Abstract
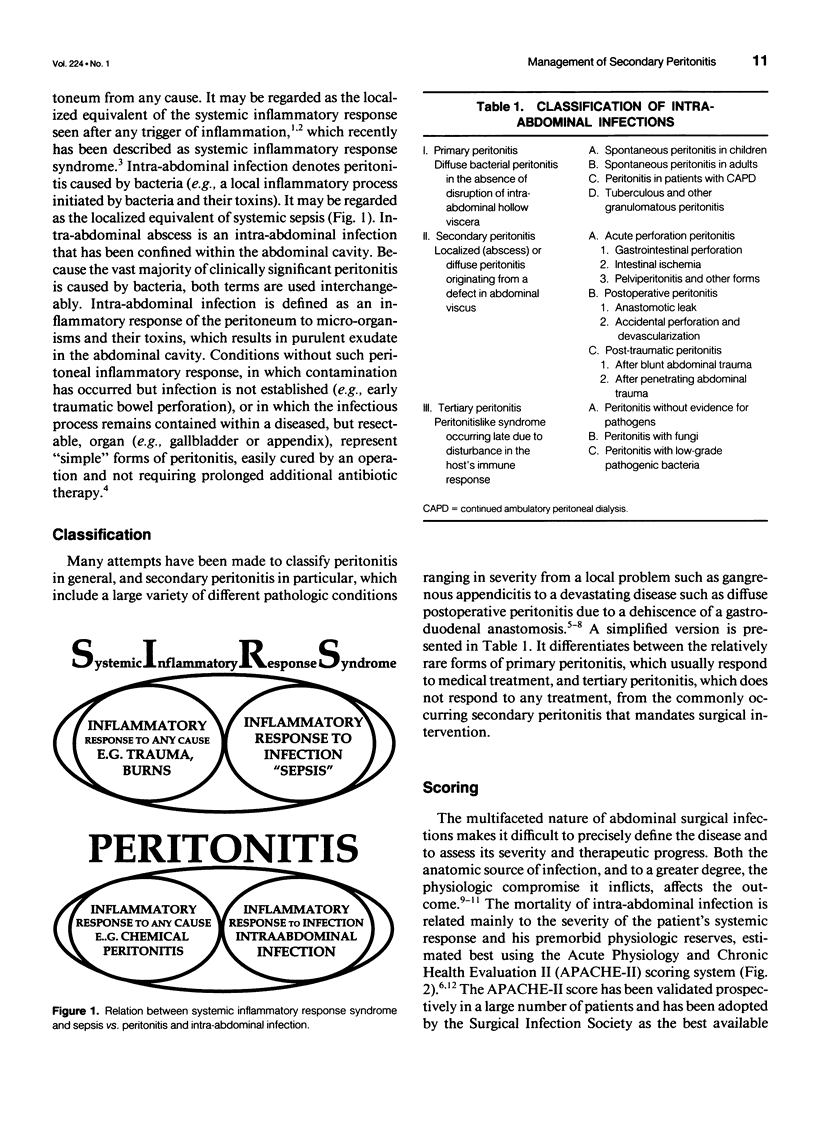
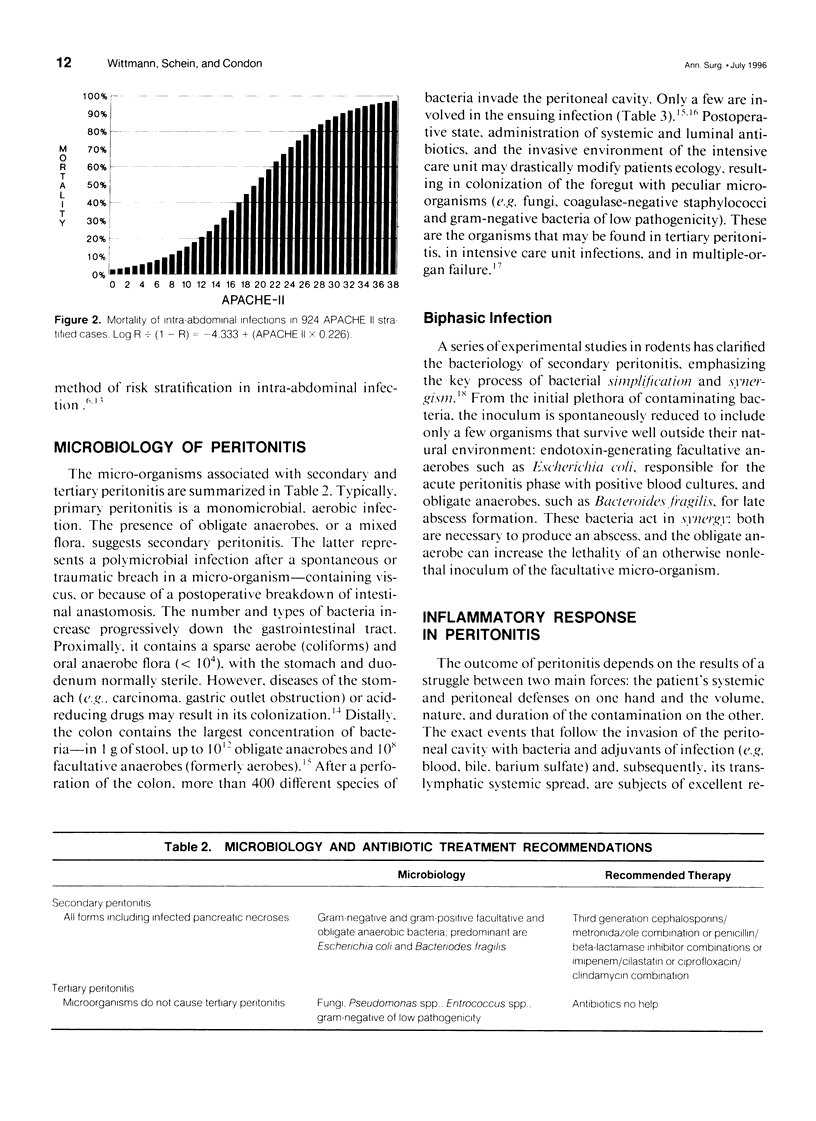
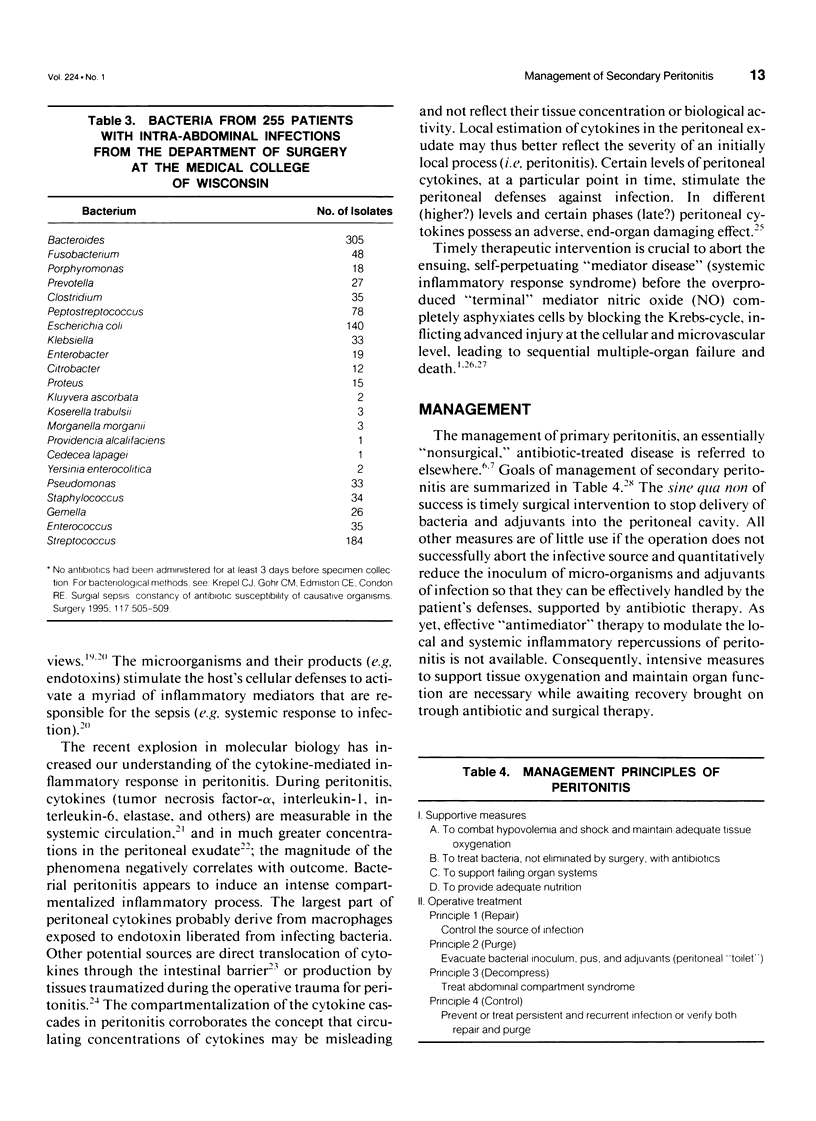
OBJECTIVE. The authors review current definition, classification, scoring, microbiology, inflammatory response, and goals of management of secondary peritonitis. SUMMARY BACKGROUND DATA. Despite improved diagnostic modalities, potent antibiotics, modern intensive care, and aggressive surgical treatment, up to one third of patients still die of severe secondary peritonitis. Against the background of current understanding of the local and systemic inflammatory response associated with peritonitis, there is growing controversy concerning the optimal antibiotic and operative therapy, intensified by lack of properly conducted randomized studies. In this overview the authors attempt to outline controversies, suggest a practical clinical approach, and highlight issues necessitating further research. METHODS. The authors review the literature and report their experience. RESULTS. The emerging concepts concerning antibiotic treatment suggest that less-in terms of the number of drugs and the duration of treatment-is better. The classical single operation for peritonitis, which obliterates the source of infection and purges the peritoneal cavity, may be inadequate for severe forms of peritonitis; for the latter, more aggressive surgical techniques are necessary to decompress increased intra-abdominal pressure and prevent or treat persistent and recurrent infection. The widespread acceptance of the more aggressive and demanding surgical methods has been hampered by the lack of randomized trials and reportedly high associated morbidity rates. CONCLUSIONS. Sepsis represents the host's systemic inflammatory response to bacterial peritonitis. To improve results, both the initiator and the biologic consequences of the peritoneal infective-inflammatory process should be addressed. The initiator may be better controlled in severe forms of peritonitis by aggressive surgical methods, whereas the search for methods to abort its systemic consequences is continuing.
