Abstract
To study the capacity of human neurons to mount innate immunity responses to viral infections, we infected cells of a human postmitotic neuron-derivative cell line, NT2-N, with rabies virus (RABV) and herpes simplex type 1 (HSV-1). Changes in neuronal gene expression were analyzed by use of Affymetrix microarrays. Applying a twofold cutoff, RABV increased the transcription of 228 genes, and HSV-1 increased the transcription of 263 genes. The most striking difference between the two infections concerns genes involved in immunity. These genes represent 24% of the RABV-upregulated genes and only 4.9% of the HSV-1-upregulated genes. Following RABV infection, the most upregulated genes belong to the immunity cluster and included almost exclusively genes for beta interferon (IFN-β) primary and secondary responses as well as genes for chemokines (CCL-5, CXCL-10) and inflammatory cytokines (interleukin 6 [IL-6], tumor necrosis factor alpha, interleukin 1 alpha). In contrast, HSV-1 infection did not increase IFN-β gene transcripts and triggered the production of only IL-6 and interferon regulatory factor 1 mRNAs. The microarray results were confirmed by real-time PCR, immunocytochemistry, and enzyme-linked immunosorbent assay. Human neurons were found to express Toll-like receptor 3. They produced IFN-β after treatment with poly(I:C) but not with lipopolysaccharide. Thus, human neurons can mount an innate immunity response to double-stranded RNA. These observations firmly establish that human neurons, in absence of glia, have the intrinsic machinery to sense virus infection.
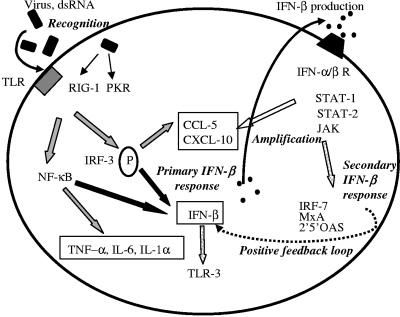
Innate immunity is the first line of defense against invading pathogens. It involves the release of cytokines, including alpha/beta interferons (IFN-α/β) and chemokines; the activation of complement; and the attraction of macrophages, neutrophils, and NK cells into infected tissues. Cells sense viral infection by detecting viral proteins (65) and/or nucleic acids, the double-stranded RNA (dsRNA), a byproduct of the replicative cycles of many viruses, in particular (30). Viral proteins and dsRNA are recognized through receptors such as the evolutionarily conserved Toll-like receptors (TLR) (22, 63). Of the 10 TLRs identified in humans, TLR-3 has been identified to respond to dsRNA (53, 70). The dsRNA can also be sensed by the dsRNA-binding enzyme protein kinase R (PKR) (47) and by the retinoic-induced gene type 1 (RIG-1) (72). Early signaling events initiated by the recognition of virus components include the activation of NF-κB and the phosphorylation of interferon regulatory factor 3 (IRF-3), leading to the production of cytokines (IFN-β, interleukin 6 [IL-6], interleukin 1 alpha [IL-1α], tumor necrosis factor alpha [TNF-α]) and chemokines (CCL-5, CXCL-10, CCL-3, and CCL-4) involved in the initiation or regulation of the inflammatory and antiviral response (1, 58, 60, 72). The interferon response to a viral infection unfolds in two steps (62, 64). The primary response leads to the production of IFN-β. The secondary response results from signaling by the secreted IFN-β through the IFN-α/β receptors (IFN-α/βR) and from the activation of transcription of genes containing IFN-stimulated response elements (ISRE) in their promoters (such as TLR-3 [48]). Signaling through IFN-α/βR triggers the activation of Janus kinases and STAT (1 and 2) transcription factors complexed with IRF-9, which stimulate the transcription of CCL-5 and CXCL-10 and the expression of genes such as the IRF-7, 2′5′OAS, MxA, and PKR genes. These last genes all contain binding sites for activated STAT in their promoters. Finally, the upregulation of IRF-7 (and of IRF-1) expression can exert a positive feedback on IFN-β production (62, 64). A scheme of typical primary and secondary IFN-β responses after sensing a viral infection is shown in Fig. 1. IFN-α and -β are important components of immunity, not only because of their antiviral activities but also because they make the link between innate immunity and adaptive immunity (40).
FIG. 1.
Scheme of innate immune responses to virus infection. dsRNA can be sensed (recognition) by TLR, dsRNA-binding enzyme PKR, or RIG-1, leading to the activation of NF-κB, the phosphorylation (P) of IRF-3, and the production of inflammatory cytokines (IL-6, IL-1α, TNF-α), chemokines (CCL-5, CXCL-10), and IFN-β. This primary IFN-β response is followed by a secondary response resulting from the signaling of the secreted IFN-β through IFN-α/βR and from the activation of the transcription of genes containing ISRE in their promoters (including the TLR-3 gene). Signaling through IFN-α/βR triggers the activation of Janus kinases (JAK) and STAT (-1 and -2) transcription factors, which trigger the expressions of genes such as the IRF-7, 2′5′OAS, MxA, and PKR genes and the amplification of CCL-5 and CXCL-10 transcription. Finally, the upregulation of IRF-7 expression can exert positive feedback on IFN-β production.
It is still unclear whether the nervous system (NS) can mount an efficient innate immune response during viral attack and which cells of the NS are involved. Neurons can produce chemokines and cytokines: human neurons produce CX3CL-1, IFN-β, IL-6, CCL-5 and CXCL-10 (17, 26, 42) and it was recently found that TLRs are constitutively expressed in the NS (6, 8, 34, 52). Human microglia contains TLR-2, -3, and -4 mRNAs (9). One report indicates that human fetal astrocytes express TLR-3 (9, 21). So far, only mouse cortical neurons have been reported to express TLR (TLR-2) (35), and TLR expression by human neurons has not been observed. Nevertheless, neurons are exclusive targets for infection by some viruses, including rabies virus (RABV) of the genus Lyssavirus and herpes simplex virus type 1 (HSV-1) of the Alphaherpesviridae subfamily. It would be interesting to know whether neurons have the intrinsic machinery to respond to infection by these viruses by a triggering of an early innate immune response and whether the nature of the innate immune response depends on the type of viral infection.
We analyzed the transcriptome of NT2-N cells, a model of human postmitotic neurons, as triggered by infection with RABV or HSV-1. NT2-N cell cultures are nearly pure populations of terminally differentiated postmitotic cells with biochemical, morphological, and functional similarities to human NS neurons (18, 56, 73). Upon transplantation into the brain, NT2-N cells display characteristics of fully mature human neurons (33, 69). The responses of human neurons to infection by RABV and HSV-1 were analyzed in vitro by using cultures of NT2-N and microarray analysis, coupled to PCR, real-time PCR analysis, immunocytochemistry, and enzyme-linked immunosorbent assay (ELISA).
We report that human neurons express TLR-3 and can mount differing innate immune responses after RABV and HSV-1 infections. This work provides new insights into the role of neurons in the defense of the NS against infection.
MATERIALS AND METHODS
Human neurons and virus.
Human NT2-N cells (56) were obtained from Ntera-2clD/1 cells (ATCC CRL, 1973) and differentiated according to a modification of the original procedure subsequently modified as described previously (15, 54). The laboratory RABV strain CVS (ATCC vr959), a highly pathogenic strain of the virus causing fatal encephalomyelitis in mouse after intramuscular injection (10), was propagated as previously described (66). HSV-1 strain KOS (61) was propagated in U373MG cells.
Analysis of gene expression after RABV or HSV-1 infection.
NT2-N cells were mock infected or infected with either RABV or HSV-1. RNAs were isolated 24 h (RABV) or 18 h (HSV-1) later from both infected and mock-infected cultures by use of an RNeasy kit. Duplicate samples obtained 2 weeks apart were used to minimize experimental variations. Control quality was monitored on Agilent RNA Nano LabChips. Gene expression profiles were analyzed using Affymetrix microarrays for the human genome (U133A and -B) containing probe sets representing 38,903 transcripts. Experiments were done at the Génopole Strasbourg-Alsace-Lorraine (http://www-genopole.u-strasbg.fr/) by Affymetrix standard protocols. Detected probe sets were selected according to the “presence calls,” and the changes (n-fold) were established by Affymetrix software (Microarray Suite v5.0 and Data Mining Tool v2.0). Only significantly changed probe sets (P < 0.05) were considered. Upregulated genes were distributed into clusters of cell functions using NetAffyx Gene Ontology Mining Tool software.
Standard and real-time RT-PCR analysis and hybridization.
RNA was extracted 1, 6, and 24 h after RABV infection and 24 h after treatment with IFN-β, poly(I:C), or lipopolysaccharide (LPS) with RNeasy kits. RNA quality was monitored on Agilent RNA Nano LabChips. cDNA synthesis was performed with 1 μg RNA by using oligo(dT) primers (100 ng) (Table 1) . Superscript II reverse transcriptase (RT) and Taq DNA polymerase were used for RT-PCR in a Px2 thermal cycler. There were 30 cycles of amplification, performed as follows: 4 min at 94°C, 1 min at 60°C, 1 min at 72°C, 10 min at 72°C, and, finally, cooling. 18S RNA was used as a reference (housekeeping gene). Real-time RT-PCR analysis was performed with an ABI Prism 77700 sequence detection system. Methods and relative quantifications of gene expressions were performed using the comparative method according to the manufacturer's instructions.
TABLE 1.
