Abstract
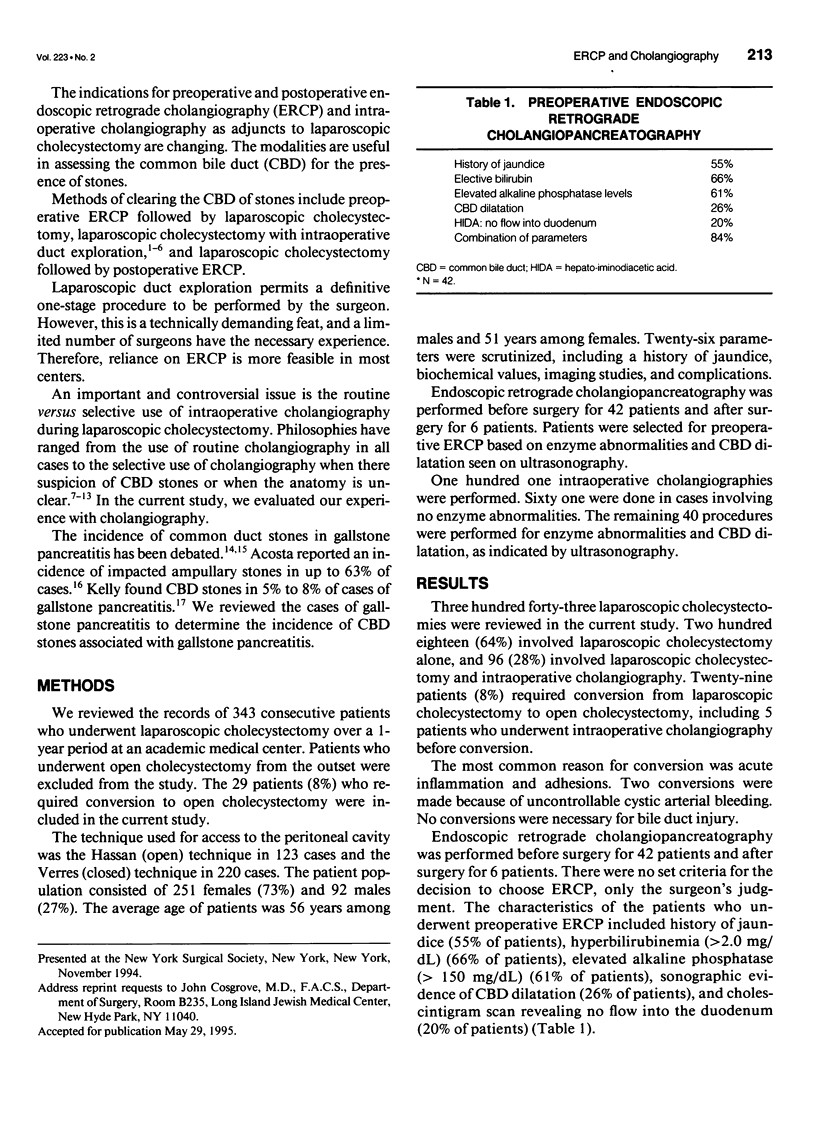
OBJECTIVE: The authors reviewed the results of endoscopic retrograde cholangiopancreatography (ERCP) and intraoperative cholangiography in a series of patients who underwent laparoscopic cholecystectomy. SUMMARY BACKGROUND DATA: The indications for preoperative and postoperative ERCP and intraoperative cholangiography as adjuncts to laparoscopic cholecystectomy are evolving. The debate regarding the use of selective or routine intraoperative cholangiography has intensified with the advent of laparoscopic cholecystectomy. METHODS: The authors reviewed the records of 343 consecutive patients who underwent laparoscopic cholecystectomy during a 1-year period. Historical, biochemical, and radiologic findings for the patients who underwent ERCP and intraoperative cholangiography were analyzed. RESULTS: Three hundred forty- three patients underwent laparoscopic cholecystectomy during the period reviewed. Preoperative ERCP was performed in 42 patients. Twenty-seven of these patients (64%) had common bile duct (CBD) stones, which were cleared with a sphincterotomy. Intraoperative cholangiography was performed for 101 patients (29%). Three cholangiograms had false- positive results (3%), leading to two CBD explorations, in which no CBD stones were found, and one normal ERCP. Six patients underwent postoperative ERCP, three for the removal of retained CBD stones (0.9%), all of which were cleared with a sphincterotomy. Fifteen patients had gallstone pancreatitis, six of whom had CBD stones (40%) that were cleared by ERCP. There were 33 complications (10%) and no CBD injuries. CONCLUSION: The use of routine intraoperative cholangiography is discouraged in view of its low yield and the significant rate of false positive cholangiogram results.
