Abstract
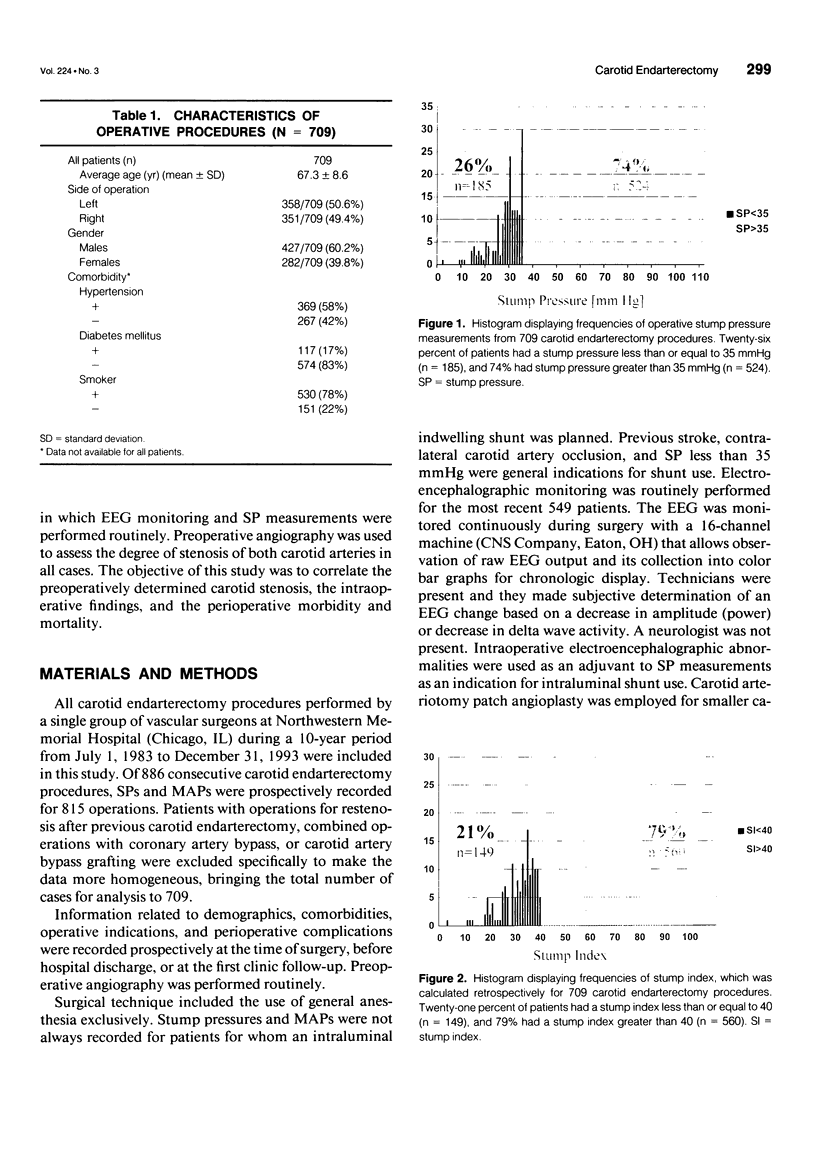
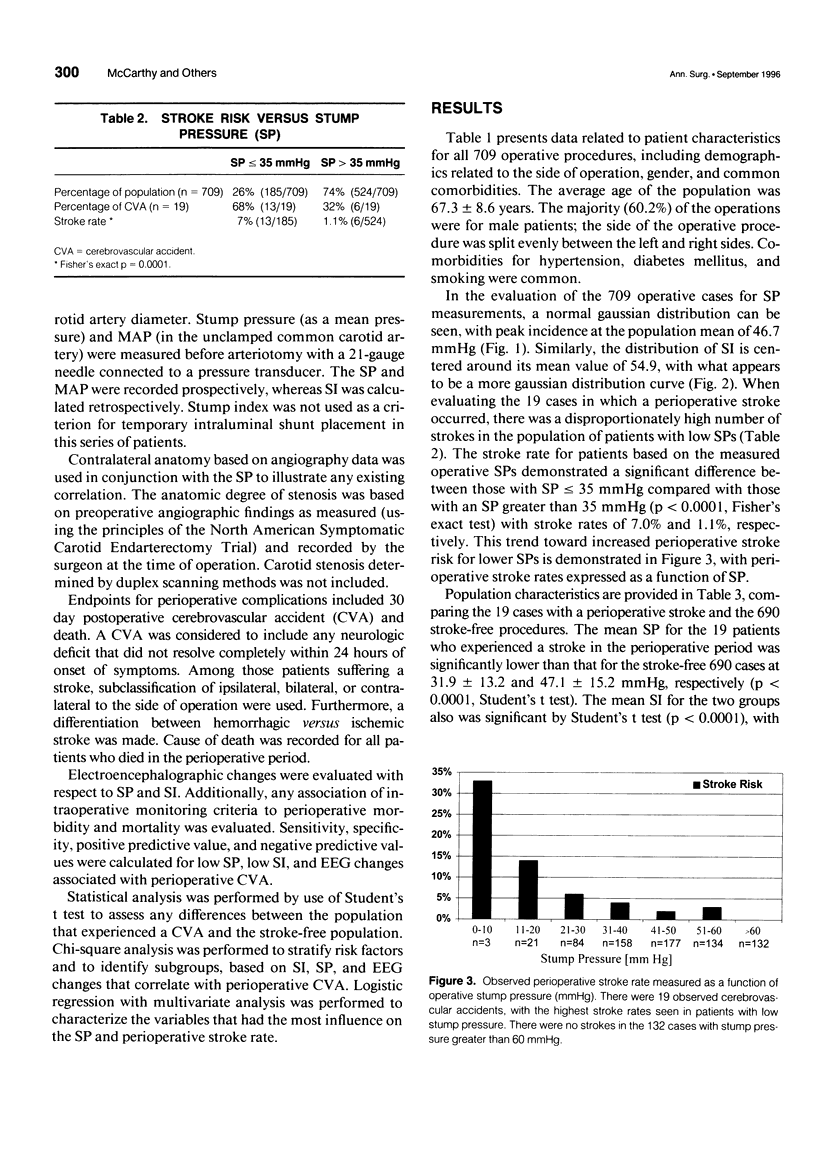
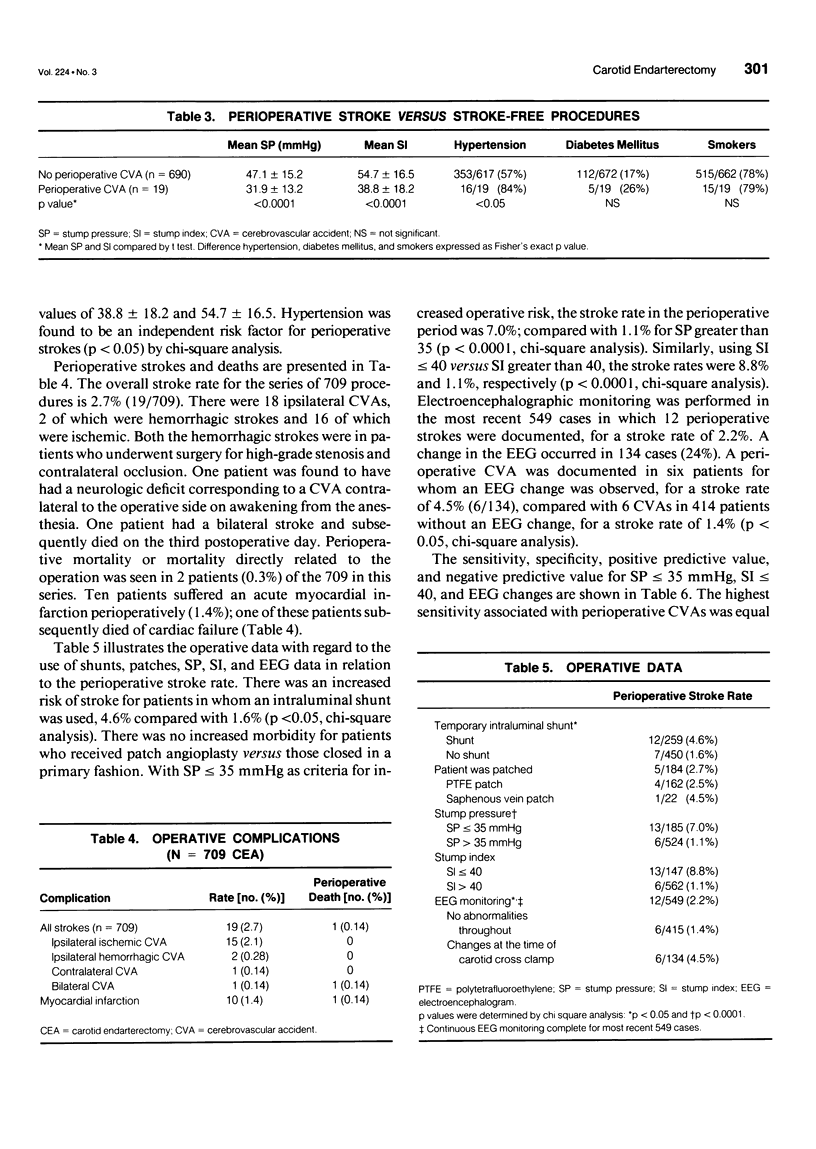
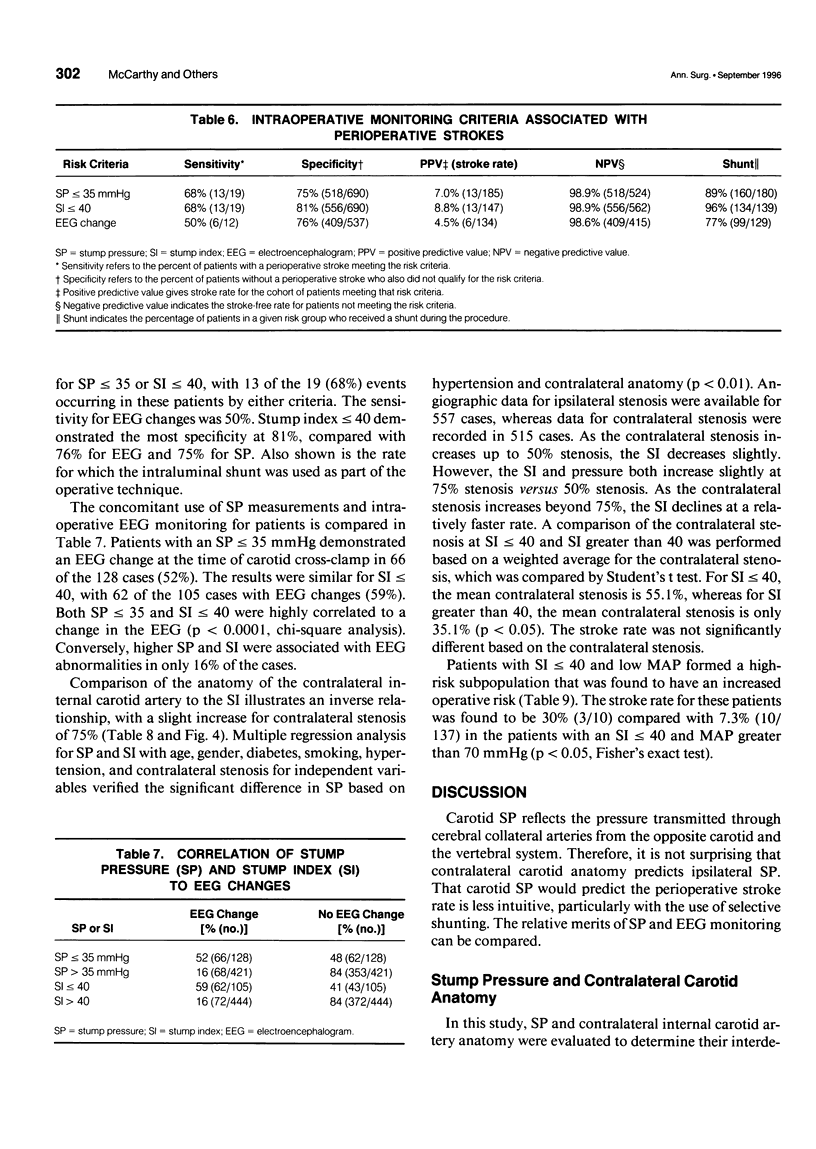
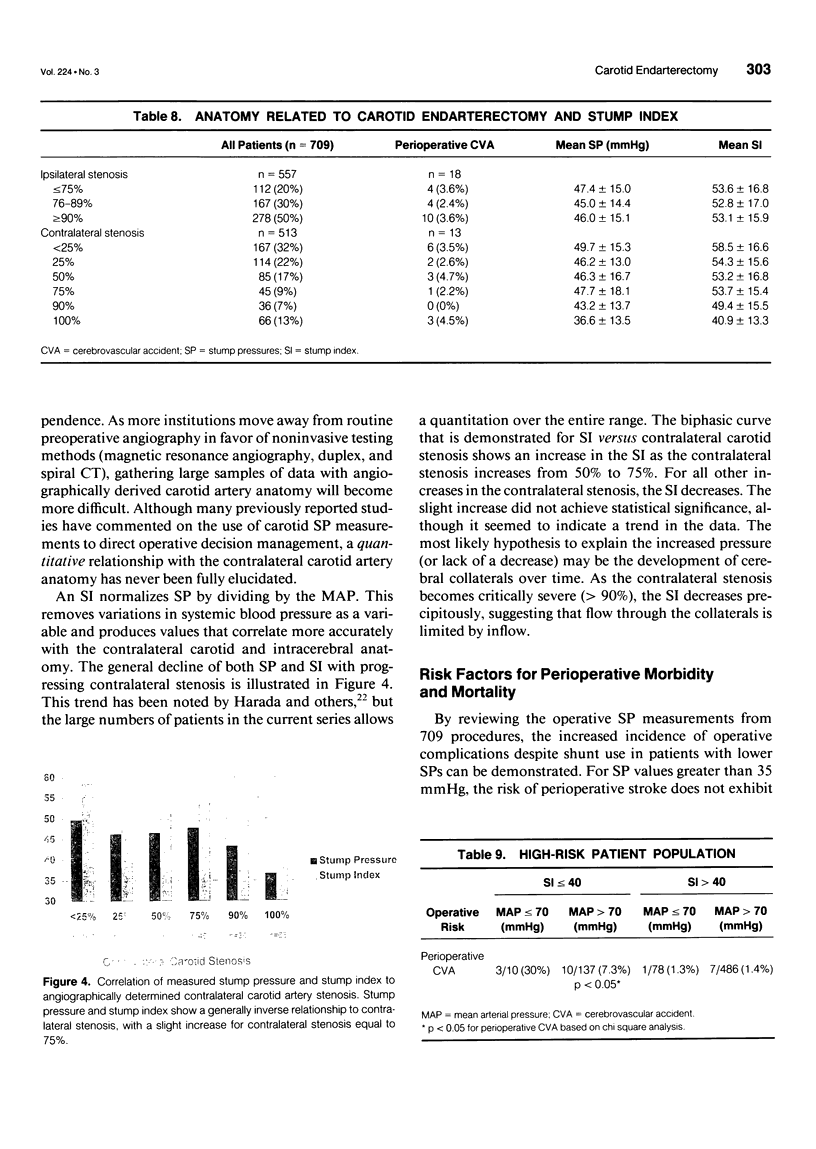
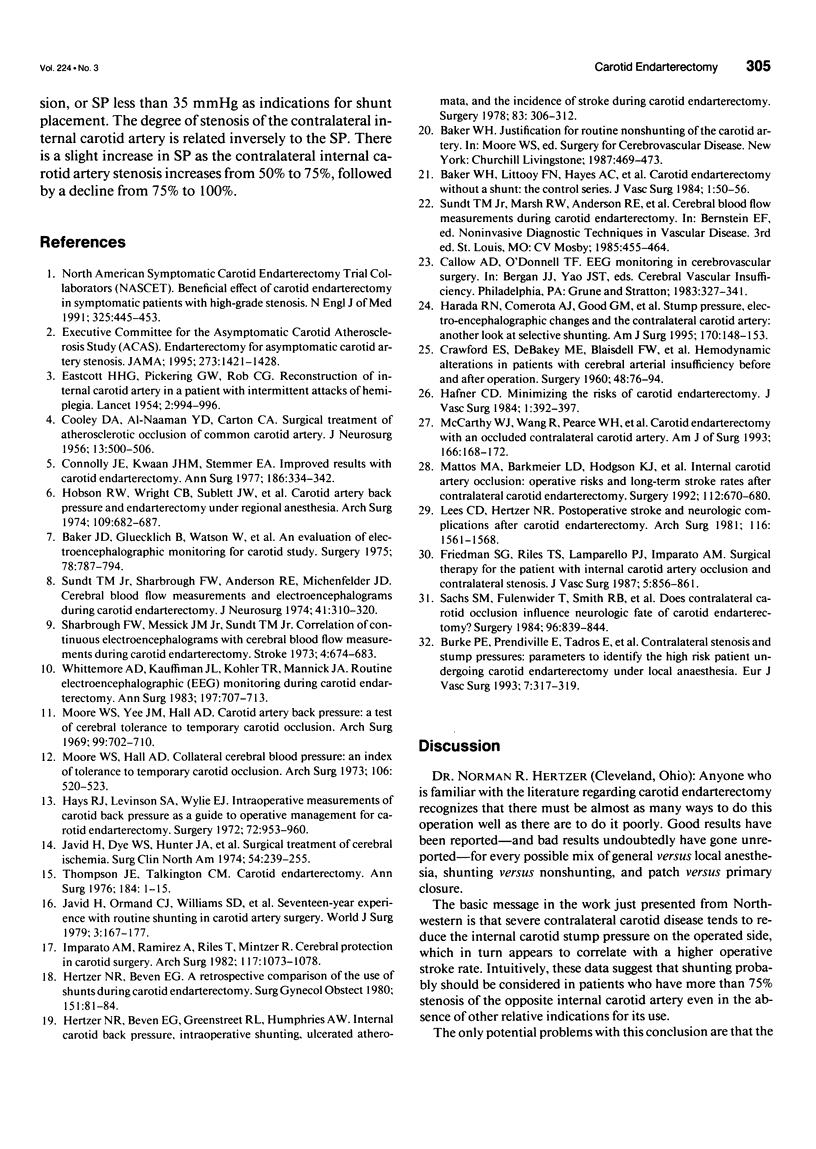
OBJECTIVE: The authors analyzed a single institution's 10-year experience with intraoperative monitoring during 709 primary carotid endarterectomies and investigated the impact of contralateral internal carotid artery stenosis on carotid artery stump pressure (SP). SUMMARY BACKGROUND DATA: Stump pressure reflects the combination of contralateral carotid artery anatomy, collateral intracranial vasculature, and systemic blood pressure. By controlling for blood pressure with a stump index (SI) (SI = [SP/mean arterial pressure] x 100), a correlation between pressure and contralateral carotid artery anatomy can be demonstrated. Although the use of SP has long been advocated as an indicator of adequate cerebral perfusion, its correlation with perioperative complications while using an intraluminal shunt has not been evaluated completely. METHODS: From a series of 886 primary carotid endarterectomy cases, SP and mean arterial pressure were measured prospectively in 709 procedures. Temporary intraluminal shunts were used in cases with demonstrated contralateral carotid occlusion, prior