Abstract
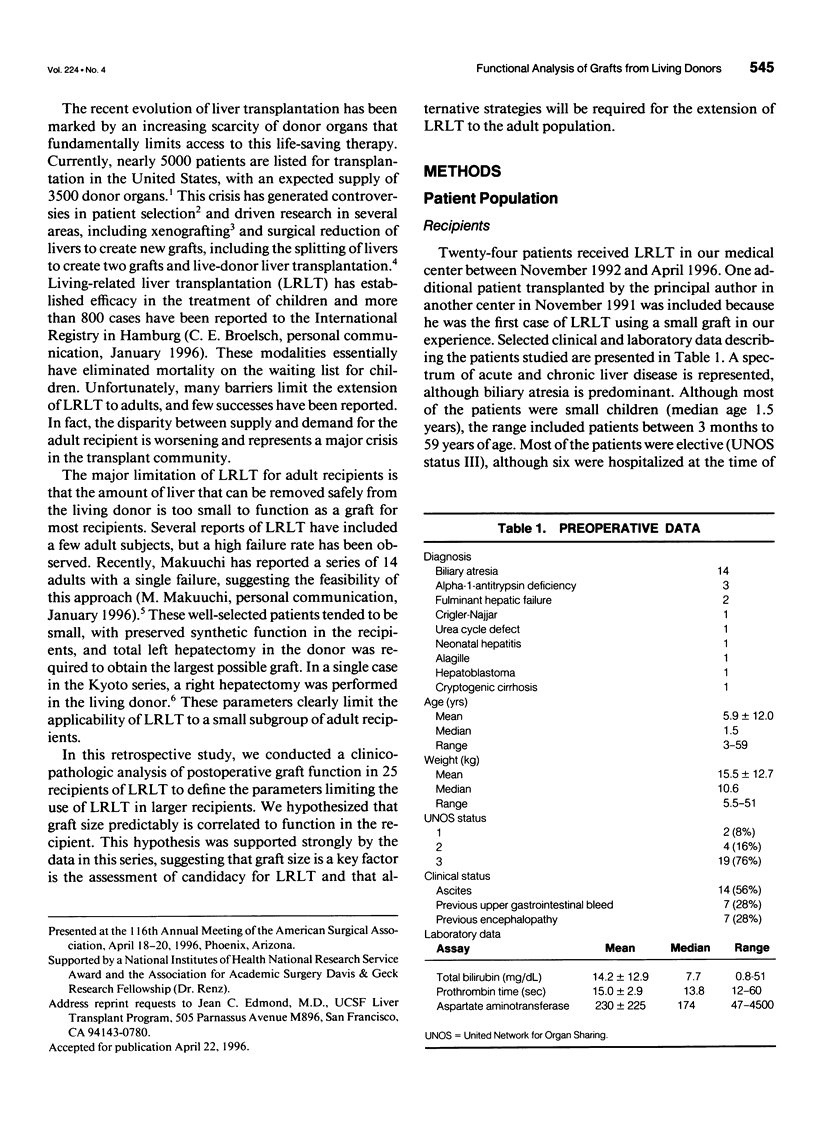
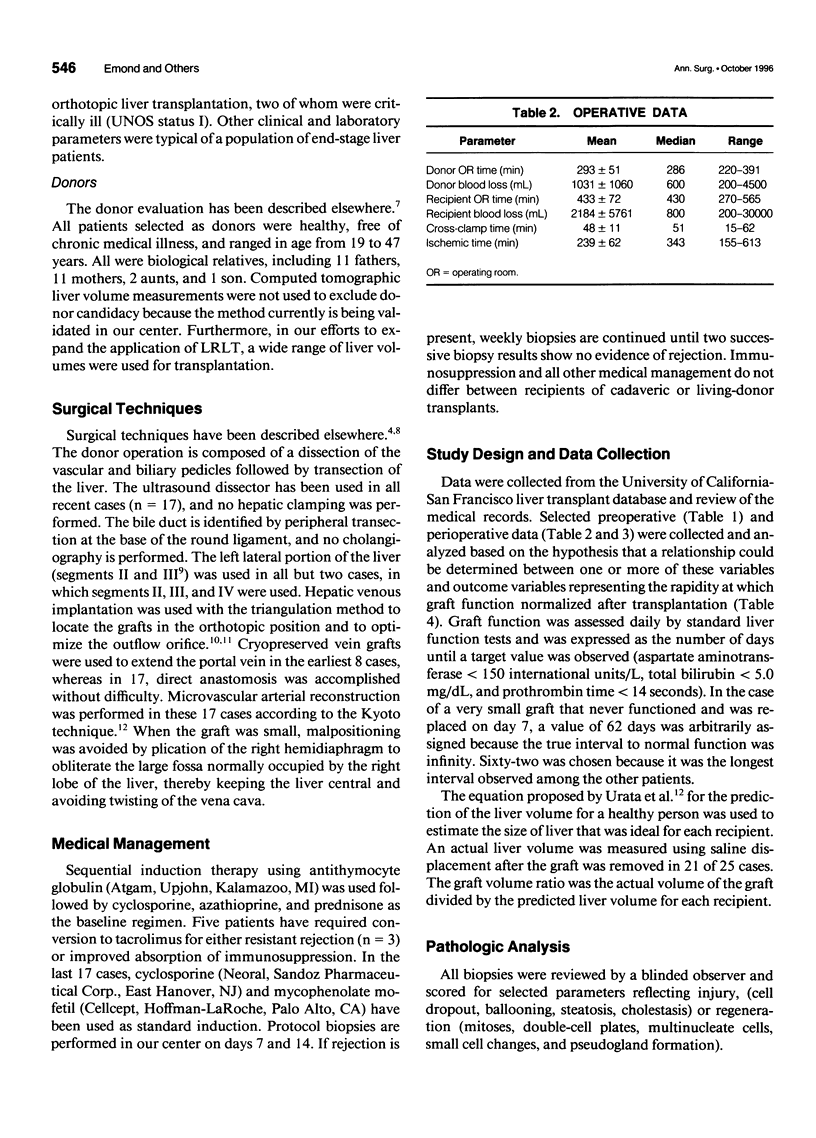
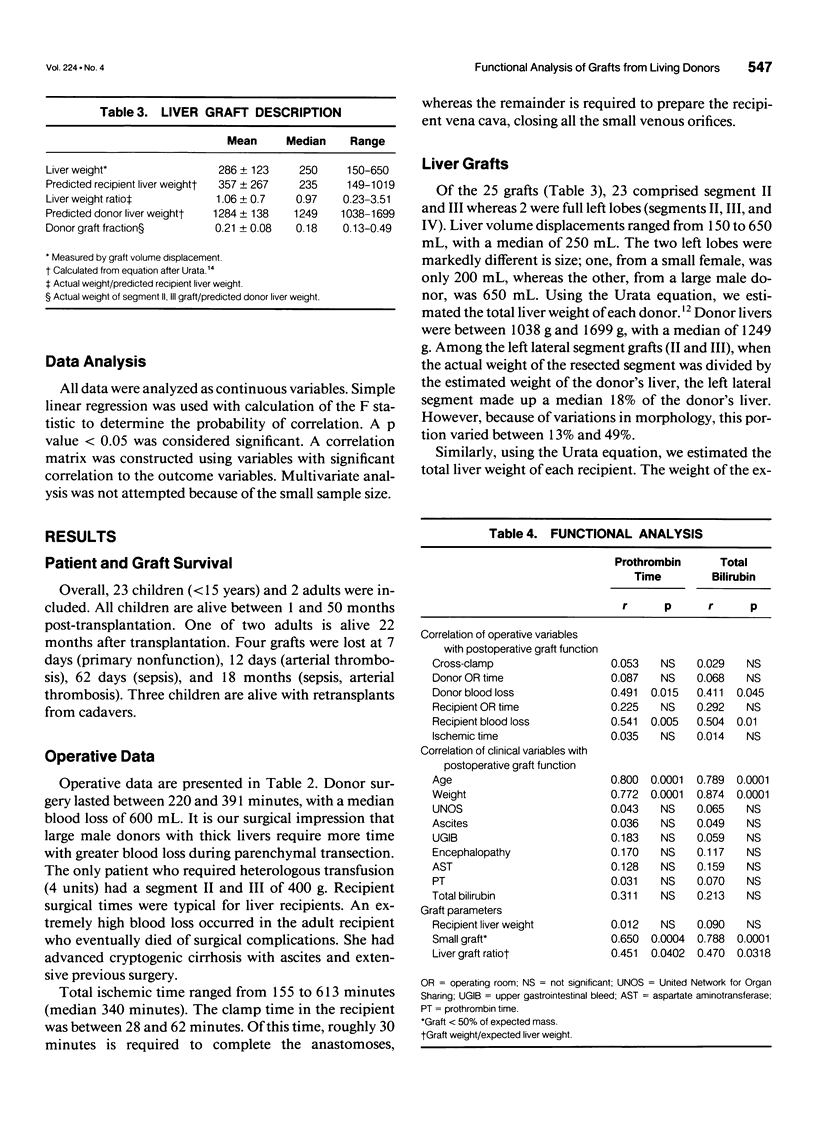
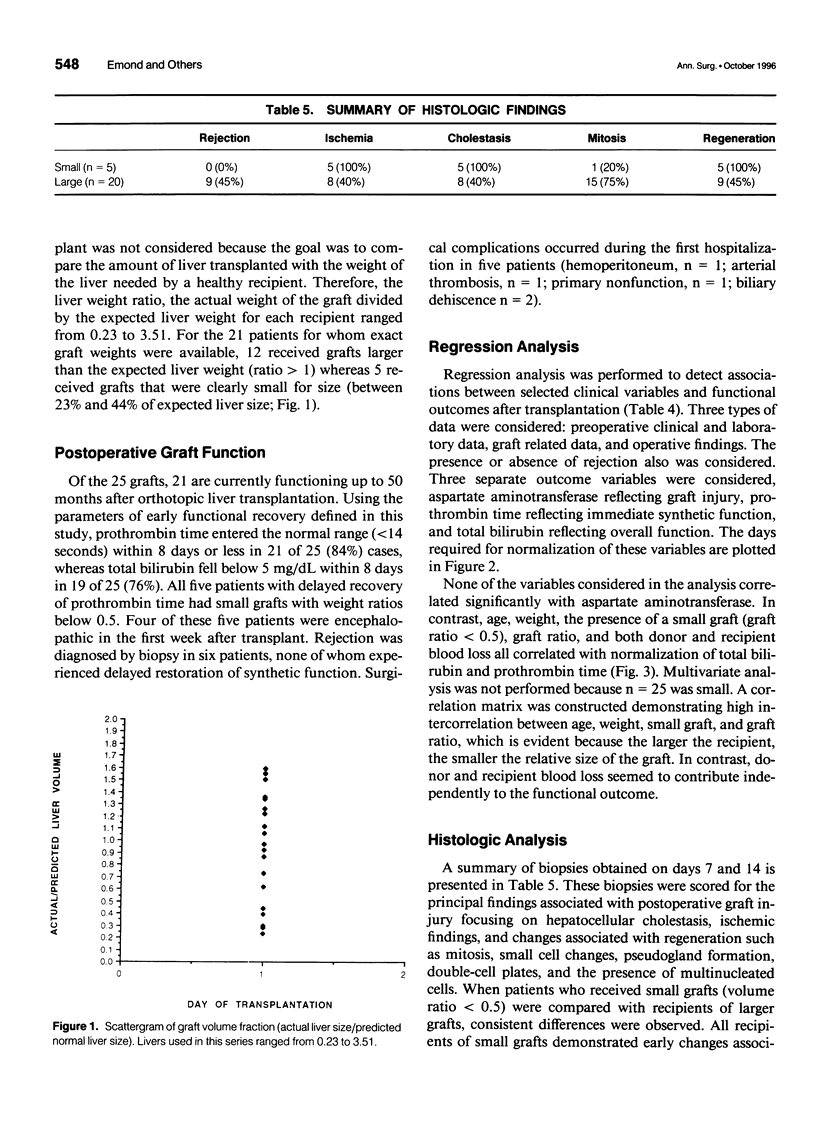
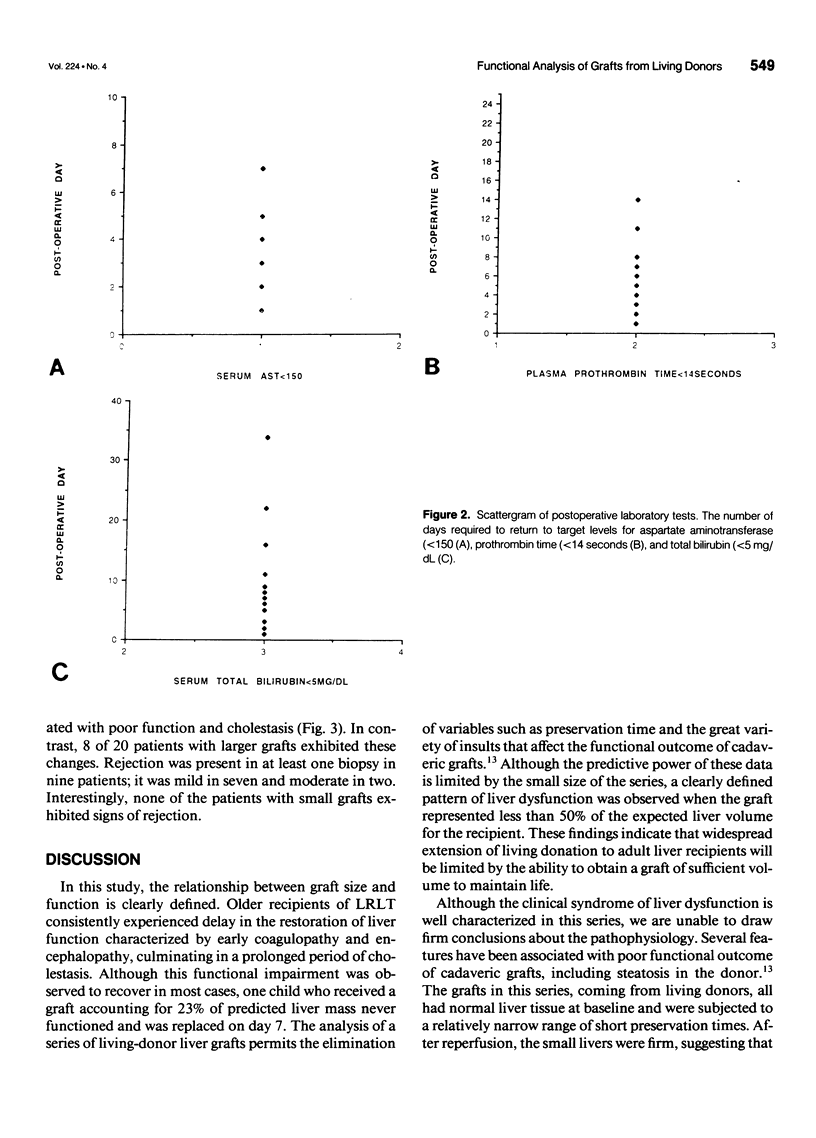
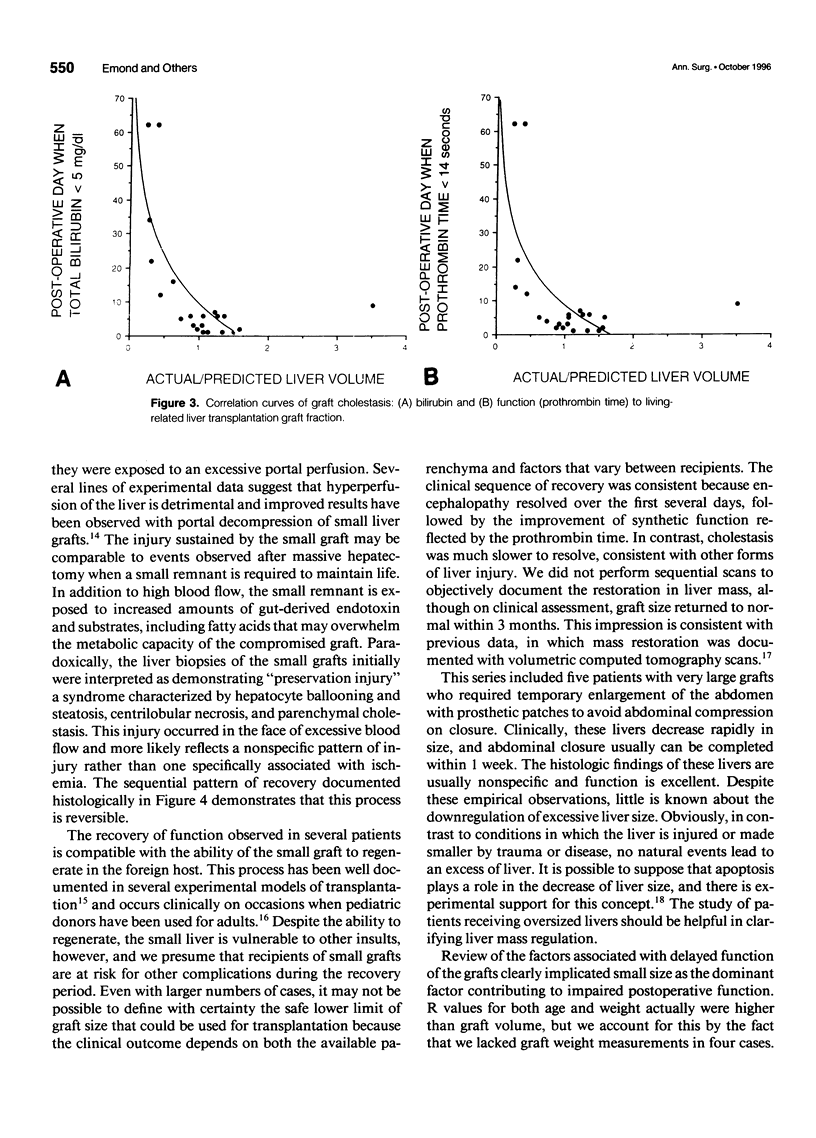
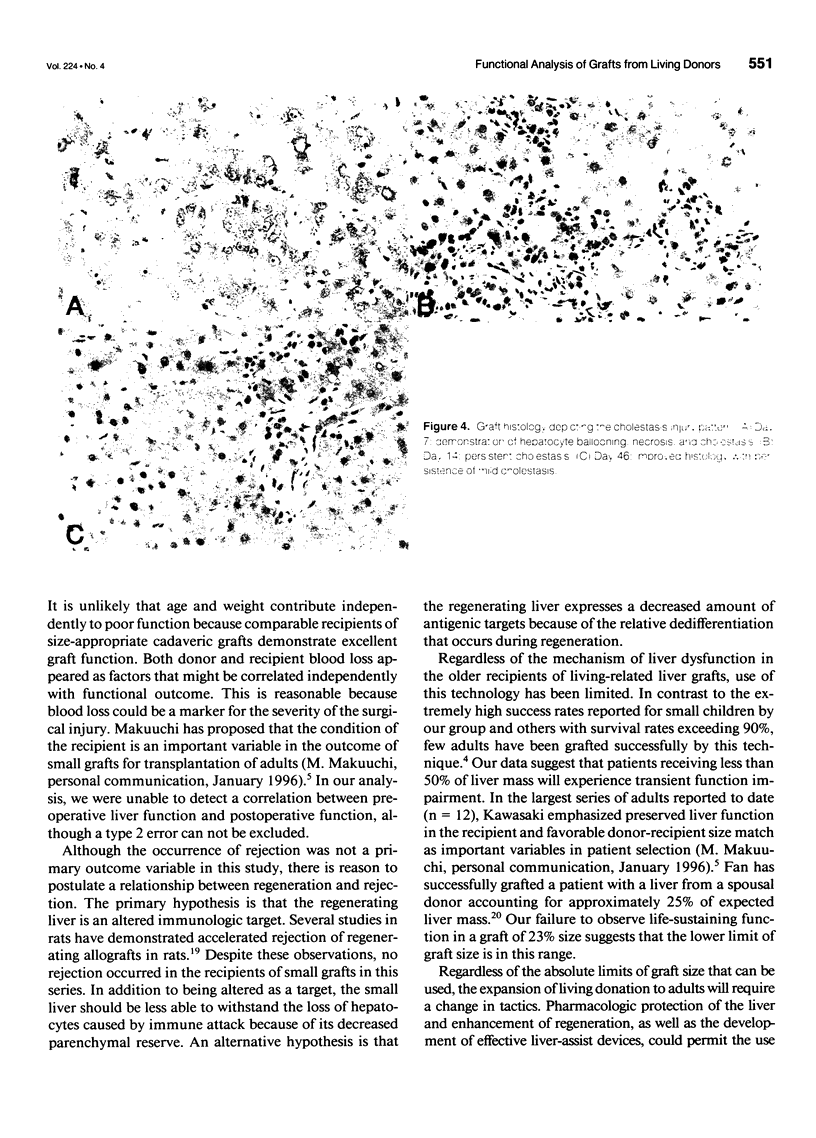
OBJECTIVE: Living-related liver transplantation (LRLT) has established efficacy in children. In a larger recipient, LRLT requires the use of a small graft because of limits on the donor hepatectomy. SUMMARY BACKGROUND DATA: The minimum graft weight required for successful transplantation has not been well established, although a characteristic pattern of graft dysfunction has been observed in our patients who receive small grafts. The authors present a clinicopathologic study of small liver grafts obtained from living donors. METHODS: Clinical and histologic data were reviewed for 25 patients receiving LRLT. In five older recipients (small group), the graft represented 50% or less of expected liver weight, whereas in 20 others (large group), the graft represented at least 60% of expected liver weight. A