Abstract
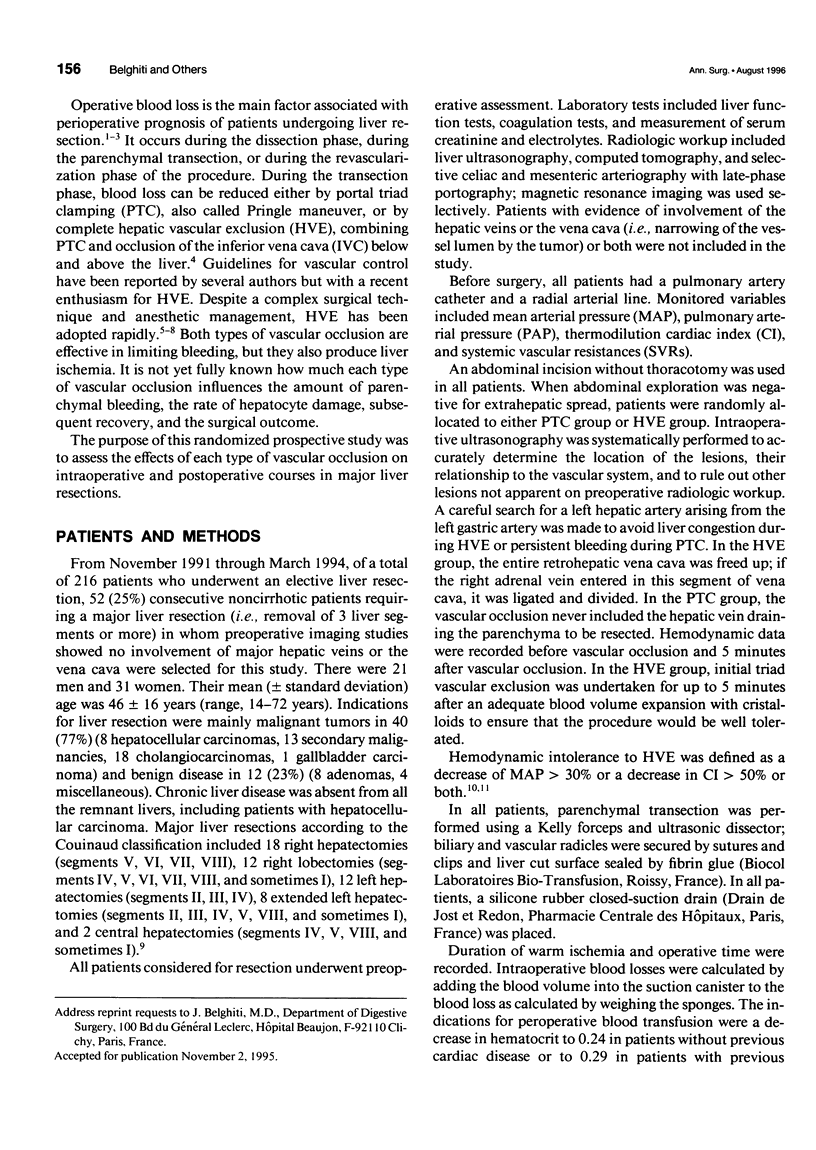
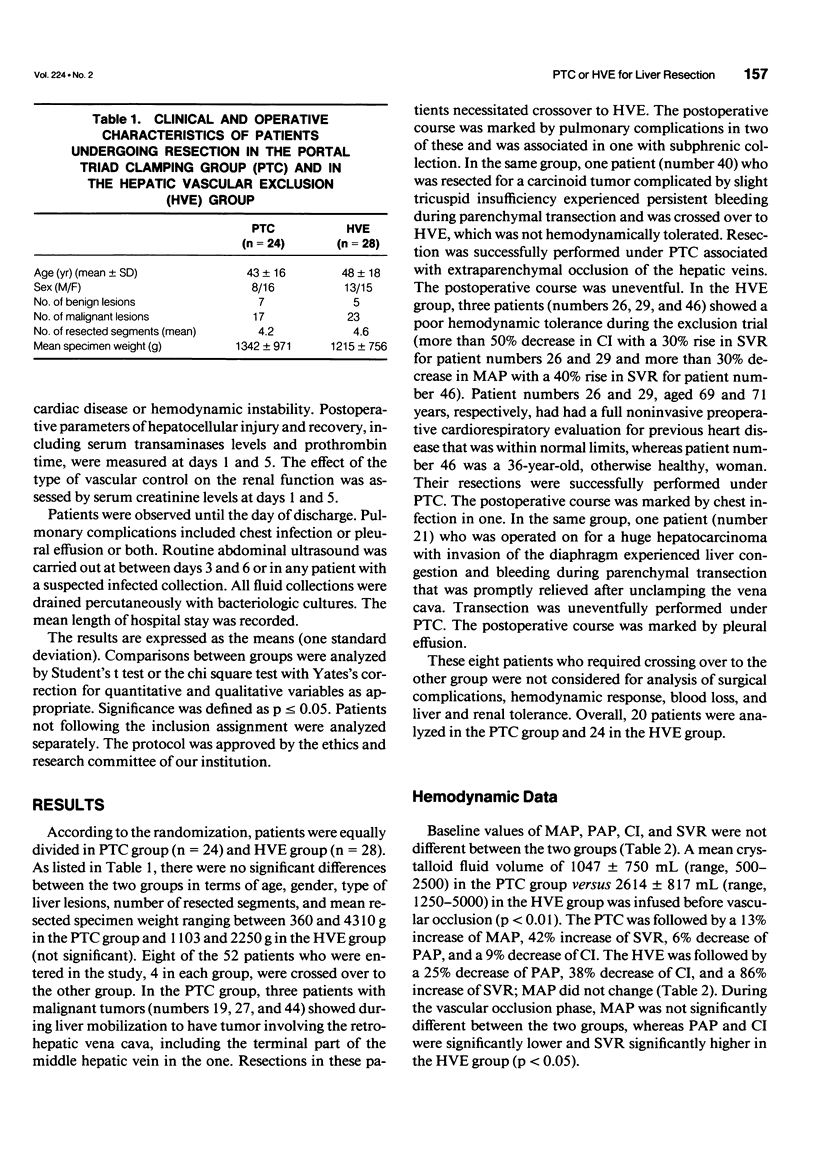
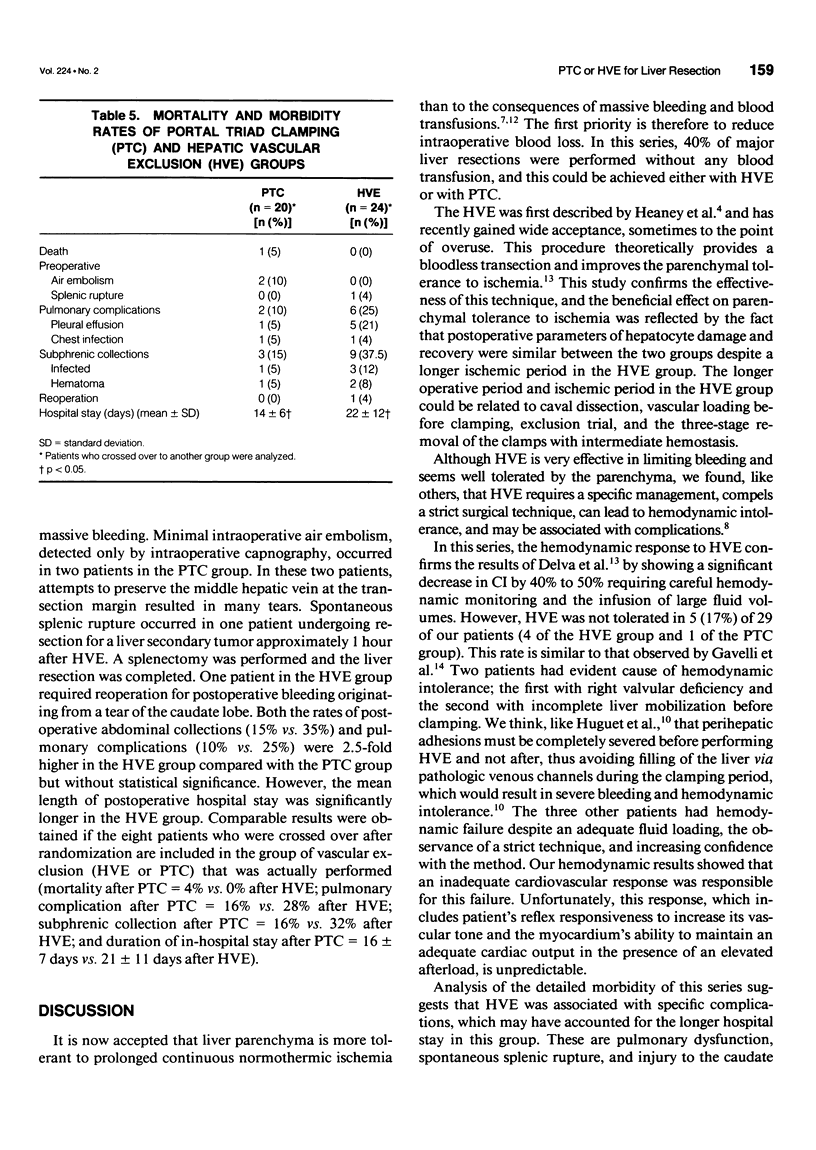
OBJECTIVE: The authors compared operative course of patients undergoing major liver resections under portal triad clamping (PTC) or under hepatic vascular exclusion (HVE). SUMMARY BACKGROUND DATA: Reduced blood loss during liver resection is achieved by PTC or HVE. Specific complications and postoperative hepatocellular injury mediated with two procedures have not been compared. METHODS: Fifty-two noncirrhotic patients undergoing major liver resections were included in a prospective randomized study comparing both the intraoperative and postoperative courses under PTC (n = 24) or under HVE (n = 28). RESULTS: The two groups were similar at entry, but eight patients were crossed over to the other group during resection. In the HVE group, hemodynamic intolerance occurred in four (14%) patients. In the PTC group, pedicular clamping was not efficient in four patients, including three with involvement of the cavohepatic intersection and one with persistent bleeding due to tricuspid insufficiency. Intraoperative blood losses and postoperative enzyme level reflecting hepatocellular injury were similar in the two groups. Mean operative duration and mean clampage duration were significantly increased after HVE. Postoperative abdominal collections and pulmonary complications were 2.5-fold higher after HVE but without statistical significance, whereas the mean length of postoperative hospital stay was longer after HVE. CONCLUSIONS: This study shows that both methods of vascular occlusion are equally effective in reducing blood loss in major liver resections. The HVE is associated with unpredictable hemodynamic intolerance, increased postoperative complications with a longer hospital stay, and should be restricted to lesions involving the cavo-hepatic intersection.