cerebrovascular accident (CVA), or SPs less than 35 mmHg. Ipsilateral and contralateral angiographic degree of carotid stenosis was recorded at the time of the operation. Neurologic status was recorded prospectively for all 709 procedures. Operative electroencephalogram (EEG) changes and SP then were compared with the neurologic status of the patient in the perioperative period. RESULTS: The mean SP for the group (n = 709) was 46.7 +/- 15.3 mmHg (mean +/- standard deviation [SD]) with a mean SI of 54.9 +/- 22.6. The distribution for the SI is a more gaussian curve than that for SP. There were 19 ipsilateral CVAs (2.7%). The mean SP in the nonstroke group was 47.1 +/- 15.2 mmHg (mean SI = 54.7 +/- 16.5) compared with 31.9 +/- 13.2 mmHg (mean SI = 38.8 +/- 18.2) in the stroke group (P < 0.0001). Stroke rate for SP < or = 35 mmHg was 7% (13/185) versus 1.1% (6/524) for SP > 35 (p < 0.0001). Stump index and SP are related to contralateral carotid artery stenosis. The pattern of SI or SP versus contralateral stenosis is biphasic, with an increase at 75%. If SI is < or = 40, the mean contralateral stenosis is 55.1%; if SI is > 40, the mean contralateral stenosis is 35.1% (p < 0.05). Continuous EEG monitoring was completed for the 549 most recent operations. Patients who had a perioperative stroke had EEG changes observed during the procedure in only 6 of 12 cases (50% sensitivity), with 76% specificity. Using SP < or = 35 mmHg, sensitivity was 68% and specificity was 75%.