retrospective analysis of graft function was conducted by analyzing clinical parameters and histology. RESULTS: In the small group, 2 of 5 grafts (40%) were lost due to poor function, leading to one patient death (20% mortality), whereas in the large group, 2 of 20 grafts (10%) were lost due to arterial thrombosis without patient mortality. Early ischemic damage related to transplant was comparable with aspartate aminotransferase 203 +/- 23 (small group) and 290 +/- 120 (large group) at 24 hours (p = not significant). Early function was significantly decreased in the small group, with prothrombin time 18.2 +/- 2.2 seconds versus 14.8 +/- 1.6 seconds (large group) on day 3 (p = 0.034). All small group patients developed cholestasis with significantly increased total bilirubin levels at day 7 (16 +/- 5.2 mg% vs. 3.7 +/- 2.7 mg%; p = 0.021) and day 14 (12.0 +/- 7.4 vs. 1.8 +/- 0.7; p = 0.021) compared with the large group. Protocol biopsies in the small group revealed a diffuse ischemic pattern with cellular ballooning on day 7, which progressed to cholestasis in subsequent biopsies. Large group biopsies showed minimal ischemic changes. Three small group patients recovered with normal liver function by 12 weeks. CONCLUSIONS: Clinical recovery after a small-for-size transplant is characterized by significant functional impairment associated with paradoxical histologic changes typical of ischemia. These changes apparently are due to graft injury, which can only be the result of small graft size. These findings have significant implications for the extension of LRLT to adults.
Full text
PDF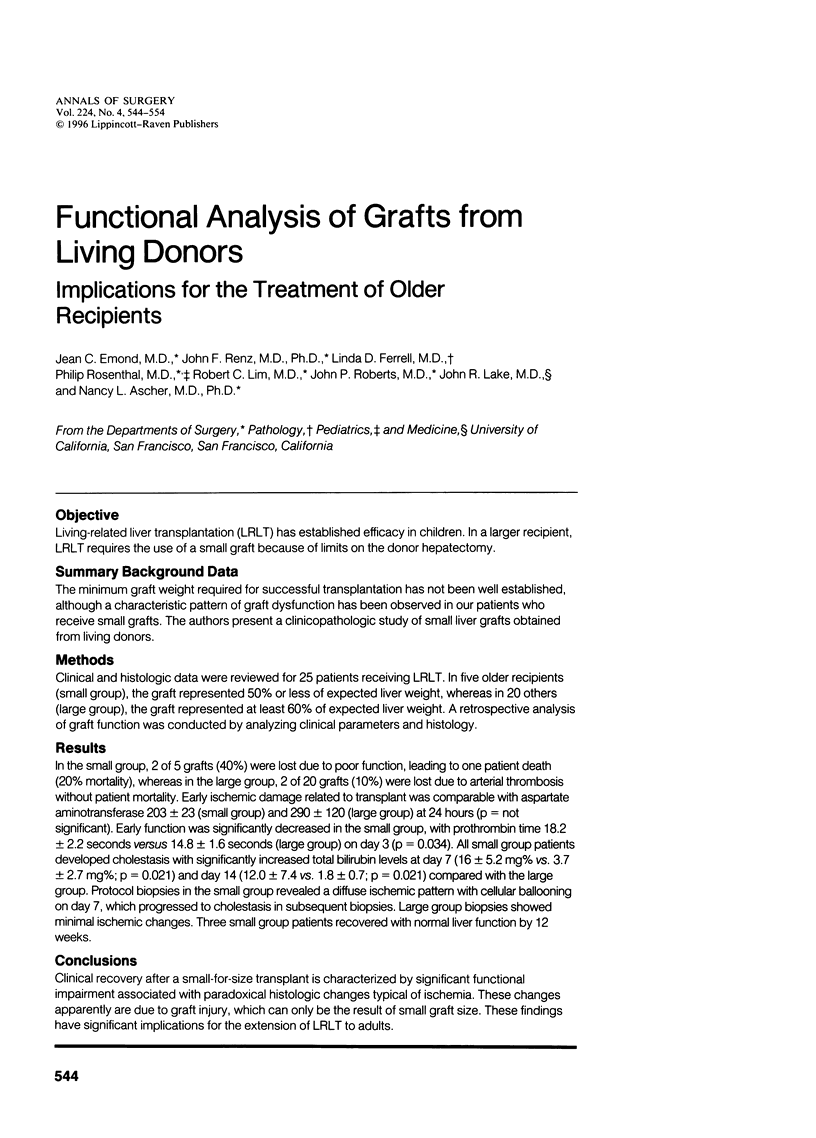
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Broelsch C. E., Emond J. C., Whitington P. F., Thistlethwaite J. R., Baker A. L., Lichtor J. L. Application of reduced-size liver transplants as split grafts, auxiliary orthotopic grafts, and living related segmental transplants. Ann Surg. 1990 Sep;212(3):368–377. doi: 10.1097/00000658-199009000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broelsch C. E., Whitington P. F., Emond J. C., Heffron T. G., Thistlethwaite J. R., Stevens L., Piper J., Whitington S. H., Lichtor J. L. Liver transplantation in children from