List of primers
| Gene product or gene | Full name and/or description | Primer sequence (5′→3′)a |
|---|---|---|
| IFITI | Interferon-induced protein 1 | F: GCCACAAAAAATCACAAGCCA |
| R: TCCATTGTCTGGATTTAAGCGG | ||
| CCL-5 | Chemokine ligand 5 (RANTES) | F: CGG CAC GCC TCG CTG TCA TC |
| R: GCA AGC AGA AAC AGG CAA AT | ||
| IFN-β | Beta interferon | F: GCC GCA TTG ACC ATC TAT GAG A |
| R: GAG ATC TTC AGT TTC GGA GGT AAC | ||
| CCL-3 | Chemokine ligand 3 MIP-1 alpha | F: TGG CTC TCT GCA ACC AGT TCT |
| R: GTA GCT GAA GCA GCA GGC G | ||
| CCL-4 | Chemokine ligand 4 MIP-1 beta | F: TGT CCT GTC TCT CCT CA |
| R: CAT TGG TGC TGA GAG CG | ||
| CXCL-11 | Chemokine ligand 11 (I-TAC) | F: GCA GTG AAA GTG GCA GA |
| R: GAT TTA GGC ATC GTT GTC C | ||
| CXCL-10 | Chemokine ligand 10 (1P-10) | F: TGA GCC TAC AGC AGA GGA A |
| R: TAC TCC TTG AAT GCC ACT TAG A | ||
| OAS-1 | 2′,5′-oligoadenylate synthetase 1 | F: TCA GAA GAG AAG CCA ACG TGA |
| R: CGG AGA CAG CGA GGG TAA AT | ||
| CCL-20 | Chemokine ligand 20 (LARC) | F: GATGTCAGTGCTGCTACTCCACC |
| R: TGTGTATCCAAGACAGCAG | ||
| CiG-5 | Viperin | F: GGGCAAGTTGGTGAGGTTCTG |
| R: CCGGATCAGGCTTCCATTG | ||
| ISG20 | Interferon-stimulated gene (20 kDa) | F: AGAGTGGCCTGGCTCGTTG |
| R: GGCCGGATGAACTTGTCGT | ||
| PTGS2 | Cox2 | F: CCCCAGGGCTCAAACATGAT |
| R: AGCTGGCCCTCGCTTATGAT | ||
| NeuF-H | Neurofilament H protein | F: CCCCAGGCGATGGACAATTATGAT |
| R: CACTTGGTTTTATTGCACAGAAGC | ||
| STAT-1 | Signal transducer and activator of transcription 1 | F: TTCTGTGTCTGAAGTGTAAGTGAA |
| R: TAACACGGGGATCTCAACAAGTTC | ||
| IRF-7 | Interferon regulatory factor 7 | F: CAGCTGCGCTACACGGAGGAACTG |
| R: CTCCAGCTCCATAAGGAAGCACTC | ||
| NF-κB | Nuclear factor of kappa light polypeptide gene enhancer | F: GATGAAGATTGAGCGGCCTGTAAC |
| R: TCCTCCGCTTCCGCTGCACCTCTT | ||
| TLR-3 | Toll-like receptor 3 | F: AAC GAC TGA TGC TCC G |
| TaqMan | R: CCA GAG CCG TGC TAA G | |
| PCR | F: GAGGCGGGTGTTTTTGAACTAGAA | |
| R: AAGTCAATTGTCAAAAATAGGCCT | ||
| MOG | Oligodendrocyte-myelin glycoprotein | F: GAAAGCTGGGCAACATGCCTGCTT |
| R: TGTCACTCCGGCTAGAGTGCAGTG | ||
| CD200R | CD200 receptor | F: TTAACACTTCATGGCCTGTAAAGA |
| R: TGTGCCATTGCTCCAGTATTCTTG | ||
| TNF-α | Tumor necrosis factor alpha | F: GGCATCCTGAAGTATGTCACATAG |
| R: CATTAGCAGCAACACCAGAAAAAT | ||
| IL-6 | Interleukin 6 | F: ATGCCAGCCTGCTGACGAAGCTGC |
| R: TATTTGAGGTAAGCCTACACTTTC | ||
| RIG-1 | Retinoic-induced gene-1 | F: GAGTGTCTTTTCTTATGTGATTTT |
| R: GCAGGCAAGTCTTACATGGCAGCA | ||
| 18S | Ribosomal 18S | F: CTT AGA GGG ACA AGT GGC G |
| R: ACG CTG AGC CAG TCA GTG TA | ||
| N | Rabies N protein | F: GGA ATT CTC CGG AAG ACT GCA CCA GCT ATG G |
| R: AGA ATT CCC ACT CAA GCC TAG TGA ACG G | ||
| UL54 | HSV-1 protein | F: CGC CAA GAA AAT TTC ATC GAG |
| R: ACA TCT TGC ACC ACG CCAG |
F, forward; R, reverse.
Immunocytochemistry.
Infected and noninfected NT2-N cells were washed once with phosphate-buffered saline (PBS) containing Ca2+Mg2+, fixed with 4% paraformaldehyde for 30 min at room temperature (Rt), washed again, and treated with gelatin (1% in water) for 5 min at 4°C. The samples were then incubated for 30 min at Rt in 0.3% Triton X-100-PBS, and the surface immunoglobulin (Ig) receptors were blocked with a saturating medium (2% bovine serum albumin and 5% fetal calf serum in PBS) for 30 min at Rt and for 10 min with Fc-block (1 mg/106 cells). Viral antigens were detected by incubation with HSV-1 (early antigens) or RABV (nucleocapsid antigens) fluorescein isothiocyanate (FITC)-conjugated rabbit antibody (Ab) for 30 min at Rt. Rabbit Ab directed against NeuF-H, mouse Ab specific for human CXCL-10, for Tau, or for synaptophysin, and rabbit Ab directed against human TLR-3 were incubated with the samples for 1 h at Rt, and then biotinylated anti-rabbit Ab, FITC-conjugated anti-mouse Fab′2, biotinylated anti-mouse IgG, or Cy5-conjugated anti-rabbit Ab was added for 30 min at Rt. Slides were also incubated for 30 min at Rt with peroxidase-conjugated streptavidin for Tau and synaptophysin detection, a procedure followed by 6 min of incubation with diaminobenzidine or with Cy3-conjugated streptavidin for the detection of NeuF-H. Nuclei were stained with Hoechst 33342 or hematoxylin. Ab and reagents were diluted in saturating medium. Slides were washed with PBS Ca2+Mg2+, except for the last wash, which was done with water. Coverslips were mounted in Fluoromount-G, and the samples were observed under a Leica DM 5000B UV microscope equipped with a DC 300FX camera. Images were processed with the Leica FW 4000 software.
IFN-β ELISA.
Human IFN-β was detected in NT2-N culture supernatants by enzyme immunoassay following the manufacturer's instructions.
Reagents and antibodies.
FITC-conjugated rabbit anti-HSV-1 protein Ab was from Dako. FITC-conjugated rabbit anti-RABV nucleocapsid was from Bio-Rad. Anti-human CXCL-10 monoclonal Ab 6D4 was from Abcam. The anti-human TLR-3 Ab, H125 (rabbit polyclonal Ab), was from Santa Cruz Biotechnology. Anti-bovine Tau mouse IgG (which also recognizes human Tau) was from Boehringer. The human IFN-β ELISA kit used was from PBL Biomedical Laboratories. Rabbit anti-neurofilament 200, NeuF-H, anti-rat synaptophysin mouse IgG (which reacts with human synaptophysin), poly(I:C), hematoxylin, LPS, and the 3,3′-diaminobenzidine tablets, Sigma Fast-DAB, were from Sigma Chemical Corp. Biotinylated anti-rabbit Ab was obtained from Vector Laboratories. Biotinylated anti-mouse IgG and peroxidase-conjugated streptavidin were from Amersham Life Sciences. Cy3-conjugated streptavidin and FITC-conjugated Fab′2 anti-mouse Ab were from Jackson Immunoresearch Laboratories. Recombinant human IFN-β (Betaferon) was from Schering. Fluoromount-G was from Southern Biotechnology Associates. The RNeasy Protect kit used was from QIAGEN. Molecular weight markers, Taq polymerase, and phiX 174 DNA/HaeIII were from Promega. Superscript II RT was from Invitrogen. oligo(dT) primers were from Eurogentec. Agilent RNA Nano LabChips were from Agilent Technologies. Human genome U133A and -B arrays were from Affymetrix. Human brain total RNA was from BD Biosciences.
RESULTS
Human NT2-N cultures are pure neuron cultures susceptible to HSV-1 and RABV infection.
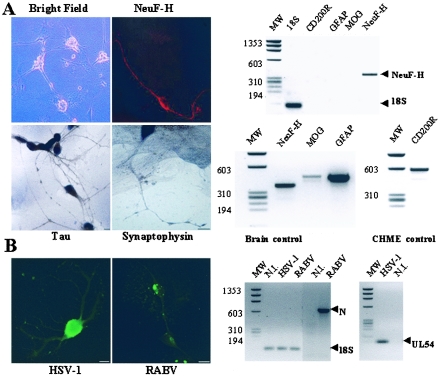
NT2-N cells progressively develop an extensive network of neurites (Fig. 2). More than 95% of the cells expressed the high-molecular-weight neurofilament protein NeuF-H, as assayed by immunocytochemistry and RT-PCR (Fig. 2A). NT2-N cells also expressed the microtubule-associated Tau protein, a marker of the late stage of neuronal differentiation essential for maintaining the cytoskeleton and axonal transport (Fig. 2A). They also expressed synaptophysin, a synaptic vesicle protein involved in neuronal transmission (Fig. 2A). Differentiation of Ntera-2clD/1 did not give rise to any glial cells, as tested by RT-PCR, and mRNAs that are markers of astrocytes (glial fibrillary acidic protein [GFAP]), oligodendrocytes (oligodendrocyte-myelin glycoprotein [MOG]), and microglia (the CD200 receptor [CD200R]) (2, 59, 71) were all absent (Fig. 2A; PCR).
