Summary
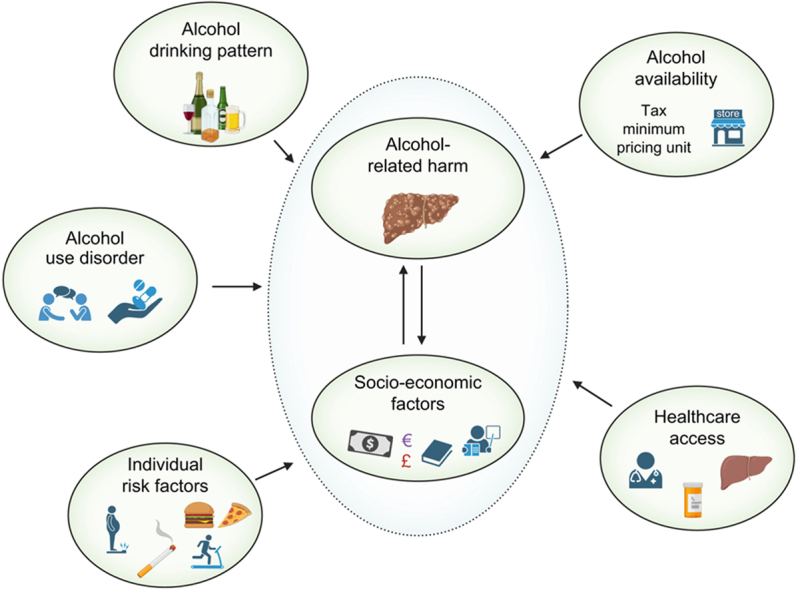
The alcohol-harm paradox (AHP) refers to the fact that people from lower socioeconomic groups experience higher rates of alcohol-related illness despite consuming the same or even lower amounts of alcohol than their more affluent counterparts. While differences in drinking patterns and associations with other risky behaviours partially explain the paradox, they do not fully account for the disparities in morbidity and mortality across socioeconomic groups. The existence of an alcohol-harm paradox in liver disease has been demonstrated in many countries worldwide. Recently, the COVID-19 pandemic further exacerbated these differences and led to an increase in alcohol intake and alcohol-related mortality among racial and ethnic minorities in the United States. Approaches to limit alcohol sales, through introduction of minimum unit pricing or taxation, have led to reductions in alcohol-related liver disease, particularly in socioeconomically deprived areas. Disparities in access to treatment of alcohol use disorder, liver disease and liver transplantation further contribute to the AHP. This review focuses on the AHP, its impact on liver disease and the multi-level strategy that will be required to curb this phenomenon.
Keywords: Alcohol, Inequalities, Public Health, Liver disease
Graphical abstract
Keypoints.
-
•
The phenomenon that lower socioeconomic groups experience higher rates of alcohol-related illness despite consuming the same or even lower amounts of alcohol than their more affluent counterparts is called the “alcohol-harm paradox” (AHP).
-
•
The AHP and its impact on liver disease has been demonstrated in many European and American countries.
-
•
Differences in alcohol drinking pattern and association with other risky health behaviours partially explain the AHP.
-
•
Inconsistent access to treatment for alcohol use disorder, liver disease, and liver transplantation further contribute to the AHP.
-
•
Strategies to limit alcohol sales through minimum unit pricing or taxation, or reduce the density of alcohol outlets, have proven effective to reduce hospitalization and death due to alcohol, particularly in socioeconomically deprived areas.
Definition of alcohol-harm paradox and its potential causes
Alcohol intake is widely known to negatively affect physical and mental health, as well as social well-being. Increased consumption is associated with unemployment, financial instability, depression, medical comorbidities, and higher mortality rates.1 Rising health inequality among socioeconomic groups presents growing challenges for individuals living in poverty, leading to poorer health outcomes and increased healthcare costs.2 Poverty has also been shown to increase the likelihood of alcohol-related illness in multiple countries, demonstrating the universality of this social issue.3 The “alcohol-harm paradox” (AHP), which is the phenomenon that lower socioeconomic groups experience higher rates of alcohol-related illness despite consuming the same or even lower amounts of alcohol than their more affluent counterparts, describes an under-recognised aspect of our understanding of alcohol use.4,5 This phenomenon has been extensively described in the United Kingdom, other European countries, as well as in Australia, New Zealand, North America, and Latin America.6 In the United States, a similar and likely related paradox seems to exist along ethnic/racial lines, with people from African American and Hispanic/Latino origins experiencing more alcohol-related harm, even after adjusting for alcohol consumption and demographic characteristics.7 The term “paradox” is somewhat controversial, as it may not be contradictory or entirely unexpected for patients at higher socioeconomic risk to experience escalating adverse health consequences. However, it is notable that the uneven burden of alcohol-related hospitalisation and mortality according to socio-economic level only seemed to arise in the last few decades.6 Prior to 1980, studies found that excess mortality from alcohol consumption was proportional to the amount of alcohol intake, regardless of social class or educational level.8,9
Potential causes of the alcohol-harm paradox
Under-reporting actual alcohol consumption and frequency has been suggested as a possible explanation for the AHP, possibly due to methodological issues with alcohol consumption recording or missing data from certain groups, such as people experiencing homelessness.10 However, there is still debate as to whether more deprived or more affluent groups tend to underreport alcohol use.4,11 Diagnostic coding bias may also play a role, as alcohol use can be underestimated or misclassified by providers in a differential manner. This may lead to underrepresentation of alcohol use disorder (AUD) and alcohol-related liver disease (ALD) among more privileged individuals, with liver disease potentially attributed to non-alcohol-related causes. In epidemiologic research, cases of ALD are often identified by codes for ALD or alcohol-associated hepatitis, or the combination of cirrhosis and AUD.12 Studies have shown significant misclassification of AUD and ALD: >30% of AUD diagnoses may be missed using ICD coding, and >65% of patients classified as having non-alcohol-related cirrhosis have documented histories of heavy alcohol use.13,14