Full text
PDF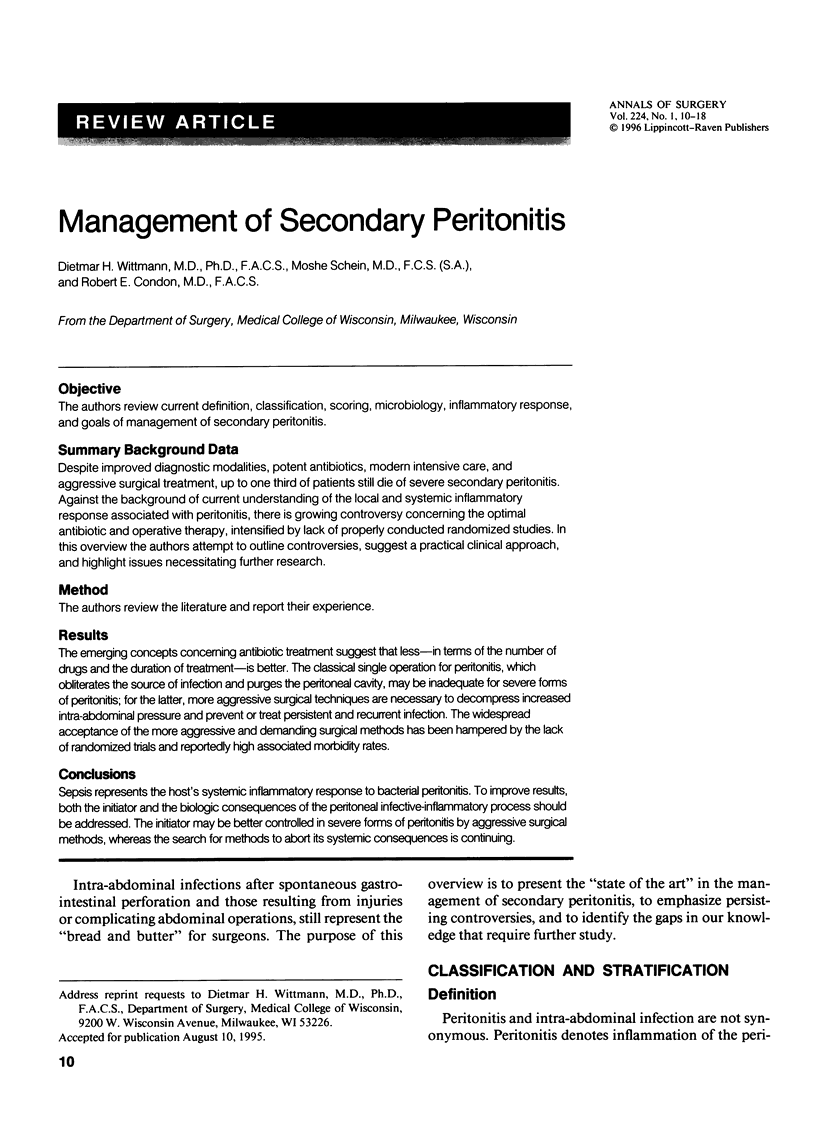


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aprahamian C., Schein M., Wittmann D. Cefotaxime and metronidazole in severe intra-abdominal infection. Diagn Microbiol Infect Dis. 1995 May-Jun;22(1-2):183–188. doi: 10.1016/0732-8893(95)00104-i. [DOI] [PubMed] [Google Scholar]
- Baigrie R. J., Lamont P. M., Kwiatkowski D., Dallman M. J., Morris P. J. Systemic cytokine response after major surgery. Br J Surg. 1992 Aug;79(8):757–760. doi: 10.1002/bjs.1800790813. [DOI] [PubMed] [Google Scholar]
- Barendregt W. B., de Boer H. H., Kubat K. The results of autopsy of patients with surgical diseases of the digestive tract. Surg Gynecol Obstet. 1992 Sep;175(3):227–232. [PubMed] [Google Scholar]
- Bartlett J. G., Onderdonk A. B., Louie T., Kasper D. L., Gorbach S. L. A review. Lessons from an animal model of intra-abdominal sepsis. Arch Surg. 1978 Jul;113(7):853–857. doi: 10.1001/archsurg.1978.01370190075013. [DOI] [PubMed] [Google Scholar]
- Bentley D. W., Nichols R. L., Condon R. E., Gorbach S. L. The microflora of the human ileum and intrabdominal colon: results of direct needle aspiration at surgery and evaluation of the technique. J Lab Clin Med. 1972 Mar;79(3):421–429. [PubMed] [Google Scholar]
- Bohnen J. M., Mustard R. A. A critical look at scheduled relaparotomy for secondary bacterial peritonitis. Surg Gynecol Obstet. 1991;172 (Suppl):25–29. [PubMed] [Google Scholar]
- Bohnen J. M., Solomkin J. S., Dellinger E. P., Bjornson H. S., Page C. P. Guidelines for clinical care: anti-infective agents for intra-abdominal infection. A Surgical Infection Society policy statement. Arch Surg. 1992 Jan;127(1):83–89. doi: 10.1001/archsurg.1992.01420010097015. [DOI] [PubMed] [Google Scholar]
- Bohnen J., Boulanger M., Meakins J. L., McLean A. P. Prognosis in generalized peritonitis. Relation to cause and risk factors. Arch Surg. 1983 Mar;118(3):285–290. doi: 10.1001/archsurg.1983.01390030017003. [DOI] [PubMed] [Google Scholar]
- Christou N. V., Barie P. S., Dellinger E. P., Waymack J. P., Stone H. H. Surgical Infection Society intra-abdominal infection study. Prospective evaluation of management techniques and outcome. Arch Surg. 1993 Feb;128(2):193–199. doi: 10.1001/archsurg.1993.01420140070011. [DOI] [PubMed] [Google Scholar]
- Condon R. E., Wittmann D. H. The use of antibiotics in general surgery. Curr Probl Surg. 1991 Dec;28(12):801–949. doi: 10.1016/0011-3840(91)90004-9. [DOI] [PubMed] [Google Scholar]
- Deitch E. A. Cytokines yes, cytokines no, cytokines maybe? Crit Care Med. 1993 Jun;21(6):817–819. doi: 10.1097/00003246-199306000-00003. [DOI] [PubMed] [Google Scholar]
- Dellinger E. P., Wertz M. J., Meakins J. L., Solomkin J. S., Allo M. D., Howard R. J., Simmons R. L. Surgical infection stratification system for intra-abdominal infection. Multicenter trial. Arch Surg. 1985 Jan;120(1):21–29. doi: 10.1001/archsurg.1985.01390250015003. [DOI] [PubMed] [Google Scholar]
