Abstract
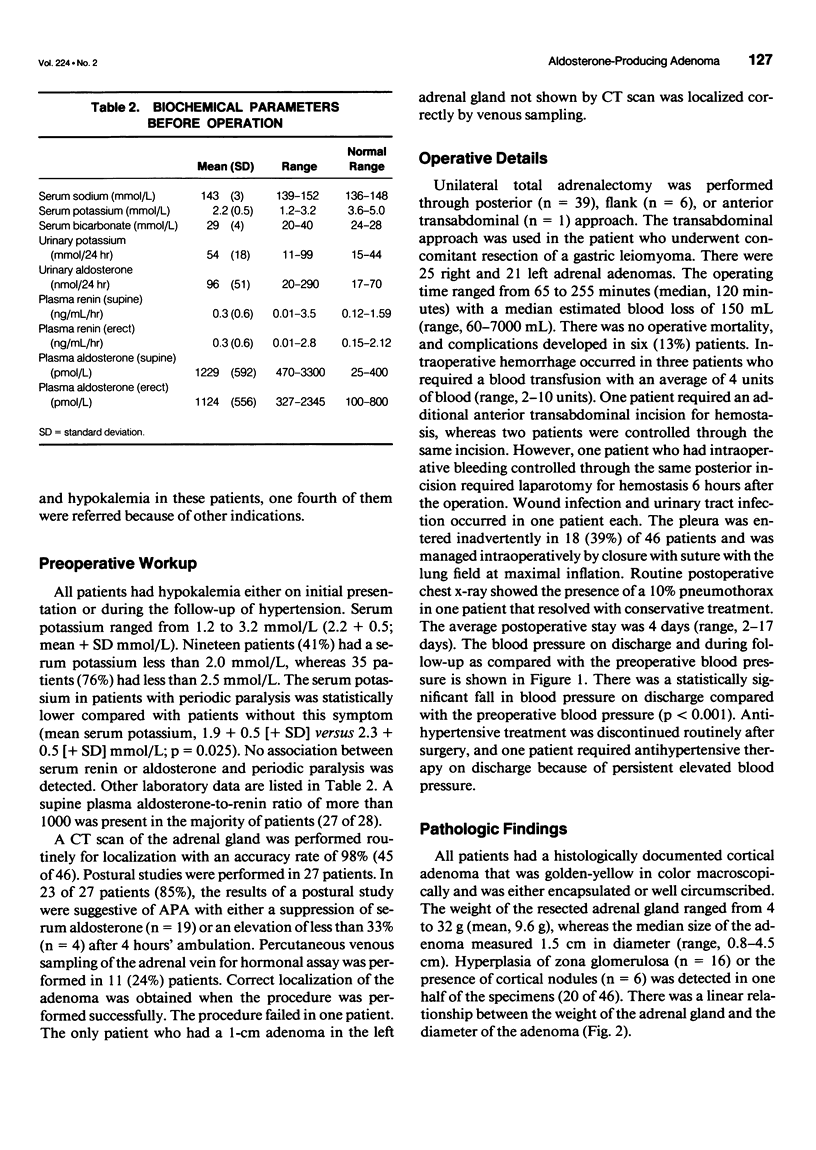
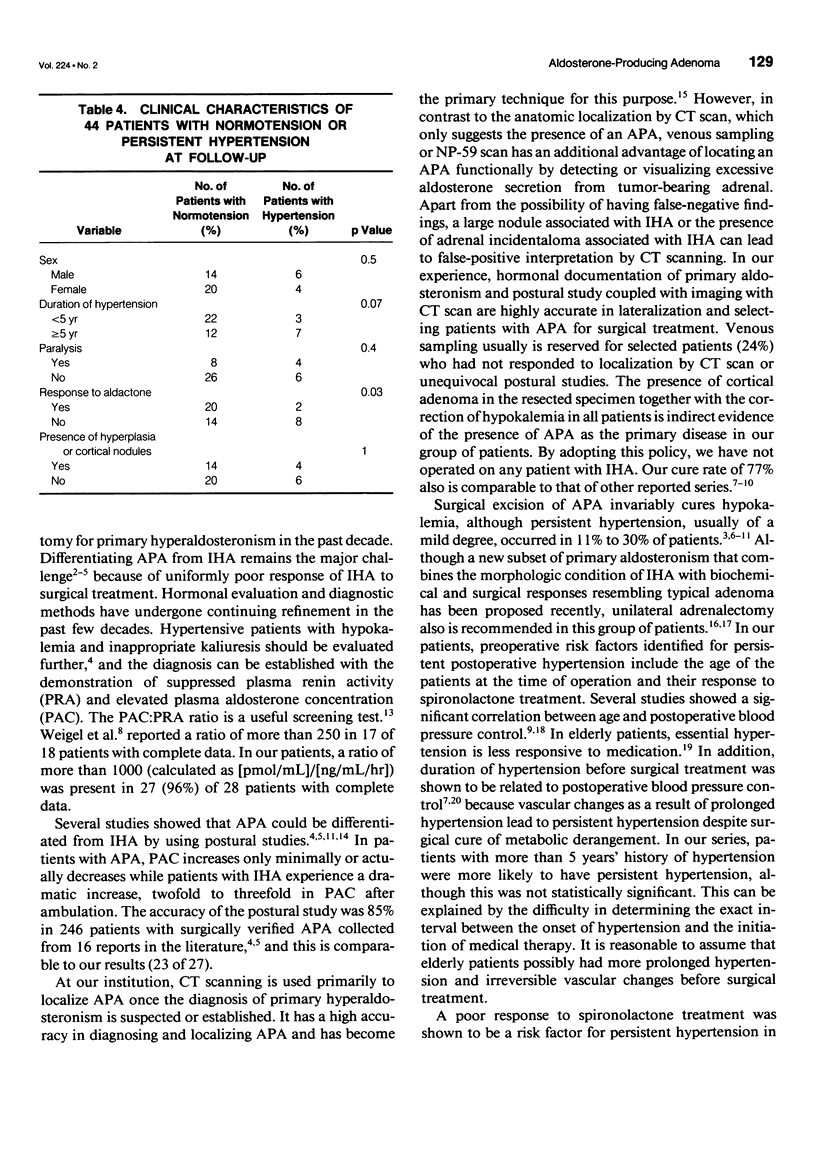
SUMMARY BACKGROUND DATA: Management of primary hyperaldosteronism has undergone dramatic changes in the past 40 years. This retrospective study was carried out to review our recent surgical experience and to identify potential factors associated with postoperative persistent hypertension. METHODS: Forty-six patients who had adrenal surgery for primary hyperaldosteronism from 1983 to 1994 were included in the study. RESULTS: Periodic paralysis occurred in 12 (26%) patients. Hypertension and hypokalemia (mean serum potassium, 2.2 + 0.5 [+ standard deviation (SD) mmol/L) were present in all patients. Postural study was diagnostic in 85% (23 of 27). Computed tomography scan correctly localized the tumor in all except 1 patient, and venous sampling was performed in 11 patients. There was no operative mortality, and complications developed in six patients (13%), including one patient requiring re-exploration for hemostasis. All patients had a histologically documented adenoma. During a mean follow-up of 51 months, 34 (77%) of the 44 patients required no further antihypertensive treatment. Two patients were lost to follow-up. Age, response to spironolactone treatment, and blood pressure on discharge were risk factors identified for persistent hypertension. CONCLUSION: Primary hyperaldosteronism due to aldosterone-producing adenoma can be diagnosed and localized expeditiously, whereas surgical treatment can be performed safely. Hypokalemia may be cured by surgical treatment, although persistent hypertension, usually of a mild degree, still occurs in selected patients.