living related donors. Surgical techniques and results. Ann Surg. 1991 Oct;214(4):428–439. doi: 10.1097/00000658-199110000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emond J. C. Clinical application of liver-related liver transplantation. Gastroenterol Clin North Am. 1993 Jun;22(2):301–315. [PubMed] [Google Scholar]
- Emond J. C., Heffron T. G., Whitington P. F., Broelsch C. E. Reconstruction of the hepatic vein in reduced size hepatic transplantation. Surg Gynecol Obstet. 1993 Jan;176(1):11–17. [PubMed] [Google Scholar]
- Emond J. C., Renz J. F. Surgical anatomy of the liver and its application to hepatobiliary surgery and transplantation. Semin Liver Dis. 1994 May;14(2):158–168. doi: 10.1055/s-2007-1007308. [DOI] [PubMed] [Google Scholar]
- Habib N., Tanaka K. Living-related liver transplantation in adult recipients: a hypothesis. Clin Transplant. 1995 Feb;9(1):31–34. [PubMed] [Google Scholar]
- Ichida T., Matsunami H., Kawasaki S., Makuuchi M., Harada T., Itoh S., Asakura H. Living related-donor liver transplantation from adult to adult for primary biliary cirrhosis. Ann Intern Med. 1995 Feb 15;122(4):275–276. doi: 10.7326/0003-4819-122-4-199502150-00006. [DOI] [PubMed] [Google Scholar]
