Abstract
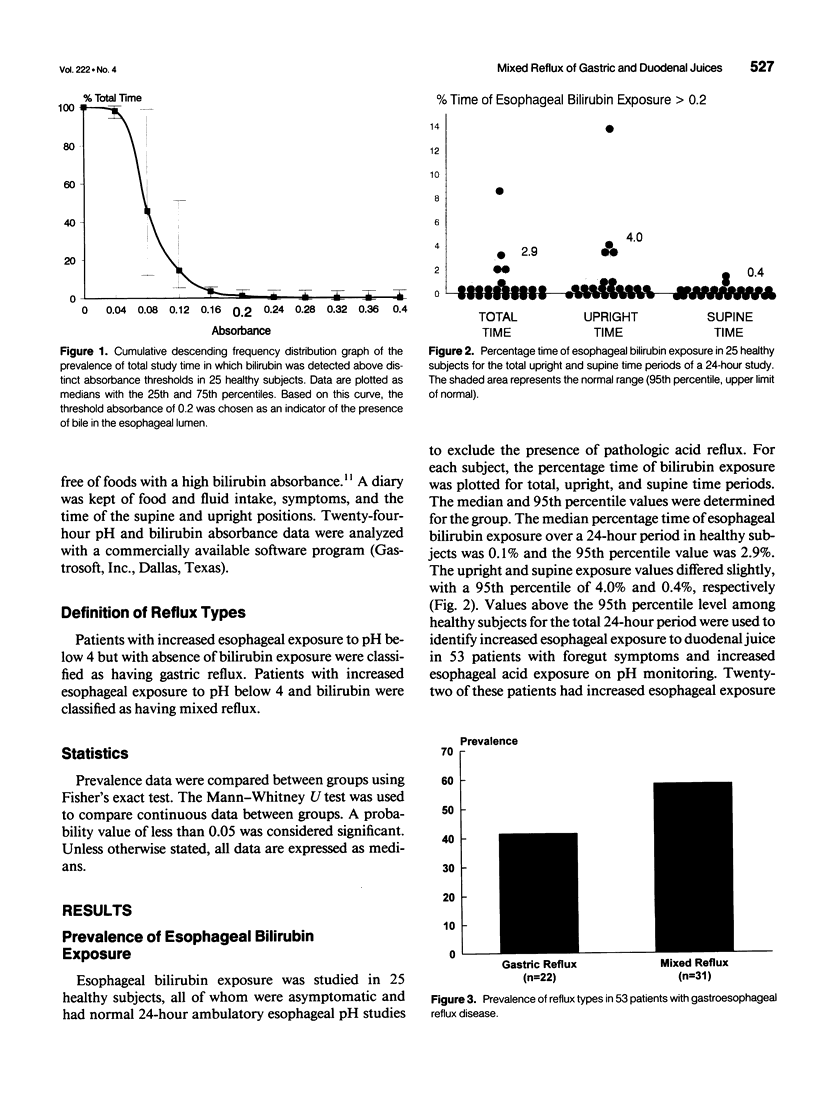
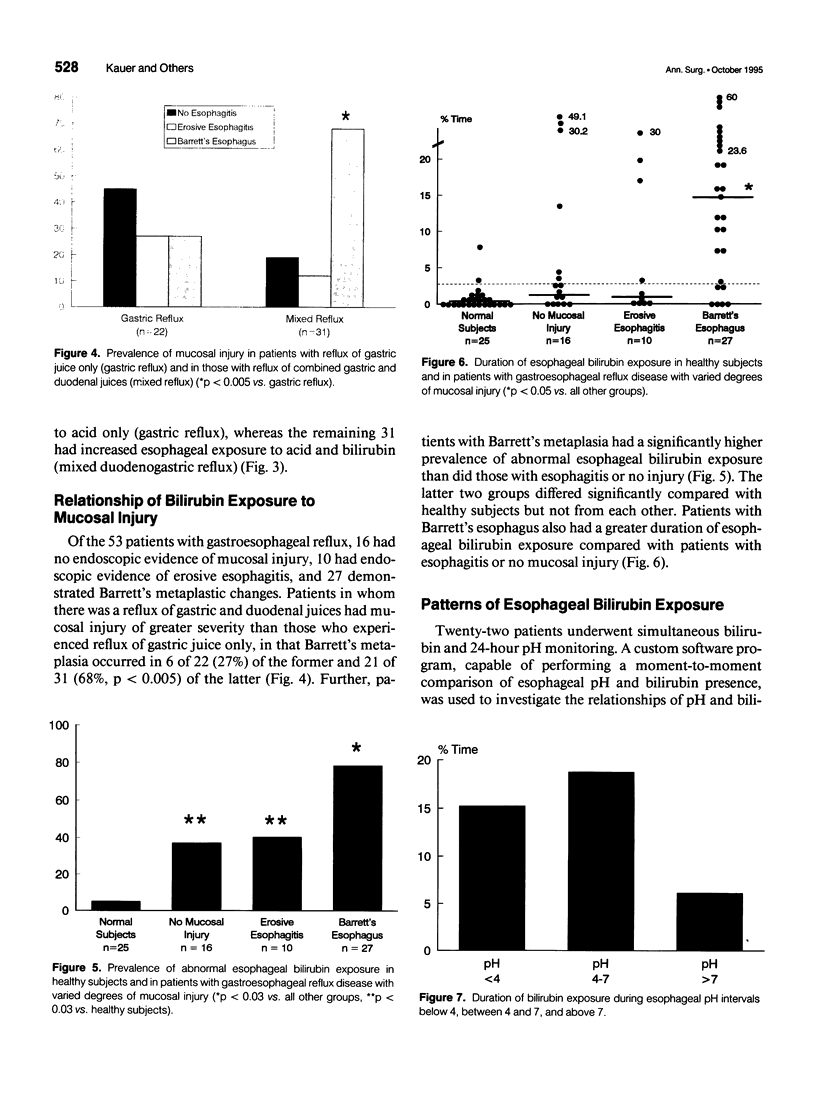
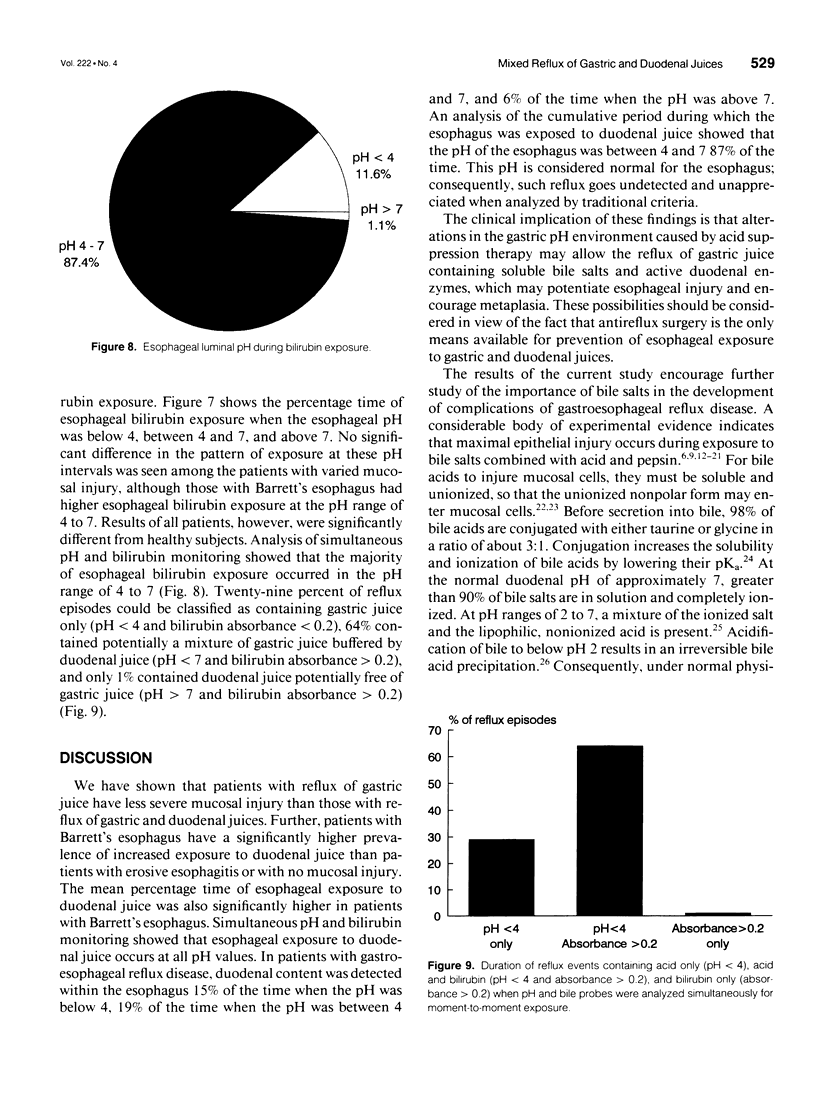
OBJECTIVE: The author's goal was to determine the role of duodenal components in the development of complications of gastroesophageal reflux disease. SUMMARY AND BACKGROUND DATA: There is a disturbing increase in the prevalence of complications, specifically the development of Barrett's esophagus among patients with gastroesophageal reflux disease. Earlier studies using pH monitoring and aspiration techniques have shown that increased esophageal exposure to fluid with a pH above 7, that is, of potential duodenal origin, may be an important factor in this phenomenon. METHODS: The presence of duodenal content in the esophagus was studied in 53 patients with gastroesophageal reflux disease confirmed by 24-hour pH monitoring. A portable spectrophotometer (Bilitec 2000, Synectics, Inc.) with a fiberoptic probe was used to measure intraluminal bilirubin as a marker for duodenal juice in the esophagus. Normal values for bilirubin monitoring were established for 25 healthy subjects. In a subgroup of 22 patients, a custom-made program was used to correlate simultaneous pH and bilirubin absorbance readings. RESULTS: Fifty-eight percent of patients were found to have increased esophageal exposure to gastric and duodenal juices. The degree of mucosal damage increased when duodenal juice was refluxed into the esophagus, in that patients with Barrett's metaplasia (n = 27) had a significantly higher prevalence of abnormal esophageal bilirubin exposure than did those with erosive esophagitis (n = 10) or with no injury (n = 16). They also had a greater esophageal bilirubin exposure compared with patients without Barrett's changes, with or without esophagitis. The correlation of pH