FIG. 2.
NT2-N cultures are pure human postmitotic neuron preparations susceptible to RABV and HSV-1 infection. (A) NT2-N cultures are pure cultures of neurons. Shown is a bright-field, phase-contrast photomicrograph of NT2-N culture (magnification, ×20). NT2-N cells express the high-molecular-weight neurofilament (NeuF-H); Tau, a marker of highly differentiated neurons (immunocytochemistry and/or RT-PCR); and synaptophysin, a marker of synaptic vesicles (immunocytochemistry). In contrast to human brain cells, they do not express MOG or GFAP markers of oligodendrocytes or astrocytes, respectively, nor CD200R, a marker of microglia, expressed here by the human microglial cell line CHME (31). (B) After a 24-h infection, NT2-N cells express HSV-1 and RABV antigens in cell bodies and neurites. Transcripts of HSV-1 (UL54 gene) and RABV (N gene) can be detected in NT2-N cultures infected for 24 h (PCR). MW, molecular weights. Bars in the photographs represent 10 μm.
Following infection, HSV-1 and RABV proteins were clearly detected by immunocytochemistry (Fig. 2B), and the HSV-1 UL54 gene and RABV N gene amplicons were detected by RT-PCR (PCR results shown in Fig. 2B). Thus, NT2-N cells were susceptible to infections by HSV-1 and RABV.
Transcriptional programs of human neurons activated during RABV and HSV-1 infection.
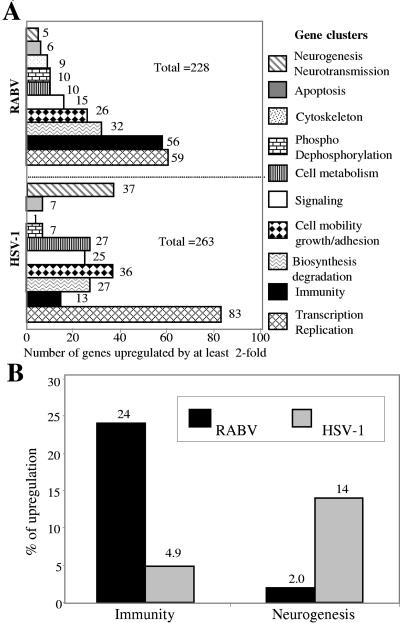
We searched for neuronal genes for which transcription is upregulated during RABV and HSV-1 infection by transcriptome analysis using Affymetrix microarrays U133A and U133B. RNAs were prepared from two batches of cultures of NT2-N cells that were either not infected (24 h and 18 h) or were infected with RABV (24 h) or with HSV-1 (18 h). The percentages of NT2-N cells infected were the same in the two infections (80% of each culture was infected, as detected by immunochemistry). A cutoff of a twofold increase was used to identify upregulated genes by microarray analysis: RABV infection upregulated the expression of 228 genes, and HSV-1 upregulated the expression of 263 genes. The genes were distributed into 10 clusters defined by the NetAffyx gene ontology mining tool software, and this suggested that RABV-1 and HSV-1 affected cell physiology in very different ways (Fig. 3A). RABV upregulated 56 genes of the immunity cluster of genes (24% of all upregulated genes), whereas HSV-1 upregulated only 13 genes in this cluster (4.9%) (Fig. 3B). RABV upregulated only 5 genes involved in neurogenesis/neurotransmission (2.0% of all genes upregulated by RABV infection), whereas HSV-1 upregulated 37 of the genes of this cluster (14%). A list of the 56 immunity genes upregulated by a 24-h RABV infection is shown in Table 2 in order of overexpression magnitude (the greatest increase was 328.5). These genes include the IFN-β (×150) gene; the genes coding for chemokines CCL-5 (×232), CCL-3 (×105), CCL-4 (×97), CCL-20 (×42), CXCL-9 (×12), CXCL-10 (×61), CXCL-11 (×86), and CXCL-3 (×3.2); several genes whose expressions are under the control of IFN-β, notably, those coding for IFIT-1 (×328.5), IFIT-2 (×39), IFIT-4 (×72) ISG-20 (×37), GBP-5 (×55), GBP-1 (×11), 2′5′OAS-1 (×43.0), 2′5′OAS-3 (×6.1), and MxA (×15.0); genes coding for the interferon regulatory factors IRF-7 (×7.3) and IRF-1 (×3.8); genes coding for the activators of transcription STAT-1 (×8.2), STAT-2 (×4.0), and NF-κB (×2.1); and genes which can sense dsRNA, in particular PKR (×2.6), RIG-1 (×3.6), and TLR-3 (×2.0). RABV upregulated a factor of the alternate pathway of complement, factor B (×10.0). It also increased the expressions of genes for inflammatory cytokines IL-6 (×8.5), IL-1α (×4.3), TNF-α (×2.4), and IL-15 (×2.0); of the HLA-E (×2.1) gene coding for the molecule of the nonclassical histocompatibility gene of class I that binds leader peptides from other class I molecules and CD94/NKG2, a receptor expressed by natural killer cells (12). RABV also stimulated the expression of Ly-6E, also called CD107 (×2.2), a marker involved in T-cell adhesion and activation, the expression of which is induced by IFN in neuronal cells (19).
FIG. 3.
Patterns of genes upregulated by RABV and HSV-1. (A) Numbers of genes upregulated by at least twofold after RABV and HSV-1 infection in each of the 10 gene clusters defined by the Affymetrix annotation program. HSV-1- and RABV-infected transcriptomes differ in terms of the clusters of genes involved with the cytoskeleton and in neurogenesis/neurotransmission, cell metabolism, and immunity. (B) Distribution (percentages) of upregulated genes into immunity and neurogenesis/neurotransmission clusters after RABV or HSV-1 infection. RABV upregulates mainly genes of immunity, whereas HSV-1 mainly upregulates genes involved in neurogenesis.
TABLE 2.
Immunity genes upregulated by RABV
| Gene product or genea | Full name and/or description | Accession no. (Affymetrix) | Fold RABV (24 h)b | Fold HSV-1 (18h)** |
|---|---|---|---|---|
| IFIT-1 | Interferon-induced protein with tetratricopeptide repeats 1 | 203153 | 328.5 | 0 |
| CCL-5 | Chemokine (C-C motif) ligand 5 | 1405 | 232.0 | 0 |
| IFN-β | Beta interferon | 208173 | 150.0 | 0 |
| CCL-3 | Chemokine (C-C motif) ligand 3 | 205114 | 105.0 | 0 |
| CCL-4 | Chemokine (C-C motif) ligand 4 | 204103 | 98.0 | 0 |
| CXCL-11 | Chemokine (C-X-C motif) ligand 11 | 211122 | 86.0 | 0 |
| IFIT-4 | Interferon-induced protein with tetratricopeptide repeats 4 | 229450 | 72.0 | 0 |
| CXCL-10 | Chemokine (C-X-C motif) ligand 10 | 204533 | 61.0 | 0 |
| GBP-5 | Guanylate binding protein 5 | 238581 | 55.0 | 0 |
| PTGS-2 | Prostaglandin-endoperoxide synthase 2 (COX-2) | 204748 | 50.0 | 0 |
| OAS-1 | 2′,5′-oligoadenylate synthetase 1 | 205552 | 43.0 | 0 |
| CCL-20 | Chemokine (C-C motif) ligand 20 | 205476 | 42.0 | 0 |
| IFIT-2 | Interferon-induced protein with tetratricopeptide repeats 2 | 226757 | 39.0 | 0 |
| CIG-5 | Viperin | 213797 | 38.0 | 0 |
| ISG-20 | Interferon-stimulated gene, 20 kDa | 204698 | 37.0 | 0 |
| GIP-2 | Interferon, alpha-inducible protein (clone IFI-15K) | 205483 | 28.0 | 0 |
| Mx-A | Myxovirus (influenza virus) resistance protein type A | 202086 | 15.0 | 0 |
| IFI-27 | Interferon, alpha-inducible protein 27 | 202411 | 15.0 | 0 |
| IFITM-1 | Interferon-induced transmembrane protein 1 (9-27) | 214022 | 13.5 | 0 |
| CXCL-9 | Chemokine (C-X-C motif) ligand 9 | 203915 | 12.0 | 0 |
| IFI644 | Interferon-induced protein 44 | 214453 | 11.0 | 0 |
| BF | Factor B alternative complement pathway | 202357 | 10.0 | 0 |
| GIP-3 | Interferon, alpha-inducible protein (clone IFI-6-16) | 204415 | 10.0 | 0 |
| GBP-1 | Guanylate binding protein 1, interferon inducible | 202269 | 10.5 | 0 |
| IL-6 | Interleukin 6 (beta interferon 2) | 205207 | 8.5 | 2.05 |
| STAT-1 | Signal transducer and activator of transcription 1 | 209969 | 8.2 | 0 |
| IRF-7 | Interferon regulatory factor 7 | 208436 | 7.3 | 0 |
| DnaJB5 | DnaJ (Hsp40) homolog, subfamily B, member 5 | 207453 | 7.0 | 0 |
| SAMHD-1 | SAM domain and HD domain 1 | 204502 | 6.5 | 0 |
| OAS-3 | 2′,5′-oligoadenylate synthetase 3 | 218400 | 6.1 | 0 |
