Abstract
Introduction
Autism Spectrum Disorders (ASD) represent a range of neurodevelopmental conditions characterized by abnormal behavioral patterns. ASD is frequently comorbid with other neurodevelopmental disorders. However, there remains a gap in research on the burden of ASD in East and Southeast Asia.
Methods
We stratified the analysis by region, country, age, and sex; used the Sociodemographic Index (SDI) as a pivot to examine the relationship between the burden of autism and SDI through frontier analysis and health inequality analysis; and finally projected global, sex-specific trends in ASD disease burden from 2022 to 2050.
Result
The global burden of ASD, including in East and Southeast Asia, has exhibited a generally increasing trend over recent decades. Japan demonstrated a relatively high ASD burden. The analysis revealed that females tend to experience a higher burden than males, and ASD is more prevalent among younger age groups. A positive correlation was observed between SDI and ASD burden, with higher SDI levels associated with greater burden. Health inequality analyses indicated that while ASD prevalence and Years Lived with Disability (YLDs) are predominantly concentrated in high-SDI countries, incidence rates are higher in low-SDI regions. Finally, the global burden of ASD among both males and females is projected to continue rising through the year 2050.
Conclusion
The burden of ASD in East and Southeast Asia continues to increase year by year. High-SDI countries tend to report a greater disease burden. From 1990 to 2021, nearly all countries in the region experienced a continuous rise in ASD burden. Although there is a growing trend of ASD incidence shifting toward low-SDI countries, prevalence and years lived with disability (YLDs) remain predominantly concentrated in high-SDI countries. Finally, the global burden of ASD among both males and females is projected to continue rising through 2050.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-23904-9.
Keywords: Autism spectrum disorder, Global, East Asia, Southeast Asia, Incidence, Prevalence
Introduction
Autism Spectrum Disorders (ASD) are a group of neurodevelopmental conditions characterized by impairments in social communication and interaction, as well as repetitive behaviors [1]. Their etiology involves a complex interplay of genetic and environmental factors [2]. The defining features of ASD include a consistent inability to initiate and maintain interpersonal relationships and societal communication, accompanied by challenges in social skills, repetitive behaviors, and both verbal and nonverbal modes of interaction [3, 4]. The diverse manifestations of ASD result in overlap with other mental health conditions [5]. Multiple studies have demonstrated a high burden of comorbid psychiatric disorders in individuals with ASD, including attention-deficit/hyperactivity disorder (ADHD), learning disabilities, anxiety disorders, depression, bipolar disorder, schizophrenia, and suicidal behavior disorders—most of which are predominantly observed in younger age groups [6–8]. Furthermore, individuals diagnosed with ASD are more susceptible to medical conditions such as diabetes, lipid metabolism disorders, coronary diseases, intestinal disorders, and orofacial health complications [9–11].
Approximately one in every hundred children worldwide receives an ASD diagnosis, a figure that is projected to grow. Discrepancies within and across various socio-demographic segments are considerable, predominantly due to the distinct ways in which the condition is recognized and defined [12, 13]. In 2019, the age-standardized prevalence of ASD was 369 per 100,000 population, equivalent to approximately 0.37%. It is common for the impacts of ASD to become evident before a child reaches their fifth birthday, with a pronounced divergence in incidence between the sexes—males at 21.6 per 100,000, exceeding females at 6.7 per 100,000 [14].
Although studies on ASD have been increasing annually [15], most of them focus on the global burden and the burden in certain developed regions. There is a lack of analysis on ASD in East Asia and Southeast Asia, which together account for 31% of the world’s population [13, 14, 16–18]. Owing to historical development, there are many structural and cultural parallels between East and Southeast Asia [19]. Therefore, studying the epidemiological characteristics of ASD in East Asia and Southeast Asia is crucial. This study adopts a comprehensive approach to assess the disease trends, health status, health disparities, and future burden projections of ASD across 17 countries and regions in East and Southeast Asia. We conducted a secondary analysis of disease burden metrics from the Global Burden of Disease (GBD) 2021 study, supplemented by frontier and health inequality analyses based on methodologies recommended by the World Health Organization. To project ASD burden trends from 2022 to 2050, we employed an integrated modeling framework using Bayesian Age-Period-Cohort (BAPC) analysis combined with Integrated Nested Laplace Approximation (INLA), enabling efficient Bayesian inference using INLA. The findings provide a comprehensive visualization of the ASD burden across the region and propose country-specific targets for mitigating its impact. Furthermore, the study examines whether disparities in ASD burden are associated with varying levels of Socio-demographic Index (SDI) across countries.