- Edmiston C. E., Jr, Goheen M. P., Kornhall S., Jones F. E., Condon R. E. Fecal peritonitis: microbial adherence to serosal mesothelium and resistance to peritoneal lavage. World J Surg. 1990 Mar-Apr;14(2):176–183. doi: 10.1007/BF01664870. [DOI] [PubMed] [Google Scholar]
- Farthmann E. H., Schöffel U. Principles and limitations of operative management of intraabdominal infections. World J Surg. 1990 Mar-Apr;14(2):210–217. doi: 10.1007/BF01664875. [DOI] [PubMed] [Google Scholar]
- Garcia-Sabrido J. L., Tallado J. M., Christou N. V., Polo J. R., Valdecantos E. Treatment of severe intra-abdominal sepsis and/or necrotic foci by an 'open-abdomen' approach. Zipper and zipper-mesh techniques. Arch Surg. 1988 Feb;123(2):152–156. doi: 10.1001/archsurg.1988.01400260032002. [DOI] [PubMed] [Google Scholar]
- Gorbach S. L. Intraabdominal infections. Clin Infect Dis. 1993 Dec;17(6):961–965. doi: 10.1093/clinids/17.6.961. [DOI] [PubMed] [Google Scholar]
- Goris R. J., te Boekhorst T. P., Nuytinck J. K., Gimbrère J. S. Multiple-organ failure. Generalized autodestructive inflammation? Arch Surg. 1985 Oct;120(10):1109–1115. doi: 10.1001/archsurg.1985.01390340007001. [DOI] [PubMed] [Google Scholar]
- Hadjiminas D., Cheadle W. G., Spain D. A., Wilson M. A., Short A., Starko K. M., Harris B. J., Livingston D. H., Rodriguez J. L. Antibiotic overkill of trauma victims? Am J Surg. 1994 Sep;168(3):288–290. doi: 10.1016/s0002-9610(05)80205-3. [DOI] [PubMed] [Google Scholar]
- Holzheimer R. G., Schein M., Wittmann D. H. Inflammatory response in peritoneal exudate and plasma of patients undergoing planned relaparotomy for severe secondary peritonitis. Arch Surg. 1995 Dec;130(12):1314–1320. doi: 10.1001/archsurg.1995.01430120068010. [DOI] [PubMed] [Google Scholar]
- Hopkins J. A., Wilson S. E., Bobey D. G. Adjunctive antimicrobial therapy for complicated appendicitis: bacterial overkill by combination therapy. World J Surg. 1994 Nov-Dec;18(6):933–938. doi: 10.1007/BF00299113. [DOI] [PubMed] [Google Scholar]
- Ivatury R. R., Nallathambi M., Rao P. M., Rohman M., Stahl W. M. Open management of the septic abdomen: therapeutic and prognostic considerations based on APACHE II. Crit Care Med. 1989 Jun;17(6):511–517. doi: 10.1097/00003246-198906000-00005. [DOI] [PubMed] [Google Scholar]
- Kinney E. V., Polk H. C., Jr Open treatment of peritonitis: an argument against. Adv Surg. 1988;21:19–27. [PubMed] [Google Scholar]
- Knaus W. A., Draper E. A., Wagner D. P., Zimmerman J. E. APACHE II: a severity of disease classification system. Crit Care Med. 1985 Oct;13(10):818–829. [PubMed] [Google Scholar]
- Krepel C. J., Gohr C. M., Edmiston C. E., Condon R. E. Surgical sepsis: constancy of antibiotic susceptibility of causative organisms. Surgery. 1995 May;117(5):505–509. doi: 10.1016/s0039-6060(05)80249-1. [DOI] [PubMed] [Google Scholar]