| IFIT-5 | Interferon-induced protein with tetratricopeptide repeats 5 | 203596 | 6.1 | 0 |
| OAS-2 | 2′,5′-oligoadenylate synthetase 3, 100 kDa | 204972 | 5.2 | 0 |
| INDO | Indoleamine-pyrrole 2,3 dioxygenase | 210029 | 4.4 | 0 |
| IL1-α | Interleukin 1 alpha | 210118 | 4.3 | 0 |
| STAT-2 | Signal transducer and activator of transcription 2, 113 kDa | 225636 | 4.0 | 0 |
| IRF-1 | Interferon regulatory factor 1 | 202531 | 3.8 | 3.2 |
| ISGF-3G | Interferon-stimulated gene factor 3 gamma, 48 kDa | 203882 | 3.8 | 0 |
| IF-35 | Interferon-induced protein 35 | 209417 | 3.6 | 0 |
| RIG-1 | Retinoic acid-inducible gene 1 (DEAD/H box polypeptide) | 242961 | 3.6 | 0 |
| TAP-1 | Transporter 1, ATP binding cassette, subfamily B (MDR/TAP) | 202307 | 3.4 | 0 |
| CIS | Complement component 1, S subcomponent | 208747 | 3.3 | 0 |
| CXCL-3 | Chemokine (C-X-C motif) ligand 3 | 207850 | 3.2 | 0 |
| TAP-2 | Transporter2, ATP-binding cassette, subfamily B (MDR/TAP) | 204770 | 3.1 | 0 |
| PTX-3 | Pentaxin-related gene, rapidly induced by IL-1 beta | 206157 | 2.9 | 0 |
| IF-16 | Interferon, gamma-inducible protein 16 | 208965 | 2.8 | 0 |
| NCF-2 | Neutrophil cytosolic factor 2 | 209949 | 2.6 | 0 |
| PKR | Interferon-inducible double-stranded RNA-dependent protein kinase | 204211 | 2.6 | 0 |
| NOD27 | Nucleotide-binding oligomerization domain 27 | 226474 | 2.5 | 0 |
| GBP-3 | Guanylate binding protein 3 | 223434 | 2.5 | 0 |
| TNF-α | Tumor necrosis factor alpha | 223501 | 2.4 | 0 |
| PTGER-4 | Prostaglandin E receptor 4 (subtype EP4) | 204897 | 2.4 | 0 |
| Ly-6E | Lymphocyte antigen 6 complex locus E (CD107) | 202145 | 2.2 | 0 |
| NF-κB2 | Nuclear factor kappa-B2 | 207535 | 2.1 | 0 |
| HLA-E | Major histocompatibility complex, class 1, E | 200904 | 2.1 | 0 |
| TLR-3 | Toll-like receptor 3 | 206271 | 2.0 | 0 |
| IL-15 | Interleukin 15 | 205992 | 2.0 | 0 |
Underlined genes and gene products are those for which transcriptions were verified by PCR (see Fig. 4).
Transcripts that were more than twofold more abundant in NT2-N cultures infected by RABV for 24 h than in mock-infected NT2-N cultures.
Increases (n-fold) of the same transcripts in NT2-N cultures infected by HSV-1 for 18 h. In addition to those for IL-6 and IRF-1, which were activated both by RABV and HSV-1, HSV-1 specifically amplified the expressions of 11 other immunity genes/gene products: EDA, Affymetrix identification number (AIN) 211128 (×10.5); CXCR-4, AIN 217028 (×7.9); CXCL-12, AIN 203666 (×4.5); CD80, AIN 207176 (×3.05); CEBPE, AIN 214523 (×3.65); PGLYRP4, AIN 220944 (×2.8); SCUBE-1, AIN 233988 (×4.4); LILRB-4, AIN 210152 (×3.4); CEACAM-1, AIN 211883 (×3.4); C4A/B, AIN 214428 (×3.9); and ULBP-1, AIN 221323 (×2.5).
The 25 genes for which expression was most strongly stimulated were all genes involved in the innate immunity response.
HSV-1 upregulated only 2 of the 56 immunity genes upregulated by RABV: those coding for IL-6 and IRF-1. The increases were only moderate (×3.2 and ×2.05, respectively) (Table 2). Thus, in striking contrast to RABV infection, HSV-1 infection did not increase the abundance of IFN-β transcripts or of any of the transcripts of the IFN response genes. HSV-1 specifically stimulated the transcription of genes belonging to the immunity cluster which were not increased by RABV, for example, those coding for CXCR-4 (×7.9), CXCL-12 (×4.05), and CD80, a costimulatory adhesion molecule (×3.05).
Of the 10 TLR present on an Affymetrix U133 array, only TLR-1, TLR-2, TLR-3, and TLR-4 could be detected in NT2-N (Table 3). RABV infection, but not HSV-1 infection, upregulated the expression of TLR-3 only (×2.0). This observation suggests that, among the TLRs, NT2-N cells have the capacity to express those which react with dsRNA (TLR-3) and LPS (TLR-4).
TABLE 3.
NT2-expressed TLR-1, -2, -3, and -4
| Gene | ProbeSet no. | Presencea | P value |
|---|---|---|---|
| TLR-1 | 210176 | + | 0.030273 |
| TLR-2 | 204924 | + | 0.037598 |
| TLR-3 | 206271 | + | 0.000732 |
| TLR-4 | 221060 | + | 0.023926 |
| TLR-5 | 210166 | − | 0.219482 |
| TLR-6 | 207446 | − | 0.533936 |
| TLR-7 | 220146 | − | 0.633789 |
| TLR-8 | 220832 | − | 0.725830 |
| TLR-9 | 223903 | − | 0.466064 |
| TLR-10 | 223750 | − | 0.432373 |
Presence (+) of TLR is indicated when the P value is lower than 0.02; the presence is uncertain (−) when the P value is higher than 0.02.
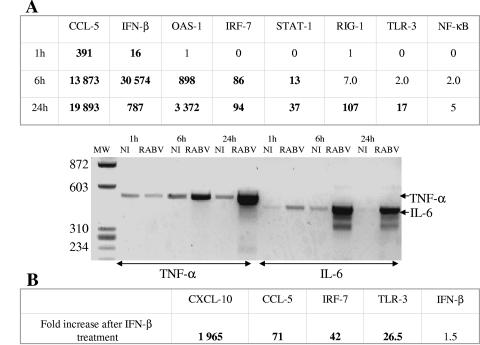
We used PCR to validate the expression patterns detected by using microarrays in RABV-infected NT2-N cells. Cultures of NT2-N cells were infected for 24 h with RABV, RNA was extracted, and mRNAs of particular genes were studied by RT-PCR and quantified by real-time RT-PCR using 18S mRNA as a control (Fig. 4A). Fourteen genes were chosen as representative either of the early innate immunity response (the genes for IFN-β and the chemokines CCL-5 and CXCL-10) or of inflammatory cytokines (TNF-α) and interferon-regulated genes (PTSG, ISG-20, CiG-5, 2′5′OAS, TLR-3). PCR and real-time PCR analysis confirmed the increases of the expressions of these genes (Fig. 4A for PCR and Fig. 4B for real-time PCR with representative genes, such as those coding for 2′5′OAS-1, PTSG-20, IFN-β, IFIT-1, and CCL-5). Uninfected neurons expressed IFIT-1, CCL-4, CXCL-10, 2′5′OAS-1, CCL-20, ISG-20, TLR-3, and TNF-α but not CCL-5, IFN-β, PTGS-2, or CiG-5. The absence of transcription in control cells may account for the strong relative amplification of the IFN-β or CCL-5 genes after RABV infection, as observed both by microarray analysis (×150 and ×232, respectively; Table 2) and by real-time PCR analysis (×700 and ×52,000, respectively; Fig. 4B). We specifically confirmed the absence of IFN-β transcripts after 6 and 24 h in HSV-1-infected cultures (data not shown).
FIG. 4.
PCR confirmation of the differential gene expression detected by microarray analysis. (A) PCR in 24-h noninfected (N.I.) and RABV-infected NT2-N cells. 18S was used as a reference housekeeping gene. (B) Real-time PCR. Results are expressed as multiples of the noninfected NT2-N value (defined as 1). Error for the measure was less than 10%.
Thus, the expression of IFN-β, inflammatory cytokines/chemokines, and IFN-β-regulated genes is activated in NT2-N cells following RABV infection. This reaction is specific to RABV and is not observed after HSV-1 infection. NT2-N cells react to HSV-1 infection by a more limited innate immune response involving the stimulation of only a few innate immunity genes, including the IL-6, IRF-1, and CXCL-12 genes but excluding IFN-β and IFN-β-regulated genes.
RABV-infected NT2-N cells produce CXCL-10 and TLR-3 proteins and secrete IFN-β.
We used immunocytochemistry (CXCL-10 and TLR-3) and immunoassay (IFN-β) to demonstrate that the activation of gene transcription led to the production of IFN-β, CXCL-10, and TLR-3 proteins.
The accumulation of CXCL-10 was clearly demonstrated in the cytoplasms of NT2-N cells infected with RABV for 24 h, whereas only traces of the protein were detected in uninfected cells (Fig. 5A), consistent with the transcription level (Fig. 4).
FIG. 5.
