovascular devices. ASAIO Trans. 1989 Jan-Mar;35(1):54–70. [PubMed] [Google Scholar]
- Evans R. W., Manninen D. L., Garrison L. P., Jr, Maier A. M. Donor availability as the primary determinant of the future of heart transplantation. JAMA. 1986 Apr 11;255(14):1892–1898. [PubMed] [Google Scholar]
- Frazier O. H., Baldwin R. T., Eskin S. G., Duncan J. M. Immunochemical identification of human endothelial cells on the lining of a ventricular assist device. Tex Heart Inst J. 1993;20(2):78–82. [PMC free article] [PubMed] [Google Scholar]
- Frazier O. H. First use of an untethered, vented electric left ventricular assist device for long-term support. Circulation. 1994 Jun;89(6):2908–2914. doi: 10.1161/01.cir.89.6.2908. [DOI] [PubMed] [Google Scholar]
- Frazier O. H., Rose E. A., Macmanus Q., Burton N. A., Lefrak E. A., Poirier V. L., Dasse K. A. Multicenter clinical evaluation of the HeartMate 1000 IP left ventricular assist device. Ann Thorac Surg. 1992 Jun;53(6):1080–1090. doi: 10.1016/0003-4975(92)90393-i. [DOI] [PubMed] [Google Scholar]
- Frazier O. H. The development of an implantable, portable, electrically powered left ventricular assist device. Semin Thorac Cardiovasc Surg. 1994 Jul;6(3):181–187. [PubMed] [Google Scholar]
- Griffith B. P., Kormos R. L., Hardesty R. L., Armitage J. M., Dummer J. S. The artificial heart: infection-related morbidity and its effect on transplantation. Ann Thorac Surg. 1988 Apr;45(4):409–414. doi: 10.1016/s0003-4975(98)90014-5. [DOI] [PubMed] [Google Scholar]
- Hill J. D., Farrar D. J., Hershon J. J., Compton P. G., Avery G. J., 2nd, Levin B. S., Brent B. N. Use of a prosthetic ventricle as a bridge to cardiac transplantation for postinfarction cardiogenic shock. N Engl J Med. 1986 Mar 6;314(10):626–628. doi: 10.1056/NEJM198603063141007. [DOI] [PubMed] [Google Scholar]
- Icenogle T. B., Smith R. G., Cleavinger M., Vasu M. A., Williams R. J., Sethi G. K., Copeland J. G. Thromboembolic complications of the Symbion AVAD System. Artif Organs. 1989 Dec;13(6):532–538. doi: 10.1111/j.1525-1594.1989.tb01575.x. [DOI] [PubMed] [Google Scholar]
- Journois D., Pouard P., Mauriat P., Malhère T., Vouhé P., Safran D. Inhaled nitric oxide as a therapy for pulmonary hypertension after operations for congenital heart defects. J Thorac Cardiovasc Surg. 1994 Apr;107(4):1129–1135. [PubMed] [Google Scholar]
- Kanter K. R., McBride L. R., Pennington D. G., Swartz M. T., Ruzevich S. A., Miller L. W., Willman V. L. Bridging to cardiac transplantation with pulsatile ventricular assist devices. Ann Thorac Surg. 1988 Aug;46(2):134–140. doi: 10.1016/s0003-4975(10)65884-5. [DOI] [PubMed] [Google Scholar]
- Kormos R. L., Murali S., Dew M. A., Armitage J. M., Hardesty R. L., Borovetz H. S., Griffith B. P. Chronic mechanical circulatory support: rehabilitation, low morbidity, and superior survival. Ann Thorac Surg. 1994 Jan;57(1):51–58. doi: 10.1016/0003-4975(94)90364-6. [DOI] [PubMed] [Google Scholar]
- Levinson M. M., Smith R. G., Cork R. C., Gallo J., Emery R. W., Icenogle T. B., Ott R. A., Burns G. L., Copeland J. G. Thromboembolic complications of the Jarvik-7 total artificial heart: case report. Artif Organs. 1986 Jun;10(3):236–244. doi: 10.1111/j.1525-1594.1986.tb02552.x. [DOI] [PubMed] [Google Scholar]