- Lancaster J. R., Jr, Hibbs J. B., Jr EPR demonstration of iron-nitrosyl complex formation by cytotoxic activated macrophages. Proc Natl Acad Sci U S A. 1990 Feb;87(3):1223–1227. doi: 10.1073/pnas.87.3.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiboff A. R., Soroff H. S. The treatment of generalized peritonitis by closed postoperative peritoneal lavage. A critical review of the literature. Arch Surg. 1987 Sep;122(9):1005–1010. doi: 10.1001/archsurg.1987.01400210043006. [DOI] [PubMed] [Google Scholar]
- Lennard E. S., Dellinger E. P., Wertz M. J., Minshew B. H. Implications of leukocytosis and fever at conclusion of antibiotic therapy for intra-abdominal sepsis. Ann Surg. 1982 Jan;195(1):19–24. doi: 10.1097/00000658-198201001-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levison M. A., Zeigler D. Correlation of APACHE II score, drainage technique and outcome in postoperative intra-abdominal abscess. Surg Gynecol Obstet. 1991 Feb;172(2):89–94. [PubMed] [Google Scholar]
- Lévy E., Palmer D. L., Frileux P., Hannoun L., Nordlinger B., Tiret E., Honiger J., Parc R. Septic necrosis of the midline wound in postoperative peritonitis. Successful management by debridement, myocutaneous advancement, and primary skin closure. Ann Surg. 1988 Apr;207(4):470–479. doi: 10.1097/00000658-198804000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddaus M. A., Ahrenholz D., Simmons R. L. The biology of peritonitis and implications for treatment. Surg Clin North Am. 1988 Apr;68(2):431–443. doi: 10.1016/s0039-6109(16)44487-7. [DOI] [PubMed] [Google Scholar]
- Marshall J. C., Christou N. V., Meakins J. L. The gastrointestinal tract. The "undrained abscess" of multiple organ failure. Ann Surg. 1993 Aug;218(2):111–119. doi: 10.1097/00000658-199308000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J., Sweeney D. Microbial infection and the septic response in critical surgical illness. Sepsis, not infection, determines outcome. Arch Surg. 1990 Jan;125(1):17–23. doi: 10.1001/archsurg.1990.01410130019002. [DOI] [PubMed] [Google Scholar]
- Meakins J. L., Solomkin J. S., Allo M. D., Dellinger E. P., Howard R. J., Simmons R. L. A proposed classification of intra-abdominal infections. Stratification of etiology and risk for future therapeutic trials. Arch Surg. 1984 Dec;119(12):1372–1378. doi: 10.1001/archsurg.1984.01390240010002. [DOI] [PubMed] [Google Scholar]
- Mock C. N., Jurkovich G. J., Dries D. J., Maier R. V. Clinical significance of antibiotic endotoxin-releasing properties in trauma patients. Arch Surg. 1995 Nov;130(11):1234–1241. doi: 10.1001/archsurg.1995.01430110092017. [DOI] [PubMed] [Google Scholar]
- Mosdell D. M., Morris D. M., Fry D. E. Peritoneal cultures and antibiotic therapy in pediatric perforated appendicitis. Am J Surg. 1994 Mar;167(3):313–316. doi: 10.1016/0002-9610(94)90207-0. [DOI] [PubMed] [Google Scholar]
