ABSTRACT
Merkel cell carcinoma (MCC) is a rare neuroendocrine carcinoma with aggressive behavior that predominantly affects the sun-damaged skin of the head and neck regions, extremities, and trunk of white older individuals. We present a unique case of MCC presenting as painless upper lip swelling, initially mistaken for a benign lesion. Histopathological examination revealed characteristic features of MCC. Early diagnosis and intervention led to improved outcomes. This case emphasizes the importance of considering MCC in the differential diagnosis of seemingly innocuous cutaneous lesions. To the best of our knowledge, 24 cases of MCC of the lips have been reported to date in the English language literature, and this case is probably the first to be reported from the Middle East region.
Keywords: Elderly, lip, Merkel cell carcinoma
Introduction
Merkel cell carcinoma (MCC), a rare, aggressive, neuroendocrine carcinoma arising from Merkel cells in the skin, presents a unique set of challenges in its clinical understanding and management. Despite its infrequent occurrence, MCC demands attention due to its potential for aggressive behavior and the nuances observed in its diverse clinical presentations including its high chances for recurrence and metastases.
Traditionally associated with elderly individuals of fair complexion and sun-exposed areas, MCC has recently demonstrated a broader epidemiological footprint. While existing literature has predominantly focused on Caucasian populations, a shifting narrative is apparent with emerging data suggesting distinctive patterns in non-Caucasian cohorts.[1] This dynamic epidemiological perspective prompts a reconsideration of established paradigms, necessitating a more comprehensive understanding of MCC across diverse demographic backgrounds.
This article aims to contribute to this evolving narrative, particularly through the presentation of a distinctive MCC case involving an elderly Emirati male. The uniqueness of the case lies not only in its demographic context but also in the atypical presentation as painless upper lip swelling, adding to the spectrum of clinical scenarios that clinicians may encounter. As we navigate through this case study and the broader MCC literature, the goal is to provide insights that are clinically relevant and contribute to the refinement of diagnostic approaches.
By presenting an overview of MCC’s clinical characteristics, exploring its demographic variations, and delving into the complexities of atypical presentations, this article seeks to offer valuable insights to the medical community. Here, we report an unusual case of MCC presenting as a benign upper lip swelling, highlighting the diagnostic challenge it posed.
Case Presentation
An 87-year-old elderly Emirati Arab male, known to have well controlled type 2 diabetes, hypertension, dyslipidemia, essential thrombocytosis, CKD stage 4, ischemic heart disease, cholecystectomy in 2017, and ERCP done in 2019 with multiple stones presented to us with complaints of nausea and vomiting of 2 days duration associated with fever of one day duration. In view of cholestatic liver function tests, ERCP was performed, and a plastic stent was inserted with a good drain. Serology was negative for HbsAg and HIV. He was also noted to have an erythematous plaque on the right upper lip extending to the nasolabial fold, induration and nodules felt under the plaque. He had been noticing this lesion for the past 2–3 weeks and was gradually progressive. It was nontender and not associated with any itching. There was no associated lymphadenopathy. Chest X-ray was normal. MRI of the face and neck revealed a poorly defined, relatively homogenous subcutaneous lesion with intermediate signal intensity on T1W and T2W images, high signal on STIR and multiple flow voids within the altered signals. Biopsy of the lesion revealed a diffusely infiltrative carcinoma within the dermis. Carcinoma cells are composed of small round blue cell carcinomas with a high N: C ratio, round/oval nuclei, finely dispersed chromatin (salt and pepper) [Figure 1], indistinct nucleoli and scant cytoplasm. Conspicuous mitoses and apoptotic bodies are seen in between. There is nuclear molding and crush artifact also noted. In addition, prominent solar elastosis and a telangiectatic blood vessels are seen in the superficial dermis. Immunohistochemistry revealed diffuse positivity for synaptophysin [Figure 2], chromogranin, and CD56 in the carcinoma cells. CK (AE 1/AE3) [Figure 3] was positive with focal paranuclear staining [Figures 4 and 5], and Ki67 showed a high proliferative index. CD45, CD 20, CD3, CD38, CD30, and Melan-A are negative in carcinoma cells. Additional IHC markers were done; TTF-1 was negative [Figure 6] and CK20 is positive in the carcinoma cell, which confirms the diagnosis of Merkel cell carcinoma and ruled out metastatic deposit of small cell carcinoma of the lung. MCPyV was not done. Following diagnosis, the patient was discharged home with advise to follow-up with the oncologist advise, but he died at home a week later, presumably due to a cardiac event.