RABV-infected NT2-N cells express CXCL10 and TLR-3 and secrete IFN-β. (A) CXCL-10 was detected by immunofluorescence in 24-h RABV-infected NT2-N cultures, but only trace or no CXCL-10 was present in noninfected NT2-N cultures. (B) With a polyclonal rabbit Ab directed against human TLR-3, TLR-3 protein was specifically detected by immunocytochemistry in noninfected (a) and RABV-infected (b) cultures. (c) The TLR-3 Ab was omitted. TLR-3 accumulates in intracytoplasmic vesicles (brown coloration) and at the membrane (arrows). Nuclei (blue) are stained with hematoxylin. (C) Detection of human IFN-β by ELISA in the supernatants of noninfected and 6-, 12-, 24-, and 48-h RABV- or 18-h HSV-1-infected NT2-N cultures. Betaferon was used as a positive control.
TLR-3 accumulated in NT2-N cells as cytoplasmic and perinuclear inclusions and at the membrane peripheries (arrows in Fig. 5B) in both uninfected NT2-N cells (panel a in Fig. 5B) and in NT2-N cells infected with RABV for 24 h (panel b in Fig. 5B). The intensity of TLR-3 staining in intracytoplasmic vesicles was however stronger in RABV-infected cells (compare panels a and b in Fig. 5B). This is consistent with the transcription results: TLR-3 mRNAs were detected by RT-PCR in uninfected neurons but were more abundant following RABV infection (Fig. 4A).
Supernatants of mock-infected HSV-1 and RABV-infected NT2-N cells were harvested 6, 24, and 48 h after RABV infection and 18 h after HSV-1 infection. They were assayed for the presence of IFN-β by immunoassay (Fig. 5C). IFN-β was detected in the supernatant of NT2-N cells 6 h, 24 h, and 48 h following RABV infection. IFN-β production peaked at 24 h and declined thereafter, suggesting that IFN-β is secreted transiently. In contrast, IFN-β was not detected in the supernatants of mock-infected NT2-N cells or in the 18-h supernatant of NT2-N cells infected with HSV-1, consistent with the results of the transcription analyses.
These findings establish that NT2-N cells produce TLR-3 protein and that RABV infection increases the amount produced. Immunocytochemistry analysis suggested that TLR-3 trafficking may be modified following infection. RABV-infected NT2-N cells secrete IFN-β and produce CXCL-10 protein. Thus, at least for these three genes, transcriptional increases observed by microarrays and PCR analysis are associated with increased protein production.
Kinetics of innate immune response in RABV-infected NT2-N cells.
We used real-time RT-PCR to document the time course of the IFN-β response in RABV-infected NT2-N cells and also to identify the cascades of genes involved in the innate immune response. IFN-β gene transcripts and the transcripts of six other genes were analyzed by real-time RT-PCR at 1, 6, and 24 h postinfection. The other six genes were the CCL-5 gene, the transcription of which is modulated by the phosphorylation of IRF-3; the 2′5′OAS-1 and IRF-7 gene, the expressions of which are controlled by STAT-1 and -2; the TLR-3 gene, which can sense RNA viral infection; and the NF-κB and STAT-1 genes, coding for transcription factors. Transcripts of the TNF-α and IL-6 genes, which are upregulated following NF-κB activation or phosphorylation of IRF-3, were also analyzed by RT-PCR. The CCL-5 and IFN-β genes were the first genes to be upregulated: their transcripts were more than 10-fold more abundant in infected neurons than in uninfected neurons 1 h after RABV infection (Fig. 6A). The transcription of the IFN-β gene reached a maximum 6 h postinfection and then decreased. The early increases in the transcriptions of the IFN-β and CCL-5 genes was followed by increased transcriptions of the 2′5′OAS-1, IRF-7, and STAT-1 genes, which reached 10 times the control values 6 h after infection. TNF-α and IL-6 gene transcripts were found 6 h postinfection, and that of the IL-6 gene was found even 1 h after infection (Fig. 6A). The last genes to have transcription upregulated (24 h or later) were the RIG-1, TLR-3, and NF-κB genes (Fig. 6A).
FIG. 6.
Dynamics of IFN-β- and IFN-β-controlled mRNA abundances. (Α) Kinetics of transcription of a set of genes involved in the innate immune response triggered by RABV infection, as analyzed by real-time PCR or PCR. Results are expressed as multiples of the value for mock-infected cells (defined as 1). Values with relative increases of >10-fold are in bold. The kinetics of the transcriptions of TNF-α and IL-6 during RABV infection were analyzed by RT-PCR. NI, noninfected. (B) Transcriptions of CXCL-10, CCL-5, IRF-7, TLR-3, and IFN-β after a 24-h treatment of NT2-N cells with IFN-β (1,000 IU/ml). Real-time PCR results are given as multiples of the value for mock-infected cultures (defined as 1).
Thus, during the 24 h following RABV infection, (i) CCL-5 and IFN-β genes are transcribed 1 h after infection; (ii) this transcription is followed, after 6 h, by the upregulation of IL-6, TNF-α, 2′-5′OAS-1, IRF-7, and STAT-1 gene transcription; and (iii) the transcriptions of the RIG-1, NF-κB and TLR-3 genes are upregulated later (24 h). The increased transcription of the IFN-β gene is transient. These results suggest that the transcriptome analysis performed 24 h after RABV infection reflects both the triggering of IFN-β and CCL-5 in the first hour of infection and a subsequent cascade of events triggered by the early expression of these two mediators.
Treatment of NT2-N cells with human recombinant IFN-β increased the responses of genes which regulate the secondary IFN-β response genes but did not amplify IFN-β gene transcription.
IFN-β is present in the supernatant of RABV-infected NT2-N cultures, and we therefore tested whether the addition of IFN-β to NT2-N cultures triggers the cascade of events upregulated by IFN-β (Fig. 1). Uninfected NT2-N cells were treated (or mock treated) with 1,000 IU of recombinant IFN-β (rIFN-β) for 24 h, and the expressions of the CCL-5, CXCL-10, TLR-3, and IRF-7 genes were compared by real-time RT-PCR (Fig. 6B). The transcriptions of the CXCL-10, CCL-5, IRF-7, and TLR-3 genes were increased by this treatment (increases of 1,965-, 71-, 42-, and 26.5-fold, respectively), indicating that exogenous IFN-β triggered in NT2-N cells a cascade of events compatible with a secondary IFN-β response. In particular, these events include the upregulation of TLR-3, the promoter region of which contains an ISRE susceptible to IFN-α/β. Thus, TLR-3 upregulation in human neurons may be controlled by IFN. The effect of exogenous IFN-β on IFN-β transcription through the upregulation of IRF-7 was also tested by real-time RT-PCR (Fig. 6B): IFN-β transcription in NT2-N cells was not significantly affected (1.5-fold increase) by treatment of with either 1,000 or 10,000 IU/ml rIFN-β (result not shown for the highest dose).
These observations strongly suggest that NT2-N cells can mount a secondary IFN-β response and therefore that human neurons express IFN-α/βR. However, these cells are not able to increase the expression of IFN-β transcripts themselves in the absence of RABV infection.
NT2-N cells can sense synthetic dsRNA but not LPS.
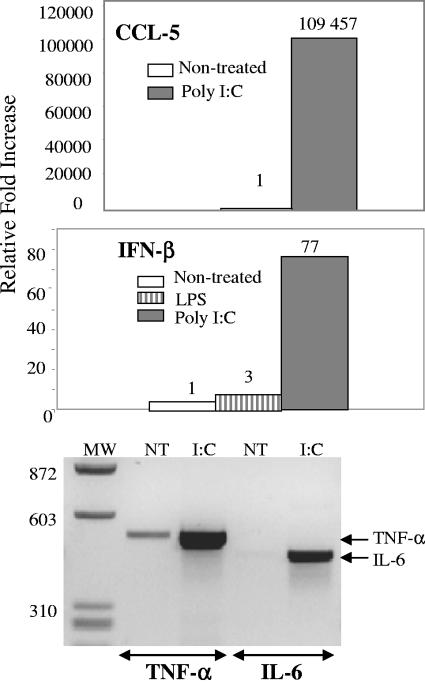
NT2-N expressed three molecules, TLR-3 (mRNAs and protein), PKR (transcripts only), and RIG-1 (transcripts only), which can sense dsRNA. Therefore, we analyzed whether these cells can sense the presence of dsRNA in the extracellular compartment. Synthetic dsRNA poly(I:C) (100 μg/ml) was added to the NT2-N cultures, and, after 24 h, the expressions of IFN-β and CCL-5 were analyzed by real-time RT-PCR and those of TNF-α and IL-6 were analyzed by RT-PCR. The response of NT2-N cells to LPS (1 μg/ml) was also tested by real-time RT-PCR (Fig. 7). Treatment with dsRNA led to the upregulation of IFN-β, CCL-5, TNF-α, and IL-6 transcripts, whereas LPS treatment had no effect (only the real-time PCR data are shown for LPS). Transfection of the cells was not required for an effective sensing of dsRNA (data not shown).
FIG. 7.
Synthetic dsRNA but not LPS triggers an innate immune response in NT2-N cells. A 24-h treatment with poly(I:C) (100 μg/ml) triggers the upregulation of IFN-β (×77) and CCL-5 (×109,457) transcripts, as determined by real-time PCR, and the upregulation of TNF-α and IL-6 transcripts, as assessed by RT-PCR. LPS has no effect. NT, nontreated.