and bilirubin monitoring showed that the majority (87%) of esophageal bilirubin exposure occurred when the pH of the esophagus was between 4 and 7. CONCLUSIONS: Reflux of duodenal juice in gastroesophageal reflux disease is more common than pH studies alone would suggest. The combined reflux of gastric and duodenal juices causes severe esophageal mucosal damage. The vast majority of duodenal reflux occurs at a pH range of 4 to 7, at which bile acids, the major component of duodenal juice, are capable of damaging the esophageal mucosa.
Full text
PDF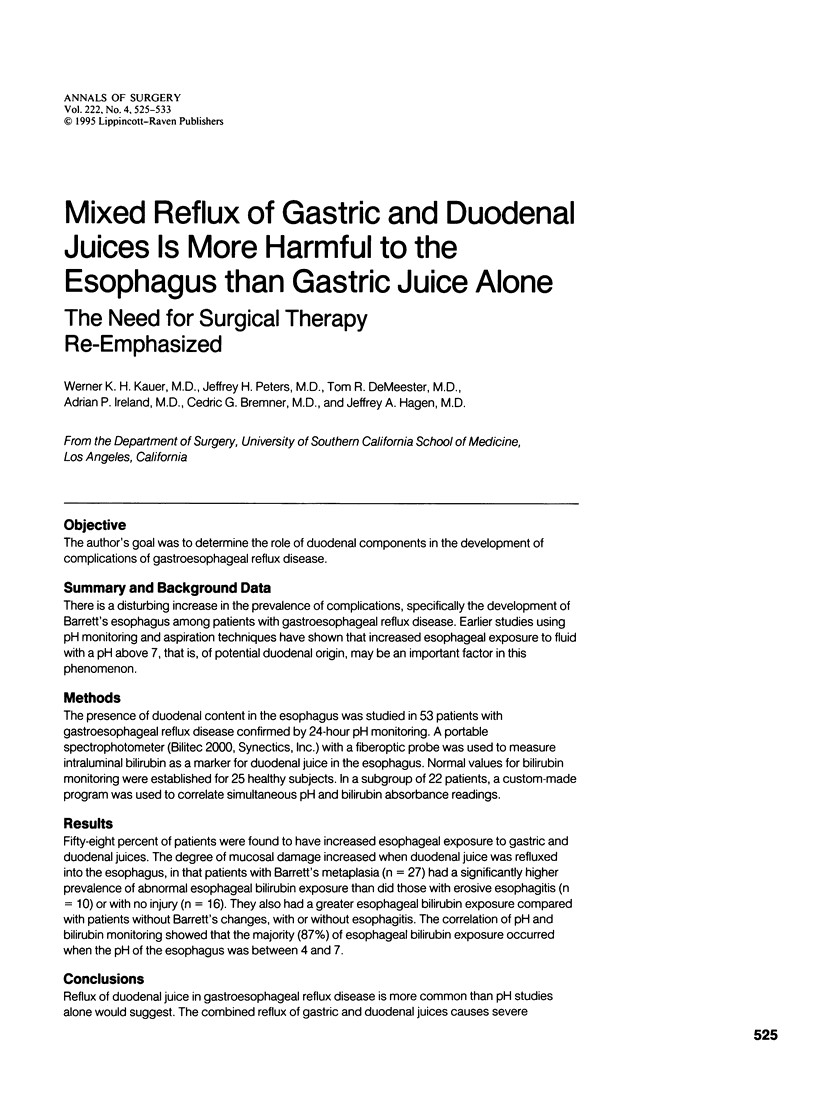

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bremner R. M., Crookes P. F., DeMeester T. R., Peters J. H., Stein H. J. Concentration of refluxed acid and esophageal mucosal injury. Am J Surg. 1992 Nov;164(5):522–527. doi: 10.1016/s0002-9610(05)81193-6. [DOI] [PubMed] [Google Scholar]
- Champion G., Richter J. E., Vaezi M. F., Singh S., Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett's esophagus. Gastroenterology. 1994 Sep;107(3):747–754. doi: 10.1016/0016-5085(94)90123-6. [DOI] [PubMed] [Google Scholar]
- DeMeester T. R., Bonavina L., Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg. 1986 Jul;204(1):9–20. doi: 10.1097/00000658-198607000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillison E. W., De Castro V. A., Nyhus L. M., Kusakari K., Bombeck C. T. The significance of bile in reflux esophagitis. Surg Gynecol Obstet. 1972 Mar;134(3):419–424. [PubMed] [Google Scholar]
- Gotley D. C., Morgan A. P., Cooper M. J. Bile acid concentrations in the refluxate of patients with reflux oesophagitis. Br J Surg. 1988 Jun;75(6):587–590. doi: 10.1002/bjs.1800750632. [DOI] [PubMed] [Google Scholar]
- Harmon J. W., Johnson L. F., Maydonovitch C. L. Effects of acid and bile salts on the rabbit esophageal mucosa. Dig Dis Sci. 1981 Jan;26(1):65–72. doi: 10.1007/BF01307977. [DOI] [PubMed] [Google Scholar]