Figure 1.
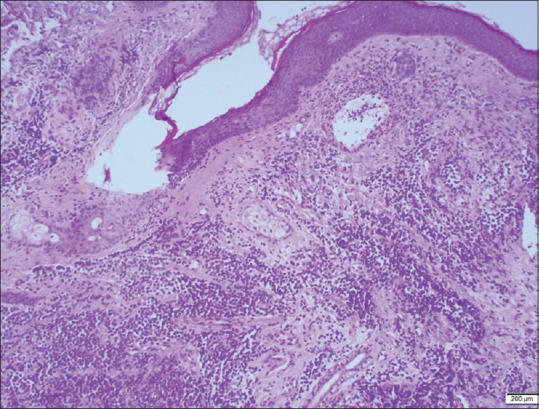
Neoplasm is composed of cells arranged in sheets, nests and trabeculae
Figure 2.
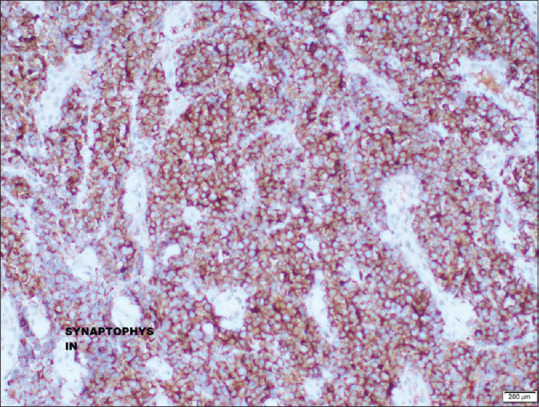
Cells are positive for synaptophysin
Figure 3.

Section shows skin with dermis showing an infiltrating neoplasm
Figure 4.

Cells are small, round with high nuclear cytoplasmic ratio, round vesicular nuclei with small nucleoli. Cytoplasm is scanty. Stroma showing lymphocytic infiltration
Figure 5.

Cells are positive for CKAE1/AE3
Figure 6.

Cells are negative for TTF-1
Discussion
MCC is a rare and aggressive neuroendocrine carcinoma arising from Merkel cells within the skin.[2] With an annual incidence rate of approximately 0.7 per 100,000 individuals, MCC represents a diagnostic challenge due to its uncommon occurrence and diverse clinical presentations.[3] Traditionally, MCC has been associated with elderly Caucasian individuals and typically presents as a rapidly growing, painless nodule in sun-exposed areas. However, the literature has recently witnessed an expanding understanding of MCC epidemiology, revealing intriguing patterns in non-Caucasian populations. Typically, it manifests as a rapidly expanding, painless nodule in sun-exposed areas of older individuals.[4] However, the presentation of MCC in the upper lip, as in this case, is an atypical occurrence.[5] To date, only a limited number of MCC cases involving the lips have been documented in the English language literature.[6,7] Histopathologically, MCC is characterized by nests of small, round, blue cells with scant cytoplasm, prominent nuclei, and characteristic “salt-and-pepper” chromatin.[8] Immunohistochemistry plays a pivotal role in confirming the diagnosis, with markers such as CK20, chromogranin, synaptophysin, and CD56 commonly employed.[2,8]
The epidemiological landscape of MCC is characterized by its rarity and predilection for the elderly. Most reported cases are Caucasians, particularly those with fair skin and prolonged sun exposure. The carcinoma frequently arises on the head and neck, extremities, and trunk, areas prone to sun damage.[3] Moreover, MCC is more prevalent in men, with a male-to-female ratio of approximately 2:1.[3] Despite these well-established patterns, an intriguing shift is noted in non-Caucasian populations. Increased frequency is noted in immunosuppressed individuals—organ transplant recipient and individuals afflicted with HIV or hematological malignancies—all of which was negative in our patient. The risk of MCC increases in patients with other malignancies, especially hematological malignancies like multiple myeloma, chronic lymphocytic leukemia and malignant melanoma.[9]
It is hypothesized that MCC has two different etiologies: Merkel cell polyoma virus (MCPyV) positive MCC originating from dermal fibroblasts and MCPyV-negative MCCs from epidermal keratinocytes, although this is still a debatable topic. Ultraviolet radiation exposure, especially sun, plays an important role in the etiology of many MCC, affecting predominantly sun exposed areas
MCC typically presents as a rapidly growing, firm, nontender, shiny flesh colored or bluish red intracutaneous nodule, mostly in sun exposed areas and a majority of the lesions reported in the head and neck region. It is often clinically misdiagnosed as a benign lesion like a cyst, lipoma or a pyogenic granuloma.