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belghiti J., Di Carlo I., Sauvanet A., Uribe M., Fekete F. A ten-year experience with hepatic resection in 338 patients: evolutions in indications and of operative mortality. Eur J Surg. 1994 May;160(5):277–282. [PubMed] [Google Scholar]
- Bismuth H., Castaing D., Garden O. J. Major hepatic resection under total vascular exclusion. Ann Surg. 1989 Jul;210(1):13–19. doi: 10.1097/00000658-198907000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham J. D., Fong Y., Shriver C., Melendez J., Marx W. L., Blumgart L. H. One hundred consecutive hepatic resections. Blood loss, transfusion, and operative technique. Arch Surg. 1994 Oct;129(10):1050–1056. doi: 10.1001/archsurg.1994.01420340064011. [DOI] [PubMed] [Google Scholar]
- Delva E., Barberousse J. P., Nordlinger B., Ollivier J. M., Vacher B., Guilmet C., Huguet C. Hemodynamic and biochemical monitoring during major liver resection with use of hepatic vascular exclusion. Surgery. 1984 Mar;95(3):309–318. [PubMed] [Google Scholar]
- Delva E., Camus Y., Nordlinger B., Hannoun L., Parc R., Deriaz H., Lienhart A., Huguet C. Vascular occlusions for liver resections. Operative management and tolerance to hepatic ischemia: 142 cases. Ann Surg. 1989 Feb;209(2):211–218. doi: 10.1097/00000658-198902000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douzdjian V., Broughan T. A. Spontaneous splenic rupture during total vascular occlusion of the liver. Br J Surg. 1995 Mar;82(3):406–407. doi: 10.1002/bjs.1800820343. [DOI] [PubMed] [Google Scholar]
- Elias D., Lasser P., Rougier P., Ducreux M., Bognel C., Roche A. Frequency, technical aspects, results, and indications of major hepatectomy after prolonged intra-arterial hepatic chemotherapy for initially unresectable hepatic tumors. J Am Coll Surg. 1995 Feb;180(2):213–219. [PubMed] [Google Scholar]