- Kawasaki S., Makuuchi M., Ishizone S., Matsunami H., Terada M., Kawarazaki H. Liver regeneration in recipients and donors after transplantation. Lancet. 1992 Mar 7;339(8793):580–581. doi: 10.1016/0140-6736(92)90867-3. [DOI] [PubMed] [Google Scholar]
- Krams S. M., Egawa H., Quinn M. B., Villanueva J. C., Garcia-Kennedy R., Martinez O. M. Apoptosis as a mechanism of cell death in liver allograft rejection. Transplantation. 1995 Feb 27;59(4):621–625. [PubMed] [Google Scholar]
- Ku Y., Fukumoto T., Nishida T., Tominaga M., Maeda I., Kitagawa T., Takao S., Shiotani M., Tseng A., Kuroda Y. Evidence that portal vein decompression improves survival of canine quarter orthotopic liver transplantation. Transplantation. 1995 May 27;59(10):1388–1392. doi: 10.1097/00007890-199505270-00005. [DOI] [PubMed] [Google Scholar]
- Lake J. R. Changing indications for liver transplantation. Gastroenterol Clin North Am. 1993 Jun;22(2):213–229. [PubMed] [Google Scholar]
- Lo C. M., Gertsch P., Fan S. T. Living unrelated liver transplantation between spouses for fulminant hepatic failure. Br J Surg. 1995 Aug;82(8):1037–1037. doi: 10.1002/bjs.1800820811. [DOI] [PubMed] [Google Scholar]
- Mori K., Nagata I., Yamagata S., Sasaki H., Nishizawa F., Takada Y., Moriyasu F., Tanaka K., Yamaoka Y., Kumada K. The introduction of microvascular surgery to hepatic artery reconstruction in living-donor liver transplantation--its surgical advantages compared with conventional procedures. Transplantation. 1992 Aug;54(2):263–268. doi: 10.1097/00007890-199208000-00014. [DOI] [PubMed] [Google Scholar]
- Renz J. F., Mudge C. L., Heyman M. B., Tomlanovich S., Kingsford R. P., Moore B. J., Snyder J. D., Perr H. A., Paschal A. L., Roberts J. P. Donor selection limits use of living-related liver transplantation. Hepatology. 1995 Oct;22(4 Pt 1):1122–1126. doi: 10.1016/0270-9139(95)90618-5. [DOI] [PubMed] [Google Scholar]
- Shiraishi M., Csete M. E., Yasunaga C., Drazan K. E., Jurim O., Cramer D. V., Busuttil R. W., Shaked A. Regeneration-induced accelerated rejection in reduced-size liver grafts. Transplantation. 1994 Feb;57(3):336–340. doi: 10.1097/00007890-199402150-00004. [DOI] [PubMed] [Google Scholar]
