Abstract
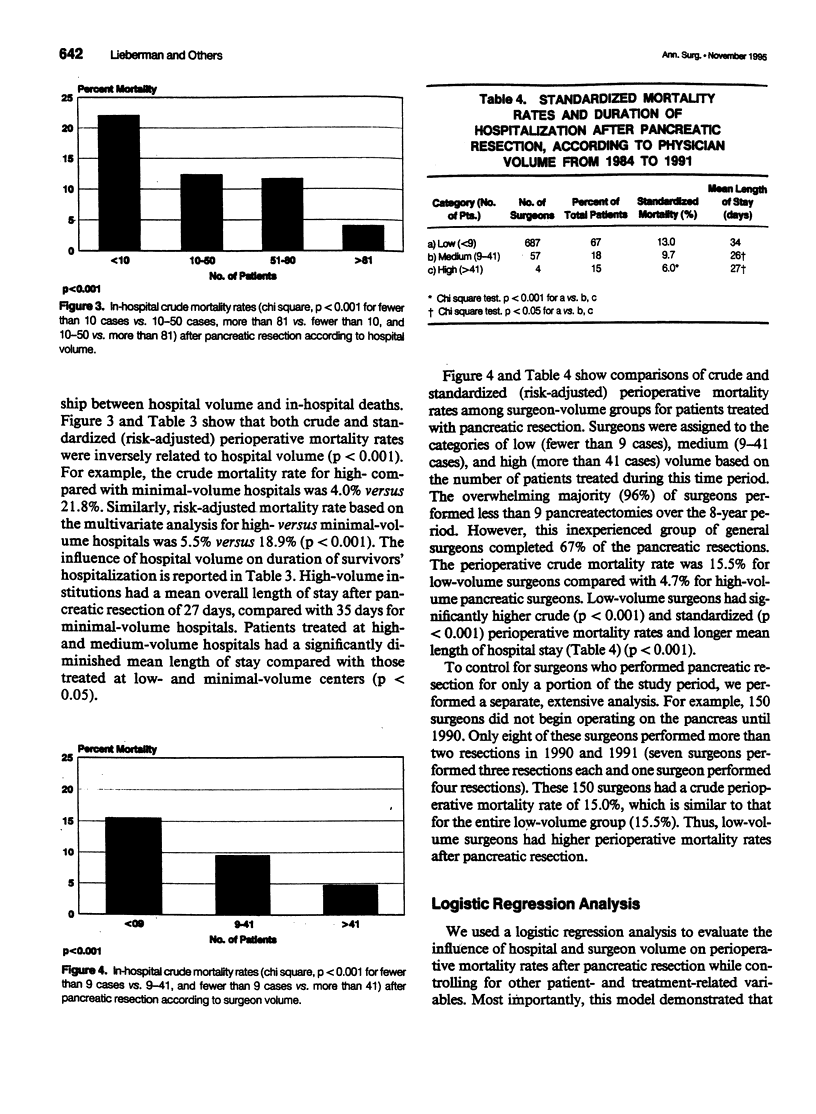
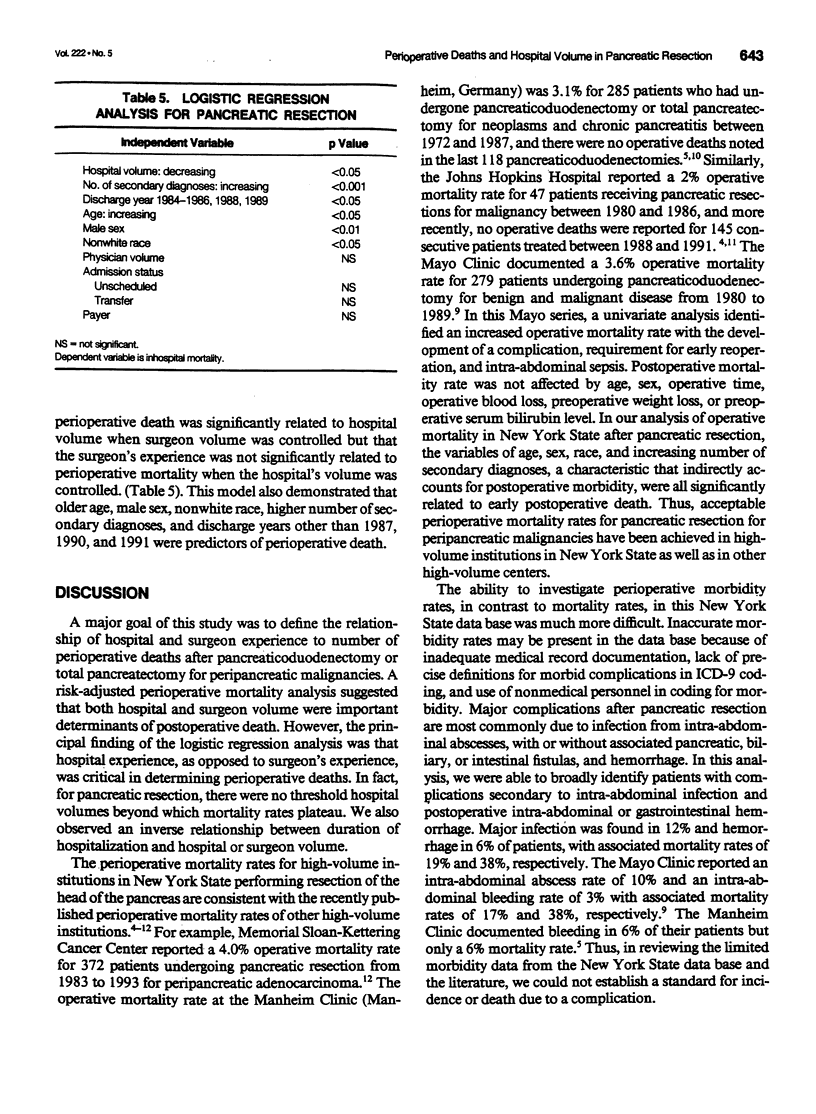
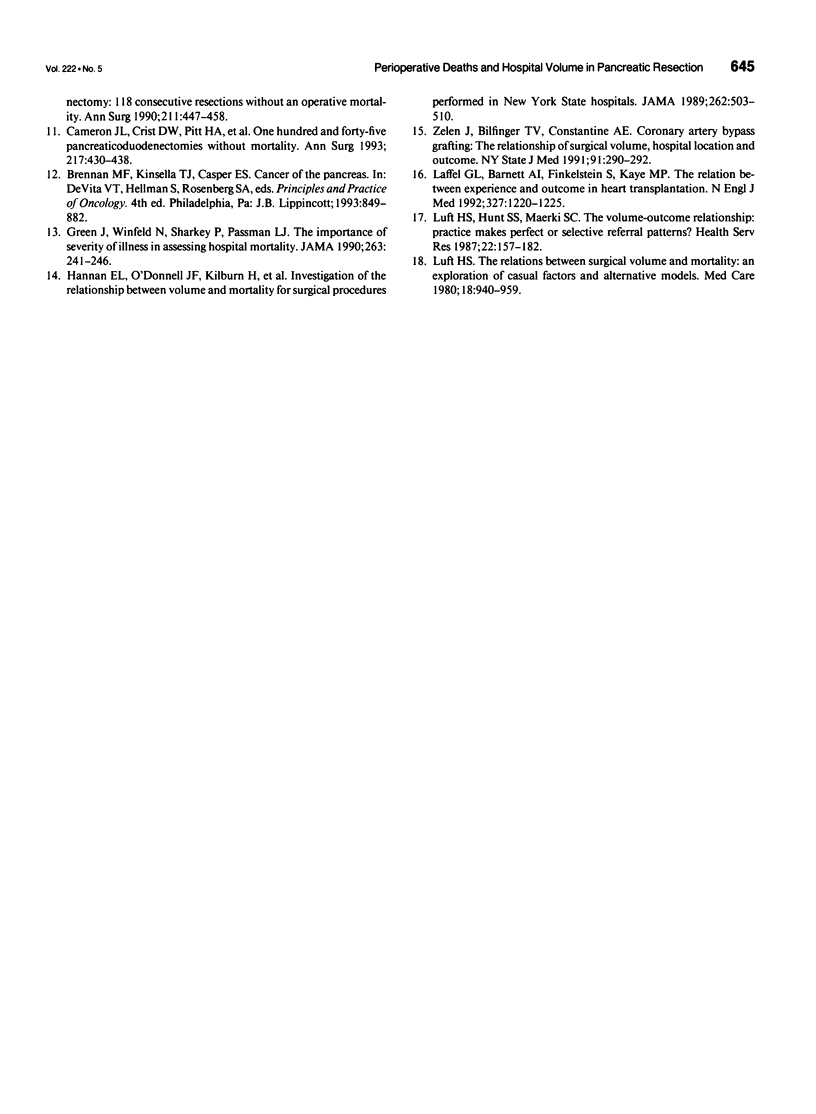
OBJECTIVE: The authors examined the effect of hospital and surgeon volume on perioperative mortality rates after pancreatic resection for the treatment of pancreatic cancer. METHODS: Discharge abstracts from 1972 patients who had undergone pancreaticoduodenectomy or total pancreatectomy for malignancy in New York State between 1984 and 1991 were obtained from the Statewide Planning and Research Cooperative System. Logistic regression analysis was used to determine the relationship between hospital and surgeon experience to perioperative outcome. RESULTS: More than 75% of patients underwent resection at minimal-volume (fewer than 10 cases) or low-volume (10-50 cases) centers (defined as hospitals in which a minimal number of resections were performed in a given year), and these hospitals represented 98% of the institutions treating peripancreatic cancer. The two high-volume hospitals (more than 81 cases) demonstrated a significantly lower perioperative mortality rate (4.0%) compared with the minimal- (21.8%) and low-volume (12.3%) hospitals (p < 0.001). The perioperative mortality rate was 15.5% for low-volume (fewer than 9 cases) surgeons (defined as surgeons who had performed a minimal number of resections in any hospital in a given year) (n = 687) compared with 4.7% for high-volume (more than 41 cases) pancreatic surgeons (n = 4) (p < 0.001). Logistic regression analysis demonstrated that perioperative death is significantly (p < 0.05) related to hospital volume, but the surgeon's experience is not significantly related to perioperative deaths when hospital volume is controlled. CONCLUSIONS: These data support a defined minimum hospital experience for elective pancreatectomy for malignancy to minimize perioperative deaths.