Differences in drinking patterns rather than weekly amount of alcohol have also been implicated, with people from lower socio-economic status engaging in less frequent but heavier episodic drinking than their more privileged counterparts.4,[15], [16], [17], [18] Binge drinking affects the liver more acutely than gradually paced alcohol intake, increasing the risk of alcohol intoxication, alcohol-associated hepatitis, and liver failure.3,19 These differences in binge-drinking patterns could explain up to 25% of the socioeconomic inequalities in alcohol-related health problems in some countries.3,20,21 Alcohol consumption without food intake can also lead to a higher incidence of cirrhosis.22 Whether this plays into the AHP is understudied. Yet, there is some evidence that people from low socio-economic status tend to drink more often without meals23 and that the protective effect of drinking with food on all-cause mortality is mostly apparent in people with socioeconomic risk factors.24 Additionally, the choice of alcoholic beverage may factor into the AHP. Deprived individuals are more likely to drink beer and spirits,4 while more affluent individuals tend to drink wine, which may be associated with cardioprotective qualities.[25], [26], [27]
Several studies have reported the importance of the association with other risky health-related behaviours among people with lower educational and social levels. Indeed, they are more likely to be overweight, smoke, and/or have a poor diet and exercise routine,4 which, taken together, potentially makes them more vulnerable to alcohol-related harm. Studies in Sweden and Finland found no interaction between BMI and low income, and adjusting for physical inactivity and high BMI did not reduce the socio-economic difference in all-cause20 or alcohol-related11 mortality. On the other hand, the interaction between low income and smoking led to 11.4 extra deaths per 10,000 person-years in Finland.11 An English survey found the association with smoking, higher BMI and poor diet and exercise to be stronger in deprived individuals consuming what they called “increased risk levels” of alcohol (>168–400 g/week in males, >112–280 g/week in females) compared to higher risk drinkers (>400 g/week in males, >280 g/week in females).4 The updated nomenclature for steatotic liver disease (SLD) recognises the contributions of cardiometabolic risk factors to the liver disease, categorising patients with hepatic steatosis into metabolic dysfunction-associated steatotic liver disease (MASLD), ALD, and MetALD based on their reported alcohol consumption.28 Cardiometabolic risk factors, which include hypertension, hyperlipidaemia, diabetes, and obesity, are more common in socioeconomically disadvantaged populations.29,30 In the United States, the burden of unfavourable social determinants of health (SDOH) has been disproportionately found in those with ALD-predominant MetALD and ALD, with higher rates of food insecurity, limited healthcare access, and single living (not married nor living with a partner), relative to those with MASLD.31 In this study, the association of Hispanic ethnicity with SLD was attributable not only to metabolic risk factors and alcohol use but also to social factors including cumulative SDOH and foreign-born status. These findings suggest a negative synergistic contribution of these risk factors to the perceived AHP.
Furthermore, limited access to primary healthcare providers, specialty care, and mental health resources – due to associated costs – can increase the risk of disease progression, including of alcohol-related conditions.32 Treatment of ALD inherently requires treatment of the underlying AUD, yet access to these resources can be unreliable. Gender and racial/ethnic differences in access to treatment for AUD have been described, and admission to treatment is dependent on a variety of factors including sociodemographic characteristics, cultural expectations, time, transportation, social supports, and the availability of services.[33], [34], [35], [36] In the United States, Black patients seeking addiction treatment commonly report experiencing racial discrimination in the medical setting, which may lead to mistrust and decrease help-seeking.37 Similarly, Black patients are less likely than White or Hispanic patients to receive pharmacotherapy for AUDs.38 In addition, higher geographic density of gastroenterologists has been associated with lower ALD mortality, with physician-dependent variables influencing access to liver transplantation, yet there remains significant regional variability in the availability of such subspecialty care.39,40 In this context, delayed presentations or referrals may also contribute to the observation that patients of lower socioeconomic status experience a higher burden of symptomatic disease.
Finally, more severe alcohol-consuming behaviour can lead to unemployment and adverse socioeconomic circumstances, and could thus contribute to the AHP via reverse causation.6,20,41 Indeed, a causal risk pathway of socioeconomic deprivation leading to increased risk of aversive experience or trauma, followed by internalized symptoms, drinking to cope, and alcohol dependence, has been described.42
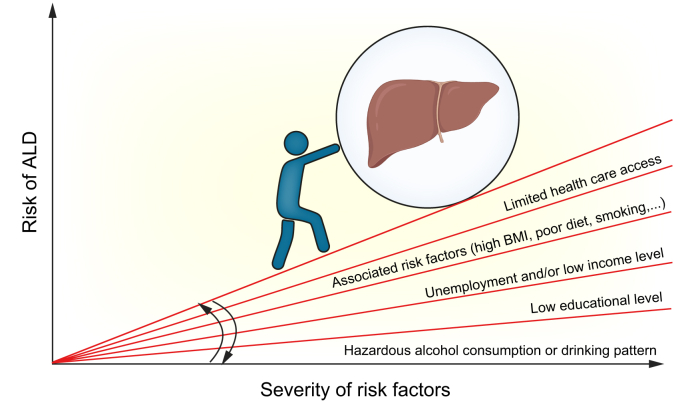
These various factors likely contribute to this paradox but may not fully explain the difference in alcohol-related morbidity and mortality observed between people from different socio-economic backgrounds. Indeed, one study found that after adjusting for alcohol intake and other risky health behaviours such as smoking and high BMI, socioeconomically disadvantaged populations still experienced a three-fold increase in alcohol-related harm compared to people with more privileged status.5 It is also worth noting that the association of deprivation with alcohol-related harm seems stronger in males than in females.10,43,44 Overall, most studies aiming to understand the AHP have focused on individualised behavioural causes, rather than the systemic social, economic and health inequalities that also deserve attention (Fig. 1).
Fig. 1.
Health gradient in alcohol-related liver disease.
The illustration is conceptual and the thickness of each layer does not reflect the weight of the associated factor.