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker J. D., Gluecklich B., Watson C. W., Marcus E., Kamat V., Callow A. D. An evaluation of electroencephalographic monitoring for carotid study. Surgery. 1975 Dec;78(6):787–794. [PubMed] [Google Scholar]
- Baker W. H., Littooy F. N., Hayes A. C., Dorner D. B., Stubbs D. Carotid endarterectomy without a shunt: the control series. J Vasc Surg. 1984 Jan;1(1):50–56. [PubMed] [Google Scholar]
- Burke P. E., Prendiville E., Tadros E., Colgan M. P., Moore D. J., Shanik D. G. Contralateral stenosis and stump pressures: parameters to identify the high risk patient undergoing carotid endarterectomy under local anaesthesia. Eur J Vasc Surg. 1993 May;7(3):317–319. doi: 10.1016/s0950-821x(05)80015-5. [DOI] [PubMed] [Google Scholar]
- COOLEY D. A., AL-NAAMAN Y. D., CARTON C. A. Surgical treatment of arteriosclerotic occlusion of common carotid artery. J Neurosurg. 1956 Sep;13(5):500–506. doi: 10.3171/jns.1956.13.5.0500. [DOI] [PubMed] [Google Scholar]
- CRAWFORD E. S., DE BAKEY M. E., BLAISDELL F. W., MORRIS G. C., Jr, FIELDS W. S. Hemodynamic alterations in patients with cerebral arterial insufficiency before and after operation. Surgery. 1960 Jul;48:76–94. [PubMed] [Google Scholar]