- Emond J., Wachs M. E., Renz J. F., Kelley S., Harris H., Roberts J. P., Ascher N. L., Lim R. C., Jr Total vascular exclusion for major hepatectomy in patients with abnormal liver parenchyma. Arch Surg. 1995 Aug;130(8):824–831. doi: 10.1001/archsurg.1995.01430080026003. [DOI] [PubMed] [Google Scholar]
- Emre S., Schwartz M. E., Katz E., Miller C. M. Liver resection under total vascular isolation. Variations on a theme. Ann Surg. 1993 Jan;217(1):15–19. doi: 10.1097/00000658-199301000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney J. P., Stanton W. K., Halbert D. S., Seidel J., Vice T. An improved technic for vascular isolation of the liver: experimental study and case reports. Ann Surg. 1966 Feb;163(2):237–241. doi: 10.1097/00000658-196602000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huguet C., Addario-Chieco P., Gavelli A., Arrigo E., Harb J., Clement R. R. Technique of hepatic vascular exclusion for extensive liver resection. Am J Surg. 1992 Jun;163(6):602–605. doi: 10.1016/0002-9610(92)90567-b. [DOI] [PubMed] [Google Scholar]
- Huguet C., Gavelli A., Chieco P. A., Bona S., Harb J., Joseph J. M., Jobard J., Gramaglia M., Lasserre M. Liver ischemia for hepatic resection: where is the limit? Surgery. 1992 Mar;111(3):251–259. [PubMed] [Google Scholar]
- Jamieson G. G., Corbel L., Campion J. P., Launois B. Major liver resection without a blood transfusion: is it a realistic objective? Surgery. 1992 Jul;112(1):32–36. [PubMed] [Google Scholar]
- Makuuchi M., Takayama T., Gunvén P., Kosuge T., Yamazaki S., Hasegawa H. Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients. World J Surg. 1989 Sep-Oct;13(5):644–648. doi: 10.1007/BF01658893. [DOI] [PubMed] [Google Scholar]