Method
Data source
The GBD database is a project led by the Institute for Health Metrics and Evaluation, while the GBD collaborators cooperate to collect and process the GBD 2021 for seven global super-regions, 21 regions, 204 nations, and 371 diseases, as well as a number of burdens of disease indicators [20]. GBD collaborators process sparse, inconsistent, and heterogeneous data using DisMod-MR tools and a meta-analysis–based integrated estimation approach to quantify disease burden [21]. They then process raw data through denoising, cleaning, and weighting to minimize bias and enhance data quality. This is followed by comprehensive modeling and a series of adjustments, ultimately producing the standardized data available for analysis [22]. All data used in this study were obtained from GBD 2021(https://vizhub.healthdata.org/gbd-results/ and https://ghdx.healthdata.org/gbd-2021).
Statistical analysis
We collected data on the incidence, prevalence, and YLDs of ASD for 17 countries and regions in East and Southeast Asia using the GBD 2021 query tool. The diagnostic criteria and corresponding ICD codes for ASD used in the GBD 2021 study are detailed in Supplement Methods (Appendix 1&2). We measured the trend in ASD burden using the age-standardized incidence rate (ASR, per 100,000 population) and estimated annual percentage change (EAPC). The beta value for EAPC was calculated using linear regression equations [23] (Appendix 3).
We assessed the disparity between the current and potential ASD burden across 17 countries and regions in East and Southeast Asia by employing frontier analysis to calculate SDI-adjusted “effective differences“ [24]. This approach enabled comparison between high-performing countries and regions and their counterparts. The detailed calculation method can be found in Appendix 4.
We applied the World Health Organization’s methodology for health inequality analysis to examine disparities in health status, disease burden, healthcare access, and health outcomes across socioeconomic groups [25]. Two key health inequality metrics were used: the Slope Index of Inequality (SII) and the Concentration Index (CI, a relative inequality measure), which measure absolute and relative inequalities in ASD burden across regions and countries, respectively. The detailed calculation method can be found in Appendix 5.
We developed the predictive model by integrating BAPC analysis with INLA. With GBD data from 1990 to 2021 and GBD 2017–2100 population predictions, the BAPC model was used to calculate the global disease burden of ASD [26]. The detailed calculation method can be found in Appendix 6.
The R program (v4.4.0) was used to carry out all of the aforementioned computations, tables, and charts. SII, CI, and EAPC were all presented with 95% confidence intervals (95% CI).
Results
Global, east asian, southeast asian autism spectrum disorders burden
In 2021, there were 1.14 million ASD incidence cases in global, 81 thousand cases in East Asia, and 85 thousand cases in Southeast Asia. The EAPC for age-standardized incidence rates (ASIR) increased by 0.13% per year globally (95% CI: 0.11–0.14), decreased by 0.05% (95% CI: −0.1 to 0) per year in East Asia, and increased by 0.02% (95% CI: 0.01 to 0.04) per year in Southeast Asia (Supplement Tables 1 and 2).
In 2021, the global prevalence of ASD was 61.8 million, and the age-standardized prevalence rate (ASPR) was 788. In the same year, the number of cases of ASD in East and Southeast Asia was 9.47 million and 4.78 million, respectively. Since 1990, the EAPC for age-standardized prevalence rates (ASPR) has been an annual increase of 0.07% annually globally (95% CI: 0.07–0.08), 0.24% (95% CIs: 0.22 to 0.27) in East Asia, and 0.1% (95% CIs: 0.09 to 0.11) in Southeast Asia (Supplement Tables 1 and 2).
In 2021, a total of 11.5 million Years Lived with Disability (YLDs) were attributed to ASD globally, 1.77 million in East Asia, and 0.9 million in Southeast Asia. Since 1990, the EAPC for age-standardized YLDs rates (ASYR) has increased by 0.08% (95% CIs: 0.08 to 0.09) per year in global, 0.25% (95% CIs: 0.23 to 0.27) per year in East Asia, and 0.12% (95% CIs: 0.11 to 0.13) per year in Southeast Asia (Supplement Tables 1 and 4).
Country level
East Asia, Southeast Asia, and the corresponding nations have ASIRs ranging from 15 to 35 per 100,000 population. China has the lowest ASIR, at 15, and Japan has the greatest, at 35. The highest EAPC was in Thailand (0.34%), and the lowest in Timor-Leste (−0.24%) in ASIR (Fig. 1A and Supplementary Table 2).
Fig. 1.
EAPC in age-standardized incidence (A), prevalence (B), and YLDs rate (C) of ASD per 100,000 population global, East Asia and Southeast Asia, by country, from 1990 to 2021
The ASPR of ASD across East Asia, Southeast Asia, and their respective countries ranges between 1,587 and 647 cases. In line with the ASIR, Japan has the greatest ASPR at 1,587, Indonesia has the lowest at 647 (Supplementary Table 3). Japan has the greatest EAPC at 0.28%, while the Philippines has the lowest at 0.02% (Fig. 1B and Supplementary Table 3).