- McGee M. G., Parnis S. M., Nakatani T., Myers T., Dasse K., Hare W. D., Duncan J. M., Poirier V. L., Frazier O. H. Extended clinical support with an implantable left ventricular assist device. ASAIO Trans. 1989 Jul-Sep;35(3):614–616. doi: 10.1097/00002480-198907000-00145. [DOI] [PubMed] [Google Scholar]
- Myers T. J., McGee M. G., Zeluff B. J., Radovancevic B., Frazier O. H. Frequency and significance of infections in patients receiving prolonged LVAD support. ASAIO Trans. 1991 Jul-Sep;37(3):M283–M285. [PubMed] [Google Scholar]
- Norman J. C., Brook M. I., Cooley D. A., Klima T., Kahan B. D., Frazier O. H., Keats A. S., Hacker J., Massin E. K., Duncan J. M. Total support of the circulation of a patient with post-cardiotomy stone-heart syndrome by a partial artificial heart (ALVAD) for 5 days followed by heart and kidney transplantation. Lancet. 1978 May 27;1(8074):1125–1127. doi: 10.1016/s0140-6736(78)90301-x. [DOI] [PubMed] [Google Scholar]
- Pae W. E., Jr, Pierce W. S. Temporary left ventricular assistance in acute myocardial infarction and cardiogenic shock: rationale and criteria for utilization. Chest. 1981 Jun;79(6):692–695. doi: 10.1378/chest.79.6.692. [DOI] [PubMed] [Google Scholar]
- Pennington D. G., McBride L. R., Kanter K. R., Miller L. W., Ruzevich S. A., Naunheim K., Swartz M. T., Termuhlen D. Bridging to heart transplantation with circulatory support devices. J Heart Transplant. 1989 Mar-Apr;8(2):116–123. [PubMed] [Google Scholar]
- Pennington D. G., McBride L. R., Peigh P. S., Miller L. W., Swartz M. T. Eight years' experience with bridging to cardiac transplantation. J Thorac Cardiovasc Surg. 1994 Feb;107(2):472–481. [PubMed] [Google Scholar]
- Pennington D. G., Samuels L. D., Williams G., Palmer D., Swartz M. T., Codd J. E., Merjavy J. P., Lagunoff D., Joist J. H. Experience with the Pierce-Donachy ventricular assist device in postcardiotomy patients with cardiogenic shock. World J Surg. 1985 Feb;9(1):37–46. doi: 10.1007/BF01656254. [DOI] [PubMed] [Google Scholar]
- Pierce W. S., Parr G. V., Myers J. L., Pae W. E., Jr, Bull A. P., Waldhausen J. A. Ventricular-assist pumping patients with cardiogenic shock after cardiac operations. N Engl J Med. 1981 Dec 31;305(27):1606–1610. doi: 10.1056/NEJM198112313052702. [DOI] [PubMed] [Google Scholar]
- Portner P. M., Oyer P. E., Pennington D. G., Baumgartner W. A., Griffith B. P., Frist W. R., Magilligan D. J., Jr, Noon G. P., Ramasamy N., Miller P. J. Implantable electrical left ventricular assist system: bridge to transplantation and the future. Ann Thorac Surg. 1989 Jan;47(1):142–150. doi: 10.1016/0003-4975(89)90256-7. [DOI] [PubMed] [Google Scholar]
- Rice L. B., Karchmer A. W. Artificial heart implantation: what limitations are imposed by infectious complications? JAMA. 1988 Feb 12;259(6):894–895. [PubMed] [Google Scholar]
- STUMP M. M., JORDAN G. L., Jr, DEBAKEY M. E., HALPERT B. ENDOTHELIUM GROWN FROM CIRCULATING BLOOD ON ISOLATED INTRAVASCULAR DACRON HUB. Am J Pathol. 1963 Sep;43:361–367. [PMC free article] [PubMed] [Google Scholar]
- Wessel D. L., Adatia I., Thompson J. E., Hickey P. R. Delivery and monitoring of inhaled nitric oxide in patients with pulmonary hypertension. Crit Care Med. 1994 Jun;22(6):930–938. doi: 10.1097/00003246-199406000-00009. [DOI] [PubMed] [Google Scholar]