DISCUSSION
We report evidence that human postmitotic neurons (NT2-N cells) express TLR-3 and can mount an innate immune response characterized by the production of IFN-β, chemokines, and inflammatory cytokines in response to RABV and dsRNA [poly(I:C)]. NT2-N can also mount a partial innate immune response to HSV-1 characterized by an increase of inflammatory cytokine transcripts but not of IFN-β transcripts. Thus, human neurons, even in the absence of astrocytes, oligodendrocytes, and microglia, have the machinery to sense viral infection, and the nature of the innate immune response depends on the nature of the infection.
TLR-3 mRNA has been detected in the human lung, placenta, pancreas, liver, heart, and brain (6, 11, 25, 44, 51). Here, we demonstrate for the first time that human neurons constitutively express TLR-3. Immunocytochemistry confirms the transcriptome analysis findings that TLR-3 transcripts are present in NT2-N cells. TLR-3 is present mostly in the cytoplasm as cytoplasmic and perinuclear vesicles, as reported for human dendritic cells (44). In addition, there is an immunochemical indication that TLR-3 may also be present at the membrane. RABV infection seems to modify intracytoplasmic distribution of TLR-3, presumably by affecting TLR-3 trafficking, as proposed for TLR-9, which was rapidly redistributed from the reticulum to the lysosomal compartments of human dendritic cells when they had been treated with CpG DNA (39).
TLR-2 mRNAs were present in the NT2-N transcriptome. TLR-2 senses several human viruses, including cytomegalovirus, rubella virus, and HSV-1 and -2 (5, 22). Signaling through TLR-2 results in the activation of NF-κB and the stimulation of inflammatory cytokines, including IL-6. After HSV-1 infection, IL-6 transcripts were indeed upregulated in NT2-N cells, even though the increase was modest (doubling), suggesting that the increase of IL-6 transcription may reflect the engagement of TLR-2 in HSV-1 detection. Thus, the nature of the TLR expressed by human NT2-N cells supports the idea that human neurons have the machinery to sense RABV and HSV-1 infections. In contrast, NT2-N cells were not reactive to LPS, despite the presence of TLR-4 in the NT2-N transcriptome. This is consistent with a previous report indicating that the treatment of NT2-N cells with LPS did not result in any detectable TNF-α synthesis, whereas treatment with HTLV-1 Tax protein did (18), and is also consistent with the observation that mouse cortical neurons do not recognize fluorescent LPS (41). Since LPS is recognized by TLR-4 in association with CD14 and MD2, the inability of neurons to sense LPS may result of the default expression of one of these molecules (23).
We provide experimental evidence that human NT2-N cells can sense dsRNA and express genes coding for molecules which can sense dsRNA: NF-κB, RIG-1, and PKR (as transcripts) and TLR-3 (both mRNAs and protein). It is likely that dsRNAs are produced during RABV and HSV-1 infections, and indeed they are byproducts of almost all viral infections. Thus, dsRNA could be the main viral element sensed by human neurons as a trigger of an innate immune response. We do not know which of the group consisting of TLR-3, PKR, and RIG-1 is involved in this response. Despite the strong expression of TLR-3 in human neurons (Fig. 5B), it is possible that viral components other than dsRNA trigger the innate immune response. Were this the case, neurons would express receptors other than TLR-3 and -2 for sensing viral infection. Further analysis is required to resolve these issues.
The natures and dynamics of the genes recruited by RABV are consistent with the cascade of events of the innate immunity response (illustrated in Fig. 1), with the exception of the positive-feedback loop. Nevertheless, evidence for the involvement of some factors in RABV-induced innate immunity is lacking. For example, the phosphorylation of IRF-3 and the activation of NF-κB cannot be tested by the microarray technique. These points deserve further attention.
Our data clearly indicate that human neurons, in the absence of glia, have the intrinsic machinery to trigger a typical innate immune response, including the two-step interferon response during RABV infection. This is not the case after HSV-1 infection, to which NT2-N cells respond by upregulating a partial innate immune response with an increase of IL-6 gene transcripts only. The differing patterns of IFN production may reflect the natures of the TLR engaged by the two viruses: TLR-3 is associated with a strong stimulation of IFN-β, inflammatory cytokines, and chemokines in the case of RABV infection, and TLR-2 is associated with inflammatory cytokines only in the case of HSV-1 infection. However, if dsRNA is sensed by human neurons, the innate immune responses to the two viruses should be the same afterwards, because both should produce dsRNA (30). The absence of IFN-β production during HSV-1 infection may be a consequence of the mechanisms expressed by HSV-1 to block IFN production (13, 20, 24, 45, 50).
The decline of IFN-β transcription 24 h postinfection in RABV-infected NT2-N cells and the decrease of IFN-β in the supernatants of NT2-N cells infected with RABV for 48 h suggest that RABV may modulate IFN-β production at least in the late steps of infection. Conzelmann and colleagues propose that the P protein of RABV prevents the activation of IRF-3 (8a, 16). In addition, Fu et al., in a companion study in which they compared transcriptomes of mouse NS infected with strains of various pathogenicities, propose that pathogenic RABV controls IFN production in the NS (70a). Nevertheless, RABV seems not to entirely escape the antiviral response it triggers, since an antiviral role, albeit one of limited impact, has been described for IFN-β in RABV infection by Hooper and colleagues (28). RABV infection of human neurons triggers a typical antiviral immune response, with increases of 2′5′OAS-1, MxA, and GPB in particular, in addition to a response by IFN-β (43). The antiviral effects of MxA, 2′5′OAS-1, and GTPases have not been shown to limit RABV infection, but such a possibility cannot be excluded. RABV also upregulated the transcription of several chemokines, including CCL-5, -3, -4, and -20 and CXCL-11, -10, -9, and -3, the main function of which is to recruit and attract immune cells (38, 68). Nevertheless, RABV is one of the rare diseases with an almost 100% mortality rate, and it is intriguing that this virus is so neuroinvasive despite causing a strong innate immune response. A similar discrepancy has also been observed for Sindbis virus infection: the most virulent strain of Sindbis virus triggers the strongest production of CCL-5 mRNAs and Mx1 (32). It is possible that the strong early innate immune response observed in this in vitro study corresponds to an only moderate innate immune response in vivo because the response is modulated by pathogenic viral strains, as suggested by Wang et al. (70a). It is also possible that innate immunity is only one component of the subtle balance between the antiviral response of the host and viral virulence.
It is intriguing to note that RABV neuroinvasiveness requires the preservation of neuron integrity to support virus transport through the NS and virus replication (3, 4, 36, 37, 49, 67). In this scheme, neuroprotective factors should favor RABV neuroinvasiveness. Complementary to their inflammatory or antiviral effects, there is increasing evidence that TNF-α, IL-1, IL-6, CCL-5, and even IFN-α/β have neuroprotective functions (7, 14, 27, 29, 46, 55, 57). Thus, it is plausible that a strong innate immune response, as a consequence of the neuroprotective properties of its components, favors RABV neuroinvasiveness. This opens new avenues for the analysis of the possible relationship between neuroinflammation and neuroprotection. The infection of a human neuron-derivative cell line, NT2-N, by neuronotropic viruses, RABV in particular, is a powerful model system to dissect these new mechanisms of neuroprotection.
Acknowledgments
We thank C. Thibault and P. Kastner for microarray analysis; Lars Rogge for help with computer analysis; M. Ti-Sahar and R. Le Goffic for TLR-3 MAb and real-time PCR primers; M. Tardieu for CPME cells; A. Plonquet for Ntera-2clD/1; A. Créange for Betaferon; J.-M. Cavaillon, E. Meurs, I. Chaudieu, and S. Pellegrini for helpful discussions; and Z. Fu and K.-K. Conzelmann for communication of unpublished results.
This work was supported by institutional grants from Institut Pasteur.