In 2021, the ASYR varied between 299 and 122 instances per 100,000 people. Japan had the greatest ASYR at 299, and Indonesia had the lowest at 122. Japan had the greatest EAPC in ASYR at 0.28%, Brunei Darussalam had the lowest, at 0.03% (Fig. 1C and Supplementary Table 3).
Gender level
From 1990 to 2021, there were notable differences in the EAPC of ASD between males and females.
In terms of incidence, Thailand had the greatest annual increase in ASD incidence among males, while Japan had the highest annual increase among females. Interestingly, Timor-Leste showed the greatest annual decline in ASD incidence for both sexes (Supplement Fig. 2A).
In terms of prevalence, the ASPR for females decreased annually only in Viet Nam and the Philippines, while it increased annually for both genders in all other countries and regions (Supplement Fig. 2B).
For YLDs, the ASYR for females in North Korea, the Philippines, Malaysia, and Brunei Darussalam remained largely stable over time, whereas it decreased annually for females in Viet Nam. For males, the ASYR increased annually in all countries and regions (Supplement Fig. 2C).
Age level
In 2021, both in East Asia and Southeast Asia, the ASIR and ASYR for ASD were negatively correlated with age, decreasing as age increased. In both East and Southeast Asia, males had a larger burden of ASD than females across all age categories. The majority of people with ASD were under 60 years old (Fig. 2).
Fig. 2.
Total prevalence and number of YLDs, age-standardized prevalence and YLDs rates per 100,000 population of ASD in East Asia (A) and Southeast Asia (B) in 2021 by sex and age; dotted and dashed lines indicate the 95% upper limit, respectively and lower bound uncertainty interval
In East Asia, the majority of ASD prevalence cases and YLDs among those under 60 were concentrated in children and adolescents under the age of 14, as well as middle-aged people aged 30 to 60 years. Figure 2A shows that both the ASPR and ASYR decreased with age.
In Southeast Asia, the number of prevalence cases and YLDs related to ASD decreased with age. There was a greater percentage of females than males under the age of 60. Similarly, ASPR and ASYR decreased with age (Fig. 2B).
Relationships with SDI
ASIR, ASPR, and ASYR showed strong positive correlations with SDI values between 1990 and 2021. East and Southeast Asian nations with higher disease burdens were Japan, South Korea, and Singapore; in contrast, Mongolia had a higher disease burden among medium-SDI nations than other low- and medium-SDI nations but a lower burden than high-SDI nations (Supplement Fig. 2).
Frontier analysis
From 1990 to 2021, we conducted frontier analysis of SDI and age-standardized ASD burden across 17 countries and regions in East and Southeast Asia, revealing a notable trend. As SDI values increased from 0 to 1, the disease burden of ASD showed an upward trajectory (Supplementary Fig. 3).
South Korea, Japan, and Singapore— as high-SDI countries—exhibited the greatest effective differences from the minimum ASD disease burden. This indicates a need for these countries to further optimize their healthcare systems and resource distribution to reduce preventable disease burden and enhance health system efficiency. In contrast, the three low-SDI nations with the least effective differences from the minimum disease burden are Laos, Cambodia, and Timor-Leste (Supplementary Fig. 3).
Health inequalities analysis
This study found that the distribution of the ASD burden varied according to SDI levels and disease burden metrics. In terms of incidence, the burden remained higher in low-SDI countries in both 1990 and 2021, as indicated by persistently negative SII and CI values. However, the CI decreased from − 0.135 to − 0.061, indicating a slight narrowing of inequality over time. Despite this improvement, the burden of disease continues to be disproportionately higher in low-SDI countries. In contrast, prevalence and YLDs were more heavily concentrated in high-SDI countries (Fig. 3). Overall, while inequality in ASD incidence has slightly improved, disparities in prevalence and YLDs have widened, disproportionately impacting high-SDI countries.
Fig. 3.