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cameron J. L., Pitt H. A., Yeo C. J., Lillemoe K. D., Kaufman H. S., Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993 May;217(5):430–438. doi: 10.1097/00000658-199305010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crist D. W., Sitzmann J. V., Cameron J. L. Improved hospital morbidity, mortality, and survival after the Whipple procedure. Ann Surg. 1987 Sep;206(3):358–365. doi: 10.1097/00000658-198709000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geer R. J., Brennan M. F. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993 Jan;165(1):68–73. doi: 10.1016/s0002-9610(05)80406-4. [DOI] [PubMed] [Google Scholar]
- Gilsdorf R. B., Spanos P. Factors influencing morbidity and mortality in pancreaticoduodenectomy. Ann Surg. 1973 Mar;177(3):332–337. doi: 10.1097/00000658-197303000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace P. A., Pitt H. A., Tompkins R. K., DenBesten L., Longmire W. P., Jr Decreased morbidity and mortality after pancreatoduodenectomy. Am J Surg. 1986 Jan;151(1):141–149. doi: 10.1016/0002-9610(86)90024-3. [DOI] [PubMed] [Google Scholar]
- Green J., Wintfeld N., Sharkey P., Passman L. J. The importance of severity of illness in assessing hospital mortality. JAMA. 1990 Jan 12;263(2):241–246. [PubMed] [Google Scholar]
- Hannan E. L., O'Donnell J. F., Kilburn H., Jr, Bernard H. R., Yazici A. Investigation of the relationship between volume and mortality for surgical procedures performed in New York State hospitals. JAMA. 1989 Jul 28;262(4):503–510. [PubMed] [Google Scholar]
- Laffel G. L., Barnett A. I., Finkelstein S., Kaye M. P. The relation between experience and outcome in heart transplantation. N Engl J Med. 1992 Oct 22;327(17):1220–1225. doi: 10.1056/NEJM199210223271707. [DOI] [PubMed] [Google Scholar]