REFERENCES
- 1.Akira, S., K. Takeda, and T. Kaisho. 2001. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat. Immunol. 2:675-680. [DOI] [PubMed] [Google Scholar]
- 2.Bachoo, R. M., R. S. Kim, K. L. Ligon, E. A. Maher, C. Brennan, N. Billings, S. Chan, C. Li, D. H. Rowitch, W. H. Wong, and R. A. DePinho. 2004. Molecular diversity of astrocytes with implications for neurological disorders. Proc. Natl. Acad. Sci. USA 101:8384-8389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baloul, L., S. Camelo, and M. Lafon. 2004. Up-regulation of Fas ligand (FasL) in the central nervous system: a mechanism of immune evasion by rabies virus. J. Neurovirol. 10:372-382. [DOI] [PubMed] [Google Scholar]
- 4.Baloul, L., and M. Lafon. 2003. Apoptosis and rabies virus neuroinvasion. Biochimie 85:777-788. [DOI] [PubMed] [Google Scholar]
- 5.Boehme, K. W., and T. Compton. 2004. Innate sensing of viruses by Toll-like receptors. J. Virol. 78:7867-7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boivin, G., Z. Coulombe, and S. Rivest. 2002. Intranasal herpes simplex virus type 2 inoculation causes a profound thymidine kinase dependent cerebral inflammatory response in the mouse hindbrain. Eur. J. Neurosci. 16:29-43. [DOI] [PubMed] [Google Scholar]
- 7.Bolin, L. M., R. Murray, N. W. Lukacs, R. M. Strieter, S. L. Kunkel, T. J. Schall, and K. B. Bacon. 1998. Primary sensory neurons migrate in response to the chemokine RANTES. J. Neuroimmunol. 81:49-57. [DOI] [PubMed] [Google Scholar]
- 8.Bottcher, T., M. von Mering, S. Ebert, U. Meyding-Lamade, U. Kuhnt, J. Gerber, and R. Nau. 2003. Differential regulation of Toll-like receptor mRNAs in experimental murine central nervous system infections. Neurosci. Lett. 344:17-20. [DOI] [PubMed] [Google Scholar]
- 8a.Brzózka, K. S. Finke, and K.-K. Conzelmann. 2005. Identification of the rabies virus alpha/beta interferon antagonist: phosphoprotein P interferes with phosphorylation of interferon regulatory factor 3. J. Virol. 79:7673-7681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bsibsi, M., R. Ravid, D. Gveric, and J. M. van Noort. 2002. Broad expression of Toll-like receptors in the human central nervous system. J. Neuropathol. Exp. Neurol. 61:1013-1021. [DOI] [PubMed] [Google Scholar]
- 10.Camelo, S., M. Lafage, and M. Lafon. 2000. Absence of the p55 Kd TNF-alpha receptor promotes survival in rabies virus acute encephalitis. J. Neurovirol. 6:507-518. [DOI] [PubMed] [Google Scholar]
- 11.Cario, E., and D. K. Podolsky. 2000. Differential alteration in intestinal epithelial cell expression of Toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect. Immun. 68:7010-7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carosella, E. D., P. Paul, P. Moreau, and N. Rouas-Freiss. 2000. HLA-G and HLA-E: fundamental and pathophysiological aspects. Immunol. Today 21:532-534. [PubMed] [Google Scholar]
- 13.Chee, A. V., and B. Roizman. 2004. Herpes simplex virus 1 gene products occlude the interferon signaling pathway at multiple sites. J. Virol. 78:4185-4196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng, B., S. Christakos, and M. P. Mattson. 1994. Tumor necrosis factors protect neurons against metabolic-excitotoxic insults and promote maintenance of calcium homeostasis. Neuron 12:139-153. [DOI] [PubMed] [Google Scholar]
- 15.Cheung, W. M., W. Y. Fu, W. S. Hui, and N. Y. Ip. 1999. Production of human CNS neurons from embryonal carcinoma cells using a cell aggregation method. BioTechniques 26:946-954. [DOI] [PubMed] [Google Scholar]
- 16.Conzelmann, K. K. 2005. Transcriptional activation of alpha/beta interferon genes: interference by nonsegmented negative-strand RNA viruses. J. Virol. 79:5241-5248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coughlan, C. M., C. M. McManus, M. Sharron, Z. Gao, D. Murphy, S. Jaffer, W. Choe, W. Chen, J. Hesselgesser, H. Gaylord, A. Kalyuzhny, V. M. Lee, B. Wolf, R. W. Doms, and D. L. Kolson. 2000. Expression of multiple functional chemokine receptors and monocyte chemoattractant protein-1 in human neurons. Neuroscience 97:591-600. [DOI] [PubMed] [Google Scholar]
- 18.Cowan, E. P., R. K. Alexander, S. Daniel, F. Kashanchi, and J. N. Brady. 1997. Induction of tumor necrosis factor alpha in human neuronal cells by extracellular human T-cell lymphotropic virus type 1 Tax. J. Virol. 71:6982-6989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cray, C., R. W. Keane, T. R. Malek, and R. B. Levy. 1990. Regulation and selective expression of Ly-6A/E, a lymphocyte activation molecule, in the central nervous system. Brain Res. Mol. Brain Res. 8:9-15. [DOI] [PubMed] [Google Scholar]
- 20.Duerst, R. J., and L. A. Morrison. 2004. Herpes simplex virus 2 virion host shutoff protein interferes with type I interferon production and responsiveness. Virology 322:158-167. [DOI] [PubMed] [Google Scholar]
- 21.Farina, C., M. Krumbholz, T. Giese, G. Hartmann, F. Aloisi, and E. Meinl. 2005. Preferential expression and function of Toll-like receptor 3 in human astrocytes. J. Neuroimmunol. 159:12-19. [DOI] [PubMed] [Google Scholar]
- 22.Finberg, R. W., and E. A. Kurt-Jones. 2004. Viruses and Toll-like receptors. Microbes Infect. 6:1356-1360. [DOI] [PubMed] [Google Scholar]
- 23.Fitzgerald, K. A., D. C. Rowe, and D. T. Golenbock. 2004. Endotoxin recognition and signal transduction by the TLR4/MD2-complex. Microbes Infect. 6:1361-1367. [DOI] [PubMed] [Google Scholar]
- 24.Goodbourn, S., L. Didcock, and R. E. Randall. 2000. Interferons: cell signalling, immune modulation, antiviral response and virus countermeasures. J Gen. Virol. 81:2341-2364. [DOI] [PubMed] [Google Scholar]
- 25.Guillot, L., R. Le Goffic, S. Bloch, N. Escriou, S. Akira, M. Chignard, and M. Si-Tahar. 2005. Involvement of Toll-like receptor 3 in the immune response of lung epithelial cells to double-stranded RNA and influenza A virus. J. Biol. Chem. 280:5571-5580. [DOI] [PubMed] [Google Scholar]
- 26.Guo, C. J., S. D. Douglas, J. P. Lai, D. E. Pleasure, Y. Li, M. Williams, P. Bannerman, L. Song, and W. Z. Ho. 2003. Interleukin-1beta stimulates macrophage inflammatory protein-1alpha and -1beta expression in human neuronal cells (NT2-N). J. Neurochem. 84:997-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirota, H., H. Kiyama, T. Kishimoto, and T. Taga. 1996. Accelerated nerve regeneration in mice by upregulated expression of interleukin (IL) 6 and IL-6 receptor after trauma. J Exp. Med. 183:2627-2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hooper, D. C., K. Morimoto, M. Bette, E. Weihe, H. Koprowski, and B. Dietzschold. 1998. Collaboration of antibody and inflammation in clearance of rabies virus from the central nervous system. J. Virol. 72:3711-3719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inoue, K. 2002. Microglial activation by purines and pyrimidines. Glia 40:156-163. [DOI] [PubMed] [Google Scholar]
- 30.Jacobs, B. L., and J. O. Langland. 1996. When two strands are better than one: the mediators and modulators of the cellular responses to double-stranded RNA. Virology 219:339-349. [DOI] [PubMed] [Google Scholar]
- 31.Janabi, N., S. Peudenier, B. Heron, K. H. Ng, and M. Tardieu. 1995. Establishment of human microglial cell lines after transfection of primary cultures of embryonic microglial cells with the SV40 large T antigen. Neurosci. Lett. 195:105-108. [DOI] [PubMed] [Google Scholar]
- 32.Johnston, C., W. Jiang, T. Chu, and B. Levine. 2001. Identification of genes involved in the host response to neurovirulent alphavirus infection. J. Virol. 75:10431-10445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kleppner, S. R., K. A. Robinson, J. Q. Trojanowski, and V. M. Lee. 1995. Transplanted human neurons derived from a teratocarcinoma cell line (NTera-2) mature, integrate, and survive for over 1 year in the nude mouse brain. J. Comp. Neurol. 357:618-632. [DOI] [PubMed] [Google Scholar]
- 34.Koedel, U., B. Angele, T. Rupprecht, H. Wagner, A. Roggenkamp, H. W. Pfister, and C. J. Kirschning. 2003. Toll-like receptor 2 participates in mediation of immune response in experimental pneumococcal meningitis. J. Immunol. 170:438-444. [DOI] [PubMed] [Google Scholar]
- 35.Kurt-Jones, E. A., M. Chan, S. Zhou, J. Wang, G. Reed, R. Bronson, M. M. Arnold, D. M. Knipe, and R. W. Finberg. 2004. Herpes simplex virus 1 interaction with Toll-like receptor 2 contributes to lethal encephalitis. Proc. Natl. Acad. Sci. USA 101:1315-1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lafon, M. 2005. Modulation of the immune response in the nervous system by rabies virus. Curr. Top. Microbiol. Immunol. 289:239-258. [DOI] [PubMed] [Google Scholar]
- 37.Lafon, M. 2004. Subversive neuroinvasive strategy of rabies virus. Arch. Virol. Suppl. 18:149-159. [DOI] [PubMed] [Google Scholar]