Socio-Demographic Index inequality regression and concentration curves for the burden of Incidence (A), Prevalence (B), and YLDs (C) due to ASD in the East Asia and South Asia, 1990 and 2021
Global disease burden prediction for autism spectrum disorders
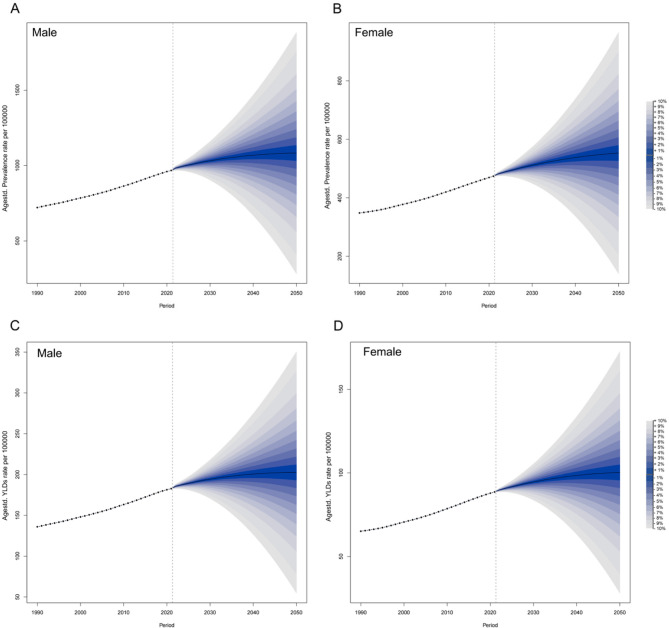
We used the BAPC model, based on GBD data from 1990 to 2021 and GBD population projections, to project the period 2022 to 2050, which revealed that age-standardized prevalence rates and age-standardized YLDs are increasing in both men and women (Fig. 4A-D), and The shaded regions in the diagrams indicate that if prevalence rates or YLDs increase or decrease by 1% per year, the prevalence rates or YLDs are also likely to fluctuate.
Fig. 4.
Observed and predicted trends of ASPR and ASYR of ASD by sex globally from 1990 to 2050 using the BAPC model. A ASYR in males. B ASPR in females. C ASYR in males. D ASYR in females
Discussion
This study utilized data from the GBD 2021 to assess the burden of ASD in East and Southeast Asia, focusing on incidence, prevalence, and YLDs. It examined the potential of different SDI levels to alleviate the burden of ASD, and investigated the association between ASD burden and absolute SDI inequality. Additionally, the study projected the global ASD burden from 2022 to 2050 using predictive modeling.
Consistent with our findings, both ASD incidence and declines in healthy life expectancy increased significantly between 1990 and 2021. Previous studies have also demonstrated that ASD contributes substantially to the number of YLDs [12]. Our study found that Japan had the highest ASD burden among countries in East and Southeast Asia. This may be partly attributed to Japan’s internationally aligned ASD diagnostic standards, which likely reduce underreporting due to misdiagnosis during GBD data collection. In addition, public awareness of ASD is relatively high in Japan, and the country has a well-established healthcare system that enables timely access to diagnostic services and effective treatment options for individuals with ASD [27]. Interestingly, in contrast to Japan, Timor-Leste exhibited a significant decline in ASD burden and reported one of the lowest burdens in the region, despite its low development status. Several factors may contribute to this finding. First, TimorLeste is a relatively young country. Second, postconflict reconstruction has posed challenges, leaving healthcare infrastructure underdeveloped and limiting accurate ASD diagnosis [28]. Third, a severe shortage of trained professionals qualified to diagnose ASD persists. These limitations likely lead to significant underreporting of ASD cases, resulting in an artificially low estimated burden. It is important to note that such challenges are common across many countries in East and Southeast Asia.
Furthermore, the disease burden of ASD varies significantly by gender, with males bearing a notably greater burden than females; these conclusions are in line with prior research [14], and they may be related to variations in hormones, gene expression, and brain structure between both sexes [29, 30]. One study suggested that adolescent females, influenced by hormonal changes and psychological factors, may present with distinct phenotypes, psychiatric comorbidities, and “camouflaging” behaviors, which can contribute to misdiagnosis or delayed diagnosis of ASD [31]. Conversely, another study reported that girls with autism spectrum disorder are more likely than boys to be overlooked during the diagnostic process [32]. According to our findings, in East Asia, the prevalence and YLDs numbers of ASD peaked in the age cohorts of 5 to 9 years, 30 to 34 years, and 50 to 54 years. After those age groups, the numbers essentially declined with age, whereas the ASYR and the ASPR decreased as age increased; however, in Southeast Asia, as people became older, fewer prevalences and YLDs were recorded; this pattern was also observed for age-standardized prevalences and YLDs. These findings highlight the increased need for social, psychosocial, and health care as well as the necessity of screening and intervention before the age of peak prevalence in the child and adolescent population. In East Asia, more focus should be placed on the mental and psychiatric health of the middle-aged population. ASD tends to start in childhood, which leads to a large number of YLDs, a lifelong disorder. These dysfunctions include sleep disturbances, language and communication disorders, social interaction difficulties, and restricted and repetitive behaviors [13, 33, 34].