Full text
PDF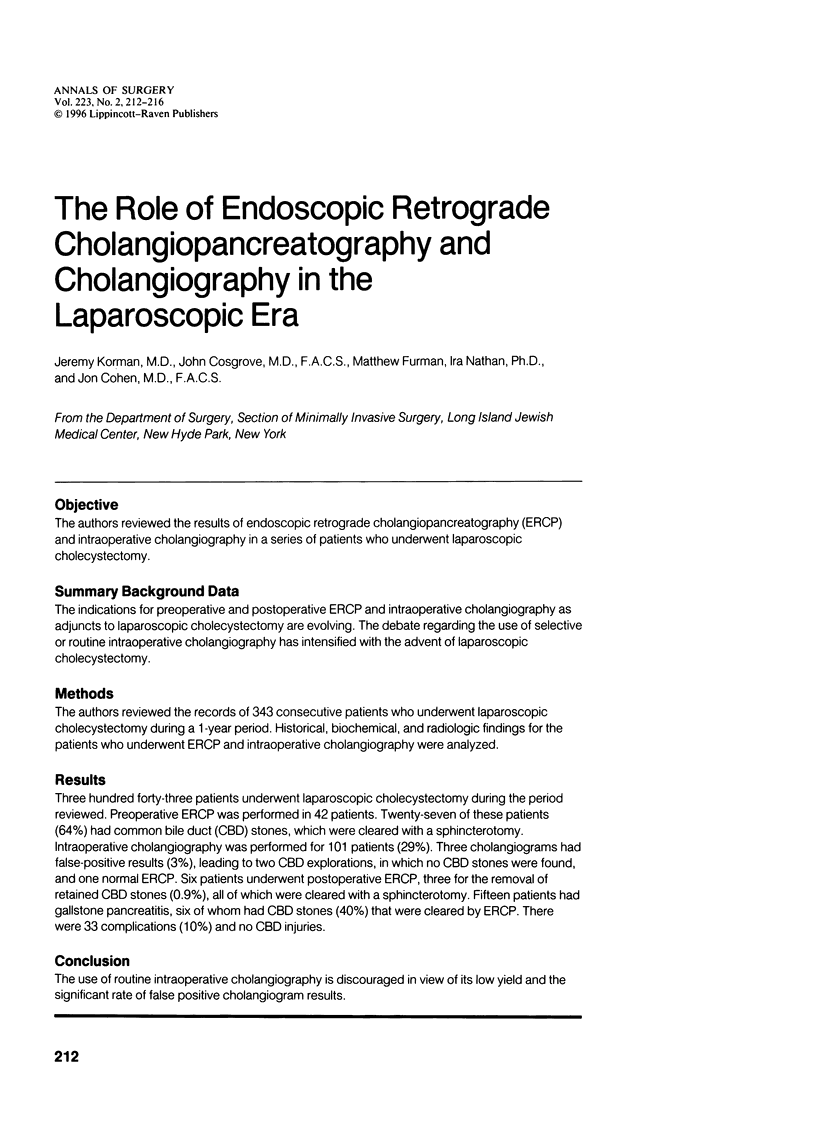


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Acosta J. M., Pellegrini C. A., Skinner D. B. Etiology and pathogenesis of acute biliary pancreatitis. Surgery. 1980 Jul;88(1):118–125. [PubMed] [Google Scholar]
- Arregui M. E., Davis C. J., Arkush A. M., Nagan R. F. Laparoscopic cholecystectomy combined with endoscopic sphincterotomy and stone extraction or laparoscopic choledochoscopy and electrohydraulic lithotripsy for management of cholelithiasis with choledocholithiasis. Surg Endosc. 1992 Jan-Feb;6(1):10–15. doi: 10.1007/BF00591180. [DOI] [PubMed] [Google Scholar]
- Barkun A. N., Barkun J. S., Fried G. M., Ghitulescu G., Steinmetz O., Pham C., Meakins J. L., Goresky C. A. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. McGill Gallstone Treatment Group. Ann Surg. 1994 Jul;220(1):32–39. doi: 10.1097/00000658-199407000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkun J. S., Fried G. M., Barkun A. N., Sigman H. H., Hinchey E. J., Garzon J., Wexler M. J., Meakins J. L. Cholecystectomy without operative cholangiography. Implications for common bile duct injury and retained common bile duct stones. Ann Surg. 1993 Sep;218(3):371–379. doi: 10.1097/00000658-199309000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berci G., Morgenstern L. Laparoscopic management of common bile duct stones. A multi-institutional SAGES study. Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc. 1994 Oct;8(10):1168–1175. doi: 10.1007/BF00591044. [DOI] [PubMed] [Google Scholar]
- Berci G., Sackier J. M., Paz-Partlow M. Routine or selected intraoperative cholangiography during laparoscopic cholecystectomy? Am J Surg. 1991 Mar;161(3):355–360. doi: 10.1016/0002-9610(91)90597-7. [DOI] [PubMed] [Google Scholar]
- Cuschieri A., Shimi S., Banting S., Nathanson L. K., Pietrabissa A. Intraoperative cholangiography during laparoscopic cholecystectomy. Routine vs selective policy. Surg Endosc. 1994 Apr;8(4):302–305. doi: 10.1007/BF00590958. [DOI] [PubMed] [Google Scholar]
- Ferzli G. S., Massaad A., Kiel T., Worth M. H., Jr The utility of laparoscopic common bile duct exploration in the treatment of choledocholithiasis. Surg Endosc. 1994 Apr;8(4):296–298. doi: 10.1007/BF00590956. [DOI] [PubMed] [Google Scholar]
- Gerber A., Apt M. K. The case against routine operative cholangiography. Am J Surg. 1982 Jun;143(6):734–736. doi: 10.1016/0002-9610(82)90048-4. [DOI] [PubMed] [Google Scholar]