- Singer P. A., Siegler M., Whitington P. F., Lantos J. D., Emond J. C., Thistlethwaite J. R., Broelsch C. E. Ethics of liver transplantation with living donors. N Engl J Med. 1989 Aug 31;321(9):620–622. doi: 10.1056/NEJM198908313210919. [DOI] [PubMed] [Google Scholar]
- Starzl T. E., Fung J., Tzakis A., Todo S., Demetris A. J., Marino I. R., Doyle H., Zeevi A., Warty V., Michaels M. Baboon-to-human liver transplantation. Lancet. 1993 Jan 9;341(8837):65–71. doi: 10.1016/0140-6736(93)92553-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasberg S. M., Howard T. K., Molmenti E. P., Hertl M. Selecting the donor liver: risk factors for poor function after orthotopic liver transplantation. Hepatology. 1994 Oct;20(4 Pt 1):829–838. doi: 10.1002/hep.1840200410. [DOI] [PubMed] [Google Scholar]
- Terpstra O. T., Schalm S. W., Weimar W., Willemse P. J., Baumgartner D., Groenland T. H., ten Kate F. W., Porte R. J., de Rave S., Reuvers C. B. Auxiliary partial liver transplantation for end-stage chronic liver disease. N Engl J Med. 1988 Dec 8;319(23):1507–1511. doi: 10.1056/NEJM198812083192303. [DOI] [PubMed] [Google Scholar]
- Urata K., Kawasaki S., Matsunami H., Hashikura Y., Ikegami T., Ishizone S., Momose Y., Komiyama A., Makuuchi M. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995 May;21(5):1317–1321. [PubMed] [Google Scholar]
- Van Thiel D. H., Gavaler J. S., Kam I., Francavilla A., Polimeno L., Schade R. R., Smith J., Diven W., Penkrot R. J., Starzl T. E. Rapid growth of an intact human liver transplanted into a recipient larger than the donor. Gastroenterology. 1987 Dec;93(6):1414–1419. doi: 10.1016/0016-5085(87)90274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitington P. F., Emond J. C., Heffron T., Thistlethwaite J. R. Orthotopic auxiliary liver transplantation for Crigler-Najjar syndrome type 1. Lancet. 1993 Sep 25;342(8874):779–780. doi: 10.1016/0140-6736(93)91543-u. [DOI] [PubMed] [Google Scholar]
- Xia R., Emond J. C. Orthotopic partial liver transplantation in the rat: a model of 70% hepatectomy and reduced size liver transplantation. Transplantation. 1993 Oct;56(4):1041–1043. [PubMed] [Google Scholar]