According to our findings, there is a positive correlation between high Socio-demographic Index (SDI > 0.6) and the incidence, prevalence, and YLDs of ASD in high-SDI regions. Through frontier analysis, it confirms that from 1990 to 2021, the burden of disease for ASD in Loas, Cambodia, and Timor-Leste with low SDI progressively approached the minimum disease burden. For these high-SDI regions, Japan, South Korea, and Singapore tend to have higher ASD disease burdens. From 1990 to 2021, the burden of ASD in East and South Asia appeared to shift toward greater inequality, with increasing SII and CI values across incidence, prevalence, and YLDs. Although the point estimates of the Slope Index of Inequality SII and CI suggest a tendency toward increasing inequality in ASD burden between SDI groups, the 95%CI include zero, indicating that these differences are not statistically significant. Nevertheless, it also can explain the trend of health inequality related to ASD in East and South Asia, where the most pronounced increases in incidence are observed in low-SDI countries, while prevalence and YLDs are more concentrated in high-SDI countries. This may reflect data variability, differences in diagnostic practices, or limitations of GBD estimations, rather than conclusive evidence of inequality. As most countries in East and Southeast Asia are developing nations, they often face greater disparities in the distribution of healthcare resources, wider urban–rural and socioeconomic gaps, a shortage of specialized mental health professionals, and less developed mental health infrastructure [35]. In Southeast Asia, the implementation of mental health services often faces numerous barriers, including distrust in services or external institutions, stigma, a paternalistic cultural framework, and limited resources and infrastructure [36]. These challenges significantly reduce the diagnostic rate of ASD in the region, which may explain the seemingly lower disease burden in low-SDI areas. In contrast, high-SDI regions such as Japan have more developed mental health systems and smaller urban–rural disparities, contributing to the higher reported burden of ASD in these areas [37]. One study indicated that ASD prevalence varies significantly across different ethnic and socioeconomic groups [38]. In East and Southeast Asia, disparities in ASD prevalence are more likely to be linked to differences in socioeconomic conditions. In developing countries, the absence of universal health insurance systems—combined with substantial socioeconomic disparities between urban and rural households—means that families with lower socioeconomic status, or those not covered by national health insurance, often forgo diagnosis and treatment due to the high cost of ASD-related care [39]. The global Vision ASPR and ASYR for both sexes with ASD are anticipated to gradually increase globally between 2022 and 2050, according to prevalence rates and YLDs from 1990 to 2021.
It must be acknowledged that, across East and Southeast Asia, diagnostic criteria and early ASD screening tools vary considerably. For example, pediatricians in Vietnam primarily rely on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) for diagnosis [40]; in Singapore, both DSM-5 and DSM-IV-TR (Fourth Edition, Text Revision), as well as the Modified Checklist for Autism in Toddlers, Revised with Follow-Up (M-CHAT-R/F), are commonly used [41, 42]; in China, diagnostic practices are more complex and may involve DSM-5, DSM-IV-TR, the Mandarin Chinese Autism Spectrum Rating Scale (MC-ASRS), and the Chinese Classification of Mental Disorders (CCMD) [43]. In Japan, the Social Responsiveness Scale–Parent version (SRS-P) is often employed for early diagnosis [44], while Thailand utilizes the Thai Diagnostic Autism Scale (TDAS) for early screening [45]. This variation reflects a lack of unified, region-wide consensus on diagnostic standards for ASD. The diversity and complexity of these diagnostic tools—and the absence of validation across populations—may compromise diagnostic accuracy and introduce unavoidable bias into GBD–derived estimates. Therefore, in East and Southeast Asia — a subregion characterized by strong historical and cultural similarities — there is an urgent need to update and harmonize ASD diagnostic criteria in alignment with international standards. Establishing a clear diagnostic gold standard is essential to ensure both diagnostic consistency and accuracy. Moreover, early screening cases should not be indiscriminately included in confirmed case counts unless they meet definitive diagnostic criteria. A lack of understanding and public awareness about ASD has contributed to cultural stigmatization in many societies. Individuals with ASD are often subject to shame, discrimination, prejudice, and even social exclusion, which can have profound psychological and social impacts — not only on the individuals themselves but also on their families, including parents and close relatives. In severe cases, this stigma may even lead to suicidal ideation among parents of children with ASD [46]. A study has also shown that cultural stigma can drive individuals with ASD to engage in “camouflaging” behaviors, whereby they consciously mask their symptoms in order to appear neurotypical [47]. Therefore, improving public awareness of ASD and reducing stigma, discrimination, and prejudice are essential for promoting timely diagnosis and treatment. Additionally, early social integration and acceptance can help alleviate emotional and psychological burdens on individuals with ASD and their families.