Alcohol-harm paradox in liver disease
Alcohol has detrimental effects on health and increases the risks of depression, cardiovascular disease, cancer, and liver disease, which can be debilitating and life-threatening. ALD is a primary preventable cause of morbidity and mortality worldwide, encompassing a spectrum of disorders that include hepatic steatosis, alcohol-associated hepatitis, and alcohol-associated cirrhosis. SLD due to alcohol can be exacerbated by additional factors, including diet and exercise, obesity, metabolic diseases, genetics (e.g. PNPLA3 mutations) and medications.45 Approximately 10-20% of people with AUD develop hepatitis or cirrhosis, and alcohol contributes to half of all cases of cirrhosis worldwide. Mortality from ALD, particularly alcohol-related cirrhosis, typically correlates directly with per capita alcohol consumption and income inequality.46,47
Rates of ALD, as well as morbidity and mortality, vary by region and country. In the United Kingdom, an overall trend from drinking beers to stronger wines and spirits was correlated with a fourfold increase in mortality from chronic liver disease. Conversely, declines in overall alcohol consumption in France, Italy, Spain, and the Baltic countries were followed by falls in cirrhosis-related mortality.48
Europe has the highest annual per capita alcohol consumption rate in the world, with Eastern Europe leading at 15.7 L per person. Rates of ALD in Europe have been declining, down to 3.0% by 2023, partly due to declining alcohol consumption.49 This trend is especially evident in Eastern Europe, where minimum unit pricing and increased tax on alcoholic products in Baltic countries (Estonia, Latvia, and Lithuania) have reduced alcohol purchases.[50], [51], [52]
Asian countries such as China, India, South Korea, and Japan have slightly lower per capita alcohol consumption, ranging from 4.3 to 12.3 L per person, yet still experience high rates of deaths due to cirrhosis and disability-adjusted life years attributable to alcohol consumption (456.1 per 100,000), following the broader Asian region.47 Rising rates of ALD-related mortality in Asia may be linked to several factors. Asian individuals are genetically predisposed to elevated acetaldehyde exposure, owing to variants in alcohol dehydrogenase, making them more susceptible to alcohol-related liver injury. From an epidemiological perspective, higher rates of comorbid viral hepatitis B infection along with ALD may contribute to higher rates of liver-related death. Additionally, growing economies such as China and India have shown rapid increases in per capita alcohol consumption.47
Global impact
Most studies on the AHP have looked at non-liver-specific outcomes such as all-cause mortality or acute and chronic alcohol-related harm. Yet, specific evidence of the AHP and its impact on liver health has been demonstrated across multiple geographic settings, including the Americas and Europe3 (Table 1). In Europe, a socio-economic gradient was identified for most alcohol-associated hospital admissions in England2 and for new diagnoses of ALD in Denmark.53 In 2015, higher rates of alcohol-related mortality were found among lower educational and occupational groups in 17 European countries,54 with the greatest disparities observed in Eastern Europe, Finland and Denmark. Interestingly, based on the WHO mortality database, Finland and Denmark also have the lowest proportions of unrecorded aetiology of liver disease using ICD coding: 9% in Finland compared to 62% in Italy.55 It is thus conceivable that socioeconomic disparities in alcohol-related mortalities in other European countries may be missed by ICD coding misclassification.
Table 1.
Alcohol-harm paradox in liver-related studies.
| Authors | Region | Study design | Main findings |
|---|---|---|---|
| Europe | |||
| Petrovski et al., 201189,90 | Eastern Europe (Hungary) | Case control study |
|
| Sadler et al., 20172 | United Kingdom (England) | Use of national health service hospital admissions (2010 – 2013) |
|
| Askgaard et al., 202153 | Northern Europe (Denmark) | Use of national registries (2009 – 2018) |
|
| Latin America | |||
| Arab et al., 202056 | Latin America | Regional Health Reports |
|
| Oneto et al., 202191 | Latin America (Chile) | National health survey (2016 -2017) |
|
| North America | |||
| Major et al., 201464 | North America (USA) | NIH American Association of Retired Persons Health study |
|
| Case and Deaton, 201792 | North America (USA) | National surveys |
|
| Damjanovska et al., 202393 | North America (USA) | Electronic records from health care systems (1999 - 2021) |
|
| Ayares et al., 202494 | North America (USA) | National databases (2011 – 2018) |
|
ALD, alcohol-related liver disease; HR, hazard ratio; OR, odds ratio.