- Connolly J. E., Kwaan J. H., Stemmer E. A. Improved results with carotid endarterectomy. Ann Surg. 1977 Sep;186(3):334–342. doi: 10.1097/00000658-197709000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EASTCOTT H. H., PICKERING G. W., ROB C. G. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet. 1954 Nov 13;267(6846):994–996. doi: 10.1016/s0140-6736(54)90544-9. [DOI] [PubMed] [Google Scholar]
- Friedman S. G., Riles T. S., Lamparello P. J., Imparato A. M., Sakwa M. P. Surgical therapy for the patient with internal carotid artery occlusion and contralateral stenosis. J Vasc Surg. 1987 Jun;5(6):856–861. doi: 10.1067/mva.1987.avs0050856. [DOI] [PubMed] [Google Scholar]
- Hafner C. D. Minimizing the risks of carotid endarterectomy. J Vasc Surg. 1984 May;1(3):392–397. [PubMed] [Google Scholar]
- Harada R. N., Comerota A. J., Good G. M., Hashemi H. A., Hulihan J. F. Stump pressure, electroencephalographic changes, and the contralateral carotid artery: another look at selective shunting. Am J Surg. 1995 Aug;170(2):148–153. doi: 10.1016/s0002-9610(99)80275-x. [DOI] [PubMed] [Google Scholar]
- Hays R. J., Levinson S. A., Wylie E. J. Intraoperative measurement of carotid back pressure as a guide to operative management for carotid endarterectomy. Surgery. 1972 Dec;72(6):953–960. [PubMed] [Google Scholar]