- Mosdell D. M., Morris D. M., Voltura A., Pitcher D. E., Twiest M. W., Milne R. L., Miscall B. G., Fry D. E. Antibiotic treatment for surgical peritonitis. Ann Surg. 1991 Nov;214(5):543–549. doi: 10.1097/00000658-199111000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton L. W. Does drainage of intraabdominal pus reverse multiple organ failure? Am J Surg. 1985 Mar;149(3):347–350. doi: 10.1016/s0002-9610(85)80105-7. [DOI] [PubMed] [Google Scholar]
- Nyström P. O., Bax R., Dellinger E. P., Dominioni L., Knaus W. A., Meakins J. L., Ohmann C., Solomkin J. S., Wacha H., Wittmann D. H. Proposed definitions for diagnosis, severity scoring, stratification, and outcome for trials on intraabdominal infection. Joint Working Party of SIS North America and Europe. World J Surg. 1990 Mar-Apr;14(2):148–158. doi: 10.1007/BF01664867. [DOI] [PubMed] [Google Scholar]
- Palmer R. M. The discovery of nitric oxide in the vessel wall. A unifying concept in the pathogenesis of sepsis. Arch Surg. 1993 Apr;128(4):396–401. doi: 10.1001/archsurg.1993.01420160034004. [DOI] [PubMed] [Google Scholar]
- Parrillo J. E. Pathogenetic mechanisms of septic shock. N Engl J Med. 1993 May 20;328(20):1471–1477. doi: 10.1056/NEJM199305203282008. [DOI] [PubMed] [Google Scholar]
- Patel R. T., Deen K. I., Youngs D., Warwick J., Keighley M. R. Interleukin 6 is a prognostic indicator of outcome in severe intra-abdominal sepsis. Br J Surg. 1994 Sep;81(9):1306–1308. doi: 10.1002/bjs.1800810914. [DOI] [PubMed] [Google Scholar]
- Polk H. C., Jr, Fry D. E. Radical peritoneal debridement for established peritonitis. The results of a prospective randomized clinical trial. Ann Surg. 1980 Sep;192(3):350–355. doi: 10.1097/00000658-198009000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins J. M., van Deventer S. J., Kuijper E. J., Speelman P. Clinical relevance of antibiotic-induced endotoxin release. Antimicrob Agents Chemother. 1994 Jun;38(6):1211–1218. doi: 10.1128/aac.38.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotstein O. D., Meakins J. L. Diagnostic and therapeutic challenges of intraabdominal infections. World J Surg. 1990 Mar-Apr;14(2):159–166. doi: 10.1007/BF01664868. [DOI] [PubMed] [Google Scholar]
- Schein C. H., Haugg M. Deletions at the C-terminus of interferon gamma reduce RNA binding and activation of double-stranded-RNA cleavage by bovine seminal ribonuclease. Biochem J. 1995 Apr 1;307(Pt 1):123–127. doi: 10.1042/bj3070123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schein M., Assalia A., Bachus H. Minimal antibiotic therapy after emergency abdominal surgery: a prospective study. Br J Surg. 1994 Jul;81(7):989–991. doi: 10.1002/bjs.1800810720. [DOI] [PubMed] [Google Scholar]
- Schein M., Gecelter G., Freinkel W., Gerding H., Becker P. J. Peritoneal lavage in abdominal sepsis. A controlled clinical study. Arch Surg. 1990 Sep;125(9):1132–1135. doi: 10.1001/archsurg.1990.01410210058008. [DOI] [PubMed] [Google Scholar]
- Schein M. Management of severe intra-abdominal infection. Surg Annu. 1992;24(Pt 1):47–68. [PubMed] [Google Scholar]