Higher mortality due to alcohol-related cirrhosis was also reported in lower-income countries across Latin America.56 In Brazil, where the most popular alcoholic drink is cachaça (with 40% alcohol by volume) and heavy alcohol consumption costs less than a 2,000 kcal/day staple diet, lower education levels were correlated with higher risk of alcohol-related illness.57,58
In the United States, alcohol use has disproportionately affected communities of lower income. Alcohol outlets cluster in urban areas with higher levels of poverty and a higher proportion of ethnic minorities59,60 – particularly in neighbourhoods with histories of redlining, a discriminatory practice related to financial resources that created geographically deprived areas where health inequities persist today.[61], [62], [63] Increased neighbourhood alcohol outlet density has been associated with adverse alcohol-related health outcomes including liver problems, likely contributing to the differences observed in liver-related mortality by socioeconomic status.64,65
Impact of COVID-19
In the United States, the COVID-19 pandemic significantly impacted racial and ethnic minorities, immigrants, homeless individuals, inmates, and essential workers who often lived in tight and overpopulated housing units, high-density neighbourhoods, or areas with limited access to healthcare.66 These communities that were hit hardest by COVID-19 also experienced surges in alcohol purchases and alcohol use,67 partly because of social isolation and stay-at-home orders to “flatten the curve” and contain the pandemic – policies that led to disruptions in school and work, and higher rates of depression and anxiety.[68], [69], [70], [71] Overall alcohol intake rose significantly during this period, with national sales increasing by up to 54% and online sales surging by 262%.72,73 Admissions for alcohol-associated hepatitis increased and were linked to higher mortality, indicating more severe disease than previously observed.74 The number of liver transplants for alcohol-associated hepatitis increased by more than 50%, and ALD-related mortality increased by 20%, more so among Black and Hispanic communities.75 Outside of the United States, data suggest that mortality rates from chronic liver disease in other countries were less affected by the pandemic.76,77
Potential approaches to tackle the alcohol-harm paradox in liver disease
Alcohol sales have been closely linked to the burden of ALD. In 2018, a minimum unit pricing was introduced in Scotland on alcohol drinks sold to the public. The minimum unit pricing sets a legal minimum price below which alcohol cannot be sold.78 Over a period of 3 years, this legislation led to a reduction of alcohol sales by 3%, which translated into reductions of hospitalisation and death attributable to alcohol of 4.1% and 13.4%, respectively. This was also associated with a significant reduction in ALD, with the greatest impact observed in the 40% most socioeconomically deprived areas.78 This impact of the minimum pricing unit on alcohol-related hospitalisation and inequalities is consistent with what modelling studies or natural experiments conducted in Canada and the United Kingdom have observed.79 Increased taxation of alcoholic beverages has also been implemented in several countries; such policies in Estonia, Latvia, and Lithuania have successfully curbed alcohol sales with reductions in all-cause and alcohol-attributable mortality.[50], [51], [52] By contrast, less restrictive alcohol policies in Poland were associated with higher rates of liver-related mortality.51 Some may view these strategies as a “tax on the poor,” as its impact is felt disproportionately by the poor; however, proponents suggest that this group experiences the most alcohol-related harms and that this is why such policies are effective.[80], [81], [82]
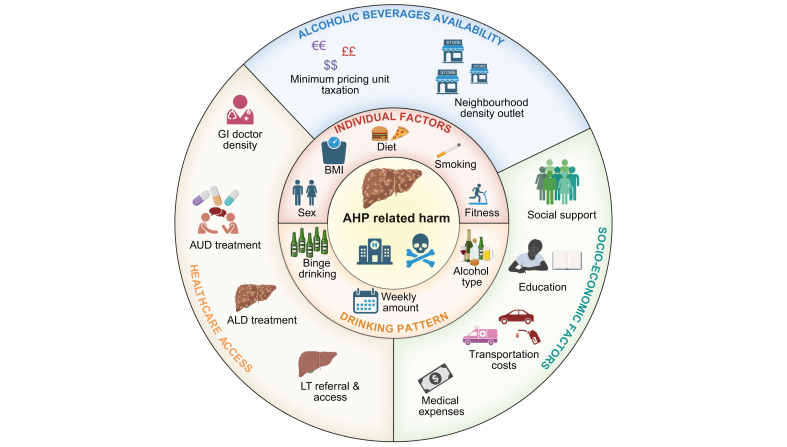
Other public health policies could help reduce the AHP, such as limiting access to alcohol by reducing the density of alcohol outlets. Interventions to address the co-morbid and compound risk of cardiometabolic risk factors on the development and progression of ALD may include taxes (e.g. soda tax), calorie labels on fast foods, restrictions on the sale of ultra-processed foods, and programmes aimed at reducing obesity and tobacco use. Population-level screening targeting at-risk populations can detect hazardous alcohol use and facilitate timely intervention to prevent adverse health consequences. Improved access to healthcare, including treatment for AUD, liver disease care and liver transplantation, would also help to address disparities in liver-related health outcomes arising from the AHP (Fig. 2).
Fig. 2.
Multiple factors involved in the alcohol-harm paradox.
AHP, alcohol-harm paradox; ALD, alcohol-related liver disease; AUD, alcohol use disorder; LT, liver transplantation.
Impact of the alcohol-harm paradox on liver transplantation
Severe ALD, including alcohol-associated hepatitis and decompensated cirrhosis, is associated with high mortality. In such cases, liver transplantation is often the only curative treatment option. Transplantation rates have historically been lower in individuals from lower socioeconomic groups, in part due to disparities seen in social support, access to health insurance, and education. These patients may find it more difficult to meet the strict selection criteria for liver transplantation, with lower health literacy, fewer social supports, and reduced access to consistent healthcare or health insurance, and may be disadvantaged when assessed on usual selection criteria, contributing to inequities in access to liver transplant.83 This population also encounters upstream barriers to being considered for or referred to a liver transplant programme.84,85 Increased area deprivation has been correlated with worse outcomes in decompensated cirrhosis, transplant waitlisting, and all-cause mortality. Factors such as lower income, lower levels of education, poor household conditions, and decreased social support are linked to a lower likelihood of being waitlisted for transplant and reduced survival.85 There are relatively few contemporary studies investigating how SDOH may influence post-transplant disparities in outcome, but low annual income and limited literacy have been associated with post-transplant non-adherence.86,87
Summary
In conclusion, tackling the AHP will require a multi-level strategy (Table 2). Individual behavioural measures aiming to reduce the prevalence or frequency of episodic heavy drinking have been shown to be effective. Understanding patterns of health and disease should integrate biologic and social factors.88 In order to be effective and achieve equity in health outcomes, interventions will need to take into account the socioeconomic context and provide additional supports to at-risk groups. Future studies should focus on deepening our understanding of the mechanisms driving the AHP to address these complex and intricate eco-social factors.
Table 2.
Causes and potential solutions to improve liver-related outcomes related to the alcohol-harm paradox.
| Influences of liver health on the AHP | Causes | Possible remedies |
|---|---|---|
| Alcohol consumption patterns |
|
Strengthen alcohol policy
|
| Education |
|
Reduce stigma and enhance awareness
|
| Healthcare access |
|
Improve access to healthcare
|
| Psychosocial stress and stigmatization |
|
Reduce social determinants of poor health
|
Abbreviations
AHP, alcohol-harm paradox; ALD, alcohol-related liver disease; AUD, alcohol-use disorder; MASLD, metabolic dysfunction-associated steatotic liver disease; SDOH, social determinants of health; SLD, steatotic liver disease.
Financial support
The authors did not receive any financial support to produce this manuscript.
Authors' contributions
LW, AK and CM designed and coordinated the study; LW, JK, and AK wrote the manuscript; LW designed the figures; LW, JK, AK and CM revised and finalized the manuscript.