- Hertzer N. R., Beven E. G. A retrospective comparison of the use of shunts during carotid endarterectomy. Surg Gynecol Obstet. 1980 Jul;151(1):81–84. [PubMed] [Google Scholar]
- Hertzer N. R., Beven E. G., Greenstreet R. L., Humphries A. W. Internal carotid back pressure, intraoperative shunting, ulcerated atheromata, and the incidence of stroke during carotid endarterectomy. Surgery. 1978 Mar;83(3):306–312. [PubMed] [Google Scholar]
- Hobson R. W., 2nd, Wright C. B., Sublett J. W., Fedde C. W., Rich N. M. Carotid artery back pressure and endarterectomy under regional anesthesia. Arch Surg. 1974 Nov;109(5):682–687. doi: 10.1001/archsurg.1974.01360050076017. [DOI] [PubMed] [Google Scholar]
- Imparato A. M., Ramirez A., Riles T., Mintzer R. Cerebral protection in carotid surgery. Arch Surg. 1982 Aug;117(8):1073–1078. doi: 10.1001/archsurg.1982.01380320057015. [DOI] [PubMed] [Google Scholar]
- Javid H., Dye W. S., Hunter J. A., Najafi H., Goldin M. D., Serry C. Surgical treatment of cerebral ischemia. Surg Clin North Am. 1974 Feb;54(1):239–255. doi: 10.1016/s0039-6109(16)40247-1. [DOI] [PubMed] [Google Scholar]
- Javid H., Julian O. C., Dye W. S., Hunter J. A., Najafi H., Goldin M. D., Serry C., DeLaria G. A. Seventeen-year experience with routine shunting in carotid artery surgery. World J Surg. 1979 Jul 16;3(2):167–177. doi: 10.1007/BF01561267. [DOI] [PubMed] [Google Scholar]