- Hinder R. A., Filipi C. J., Wetscher G., Neary P., DeMeester T. R., Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994 Oct;220(4):472–483. doi: 10.1097/00000658-199410000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iftikhar S. Y., Ledingham S., Steele R. J., Evans D. F., Lendrum K., Atkinson M., Hardcastle J. D. Bile reflux in columnar-lined Barrett's oesophagus. Ann R Coll Surg Engl. 1993 Nov;75(6):411–416. [PMC free article] [PubMed] [Google Scholar]
- Jamieson J. R., Stein H. J., DeMeester T. R., Bonavina L., Schwizer W., Hinder R. A., Albertucci M. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol. 1992 Sep;87(9):1102–1111. [PubMed] [Google Scholar]
- Kauer W. K., Burdiles P., Ireland A. P., Clark G. W., Peters J. H., Bremner C. G., DeMeester T. R. Does duodenal juice reflux into the esophagus of patients with complicated GERD? Evaluation of a fiberoptic sensor for bilirubin. Am J Surg. 1995 Jan;169(1):98–104. doi: 10.1016/s0002-9610(99)80116-0. [DOI] [PubMed] [Google Scholar]
- Kivilaakso E., Fromm D., Silen W. Effect of bile salts and related compounds on isolated esophageal mucosa. Surgery. 1980 Mar;87(3):280–285. [PubMed] [Google Scholar]
- Klinkenberg-Knol E. C., Festen H. P., Jansen J. B., Lamers C. B., Nelis F., Snel P., Lückers A., Dekkers C. P., Havu N., Meuwissen S. G. Long-term treatment with omeprazole for refractory reflux esophagitis: efficacy and safety. Ann Intern Med. 1994 Aug 1;121(3):161–167. doi: 10.7326/0003-4819-121-3-199408010-00001. [DOI] [PubMed] [Google Scholar]
- Krähenbühl S., Talos C., Fischer S., Reichen J. Toxicity of bile acids on the electron transport chain of isolated rat liver mitochondria. Hepatology. 1994 Feb;19(2):471–479. doi: 10.1002/hep.1840190228. [DOI] [PubMed] [Google Scholar]