Figures were created in BioRender. Weichselbaum, L. (2025).
Conflict of interest
Laura Weichselbaum: no conflict of interest; Judah Kupferman: no conflict of interest; Allison Kwong: National Institute on Alcohol Abuse and Alcoholism (K23AA029197, Kwong); Christophe Moreno: Gilead, Roche, Ipsen, Echosens, Julius Clinical, Abbvie, Advarra.
Please refer to the accompanying ICMJE disclosure forms for further details.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhepr.2025.101480.
Supplementary data
The following are the Supplementary data to this article:
References
- 1.Angus C., Pryce R., Holmes J., et al. Assessing the contribution of alcohol-specific causes to socio-economic inequalities in mortality in England and Wales 2001-16. Addiction. 2020;115:2268–2279. doi: 10.1111/add.15037. 20200331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadler S., Angus C., Gavens L., et al. Understanding the alcohol harm paradox: an analysis of sex- and condition-specific hospital admissions by socio-economic group for alcohol-associated conditions in England. Addiction. 2017;112:808–817. doi: 10.1111/add.13726. 20170206. [DOI] [PubMed] [Google Scholar]
- 3.Probst C., Kilian C., Sanchez S., et al. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health. 2020;5:e324–e332. doi: 10.1016/S2468-2667(20)30052-9. [DOI] [PubMed] [Google Scholar]
- 4.Bellis M.A., Hughes K., Nicholls J., et al. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16:111. doi: 10.1186/s12889-016-2766-x. 20160218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katikireddi S.V., Whitley E., Lewsey J., et al. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health. 2017;2:e267–e276. doi: 10.1016/S2468-2667(17)30078-6. 20170510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyd J., Sexton O., Angus C., et al. Causal mechanisms proposed for the alcohol harm paradox-a systematic review. Addiction. 2022;117:33–56. doi: 10.1111/add.15567. 20210525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mulia N., Ye Y., Greenfield T.K., et al. Disparities in alcohol-related problems among white, black, and Hispanic Americans. Alcohol Clin Exp Res. 2009;33:654–662. doi: 10.1111/j.1530-0277.2008.00880.x. 20090115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edwards G., Kyle E., Nicholls P., et al. Alcoholism and correlates of mortality. Implications for epidemiology. J Stud Alcohol. 1978;39:1607–1617. doi: 10.15288/jsa.1978.39.1607. [DOI] [PubMed] [Google Scholar]
- 9.Rossow I., Amundsen A. The disadvantage of being advantaged?--on a social gradient in excess mortality among alcohol abusers. Addiction. 1996;91:1821–1829. [PubMed] [Google Scholar]
- 10.Smith K.F.J. 2014. Health Inequalities and the Harm Paradox: why some groups face greater problems despite consuming less alcohol.https://iogt.org/wp-content/uploads/2015/03/IAS-report-Alcohol-andhealth-inequalities-FULL.pdf A summary of the available evidence., Available at: [Google Scholar]
- 11.Pena S., Makela P., Laatikainen T., et al. Joint effects of alcohol use, smoking and body mass index as an explanation for the alcohol harm paradox: causal mediation analysis of eight cohort studies. Addiction. 2021;116:2220–2230. doi: 10.1111/add.15395. 20210128. [DOI] [PubMed] [Google Scholar]
- 12.Swain L.A., Godley J., Brahmania M., et al. Validating new coding algorithms to improve identification of alcohol-associated and nonalcohol-associated cirrhosis hospitalizations in administrative databases. Hepatol Commun. 2024;8 doi: 10.1097/HC9.0000000000000469. 20240619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mercurio L., Garcia A., Ruest S., et al. One third of alcohol use disorder diagnoses are missed by ICD coding. Subst Use Addctn J. 2025;46:328–336. doi: 10.1177/29767342241288112. 20241107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vestberg K., Thulstrup A.M., Sorensen H.T., et al. Data quality of administratively collected hospital discharge data for liver cirrhosis epidemiology. J Med Syst. 1997;21:11–20. doi: 10.1023/a:1022835207287. [DOI] [PubMed] [Google Scholar]
- 15.Fone D.L., Farewell D.M., White J., et al. Socioeconomic patterning of excess alcohol consumption and binge drinking: a cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002337. 20130415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewer D., Meier P., Beard E., et al. Unravelling the alcohol harm paradox: a population-based study of social gradients across very heavy drinking thresholds. BMC Public Health. 2016;16:599. doi: 10.1186/s12889-016-3265-9. 20160719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nandi A., Glymour M.M., Subramanian S.V. Association among socioeconomic status, health behaviors, and all-cause mortality in the United States. Epidemiology. 2014;25:170–177. doi: 10.1097/EDE.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 18.Giskes K., Turrell G., Bentley R., et al. Individual and household-level socioeconomic position is associated with harmful alcohol consumption behaviours among adults. Aust N Z J Public Health. 2011;35:270–277. doi: 10.1111/j.1753-6405.2011.00683.x. 20110307. [DOI] [PubMed] [Google Scholar]
- 19.Britton A., McKee M. The relation between alcohol and cardiovascular disease in Eastern Europe: explaining the paradox. J Epidemiol Community Health. 2000;54:328–332. doi: 10.1136/jech.54.5.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Syden L., Landberg J. The contribution of alcohol use and other lifestyle factors to socioeconomic differences in all-cause mortality in a Swedish cohort. Drug Alcohol Rev. 2017;36:691–700. doi: 10.1111/dar.12472. 20161105. [DOI] [PubMed] [Google Scholar]
- 21.Bloomfield K., Grittner U., Kramer S., et al. Social inequalities in alcohol consumption and alcohol-related problems in the study countries of the EU concerted action 'Gender, Culture and Alcohol Problems: a Multi-national Study'. Alcohol Alcohol Suppl. 2006;41:i26–i36. doi: 10.1093/alcalc/agl073. [DOI] [PubMed] [Google Scholar]