- Lees C. D., Hertzer N. R. Postoperative stroke and late neurologic complications after carotid endarterectomy. Arch Surg. 1981 Dec;116(12):1561–1568. doi: 10.1001/archsurg.1981.01380240045007. [DOI] [PubMed] [Google Scholar]
- Mattos M. A., Barkmeier L. D., Hodgson K. J., Ramsey D. E., Sumner D. S. Internal carotid artery occlusion: operative risks and long-term stroke rates after contralateral carotid endarterectomy. Surgery. 1992 Oct;112(4):670–680. [PubMed] [Google Scholar]
- McCarthy W. J., Wang R., Pearce W. H., Flinn W. R., Yao J. S. Carotid endarterectomy with an occluded contralateral carotid artery. Am J Surg. 1993 Aug;166(2):168–172. doi: 10.1016/s0002-9610(05)81050-5. [DOI] [PubMed] [Google Scholar]
- Moore W. S., Hall A. D. Carotid artery back pressure: a test of cerebral tolerance to temporary carotid occlusion. Arch Surg. 1969 Dec;99(6):702–710. doi: 10.1001/archsurg.1969.01340180026005. [DOI] [PubMed] [Google Scholar]
- Moore W. S., Yee J. M., Hall A. D. Collateral cerebral blood pressure. An index of tolerance to temporary carotid occlusion. Arch Surg. 1973 Apr;106(4):521–523. doi: 10.1001/archsurg.1973.01350160134022. [DOI] [PubMed] [Google Scholar]