- Graham S. M., Flowers J. L., Scott T. R., Bailey R. W., Scovill W. A., Zucker K. A., Imbembo A. L. Laparoscopic cholecystectomy and common bile duct stones. The utility of planned perioperative endoscopic retrograde cholangiography and sphincterotomy: experience with 63 patients. Ann Surg. 1993 Jul;218(1):61–67. doi: 10.1097/00000658-199307000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J. G. Laparoscopic transcystic common bile duct exploration. Am J Surg. 1992 Jan;163(1):53–58. doi: 10.1016/0002-9610(92)90252-m. [DOI] [PubMed] [Google Scholar]
- Kelly T. R. Gallstone pancreatitis: pathophysiology. Surgery. 1976 Oct;80(4):488–492. [PubMed] [Google Scholar]
- Leitman I. M., Fisher M. L., McKinley M. J., Rothman R., Ward R. J., Reiner D. S., Tortolani A. J. The evaluation and management of known or suspected stones of the common bile duct in the era of minimal access surgery. Surg Gynecol Obstet. 1993 Jun;176(6):527–533. [PubMed] [Google Scholar]
- McSherry C. K. Laparoscopic management of common bile duct stones. Surg Endosc. 1994 Oct;8(10):1161–1161. [PubMed] [Google Scholar]
- Pagana T. J., Stahlgren L. H. Indications and accuracy of operative cholangiography. Arch Surg. 1980 Oct;115(10):1214–1215. doi: 10.1001/archsurg.1980.01380100060014. [DOI] [PubMed] [Google Scholar]
- Petelin J. B. Laparoscopic approach to common duct pathology. Am J Surg. 1993 Apr;165(4):487–491. doi: 10.1016/s0002-9610(05)80947-x. [DOI] [PubMed] [Google Scholar]
- Phillips E. H., Rosenthal R. J., Carroll B. J., Fallas M. J. Laparoscopic trans-cystic-duct common-bile-duct exploration. Surg Endosc. 1994 Dec;8(12):1389–1394. doi: 10.1007/BF00187342. [DOI] [PubMed] [Google Scholar]
- Ranson J. H. The timing of biliary surgery in acute pancreatitis. Ann Surg. 1979 May;189(5):654–663. doi: 10.1097/00000658-197905000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sackier J. M., Berci G., Paz-Partlow M. Laparoscopic trancystic choledocholithotomy as an adjunct to laparoscopic cholecystectomy. Am Surg. 1991 May;57(5):323–326. [PubMed] [Google Scholar]
- Salky B., Bauer J. Intravenous cholangiography, ERCP, and selective operative cholangiography in the performance of laparoscopic cholecystectomy. Surg Endosc. 1994 Apr;8(4):289–291. doi: 10.1007/BF00590954. [DOI] [PubMed] [Google Scholar]
- Voyles C. R., Sanders D. L., Hogan R. Common bile duct evaluation in the era of laparoscopic cholecystectomy. 1050 cases later. Ann Surg. 1994 Jun;219(6):744–752. [PMC free article] [PubMed] [Google Scholar]