Research has indicated that MCC in non-Caucasian individuals tends to present at a later age compared to Caucasians, and the carcinomas often arise in non–sun-exposed regions (Heath et al., 2008).[8] The clinical presentation in these populations may differ, necessitating heightened awareness among clinicians. The atypical case of MCC in an elderly Emirati male, as presented in this manuscript, underscores the importance of recognizing diverse clinical presentations, especially in regions with unique demographics and sun exposure patterns.
Early diagnosis and intervention are pivotal, as MCC displays aggressive behavior and has a propensity for local recurrence and distant metastasis.[10] A multidisciplinary approach encompassing surgical resection, radiation therapy, and, in advanced cases, systemic therapies is often employed in the treatment of MCC.[10] It is noteworthy that the incidence of MCC in non-Caucasian populations is less common, with the majority of reported cases and epidemiological studies focusing predominantly on Caucasians.[11,12] This underscores the need for further research to comprehend the prevalence, clinical behavior, and optimal management strategies of MCC in more diverse racial and ethnic groups.
While the bulk of MCC literature has been centered on Caucasian populations, recent efforts have aimed at elucidating the characteristics of MCC in non-Caucasian groups. A systematic review by Heath et al.[1] explored MCC cases in African American, Asian, and Hispanic individuals. The study revealed that MCC in these populations often demonstrated distinct clinical and histopathological features. Notably, the carcinomas were more likely to occur in non–sun-exposed areas, challenging the traditional understanding of MCC’s predilection for sun-exposed skin. In the context of the Middle East, limited data are available regarding the prevalence and clinical behavior of MCC. This scarcity of data underscores the need for increased awareness and research in non-Caucasian populations to better understand MCC’s epidemiology, clinical behavior, and optimal management strategies.
While MCC typically manifests as a painless nodule, its presentations can be highly variable, contributing to the diagnostic challenge. Notably, MCC involving the lips is a rare occurrence, with only a limited number of cases reported in the literature. A comprehensive review of MCC cases involving lip lesions by Smith et al.,[13] emphasizing the rarity of this anatomical presentation. The case presented in this manuscript adds to this limited body of evidence, specifically highlighting the unique presentation of MCC as painless upper lip swelling.
The atypical presentation of MCC in the upper lip region necessitates a reconsideration of the traditional diagnostic approach to cutaneous lesions in this area. Clinicians should be vigilant in recognizing MCC as a potential differential diagnosis, especially when faced with seemingly benign lesions in uncommon anatomical locations.
Other differential diagnosis of MCC is basal cell carcinoma (which has neuroendocrine-type chromatin and immunolabeling with chromogranin and Cam5.2 shall also be positive), melanoma (has large irregular nuclei and prominent cherry-red nucleoli), metastatic neuroendocrine carcinoma, lymphoma, sebaceous carcinoma, Ewing sarcoma, squamous cell carcinoma. In summary, the evolving literature on MCC epidemiology, particularly in non-Caucasian populations, challenges traditional paradigms associated with this aggressive neuroendocrine carcinoma. The atypical case presented here contributes to this growing body of knowledge, emphasizing the importance of recognizing diverse clinical presentations and the need for further research in underrepresented populations.
Conclusion
In conclusion, we present an extraordinary case of MCC masquerading as a benign upper lip swelling in an elderly Emirati patient. This case serves as a poignant reminder of the diagnostic challenges that clinicians may encounter when faced with atypical presentations of MCC. Through careful histopathological evaluation and precise immunohistochemical analysis, a definitive diagnosis was achieved, facilitating early intervention, and leading to improved outcomes. The rarity of MCC in the upper lip region underscores the importance of considering this aggressive neuroendocrine carcinoma in the differential diagnosis of lip lesions. We contribute this case to the evolving body of literature on MCC, particularly in non-Caucasian populations, emphasizing the need for heightened clinical suspicion and a multidisciplinary approach for timely diagnosis and optimal management.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil.