- Lillemoe K. D., Gadacz T. R., Harmon J. W. Bile absorption occurs during disruption of the esophageal mucosal barrier. J Surg Res. 1983 Jul;35(1):57–62. doi: 10.1016/0022-4804(83)90126-9. [DOI] [PubMed] [Google Scholar]
- Lillemoe K. D., Johnson L. F., Harmon J. W. Alkaline esophagitis: a comparison of the ability of components of gastroduodenal contents to injure the rabbit esophagus. Gastroenterology. 1983 Sep;85(3):621–628. [PubMed] [Google Scholar]
- Lillemoe K. D., Johnson L. F., Harmon J. W. Role of the components of the gastroduodenal contents in experimental acid esophagitis. Surgery. 1982 Aug;92(2):276–284. [PubMed] [Google Scholar]
- Lillemoe K. D., Johnson L. F., Harmon J. W. Taurodeoxycholate modulates the effects of pepsin and trypsin in experimental esophagitis. Surgery. 1985 Jun;97(6):662–667. [PubMed] [Google Scholar]
- Moffat R. C., Berkas E. M. Bile esophagitis. Arch Surg. 1965 Dec;91(6):963–966. doi: 10.1001/archsurg.1965.01320180097021. [DOI] [PubMed] [Google Scholar]
- Moore R., Madri J., Carlson S., Madara J. L. Collagens facilitate epithelial migration in restitution of native guinea pig intestinal epithelium. Gastroenterology. 1992 Jan;102(1):119–130. doi: 10.1016/0016-5085(92)91791-2. [DOI] [PubMed] [Google Scholar]
- Ostrow J. D. Bilitec to quantitate duodenogastric reflux: is it valid? Gastroenterology. 1995 Apr;108(4):1332–1334. doi: 10.1016/0016-5085(95)90256-2. [DOI] [PubMed] [Google Scholar]
- Pera M., Cameron A. J., Trastek V. F., Carpenter H. A., Zinsmeister A. R. Increasing incidence of adenocarcinoma of the esophagus and esophagogastric junction. Gastroenterology. 1993 Feb;104(2):510–513. doi: 10.1016/0016-5085(93)90420-h. [DOI] [PubMed] [Google Scholar]