- 22.Simpson R.F., Hermon C., Liu B., et al. Alcohol drinking patterns and liver cirrhosis risk: analysis of the prospective UK Million Women Study. Lancet Public Health. 2019;4:e41–e48. doi: 10.1016/S2468-2667(18)30230-5. 20181122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warde A., Sasso A., Holmes J., et al. Situated drinking: the association between eating and alcohol consumption in Great Britain. Nordisk Alkohol Nark. 2023;40:301–318. doi: 10.1177/14550725231157222. 20230221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ortola R., Sotos-Prieto M., Garcia-Esquinas E., et al. Alcohol consumption patterns and mortality among older adults with health-related or socioeconomic risk factors. JAMA Netw Open. 2024;7 doi: 10.1001/jamanetworkopen.2024.24495. 20240801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haseeb S., Alexander B., Baranchuk A. Wine and cardiovascular health: a comprehensive review. Circulation. 2017;136:1434–1448. doi: 10.1161/CIRCULATIONAHA.117.030387. [DOI] [PubMed] [Google Scholar]
- 26.Rimm E.B., Klatsky A., Grobbee D., et al. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ. 1996;312:731–736. doi: 10.1136/bmj.312.7033.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.St Leger A.S., Cochrane A.L., Moore F. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. Lancet. 1979;1:1017–1020. doi: 10.1016/s0140-6736(79)92765-x. [DOI] [PubMed] [Google Scholar]
- 28.Rinella M.E., Lazarus J.V., Ratziu V., et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology. 2023;78:1966–1986. doi: 10.1097/HEP.0000000000000520. 20230624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark A.M., DesMeules M., Luo W., et al. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6:712–722. doi: 10.1038/nrcardio.2009.163. 20090922. [DOI] [PubMed] [Google Scholar]
- 30.Stringhini S., Carmeli C., Jokela M., et al. Socioeconomic status and the 25 x 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389:1229–1237. doi: 10.1016/S0140-6736(16)32380-7. 20170201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ochoa-Allemant P., Marrero J.A., Serper M. Racial and ethnic differences and the role of unfavorable social determinants of health across steatotic liver disease subtypes in the United States. Hepatol Commun. 2023;7 doi: 10.1097/HC9.0000000000000324. 20231201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Probst C., Roerecke M., Behrendt S., et al. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 2014;43:1314–1327. doi: 10.1093/ije/dyu043. 20140311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mellinger J.L., Fernandez A., Shedden K., et al. Gender disparities in alcohol use disorder treatment among privately insured patients with alcohol-associated cirrhosis. Alcohol Clin Exp Res. 2019;43:334–341. doi: 10.1111/acer.13944. 20190122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mulia N., Tam T.W., Schmidt L.A. Disparities in the use and quality of alcohol treatment services and some proposed solutions to narrow the gap. Psychiatr Serv. 2014;65:626–633. doi: 10.1176/appi.ps.201300188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sedarous M., Flemming J.A. Culture, stigma, and inequities creating barriers in alcohol use disorder management in alcohol-associated liver disease. Clin Liver Dis (Hoboken) 2023;21:130–133. doi: 10.1097/CLD.0000000000000026. 20230320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vaeth P.A., Wang-Schweig M., Caetano R. Drinking, alcohol use disorder, and treatment access and utilization among U.S. Racial/ethnic groups. Alcohol Clin Exp Res. 2017;41:6–19. doi: 10.1111/acer.13285. 20161226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hall O.T., Jordan A., Teater J., et al. Experiences of racial discrimination in the medical setting and associations with medical mistrust and expectations of care among black patients seeking addiction treatment. J Subst Abuse Treat. 2022;133 doi: 10.1016/j.jsat.2021.108551. 20210625. [DOI] [PubMed] [Google Scholar]
- 38.Williams E.C., Gupta S., Rubinsky A.D., et al. Variation in receipt of pharmacotherapy for alcohol use disorders across racial/ethnic groups: a national study in the U.S. Veterans Health Administration. Drug Alcohol Depend. 2017;178:527–533. doi: 10.1016/j.drugalcdep.2017.06.011. 20170711. [DOI] [PubMed] [Google Scholar]
- 39.Lee B.P., Dodge J.L., Terrault N.A. Geographic density of gastroenterologists is associated with decreased mortality from alcohol-associated liver disease. Clin Gastroenterol Hepatol. 2023;21:1542–1551. doi: 10.1016/j.cgh.2022.07.020. e1546. 20220804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loy M., Rzepczynski A., Joyce C., et al. Disparity in transplant referral patterns for alcohol-related liver disease based on physician-dependent variables. Transplant Proc. 2020;52:900–904. doi: 10.1016/j.transproceed.2020.01.015. 20200306. [DOI] [PubMed] [Google Scholar]
- 41.Backhans M.C., Balliu N., Lundin A., et al. Unemployment is a risk factor for hospitalization due to alcohol problems: a longitudinal study based on the Stockholm Public Health Cohort (SPHC) J Stud Alcohol Drugs. 2016;77:936–942. doi: 10.15288/jsad.2016.77.936. [DOI] [PubMed] [Google Scholar]
- 42.Shuai R., Anker J.J., Bravo A.J., et al. Risk pathways contributing to the alcohol harm paradox: socioeconomic deprivation confers susceptibility to alcohol dependence via greater exposure to aversive experience, internalizing symptoms and drinking to cope. Front Behav Neurosci. 2022;16 doi: 10.3389/fnbeh.2022.821693. 20220214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Breakwell C.B.A., Griffiths C., Jackson G., Fegan G., Marshall D. Trends and geographical variations in alcohol-related deaths in the United Kingdom, 1991–2004. Health Stat Q. 2007;33:6–24. Spring. [PubMed] [Google Scholar]
- 44.Strong M., Pearson T., MacNab Y.C., et al. Mapping gender variation in the spatial pattern of alcohol-related mortality: a Bayesian analysis using data from South Yorkshire, United Kingdom. Spat Spatiotemporal Epidemiol. 2012;3:141–149. doi: 10.1016/j.sste.2012.04.007. 20120421. [DOI] [PubMed] [Google Scholar]