- 38.Lane, T. E., M. T. Liu, B. P. Chen, V. C. Asensio, R. M. Samawi, A. D. Paoletti, I. L. Campbell, S. L. Kunkel, H. S. Fox, and M. J. Buchmeier. 2000. A central role for CD4+ T cells and RANTES in virus-induced central nervous system inflammation and demyelination. J. Virol. 74:1415-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Latz, E., A. Schoenemeyer, A. Visintin, K. A. Fitzgerald, B. G. Monks, C. F. Knetter, E. Lien, N. J. Nilsen, T. Espevik, and D. T. Golenbock. 2004. TLR9 signals after translocating from the ER to CpG DNA in the lysosome. Nat. Immunol. 5:190-198. [DOI] [PubMed] [Google Scholar]
- 40.Le Bon, A., and D. F. Tough. 2002. Links between innate and adaptive immunity via type I interferon. Curr. Opin. Immunol. 14:432-436. [DOI] [PubMed] [Google Scholar]
- 41.Lehnardt, S., L. Massillon, P. Follett, F. E. Jensen, R. Ratan, P. A. Rosenberg, J. J. Volpe, and T. Vartanian. 2003. Activation of innate immunity in the CNS triggers neurodegeneration through a Toll-like receptor 4-dependent pathway. Proc. Natl. Acad. Sci. USA 100:8514-8519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li, Y., S. D. Douglas, D. E. Pleasure, J. Lai, C. Guo, P. Bannerman, M. Williams, and W. Ho. 2003. Human neuronal cells (NT2-N) express functional substance P and neurokinin-1 receptor coupled to MIP-1 beta expression. J. Neurosci. Res. 71:559-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacMicking, J. D. 2004. IFN-inducible GTPases and immunity to intracellular pathogens. Trends Immunol. 25:601-609. [DOI] [PubMed] [Google Scholar]
- 44.Matsumoto, M., K. Funami, M. Tanabe, H. Oshiumi, M. Shingai, Y. Seto, A. Yamamoto, and T. Seya. 2003. Subcellular localization of Toll-like receptor 3 in human dendritic cells. J. Immunol. 171:3154-3162. [DOI] [PubMed] [Google Scholar]
- 45.Melroe, G. T., N. A. DeLuca, and D. M. Knipe. 2004. Herpes simplex virus 1 has multiple mechanisms for blocking virus-induced interferon production. J. Virol. 78:8411-8420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meucci, O., A. Fatatis, A. A. Simen, T. J. Bushell, P. W. Gray, and R. J. Miller. 1998. Chemokines regulate hippocampal neuronal signaling and gp120 neurotoxicity. Proc. Natl. Acad. Sci. USA 95:14500-14505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meurs, E., K. Chong, J. Galabru, N. S. Thomas, I. M. Kerr, B. R. Williams, and A. G. Hovanessian. 1990. Molecular cloning and characterization of the human double-stranded RNA-activated protein kinase induced by interferon. Cell 62:379-390. [DOI] [PubMed] [Google Scholar]
- 48.Miettinen, M., T. Sareneva, I. Julkunen, and S. Matikainen. 2001. IFNs activate Toll-like receptor gene expression in viral infections. Genes Immun. 2:349-355. [DOI] [PubMed] [Google Scholar]
- 49.Morimoto, K., D. C. Hooper, S. Spitsin, H. Koprowski, and B. Dietzschold. 1999. Pathogenicity of different rabies virus variants inversely correlates with apoptosis and rabies virus glycoprotein expression in infected primary neuron cultures. J. Virol. 73:510-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mossman, K. 2005. Analysis of anti-interferon properties of the herpes simplex virus type I ICP0 protein. Methods Mol. Med. 116:195-205. [DOI] [PubMed] [Google Scholar]
- 51.Muzio, M., D. Bosisio, N. Polentarutti, G. D'Amico, A. Stoppacciaro, R. Mancinelli, C. van't Veer, G. Penton-Rol, L. P. Ruco, P. Allavena, and A. Mantovani. 2000. Differential expression and regulation of Toll-like receptors (TLR) in human leukocytes: selective expression of TLR3 in dendritic cells. J. Immunol. 164:5998-6004. [DOI] [PubMed] [Google Scholar]
- 52.Nguyen, M. D., J. P. Julien, and S. Rivest. 2002. Innate immunity: the missing link in neuroprotection and neurodegeneration? Nat. Rev. Neurosci. 3:216-227. [DOI] [PubMed] [Google Scholar]
- 53.O'Neill, L. A., K. A. Fitzgerald, and A. G. Bowie. 2003. The Toll-IL-1 receptor adaptor family grows to five members. Trends Immunol. 24:286-290. [DOI] [PubMed] [Google Scholar]
- 54.Paquet-Durand, F., S. Tan, and G. Bicker. 2003. Turning teratocarcinoma cells into neurons: rapid differentiation of NT-2 cells in floating spheres. Brain Res. Dev. Brain Res. 142:161-167. [DOI] [PubMed] [Google Scholar]
- 55.Pizzi, M., I. Sarnico, F. Boroni, M. Benarese, M. Dreano, G. Garotta, A. Valerio, and P. Spano. 2004. Prevention of neuron and oligodendrocyte degeneration by interleukin-6 (IL-6) and IL-6 receptor/IL-6 fusion protein in organotypic hippocampal slices. Mol. Cell. Neurosci. 25:301-311. [DOI] [PubMed] [Google Scholar]
- 56.Pleasure, S. J., C. Page, and V. M. Lee. 1992. Pure, postmitotic, polarized human neurons derived from NTera 2 cells provide a system for expressing exogenous proteins in terminally differentiated neurons. J. Neurosci. 12:1802-1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Plioplys, A. V., and N. Massimini. 1995. Alpha/beta interferon is a neuronal growth factor. Neuroimmunomodulation 2:31-35. [DOI] [PubMed] [Google Scholar]
- 58.Sato, M., N. Tanaka, N. Hata, E. Oda, and T. Taniguchi. 1998. Involvement of the IRF family transcription factor IRF-3 in virus-induced activation of the IFN-beta gene. FEBS Lett. 425:112-116. [DOI] [PubMed] [Google Scholar]
- 59.Scolding, N. J., S. Frith, C. Linington, B. P. Morgan, A. K. Campbell, and D. A. Compston. 1989. Myelin-oligodendrocyte glycoprotein (MOG) is a surface marker of oligodendrocyte maturation. J. Neuroimmunol. 22:169-176. [DOI] [PubMed] [Google Scholar]
- 60.Sharma, S., B. R. tenOever, N. Grandvaux, G. P. Zhou, R. Lin, and J. Hiscott. 2003. Triggering the interferon antiviral response through an IKK-related pathway. Science 300:1148-1151. [DOI] [PubMed] [Google Scholar]
- 61.Skare, J., W. P. Summers, and W. C. Summers. 1975. Structure and function of herpesvirus genomes. I. Comparison of five HSV-1 and two HSV-2 strains by cleavage of their DNA with Eco R I restriction endonuclease. J. Virol. 15:726-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Takaoka, A., and T. Taniguchi. 2003. New aspects of IFN-alpha/beta signalling in immunity, oncogenesis and bone metabolism. Cancer Sci. 94:405-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Takeda, K., and S. Akira. 2004. TLR signaling pathways. Semin. Immunol. 16:3-9. [DOI] [PubMed] [Google Scholar]
- 64.Taniguchi, T., and A. Takaoka. 2002. The interferon-alpha/beta system in antiviral responses: a multimodal machinery of gene regulation by the IRF family of transcription factors. Curr. Opin. Immunol. 14:111-116. [DOI] [PubMed] [Google Scholar]
- 65.tenOever, B. R., S. Sharma, W. Zou, Q. Sun, N. Grandvaux, I. Julkunen, H. Hemmi, M. Yamamoto, S. Akira, W. C. Yeh, R. Lin, and J. Hiscott. 2004. Activation of TBK1 and IKKε kinases by vesicular stomatitis virus infection and the role of viral ribonucleoprotein in the development of interferon antiviral immunity. J. Virol. 78:10636-10649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thoulouze, M. I., M. Lafage, J. A. Montano-Hirose, and M. Lafon. 1997. Rabies virus infects mouse and human lymphocytes and induces apoptosis. J. Virol. 71:7372-7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thoulouze, M. I., M. Lafage, V. J. Yuste, G. Kroemer, S. A. Susin, N. Israel, and M. Lafon. 2003. Apoptosis inversely correlates with rabies virus neurotropism. Ann. N. Y. Acad. Sci. 1010:598-603. [DOI] [PubMed] [Google Scholar]
- 68.Trifilo, M. J., C. Montalto-Morrison, L. N. Stiles, K. R. Hurst, J. L. Hardison, J. E. Manning, P. S. Masters, and T. E. Lane. 2004. CXC chemokine ligand 10 controls viral infection in the central nervous system: evidence for a role in innate immune response through recruitment and activation of natural killer cells. J. Virol. 78:585-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Trojanowski, J. Q., S. R. Kleppner, R. S. Hartley, M. Miyazono, N. W. Fraser, S. Kesari, and V. M. Lee. 1997. Transfectable and transplantable postmitotic human neurons: a potential “platform” for gene therapy of nervous system diseases. Exp. Neurol. 144:92-97. [DOI] [PubMed] [Google Scholar]
- 70.Underhill, D. M., and A. Ozinsky. 2002. Toll-like receptors: key mediators of microbe detection. Curr. Opin. Immunol. 14:103-110. [DOI] [PubMed] [Google Scholar]
- 70a.Wang, Z. W., L. Sarmento, Y. Wang, X.-Q. Li, V. Dhingra, T. Tseggai, B. Jiang, and Z. F. Fu. 2005. Attenuated rabies virus activates, while pathogenic rabies virsu evades, the host innate immune responses in the central nervous system. J. Virol. 79:12555-12566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wright, G. J., M. J. Puklavec, A. C. Willis, R. M. Hoek, J. D. Sedgwick, M. H. Brown, and A. N. Barclay. 2000. Lymphoid/neuronal cell surface OX2 glycoprotein recognizes a novel receptor on macrophages implicated in the control of their function. Immunity 13:233-242. [DOI] [PubMed] [Google Scholar]
- 72.Yoneyama, M., M. Kikuchi, T. Natsukawa, N. Shinobu, T. Imaizumi, M. Miyagishi, K. Taira, S. Akira, and T. Fujita. 2004. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat. Immunol. 5:730-737. [DOI] [PubMed] [Google Scholar]
- 73.Younkin, D. P., C. M. Tang, M. Hardy, U. R. Reddy, Q. Y. Shi, S. J. Pleasure, V. M. Lee, and D. Pleasure. 1993. Inducible expression of neuronal glutamate receptor channels in the NT2 human cell line. Proc. Natl. Acad. Sci. USA 90:2174-2178. [DOI] [PMC free article] [PubMed] [Google Scholar]