- Peters J. H., Heimbucher J., Kauer W. K., Incarbone R., Bremner C. G., DeMeester T. R. Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg. 1995 Apr;180(4):385–393. [PubMed] [Google Scholar]
- Salo J. A., Kivilaakso E. Role of bile salts and trypsin in the pathogenesis of experimental alkaline esophagitis. Surgery. 1983 Apr;93(4):525–532. [PubMed] [Google Scholar]
- Schweitzer E. J., Bass B. L., Batzri S., Harmon J. W. Bile acid accumulation by rabbit esophageal mucosa. Dig Dis Sci. 1986 Oct;31(10):1105–1113. doi: 10.1007/BF01300265. [DOI] [PubMed] [Google Scholar]
- Schweitzer E. J., Harmon J. W., Bass B. L., Batzri S. Bile acid efflux precedes mucosal barrier disruption in the rabbit esophagus. Am J Physiol. 1984 Nov;247(5 Pt 1):G480–G485. doi: 10.1152/ajpgi.1984.247.5.G480. [DOI] [PubMed] [Google Scholar]
- Spivey J. R., Bronk S. F., Gores G. J. Glycochenodeoxycholate-induced lethal hepatocellular injury in rat hepatocytes. Role of ATP depletion and cytosolic free calcium. J Clin Invest. 1993 Jul;92(1):17–24. doi: 10.1172/JCI116546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein H. J., Barlow A. P., DeMeester T. R., Hinder R. A. Complications of gastroesophageal reflux disease. Role of the lower esophageal sphincter, esophageal acid and acid/alkaline exposure, and duodenogastric reflux. Ann Surg. 1992 Jul;216(1):35–43. doi: 10.1097/00000658-199207000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein H. J., Feussner H., Kauer W., DeMeester T. R., Siewert J. R. Alkaline gastroesophageal reflux: assessment by ambulatory esophageal aspiration and pH monitoring. Am J Surg. 1994 Jan;167(1):163–168. doi: 10.1016/0002-9610(94)90068-x. [DOI] [PubMed] [Google Scholar]
- Stoker D. L., Williams J. G. Alkaline reflux oesophagitis. Gut. 1991 Oct;32(10):1090–1092. doi: 10.1136/gut.32.10.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]