- 45.European Association for the Study of the L. European Association for the Study of D and European Association for the Study of O EASL-EASD-EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD) J Hepatol. 2024;81:492–542. doi: 10.1016/j.jhep.2024.04.031. 20240607. [DOI] [PubMed] [Google Scholar]
- 46.Cutright P., Fernquist R.M. Predictors of per capita alcohol consumption and gender-specific liver cirrhosis mortality rates: thirteen European countries, circa 1970-1984 and 1995-2007. Omega (Westport) 2010;62:269–283. doi: 10.2190/om.62.3.d. [DOI] [PubMed] [Google Scholar]
- 47.Liangpunsakul S., Haber P., McCaughan G.W. Alcoholic liver disease in Asia, Europe, and North America. Gastroenterology. 2016;150:1786–1797. doi: 10.1053/j.gastro.2016.02.043. 20160227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pimpin L., Cortez-Pinto H., Negro F., et al. Burden of liver disease in Europe: epidemiology and analysis of risk factors to identify prevention policies. J Hepatol. 2018;69:718–735. doi: 10.1016/j.jhep.2018.05.011. 20180517. [DOI] [PubMed] [Google Scholar]
- 49.Aberg F., Jiang Z.G., Cortez-Pinto H., et al. Alcohol-associated liver disease-Global epidemiology. Hepatology. 2024;80:1307–1322. doi: 10.1097/HEP.0000000000000899. 20240419. [DOI] [PubMed] [Google Scholar]
- 50.Radisauskas R., Stelemekas M., Petkeviciene J., et al. Alcohol-attributable mortality and alcohol control policy in the Baltic Countries and Poland in 2001-2020: an interrupted time-series analysis. Subst Abuse Treat Prev Policy. 2023;18:65. doi: 10.1186/s13011-023-00574-7. 20231109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rehm J., Badaras R., Ferreira-Borges C., et al. Impact of the WHO “best buys” for alcohol policy on consumption and health in the Baltic countries and Poland 2000-2020. Lancet Reg Health Eur. 2023;33 doi: 10.1016/j.lanepe.2023.100704. 20230831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vaitkeviciute J., Gobina I., Janik-Koncewicz K., et al. Alcohol control policies reduce all-cause mortality in Baltic Countries and Poland between 2001 and 2020. Sci Rep. 2023;13:6326. doi: 10.1038/s41598-023-32926-5. 20230418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Askgaard G., Fleming K.M., Crooks C., et al. Socioeconomic inequalities in the incidence of alcohol-related liver disease: a nationwide Danish study. Lancet Reg Health Eur. 2021;8 doi: 10.1016/j.lanepe.2021.100172. 20210713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mackenbach J.P., Kulhanova I., Bopp M., et al. Inequalities in alcohol-related mortality in 17 European countries: a retrospective analysis of mortality registers. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001909. 20151201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sheron N. Alcohol and liver disease in Europe--Simple measures have the potential to prevent tens of thousands of premature deaths. J Hepatol. 2016;64:957–967. doi: 10.1016/j.jhep.2015.11.006. 20151116. [DOI] [PubMed] [Google Scholar]
- 56.Arab J.P., Bataller R., Roblero J.P. Are we really taking care of alcohol-related liver disease in Latin America? Clin Liver Dis (Hoboken) 2020;16:91–95. doi: 10.1002/cld.916. 20200922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nobrega I.C.C., Marques R.V.L., Ferreira M.A., et al. The paradox of alcohol and food affordability: minimal impact of leading beer and cachaca brands on Brazilian household income amid hazardous drinking patterns. Nutrients. 2024;16 doi: 10.3390/nu16101469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oliveira L.M., Demarco F.F., Zanatta F.B. Educational inequalities and alcohol-related consequences in Brazil. Alcohol Alcohol. 2024;59 doi: 10.1093/alcalc/agae030. [DOI] [PubMed] [Google Scholar]
- 59.Berke E.M., Tanski S.E., Demidenko E., et al. Alcohol retail density and demographic predictors of health disparities: a geographic analysis. Am J Public Health. 2010;100:1967–1971. doi: 10.2105/AJPH.2009.170464. 20100819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Romley J.A., Cohen D., Ringel J., et al. Alcohol and environmental justice: the density of liquor stores and bars in urban neighborhoods in the United States. J Stud Alcohol Drugs. 2007;68:48–55. doi: 10.15288/jsad.2007.68.48. [DOI] [PubMed] [Google Scholar]
- 61.Alcoholism NIoAAa Alcohol-related emergencies and deaths in the United States. https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-topics/alcohol-facts-and-statistics/alcohol-related-emergencies-and-deaths-united-states
- 62.Alpert H.R., Slater M.E., Yoon Y.H., et al. Alcohol consumption and 15 causes of fatal injuries: a systematic review and meta-analysis. Am J Prev Med. 2022;63:286–300. doi: 10.1016/j.amepre.2022.03.025. 20220515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Haley S.J., Jardine S.J., Kelvin E.A., et al. Neighborhood alcohol outlet density, historical redlining, and violent crime in NYC 2014-2018. Int J Environ Res Public Health. 2023;20 doi: 10.3390/ijerph20043212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Major J.M., Sargent J.D., Graubard B.I., et al. Local geographic variation in chronic liver disease and hepatocellular carcinoma: contributions of socioeconomic deprivation, alcohol retail outlets, and lifestyle. Ann Epidemiol. 2014;24:104–110. doi: 10.1016/j.annepidem.2013.11.006. 20131121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Theall K.P., Scribner R., Cohen D., et al. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol Alcohol. 2009;44:491–499. doi: 10.1093/alcalc/agp042. 20090810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deutsch-Link S., Curtis B., Singal A.K. Covid-19 and alcohol associated liver disease. Dig Liver Dis. 2022;54:1459–1468. doi: 10.1016/j.dld.2022.07.007. 20220804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen C.Y., Byrne E., Velez T. Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: roles of income level and race. J Fam Issues. 2022;43:719–740. doi: 10.1177/0192513X21994153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chodkiewicz J., Talarowska M., Miniszewska J., et al. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rodriguez L.M., Litt D.M., Stewart S.H. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110 doi: 10.1016/j.addbeh.2020.106532. 20200627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vanderbruggen N., Matthys F., Van Laere S., et al. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur Addict Res. 2020;26:309–315. doi: 10.1159/000510822. 20200922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weerakoon S.M., Jetelina K.K., Knell G. Longer time spent at home during COVID-19 pandemic is associated with binge drinking among US adults. Am J Drug Alcohol Abuse. 2021;47:98–106. doi: 10.1080/00952990.2020.1832508. 20201207. [DOI] [PubMed] [Google Scholar]
