Abstract
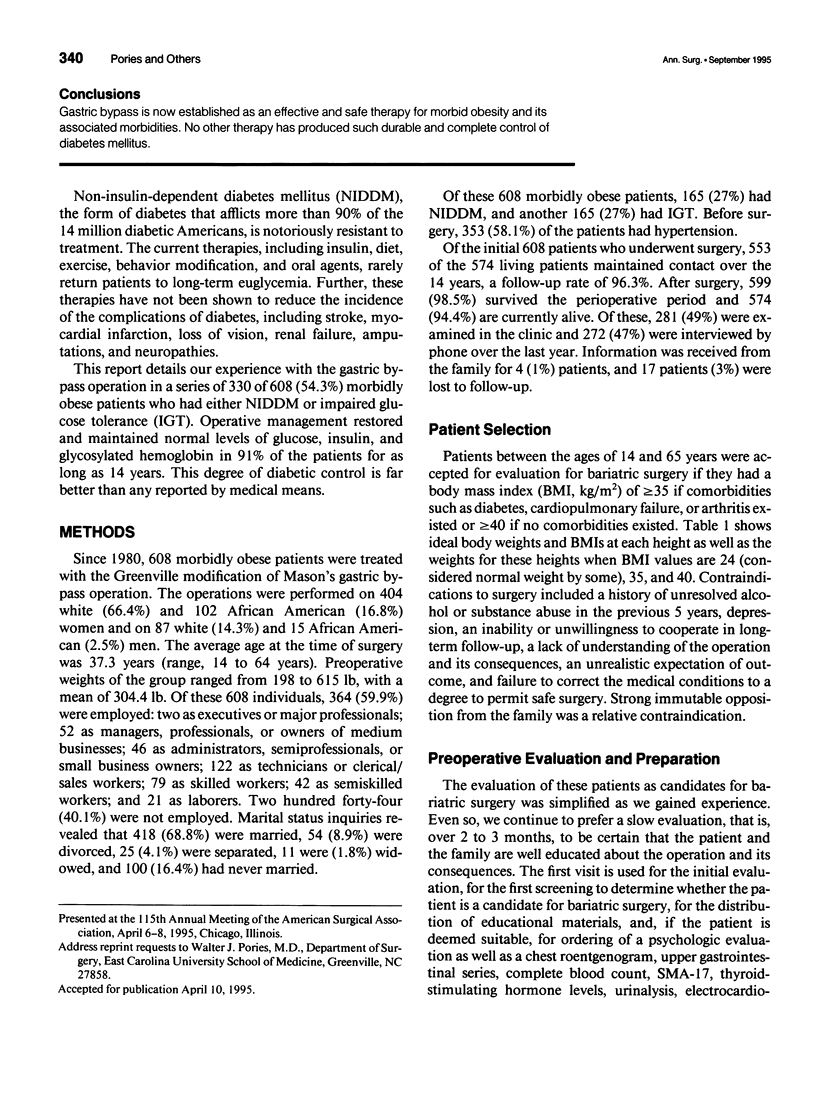
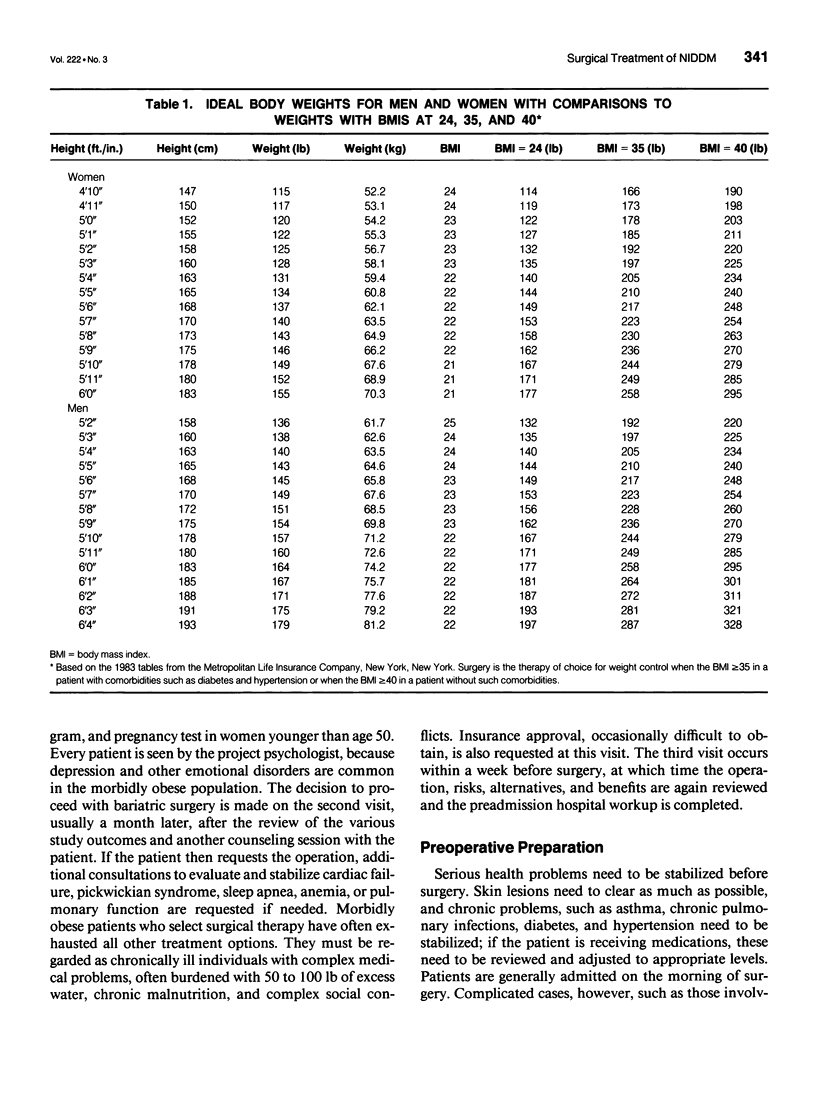
OBJECTIVE: This report documents that the gastric bypass operation provides long-term control for obesity and diabetes. SUMMARY BACKGROUND DATA: Obesity and diabetes, both notoriously resistant to medical therapy, continue to be two of our most common and serious diseases. METHODS: Over the last 14 years, 608 morbidly obese patients underwent gastric bypass, an operation that restricts caloric intake by (1) reducing the functional stomach to approximately 30 mL, (2) delaying gastric emptying with a c. 0.8 to 1.0 cm gastric outlet, and (3) excluding foregut with a 40 to 60 cm Roux-en-Y gastrojejunostomy. Even though many of the patients were seriously ill, the operation was performed with a perioperative mortality and complication rate of 1.5% and 8.5%, respectively. Seventeen of the 608 patients (< 3%) were lost to follow-up. RESULTS: Gastric bypass provides durable weight control. Weights fell from a preoperative mean of 304.4 lb (range, 198 to 615 lb) to 192.2 lb (range, 104 to 466) by 1 year and were maintained at 205.4 lb (range, 107 to 512 lb) at 5 years, 206.5 lb (130 to 388 lb) at 10 years, and 204.7 lb (158 to 270 lb) at 14 years. The operation provides long-term control of non-insulin-dependent diabetes mellitus (NIDDM). In those patients with adequate follow-up, 121 of 146 patients (82.9%) with NIDDM and 150 of 152 patients (98.7%) with glucose impairment maintained normal levels of plasma glucose, glycosylated hemoglobin, and insulin. These antidiabetic effects appear to be due primarily to a reduction in caloric intake, suggesting that insulin resistance is a secondary protective effect rather than the initial lesion. In addition to the control of weight and NIDDM, gastric bypass also corrected or alleviated a number of other comorbidities of obesity, including hypertension, sleep apnea, cardiopulmonary failure, arthritis, and infertility. Gastric bypass is now established as an effective and safe therapy for morbid obesity and its associated morbidities. No other therapy has produced such durable and complete control of diabetes mellitus.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Azevedo J. L., Jr, Carey J. O., Pories W. J., Morris P. G., Dohm G. L. Hypoxia stimulates glucose transport in insulin-resistant human skeletal muscle. Diabetes. 1995 Jun;44(6):695–698. doi: 10.2337/diab.44.6.695. [DOI] [PubMed] [Google Scholar]