There are several limitations to this study. Firstly, all data analyzed in this study were derived from the GBD 2021 study. As GBD are based on modeled estimates, they inherently carry limitations, including potential underreporting, inconsistencies in diagnostic criteria across countries, and the absence of original source data. Secondly, some Southeast Asian countries lack robust health information systems, which may lead to incomplete or missing ASD data in the GBD. Second, this study did not incorporate validation using local or country-specific datasets, which limits the interpretability of observed trends in disease burden. Lastly, given the regional focus on East and Southeast Asia, the generalizability of the findings to other areas may be constrained. Future research should strive to integrate reliable national data to validate GBD-based estimates, thereby enhancing the robustness and applicability of the study’s conclusions.
Conclusion
We conducted a careful analysis of the burden, trends, and inequalities of autism spectrum disorder (ASD) in East and Southeast Asia, using data from the GBD 2021 study. Our findings indicate that although the overall burden of ASD in the region is on the rise, significant disparities persist among countries due to differences in diagnostic practices, healthcare infrastructure, and socio-demographic development levels. High-SDI countries such as Japan and South Korea report the greatest ASD burden, likely due to enhanced diagnostic capacity and higher public awareness, which facilitate more comprehensive case identification. In contrast, low-SDI countries may experience underreporting due to shortages of trained mental health professionals and inadequate diagnostic infrastructure. While ASD incidence appears to be more concentrated in low-SDI countries, the majority of the disease burden—particularly in terms of prevalence and YLDs—is observed in high-SDI areas. it is critical to establish standardized diagnostic criteria, strengthen early screening and intervention, enhance health information systems, and address cultural stigma. These measures are essential to improving ASD identification and care, and crucial to addressing the rising burden in this culturally and demographically diverse region.
Supplementary Information
Acknowledgements
We gratefully acknowledge all the scholars who have contributed to GBD research.
Abbreviations
- ASD
Autism spectrum disorder
- ASIR
Age-standardized incidence rates
- ASPR
Age-standardized prevalence rate
- ASYR
Age-standardized years lived with disability rates
- BAPC
Bayesian age-period-cohort
- CI
Concentration Index
- EAPC
Estimated annual percentage change
- GBD
Global Burden of Disease
- GHDx
Global Health Data Exchange
- ILNA
Integrated nested Laplace approximations
- SDI
Socio-demographic index
- SII
Slope Index of Inequality
- YLDs
Years lived with disability
- 95% CI
95% confidence intervals
Authors' contributions
Wen Liu and Xinhao Gong contributed equally to this work.Wen Liu and Shoulin Chen conceived and designed the study. The research was conducted by Wen Liu, Xinhao Gong, and Jinping Ou, with all three contributing to the subsequent discussions and data analysis. Wen Liu, Xinhao Gong, and Jinping Ou collaboratively authored the manuscript. Xinhao Gong and Jinping Ou independently verified the analytical results to ensure their accuracy. Shoulin Chen provided oversight during the data analysis. All authors reviewed and approved the final manuscript.
Funding
This work was supported by grants from Natural Science Foundation of Jiangxi Province (20232ACB206024).
Data availability
All the data used in the analysis of this study were obtained from https://vizhub.healthdata.org/gbd-results/.
Declarations
Ethics approval and consent to participate
The GBD 2021 study is an open database, and all data is anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sauer AK, Stanton JE, Hans S, Grabrucker AM. Autism Spectrum Disorders: Etiology and Pathology. In: Autism Spectrum Disorders. edn. Edited by Grabrucker AM. Brisbane (AU): Exon Publications Copyright: The Authors.; 2021. [PubMed]
- 2.Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet (London England). 2018;392(10146):508–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. ICD-11 for mortality and morbidity statistics (Version: 01/2024) [https://icd.who.int/browse/2024-01/mms/en#437815624]
- 4.Malwane MI, Nguyen EB, Trejo S Jr., Kim EY, Cucalón-Calderón JR. A delayed diagnosis of autism spectrum disorder in the setting of complex attention deficit hyperactivity disorder. Cureus. 2022;14(6):e25825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leow KQ, Tonta MA, Lu J, Coleman HA, Parkington HC. Towards understanding sex differences in autism spectrum disorders. Brain Res. 2024;1833: 148877. [DOI] [PubMed] [Google Scholar]