Full text
PDF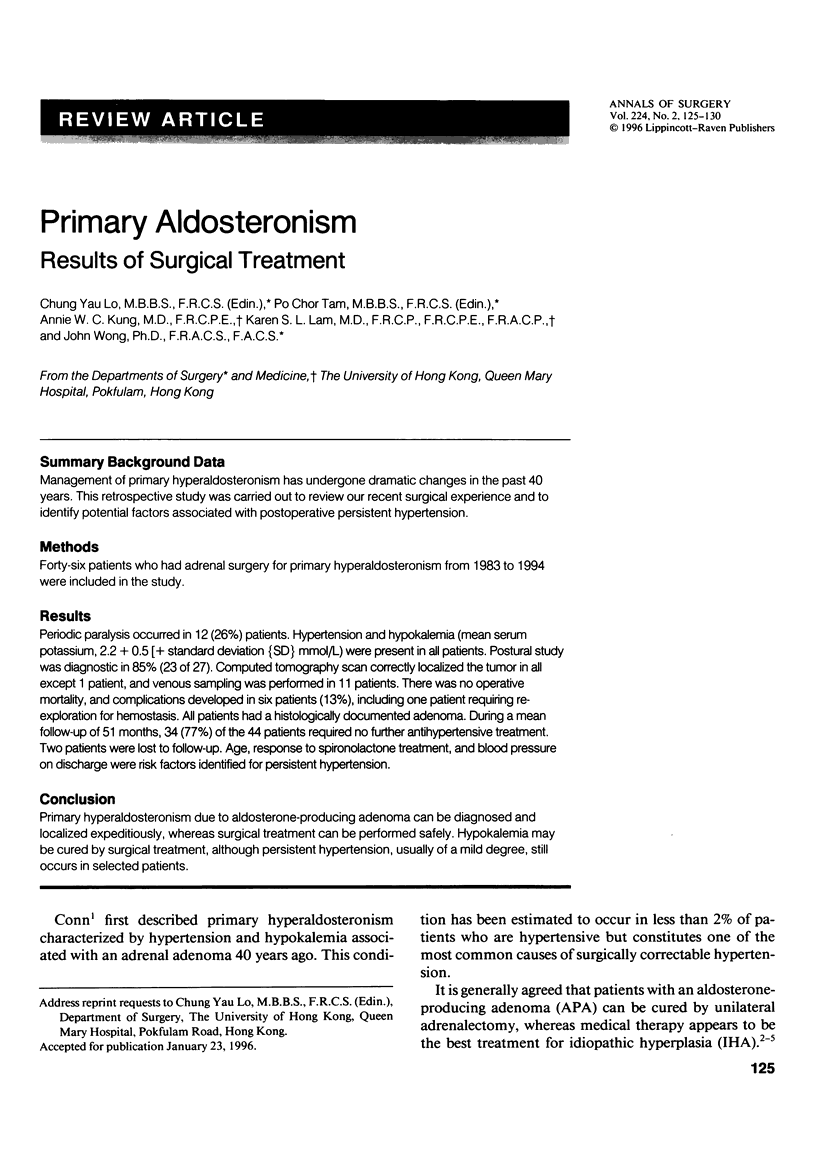


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amery A., Birkenhäger W., Brixko R., Bulpitt C., Clement D., Deruyttere M., De Schaepdryver A., Dollery C., Fagard R., Forette F. Efficacy of antihypertensive drug treatment according to age, sex, blood pressure, and previous cardiovascular disease in patients over the age of 60. Lancet. 1986 Sep 13;2(8507):589–592. doi: 10.1016/s0140-6736(86)92424-4. [DOI] [PubMed] [Google Scholar]
- Auda S. P., Brennan M. F., Gill J. R., Jr Evolution of the surgical management of primary aldosteronism. Ann Surg. 1980 Jan;191(1):1–7. doi: 10.1097/00000658-198001000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CONN J. W. Presidential address. I. Painting background. II. Primary aldosteronism, a new clinical syndrome. J Lab Clin Med. 1955 Jan;45(1):3–17. [PubMed] [Google Scholar]
- Dye N. V., Litton N. J., Varma M., Isley W. L. Unilateral adrenal hyperplasia as a cause of primary aldosteronism. South Med J. 1989 Jan;82(1):82–86. doi: 10.1097/00007611-198901000-00021. [DOI] [PubMed] [Google Scholar]
- Ganguly A., Melada G. A., Luetscher J. A., Dowdy A. J. Control of plasma aldosterone in primary aldosteronism: distinction between adenoma and hyperplasia. J Clin Endocrinol Metab. 1973 Nov;37(5):765–775. doi: 10.1210/jcem-37-5-765. [DOI] [PubMed] [Google Scholar]
- Grant C. S., Carpenter P., van Heerden J. A., Hamberger B. Primary aldosteronism. Clinical management. Arch Surg. 1984 May;119(5):585–590. doi: 10.1001/archsurg.1984.01390170081016. [DOI] [PubMed] [Google Scholar]
- Groth H., Vetter W., Stimpel M., Greminger P., Tenschert W., Klaiber E., Vetter H. Adrenalectomy in primary aldosteronism: a long-term follow-up study. Cardiology. 1985;72 (Suppl 1):107–116. doi: 10.1159/000173955. [DOI] [PubMed] [Google Scholar]
- Herf S. M., Teates D. C., Tegtmeyer C. J., Vaughan E. D., Jr, Ayers C. R., Carey R. M. Identification and differentiation of surgically correctable hypertension due to primary aldosteronism. Am J Med. 1979 Sep;67(3):397–402. doi: 10.1016/0002-9343(79)90785-x. [DOI] [PubMed] [Google Scholar]
- Hiramatsu K., Yamada T., Yukimura Y., Komiya I., Ichikawa K., Ishihara M., Nagata H., Izumiyama T. A screening test to identify aldosterone-producing adenoma by measuring plasma renin activity. Results in hypertensive patients. Arch Intern Med. 1981 Nov;141(12):1589–1593. [PubMed] [Google Scholar]
- Ito Y., Fujimoto Y., Obara T., Kodama T. Clinical significance of associated nodular lesions of the adrenal in patients with aldosteronoma. World J Surg. 1990 May-Jun;14(3):330–334. doi: 10.1007/BF01658518. [DOI] [PubMed] [Google Scholar]