- Barakat H. A., Carpenter J. W., McLendon V. D., Khazanie P., Leggett N., Heath J., Marks R. Influence of obesity, impaired glucose tolerance, and NIDDM on LDL structure and composition. Possible link between hyperinsulinemia and atherosclerosis. Diabetes. 1990 Dec;39(12):1527–1533. doi: 10.2337/diab.39.12.1527. [DOI] [PubMed] [Google Scholar]
- Boylan L. M., Sugerman H. J., Driskell J. A. Vitamin E, vitamin B-6, vitamin B-12, and folate status of gastric bypass surgery patients. J Am Diet Assoc. 1988 May;88(5):579–585. [PubMed] [Google Scholar]
- Carey J. O., Azevedo J. L., Jr, Morris P. G., Pories W. J., Dohm G. L. Okadaic acid, vanadate, and phenylarsine oxide stimulate 2-deoxyglucose transport in insulin-resistant human skeletal muscle. Diabetes. 1995 Jun;44(6):682–688. doi: 10.2337/diab.44.6.682. [DOI] [PubMed] [Google Scholar]
- Caro J. F., Sinha M. K., Raju S. M., Ittoop O., Pories W. J., Flickinger E. G., Meelheim D., Dohm G. L. Insulin receptor kinase in human skeletal muscle from obese subjects with and without noninsulin dependent diabetes. J Clin Invest. 1987 May;79(5):1330–1337. doi: 10.1172/JCI112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creutzfeldt W., Nauck M. Gut hormones and diabetes mellitus. Diabetes Metab Rev. 1992 Jul;8(2):149–177. doi: 10.1002/dmr.5610080206. [DOI] [PubMed] [Google Scholar]
- Doar J. W., Wilde C. E., Thompson M. E., Sewell P. F. Influence of treatment with diet alone on oral glucose-tolerance test and plasma sugar and insulin levels in patients with maturity-onset diabetes mellitus. Lancet. 1975 Jun 7;1(7919):1263–1266. doi: 10.1016/s0140-6736(75)92550-7. [DOI] [PubMed] [Google Scholar]
- Dohm G. L., Elton C. W., Friedman J. E., Pilch P. F., Pories W. J., Atkinson S. M., Jr, Caro J. F. Decreased expression of glucose transporter in muscle from insulin-resistant patients. Am J Physiol. 1991 Mar;260(3 Pt 1):E459–E463. doi: 10.1152/ajpendo.1991.260.3.E459. [DOI] [PubMed] [Google Scholar]
- Dohm G. L., Elton C. W., Raju M. S., Mooney N. D., DiMarchi R., Pories W. J., Flickinger E. G., Atkinson S. M., Jr, Caro J. F. IGF-I--stimulated glucose transport in human skeletal muscle and IGF-I resistance in obesity and NIDDM. Diabetes. 1990 Sep;39(9):1028–1032. doi: 10.2337/diab.39.9.1028. [DOI] [PubMed] [Google Scholar]