- Nichelmann M., Hewald B., Grune B. Thermoregulatorische Wärmeproduktion bei Legehybriden--Bezichungen zwischen zwischen Lebensalter und Wärmeproduktion. Arch Exp Veterinarmed. 1983;37(2):341–352. [PubMed] [Google Scholar]
- Sachs S. M., Fulenwider J. T., Smith R. B., 3rd, Darden W. A., Salam A. A., Perdue G. D. Does contralateral carotid occlusion influence neurologic fate of carotid endarterectomy? Surgery. 1984 Nov;96(5):839–844. [PubMed] [Google Scholar]
- Sharbrough F. W., Messick J. M., Jr, Sundt T. M., Jr Correlation of continuous electroencephalograms with cerebral blood flow measurements during carotid endarterectomy. Stroke. 1973 Jul-Aug;4(4):674–683. doi: 10.1161/01.str.4.4.674. [DOI] [PubMed] [Google Scholar]
- Sundt T. M., Jr, Sharbrough F. W., Anderson R. E., Michenfelder J. D. Cerebral blood flow measurements and electroencephalograms during carotid endarterectomy. J Neurosurg. 1974 Sep;41(3):310–320. doi: 10.3171/jns.1974.41.3.0310. [DOI] [PubMed] [Google Scholar]
- Thompson J. E., Talkington C. M. Carotid endarterectomy. Ann Surg. 1976 Jul;184(1):1–15. doi: 10.1097/00000658-197607000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore A. D., Kauffman J. L., Kohler T. R., Mannick J. A. Routine electroencephalographic (EEG) monitoring during carotid endarterectomy. Ann Surg. 1983 Jun;197(6):707–713. doi: 10.1097/00000658-198306000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]