- 72.Pollard M.S., Tucker J.S., Green H.D., Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.22942. 20200901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schecke H., Bohn A., Scherbaum N., et al. Alcohol use during COVID-19 pandemic on the long run: findings from a longitudinal study in Germany. BMC Psychol. 2022;10:266. doi: 10.1186/s40359-022-00965-8. 20221114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sohal A., Chaudhry H., Patel J., et al. Impact of COVID-19 pandemic on alcohol-related hepatitis admissions: analysis of nationwide data 2016-2020. Am J Med Sci. 2023;366:209–218. doi: 10.1016/j.amjms.2023.06.002. 20230612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Deutsch-Link S., Jiang Y., Peery A.F., et al. Alcohol-associated liver disease mortality increased from 2017 to 2020 and accelerated during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2022;20:2142–2144. doi: 10.1016/j.cgh.2022.03.017. e2142. 20220319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fedeli U., Barbiellini Amidei C., Casotto V., et al. Mortality from chronic liver disease: recent trends and impact of the COVID-19 pandemic. World J Gastroenterol. 2023;29:4166–4173. doi: 10.3748/wjg.v29.i26.4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Spijker J.J.A., Trias-Llimos S. Cause-specific mortality in Spain during the pandemic: educational differences and its impact on life expectancy. Eur J Public Health. 2023;33:543–549. doi: 10.1093/eurpub/ckad036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wyper G.M.A., Mackay D.F., Fraser C., et al. Evaluating the impact of alcohol minimum unit pricing on deaths and hospitalisations in Scotland: a controlled interrupted time series study. Lancet. 2023;401:1361–1370. doi: 10.1016/S0140-6736(23)00497-X. 20230320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maharaj T., Angus C., Fitzgerald N., et al. Impact of minimum unit pricing on alcohol-related hospital outcomes: systematic review. BMJ Open. 2023;13 doi: 10.1136/bmjopen-2022-065220. 20230203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gibbs N., Angus C., Dixon S., et al. Equity impact of minimum unit pricing of alcohol on household health and finances among rich and poor drinkers in South Africa. BMJ Glob Health. 2022;7 doi: 10.1136/bmjgh-2021-007824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Holmes J., Meng Y., Meier P.S., et al. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet. 2014;383:1655–1664. doi: 10.1016/S0140-6736(13)62417-4. 20140210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sharma A., Sinha K., Vandenberg B. Pricing as a means of controlling alcohol consumption. Br Med Bull. 2017;123:149–158. doi: 10.1093/bmb/ldx020. [DOI] [PubMed] [Google Scholar]
- 83.Deutsch-Link S., Bittermann T., Nephew L., et al. Racial and ethnic disparities in psychosocial evaluation and liver transplant waitlisting. Am J Transplant. 2023;23:776–785. doi: 10.1016/j.ajt.2023.01.011. 20230131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.De Simone P., Germani G., Lai Q., et al. The impact of socioeconomic deprivation on liver transplantation. Front Transplant. 2024;3 doi: 10.3389/frtra.2024.1352220. 20240227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hasjim B.J., Harris A., Balbale S.N., et al. Social disadvantage and disparities in chronic liver disease: a systematic review. Am J Gastroenterol. 2024 doi: 10.14309/ajg.0000000000003171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nephew L.D., Serper M. Racial, gender, and socioeconomic disparities in liver transplantation. Liver Transpl. 2021;27:900–912. doi: 10.1002/lt.25996. [DOI] [PubMed] [Google Scholar]
- 87.Serper M., Patzer R.E., Reese P.P., et al. Medication misuse, nonadherence, and clinical outcomes among liver transplant recipients. Liver Transpl. 2015;21:22–28. doi: 10.1002/lt.24023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39:887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- 89.Jones L., Bates G., McCoy E., et al. Relationship between alcohol-attributable disease and socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health. 2015;15:400. doi: 10.1186/s12889-015-1720-7. 20150418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Petrovski B.E., Szeles G., Melles M., et al. Behaviour does not fully explain the high risk of chronic liver disease in less educated men in Hungary. Eur J Public Health. 2011;21:662–666. doi: 10.1093/eurpub/ckq079. 20100615. [DOI] [PubMed] [Google Scholar]
- 91.Oneto G., Díaz L.A., Idalsoaga F., et al. P-64 the alcohol-associated liver disease paradox in Chile: an assessment with data from the national health survey (Ens 2016-2017) Annals Hepatol. 2021;24 doi: 10.1016/j.aohep.2021.100427. [DOI] [Google Scholar]
- 92.Case A., Deaton A. vol. 2017. Brookings Pap Econ Act; 2017. pp. 397–476. (Mortality and morbidity in the 21(st) century). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Damjanovska S., Karb D.B., Cohen S.M. Increasing prevalence and racial disparity of alcohol-related gastrointestinal and liver disease during the COVID-19 pandemic: a population-based national study. J Clin Gastroenterol. 2023;57:185–188. doi: 10.1097/MCG.0000000000001665. 20230201. [DOI] [PubMed] [Google Scholar]
- 94.Ayares G., Diaz L.A., Fuentes-Lopez E., et al. Racial and ethnic disparities in the natural history of alcohol-associated liver disease in the United States. Liver Int. 2024;44:2822–2833. doi: 10.1111/liv.16023. 20240803. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.