- Dohm G. L., Tapscott E. B., Pories W. J., Dabbs D. J., Flickinger E. G., Meelheim D., Fushiki T., Atkinson S. M., Elton C. W., Caro J. F. An in vitro human muscle preparation suitable for metabolic studies. Decreased insulin stimulation of glucose transport in muscle from morbidly obese and diabetic subjects. J Clin Invest. 1988 Aug;82(2):486–494. doi: 10.1172/JCI113622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J. E., Dohm G. L., Leggett-Frazier N., Elton C. W., Tapscott E. B., Pories W. P., Caro J. F. Restoration of insulin responsiveness in skeletal muscle of morbidly obese patients after weight loss. Effect on muscle glucose transport and glucose transporter GLUT4. J Clin Invest. 1992 Feb;89(2):701–705. doi: 10.1172/JCI115638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutniak M., Orskov C., Holst J. J., Ahrén B., Efendic S. Antidiabetogenic effect of glucagon-like peptide-1 (7-36)amide in normal subjects and patients with diabetes mellitus. N Engl J Med. 1992 May 14;326(20):1316–1322. doi: 10.1056/NEJM199205143262003. [DOI] [PubMed] [Google Scholar]
- Holst J. J. Glucagonlike peptide 1: a newly discovered gastrointestinal hormone. Gastroenterology. 1994 Dec;107(6):1848–1855. doi: 10.1016/0016-5085(94)90831-1. [DOI] [PubMed] [Google Scholar]
- Kellum J. M., Kuemmerle J. F., O'Dorisio T. M., Rayford P., Martin D., Engle K., Wolf L., Sugerman H. J. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg. 1990 Jun;211(6):763–771. doi: 10.1097/00000658-199006000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzmak LI. A Review of Seven Years' Experience with Silicone Gastric Banding. Obes Surg. 1991 Dec;1(4):403–408. doi: 10.1381/096089291765560809. [DOI] [PubMed] [Google Scholar]
- Long S. D., O'Brien K., MacDonald K. G., Jr, Leggett-Frazier N., Swanson M. S., Pories W. J., Caro J. F. Weight loss in severely obese subjects prevents the progression of impaired glucose tolerance to type II diabetes. A longitudinal interventional study. Diabetes Care. 1994 May;17(5):372–375. doi: 10.2337/diacare.17.5.372. [DOI] [PubMed] [Google Scholar]
- Peeples L. H., Carpenter J. W., Israel R. G., Barakat H. A. Alterations in low-density lipoproteins in subjects with abdominal adiposity. Metabolism. 1989 Oct;38(10):1029–1036. doi: 10.1016/0026-0495(89)90017-6. [DOI] [PubMed] [Google Scholar]
- Tanizawa Y., Riggs A. C., Elbein S. C., Whelan A., Donis-Keller H., Permutt M. A. Human glucagon-like peptide-1 receptor gene in NIDDM. Identification and use of simple sequence repeat polymorphisms in genetic analysis. Diabetes. 1994 Jun;43(6):752–757. doi: 10.2337/diab.43.6.752. [DOI] [PubMed] [Google Scholar]