- Makuuchi M., Yamamoto J., Takayama T., Kosuge T., Gunvén P., Yamazaki S., Hasegawa H. Extrahepatic division of the right hepatic vein in hepatectomy. Hepatogastroenterology. 1991 Apr;38(2):176–179. [PubMed] [Google Scholar]
- Nagorney D. M., van Heerden J. A., Ilstrup D. M., Adson M. A. Primary hepatic malignancy: surgical management and determinants of survival. Surgery. 1989 Oct;106(4):740–749. [PubMed] [Google Scholar]
- Roy A., Lapointe R., Dagenais M., McAlister V., Grant D. R., Brown W., Hutton L., Wall W. J. Paralysie diaphragmatique droite après transplantation hépatique. Ann Chir. 1993;47(9):810–815. [PubMed] [Google Scholar]
- Shaw B. W., Jr, Martin D. J., Marquez J. M., Kang Y. G., Bugbee A. C., Jr, Iwatsuki S., Griffith B. P., Hardesty R. L., Bahnson H. T., Starzl T. E. Venous bypass in clinical liver transplantation. Ann Surg. 1984 Oct;200(4):524–534. doi: 10.1097/00000658-198410000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka K., Uemoto S., Tokunaga Y., Fujita S., Sano K., Nishizawa T., Sawada H., Shirahase I., Kim H. J., Yamaoka Y. Surgical techniques and innovations in living related liver transplantation. Ann Surg. 1993 Jan;217(1):82–91. doi: 10.1097/00000658-199301000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veroli P., el Hage C., Ecoffey C. Does adult liver transplantation without venovenous bypass result in renal failure? Anesth Analg. 1992 Oct;75(4):489–494. doi: 10.1213/00000539-199210000-00004. [DOI] [PubMed] [Google Scholar]
- Yamaoka Y., Ozawa K., Kumada K., Shimahara Y., Tanaka K., Mori K., Takayasu T., Okamoto R., Kobayashi N., Konishi Y. Total vascular exclusion for hepatic resection in cirrhotic patients. Application of venovenous bypass. Arch Surg. 1992 Mar;127(3):276–280. doi: 10.1001/archsurg.1992.01420030038007. [DOI] [PubMed] [Google Scholar]