- Lim R. C., Jr, Nakayama D. K., Biglieri E. G., Schambelan M., Hunt T. K. Primary aldosteronism: changing concepts in diagnosis and management. Am J Surg. 1986 Jul;152(1):116–121. doi: 10.1016/0002-9610(86)90160-1. [DOI] [PubMed] [Google Scholar]
- Ma J. T., Wang C., Lam K. S., Yeung R. T., Chan F. L., Boey J., Cheung P. S., Coghlan J. P., Scoggins B. A., Stockigt J. R. Fifty cases of primary hyperaldosteronism in Hong Kong Chinese with a high frequency of periodic paralysis. Evaluation of techniques for tumour localisation. Q J Med. 1986 Nov;61(235):1021–1037. [PubMed] [Google Scholar]
- McLeod M. K., Thompson N. W., Gross M. D., Grekin R. J. Idiopathic aldosteronism masquerading as discrete aldosterone-secreting adrenal cortical neoplasms among patients with primary aldosteronism. Surgery. 1989 Dec;106(6):1161–1168. [PubMed] [Google Scholar]
- Merrell R. C. Aldosterone-producing tumors (Conn's syndrome). Semin Surg Oncol. 1990;6(2):66–70. doi: 10.1002/ssu.2980060203. [DOI] [PubMed] [Google Scholar]
- Obara T., Ito Y., Okamoto T., Kanaji Y., Yamashita T., Aiba M., Fujimoto Y. Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery. 1992 Dec;112(6):987–993. [PubMed] [Google Scholar]
- Simon D., Goretzki P. E., Lollert A., Röher H. D. Persistent hypertension after successful adrenal operation. Surgery. 1993 Dec;114(6):1189–1195. [PubMed] [Google Scholar]
- Streeten D. H., Anderson G. H., Jr, Wagner S. Effect of age on response of secondary hypertension to specific treatment. Am J Hypertens. 1990 May;3(5 Pt 1):360–365. doi: 10.1093/ajh/3.5.360. [DOI] [PubMed] [Google Scholar]
- Takeda M., Go H., Imai T., Nishiyama T., Morishita H. Laparoscopic adrenalectomy for primary aldosteronism: report of initial ten cases. Surgery. 1994 May;115(5):621–625. [PubMed] [Google Scholar]
- Weigel R. J., Wells S. A., Gunnells J. C., Leight G. S. Surgical treatment of primary hyperaldosteronism. Ann Surg. 1994 Apr;219(4):347–352. doi: 10.1097/00000658-199404000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White E. A., Schambelan M., Rost C. R., Biglieri E. G., Moss A. A., Korobkin M. Use of computed tomography in diagnosing the cause of primary aldosteronism. N Engl J Med. 1980 Dec 25;303(26):1503–1507. doi: 10.1056/NEJM198012253032603. [DOI] [PubMed] [Google Scholar]
- Young W. F., Jr, Hogan M. J., Klee G. G., Grant C. S., van Heerden J. A. Primary aldosteronism: diagnosis and treatment. Mayo Clin Proc. 1990 Jan;65(1):96–110. doi: 10.1016/s0025-6196(12)62114-4. [DOI] [PubMed] [Google Scholar]
- Young W. F., Jr, Klee G. G. Primary aldosteronism. Diagnostic evaluation. Endocrinol Metab Clin North Am. 1988 Jun;17(2):367–395. [PubMed] [Google Scholar]