- Lansing P. B., Blalock J. B., Ochsner J. L. Pancreatoduodenectomy: a retrospective review 1949 to 1969. Am Surg. 1972 Feb;38(2):79–86. [PubMed] [Google Scholar]
- Luft H. S., Hunt S. S., Maerki S. C. The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res. 1987 Jun;22(2):157–182. [PMC free article] [PubMed] [Google Scholar]
- Luft H. S. The relation between surgical volume and mortality: an exploration of causal factors and alternative models. Med Care. 1980 Sep;18(9):940–959. doi: 10.1097/00005650-198009000-00006. [DOI] [PubMed] [Google Scholar]
- Miedema B. W., Sarr M. G., van Heerden J. A., Nagorney D. M., McIlrath D. C., Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992 Aug;127(8):945–950. doi: 10.1001/archsurg.1992.01420080079012. [DOI] [PubMed] [Google Scholar]
- Pellegrini C. A., Heck C. F., Raper S., Way L. W. An analysis of the reduced morbidity and mortality rates after pancreaticoduodenectomy. Arch Surg. 1989 Jul;124(7):778–781. doi: 10.1001/archsurg.1989.01410070028006. [DOI] [PubMed] [Google Scholar]
- Trede M., Schwall G., Saeger H. D. Survival after pancreatoduodenectomy. 118 consecutive resections without an operative mortality. Ann Surg. 1990 Apr;211(4):447–458. doi: 10.1097/00000658-199004000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trede M., Schwall G. The complications of pancreatectomy. Ann Surg. 1988 Jan;207(1):39–47. doi: 10.1097/00000658-198801000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whipple A. O., Parsons W. B., Mullins C. R. TREATMENT OF CARCINOMA OF THE AMPULLA OF VATER. Ann Surg. 1935 Oct;102(4):763–779. doi: 10.1097/00000658-193510000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelen J., Bilfinger T. V., Anagnostopoulos C. E. Coronary artery bypass grafting. The relationship of surgical volume, hospital location, and outcome. N Y State J Med. 1991 Jul;91(7):290–292. [PubMed] [Google Scholar]