References
- 1.Toker C. Trabecular carcinoma of the skin. Arch Dermatol. 1972;106:501–4. [doi: 10.1001/archderm.1972.01620160039008] [PubMed] [Google Scholar]
- 2.Chiarelli TG, Grant-Kels JM, Sporn JR, Rezuke WN, Whalen JD. Unusual presentation of a Merkel cell carcinoma. J Am Acad Dermatol. 2000;42:366–70. doi: 10.1016/s0190-9622(00)90114-2. [doi: 10.1016/S0190-9622(00)90114-2] [DOI] [PubMed] [Google Scholar]
- 3.Pulitzer MP, Amin BD, Busam KJ. Merkel Cell Carcinoma: Review. Adv Anat Pathol. 2009;16:135–44. doi: 10.1097/PAP.0b013e3181a12f5a. [doi: 10.1097/PAP] [DOI] [PubMed] [Google Scholar]
- 4.Harms KL, Healy MA, Nghiem P, Sober AJ, Johnson TM, Bichakjian CK, et al. Analysis of prognostic factors from 9387 Merkel cell carcinoma cases forms the basis for the new 8th Edition AJCC staging system. Ann Surg Oncol. 2016;23:3564–71. doi: 10.1245/s10434-016-5266-4. [doi: 10.1245/s10434-016-5302-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Becker JC, Stang A, DeCaprio JA, Cerroni L, Lebbé C, Veness M, et al. Merkel cell carcinoma. Nat Rev Dis Primers. 2017;3:17077. doi: 10.1038/nrdp.2017.77. [doi: 10.1038/nrdp.2017.77] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koljonen V, Kukko H, Pukkala E, Sankila R, Böhling T, Tukiainen E, et al. Chronic lymphocytic leukemia patients have a high risk of Merkel-cell polyomavirus DNA-positive Merkel-cell carcinoma. Br J Cancer. 2009;101:1444–7. doi: 10.1038/sj.bjc.6605306. [doi: 10.1038/sj.bjc.6605306] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemos BD, Storer BE, Iyer JG, Phillips JL, Bichakjian CK, Fang LC, et al. Pathologic nodal evaluation improves prognostic accuracy in Merkel cell carcinoma: analysis of 5823 cases as the basis of the first consensus staging system. J Am Acad Dermatol. 2010;63:751–61. doi: 10.1016/j.jaad.2010.02.056. [doi: 10.1016/j.jaad.2010.02.056] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heath M, Jaimes N, Lemos B, Mostaghimi A, Wang LC, Peñas PF, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: The AEIOU features. J Am Acad Dermatol. 2008;58:375–81. doi: 10.1016/j.jaad.2007.11.020. [doi: 10.1016/j.jaad.2007.11.020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith KJ, Skelton HG, 3rd, Holland TT, Morgan AM, Lupton GP. Neuroendocrine (Merkel cell) carcinoma with an intraepidermal component. Am J Dermatopathol. 1993;15:528–33. doi: 10.1097/00000372-199312000-00002. [doi: 10.1097/00000372-199312000-00002] [DOI] [PubMed] [Google Scholar]
- 10.Howard RA, Dores GM, Curtis RE, Anderson WF, Travis LB. Merkel cell carcinoma and multiple primary cancers. Cancer Epidemiol Biomarkers Prev. 2006;15:1545–9. doi: 10.1158/1055-9965.EPI-05-0895. doi: 10.1158/1055-9965.EPI-05-0895. [DOI] [PubMed] [Google Scholar]
- 11.Mohsin N, Martin MR, Reed DJ, Vilasi SM, Miao L, Hill NT, Brownell I. Differences in Merkel Cell Carcinoma Presentation and Outcomes Among Racial and Ethnic Groups. JAMA Dermatol. 2023;159:536–540. doi: 10.1001/jamadermatol.2023.0061. doi: 10.1001/jamadermatol.2023.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tothill R, Estall V, Rischin D. Merkel cell carcinoma: emerging biology, current approaches, and future directions. Am Soc Clin Oncol Educ Book. 2015:e519–26. doi: 10.14694/EdBook_AM.2015.35.e519. doi: 10.14694/EdBook_AM.2015.35.e519. [DOI] [PubMed] [Google Scholar]
- 13.Ezaldein HH, Ventura A, DeRuyter NP, Yin ES, Giunta A. Understanding the influence of patient demographics on disease severity, treatment strategy, and survival outcomes in merkel cell carcinoma: a surveillance, epidemiology, and end-results study. Oncoscience. 2017;4:106–114. doi: 10.18632/oncoscience.358. doi: 10.18632/oncoscience.358. [DOI] [PMC free article] [PubMed] [Google Scholar]