- Schein M. Planned reoperations and open management in critical intra-abdominal infections: prospective experience in 52 cases. World J Surg. 1991 Jul-Aug;15(4):537–545. doi: 10.1007/BF01675658. [DOI] [PubMed] [Google Scholar]
- Schein M., Saadia R., Decker G. G. The open management of the septic abdomen. Surg Gynecol Obstet. 1986 Dec;163(6):587–592. [PubMed] [Google Scholar]
- Schein M., Saadia R., Decker G. Intraoperative peritoneal lavage. Surg Gynecol Obstet. 1988 Feb;166(2):187–195. [PubMed] [Google Scholar]
- Schein M., Wittmann D. H., Aprahamian C. C., Condon R. E. The abdominal compartment syndrome: the physiological and clinical consequences of elevated intra-abdominal pressure. J Am Coll Surg. 1995 Jun;180(6):745–753. [PubMed] [Google Scholar]
- Simmen H. P., Battaglia H., Kossmann T., Blaser J. Effect of peritoneal fluid pH on outcome of aminoglycoside treatment of intraabdominal infections. World J Surg. 1993 May-Jun;17(3):393–397. doi: 10.1007/BF01658708. [DOI] [PubMed] [Google Scholar]
- Solomkin J. S., Dellinger E. P., Christou N. V., Busuttil R. W. Results of a multicenter trial comparing imipenem/cilastatin to tobramycin/clindamycin for intra-abdominal infections. Ann Surg. 1990 Nov;212(5):581–591. doi: 10.1097/00000658-199011000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomkin J. S., Meakins J. L., Jr, Allo M. D., Dellinger E. P., Simmons R. L. Antibiotic trials in intra-abdominal infections. A critical evaluation of study design and outcome reporting. Ann Surg. 1984 Jul;200(1):29–39. doi: 10.1097/00000658-198407000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg D. On leaving the peritoneal cavity open in acute generalized suppurative peritonitis. Am J Surg. 1979 Feb;137(2):216–220. doi: 10.1016/0002-9610(79)90148-x. [DOI] [PubMed] [Google Scholar]
- Stone H. H., Strom P. R., Fabian T. C., Dunlop W. E. Third-generation cephalosporins for polymicrobial surgical sepsis. Arch Surg. 1983 Feb;118(2):193–200. doi: 10.1001/archsurg.1983.01390020047009. [DOI] [PubMed] [Google Scholar]
- Teichmann W., Wittmann D. H., Andreone P. A. Scheduled reoperations (etappenlavage) for diffuse peritonitis. Arch Surg. 1986 Feb;121(2):147–152. doi: 10.1001/archsurg.1986.01400020033002. [DOI] [PubMed] [Google Scholar]
- Wittman D. H., Schassan H. H. Penetration of eight beta-lactam antibiotics into the peritoneal fluid. A pharmacokinetic investigation. Arch Surg. 1983 Feb;118(2):205–213. doi: 10.1001/archsurg.1983.01390020055010. [DOI] [PubMed] [Google Scholar]
- Wittmann D. H., Aprahamian C., Bergstein J. M. Etappenlavage: advanced diffuse peritonitis managed by planned multiple laparotomies utilizing zippers, slide fastener, and Velcro analogue for temporary abdominal closure. World J Surg. 1990 Mar-Apr;14(2):218–226. doi: 10.1007/BF01664876. [DOI] [PubMed] [Google Scholar]
- Wittmann D. H. Intraabdominal infections--introduction. World J Surg. 1990 Mar-Apr;14(2):145–147. doi: 10.1007/BF01664866. [DOI] [PubMed] [Google Scholar]