- 6.Underwood JFG, DelPozo-Banos M, Frizzati A, Rai D, John A, Hall J. Neurological and psychiatric disorders among autistic adults: a population healthcare record study. Psychol Med. 2023;53(12):5663–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen TE, Mazefsky CA, Vasa RA, Lerner MD. Co-occurring psychiatric conditions in autism spectrum disorder. Int Rev Psychiatry (Abingdon). 2018;30(1):40–61. [DOI] [PubMed] [Google Scholar]
- 8.Hossain MM, Khan N, Sultana A, Ma P, McKyer ELJ, Ahmed HU, Purohit N. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: an umbrella review of systematic reviews and meta-analyses. Psychiatry Res. 2020;287: 112922. [DOI] [PubMed] [Google Scholar]
- 9.Dhanasekara CS, Ancona D, Cortes L, Hu A, Rimu AH, Robohm-Leavitt C, Payne D, Wakefield SM, Mastergeorge AM, Kahathuduwa CN. Association between autism spectrum disorders and cardiometabolic diseases: a systematic review and meta-analysis. JAMA Pediatr. 2023;177(3):248–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hung LY, Margolis KG. Autism spectrum disorders and the Gastrointestinal tract: insights into mechanisms and clinical relevance. Nat Reviews Gastroenterol Hepatol. 2024;21(3):142–63. [DOI] [PubMed] [Google Scholar]
- 11.Ferrazzano GF, Salerno C, Bravaccio C, Ingenito A, Sangianantoni G, Cantile T. Autism spectrum disorders and oral health status: review of the literature. Eur J Paediatr Dent. 2020;21(1):9–12. [DOI] [PubMed] [Google Scholar]
- 12.Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, Yusuf A, Shih A, Elsabbagh M. Global prevalence of autism: A systematic review update. Autism Research: Official J Int Soc Autism Res. 2022;15(5):778–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Correction to Lancet Neurol. 2024; 23: 344– 81. The Lancet Neurology 2024, 23(5):e9. [DOI] [PMC free article] [PubMed]
- 14.Global regional. and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The lancet Psychiatry 2022, 9(2):137–150. [DOI] [PMC free article] [PubMed]
- 15.Li YA, Chen ZJ, Li XD, Gu MH, Xia N, Gong C, Zhou ZW, Yasin G, Xie HY, Wei XP, et al. Epidemiology of autism spectrum disorders: global burden of disease 2019 and bibliometric analysis of risk factors. Front Pead. 2022;10:972809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erskine HE, Baxter AJ, Patton G, Moffitt TE, Patel V, Whiteford HA, Scott JG. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol Psychiatric Sci. 2017;26(4):395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, Scott JG. The epidemiology and global burden of autism spectrum disorders. Psychol Med. 2015;45(3):601–13. [DOI] [PubMed] [Google Scholar]
- 18.Ebrahimi Meimand S, Amiri Z, Shobeiri P, Malekpour MR, Saeedi Moghaddam S, Ghanbari A, Tehrani YS, Shokri Varniab Z, Pourabhari Langroudi A, Sohrabi H, et al. Burden of autism spectrum disorders in North Africa and Middle East from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Brain Behav. 2023;13(7): e3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qi X, Zaroff CM, Bernardo AB. Autism spectrum disorder etiology: lay beliefs and the role of cultural values and social axioms. Autism. 2016;20(6):673–86. [DOI] [PubMed] [Google Scholar]
- 20.Global incidence. prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet (London England). 2024;403(10440):2133–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Global regional. National age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet (London England). 2018;392(10159):1736–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Global burden of. 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet (London England). 2024;403(10440):2100–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, Jin L, Zhang T, Chen X. The trends in incidence of primary liver cancer caused by specific etiologies: results from the global burden of disease study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83. [DOI] [PubMed] [Google Scholar]
- 24.Liu W, Deng W, Gong X, Ou J, Yu S, Chen S. Global burden of Alzheimer’s disease and other dementias in adults aged 65 years and over, and health inequality related to SDI, 1990–2021: analysis of data from GBD 2021. BMC Public Health. 2025;25(1):1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Organization WH. Handbook on health inequality monitoring: with a special focus on low-and middle-income countries. World Health Organization; 2013.
- 26.Li S, Chen H, Man J, Zhang T, Yin X, He Q, Yang X, Lu M. Changing trends in the disease burden of esophageal cancer in China from 1990 to 2017 and its predicted level in 25 years. Cancer Med. 2021;10(5):1889–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sasayama D, Kuge R, Toibana Y, Honda H. Trends in autism spectrum disorder diagnoses in Japan, 2009 to 2019. JAMA Netw Open. 2021;4(5):e219234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Molnar AK. Timor leste: politics, history, and culture. Routledge; 2009.
- 29.Muscatello RA, Rafatjoo E, Mirpuri KK, Kim A, Vandekar S, Corbett BA. Salivary testosterone in male and female youth with and without autism spectrum disorder: considerations of development, sex, and diagnosis. Mol Autism. 2022;13(1): 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van’t Westeinde A, Cauvet É, Toro R, Kuja-Halkola R, Neufeld J, Mevel K, Bölte S. Sex differences in brain structure: a twin study on restricted and repetitive behaviors in twin pairs with and without autism. Mol Autism. 2020;11(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green RM, Travers AM, Howe Y, McDougle CJ. Women and autism spectrum disorder: diagnosis and implications for treatment of adolescents and adults. Curr Psychiatry Rep. 2019;21(4): 22. [DOI] [PubMed] [Google Scholar]
- 32.McQuaid GA, Lee NR, Wallace GL. Camouflaging in autism spectrum disorder: examining the roles of sex, gender identity, and diagnostic timing. Autism. 2022;26(2):552–9. [DOI] [PubMed] [Google Scholar]
- 33.Peters SU, Shelton AR, Malow BA, Neul JL. A clinical-translational review of sleep problems in neurodevelopmental disabilities. J Neurodev Disord. 2024;16(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kang L, Liu J, Liu Y, Liang W, Yang F, Liu M. Global, regional, and National disease burden of autism spectrum disorder among children under 5 years from 1990 to 2019: an analysis for the global burden of disease 2019 study. Asian J Psychiatry. 2023;79:103359. [DOI] [PubMed] [Google Scholar]
- 35.Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, Sreenivas V, Saxena S. Mental health systems in countries: where are we now? Lancet (London England). 2007;370(9592):1061–77. [DOI] [PubMed] [Google Scholar]
- 36.James K, Brooks H, Susanti H, Waddingham J, Irmansyah I, Keliat BA, Utomo B, Rose D, Colucci E, Lovell K. Implementing civic engagement within mental health services in South East asia: a systematic review and realist synthesis of current evidence. Int J Mental Health Syst. 2020;14:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miyamoto K, Iwakuma M, Nakayama T. Social capital and health: implication for health promotion by lay citizens in Japan. Global Health Promotion. 2015;22(4):5–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shenouda J, Barrett E, Davidow AL, Halperin W, Silenzio VMB, Zahorodny W. Prevalence of autism spectrum disorder in a large, diverse metropolitan area: variation by sociodemographic factors. Autism Research: Official J Int Soc Autism Res. 2022;15(1):146–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matin BK, Byford S, Soltani S, Kazemi-Karyani A, Atafar Z, Zereshki E, Soofi M, Rezaei S, Rakhshan ST, Jahangiri P. Contributing factors to healthcare costs in individuals with autism spectrum disorder: a systematic review. BMC Health Serv Res. 2022;22(1):604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tran TT, Nguyen VT, Nguyen MP, Huynh Nguyen PQ, Le TTH, Nguyen HY, Nguyen TH, Nguyen TL, Le CT, Nguyen VT. Prevalence of autism spectrum disorder diagnosed according to DSM-5 criteria and associated factors in preschoolers in southern Vietnam. Clin Ter. 2024;175(6):405–11. [DOI] [PubMed] [Google Scholar]
- 41.Sung M, Goh TJ, Tan BLJ, Chan JS, Liew HSA. Comparison of DSM-IV-TR and DSM-5 criteria in diagnosing autism spectrum disorders in Singapore. J Autism Dev Disord. 2018;48(10):3273–81. [DOI] [PubMed] [Google Scholar]
- 42.Zheng RM, Chan SP, Law EC, Chong SC, Aishworiya R. Validity and feasibility of using the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F) in primary care clinics in Singapore. Autism. 2024;28(7):1758–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou B, Zhou H, Wu L, Zou X, Luo X, Fombonne E, Wang Y, Yan W, Xu X. Assessing the accuracy of the modified Chinese autism spectrum rating scale and social responsiveness scale for screening autism spectrum disorder in Chinese children. Neurosci Bull. 2017;33(2):168–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stickley A, Tachibana Y, Hashimoto K, Haraguchi H, Miyake A, Morokuma S, Nitta H, Oda M, Ohya Y, Senju A, et al. Assessment of autistic traits in children aged 2 to 4½ years with the preschool version of the social responsiveness scale (SRS-P): findings from Japan. Autism Research: Official J Int Soc Autism Res. 2017;10(5):852–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Minami K, Horikawa E. Social anxiety tendency and autism spectrum disorder in Japanese adolescence. Pediatr Int. 2021;63(8):903–9. [DOI] [PubMed] [Google Scholar]
- 46.Tamura M, Cage E, Perry E, Hongo M, Takahashi T, Seto M, Shimizu E, Oshima F. Understanding camouflaging, stigma, and mental health for autistic people in Japan. Autism Adulthood: Challenges Manage. 2025;7(1):52–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang W, Yang Y, Song C, Liu Q, Mu R, Yu D. Suicidal risk among Chinese parents of autistic children and its association with perceived discrimination, affiliate stigma and social alienation. BMC Psychiatry. 2024;24(1): 784. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used in the analysis of this study were obtained from https://vizhub.healthdata.org/gbd-results/.