Abstract
Background
Intussusception is a common cause of bowel obstruction in children, often requiring prompt intervention to prevent complications. While non-surgical reduction is the preferred treatment, some patients require surgical management. Identifying factors associated with the need for surgery is essential to optimize patient outcomes. This study aimed to examine the clinical and paraclinical differences between pediatric patients who received surgical versus non-surgical treatment for intussusception.
Methods
This retrospective study reviewed the medical records of pediatric patients diagnosed with intussusception at the Children’s Medical Center, Tehran, Iran, between April 2018 and March 2020. Out of 571 pediatric patients diagnosed with intussusception, 165 were included in the analysis—55 who underwent surgery and 110 who were treated non-surgically. Demographic, clinical, and laboratory data were analyzed to identify factors influencing surgical intervention. Statistical analyses were performed using independent t-tests, chi-square tests, and Fisher’s exact tests, with significance set at P < 0.05.
Results
Patients who underwent surgery were significantly younger than those treated non-surgically (2.68 ± 1.65 vs. 3.88 ± 3.51 years; P < 0.001), with a higher proportion of cases under one year of age (P = 0.004). Laboratory parameters, including white blood cell count (P = 0.53), erythrocyte sedimentation rate (P = 0.69), and C-reactive protein levels (P = 0.55), did not differ significantly between the groups. Among clinical symptoms, the presence of bloody stools was significantly associated with surgical intervention (P < 0.001). Sonographic findings showed that ileocolic intussusception was more common in the surgical group (P < 0.001).
Conclusion
Younger age, the presence of bloody stools, and ileocolic intussusception were associated with a higher likelihood of surgical reduction in pediatric intussusception. Recognizing these risk factors may facilitate early diagnosis and support better treatment decision-making.
Keywords: Intussusception, Pediatrics, Surgery, Risk factors
Introduction
Intussusception is a common cause of intestinal obstruction in infants and young children [1]. It occurs when a segment of the intestine telescopes into an adjacent segment, resulting in obstruction of the bowel lumen, compression of blood vessels, and potentially ischemic injury to the affected tissue [2, 3]. Early diagnosis and prompt management are essential to prevent serious complications, including intestinal necrosis, perforation, peritonitis, and sepsis [4, 5].
Intussusception most commonly affects infants between 4 and 10 months of age. It is more frequent in boys, who represent approximately two-thirds of cases [6]. The annual incidence ranges from 3 to 40 cases per 10,000 live births [7].
The classic triad of symptoms includes intermittent colicky abdominal pain, vomiting, and bloody stools (often described as “currant jelly” stools due to the presence of blood and mucus) [8, 9]. However, these symptoms are not present in all patients, which can contribute to diagnostic delays [7]. Other symptoms include lethargy, fever, dehydration, and a palpable abdominal mass [10].
Diagnosis is typically based on clinical evaluation supported by imaging studies. Abdominal ultrasound is the preferred imaging modality due to its non-invasive nature and ease of use [3, 11]. The characteristic “target sign” or “doughnut sign” seen on ultrasound is a reliable indicator of intussusception [12, 13]. In some cases, abdominal X-rays may show signs of bowel obstruction, such as dilated loops of bowel, air-fluid levels, and absence of gas in the distal colon, but plain radiography is less sensitive than ultrasound [14, 15]. Laboratory investigations play a supportive role in the diagnosis and management of this condition. Leukocytosis, elevated C-reactive protein (CRP), and electrolyte imbalances may indicate inflammation, dehydration, or metabolic disturbances [3, 16].
Treatment depends on the severity of the condition and the feasibility of non-surgical reduction [17]. The preferred initial approach for stable patients without signs of bowel perforation is non-operative reduction using hydrostatic (saline or contrast) or pneumatic (air) enema under fluoroscopic guidance or ultrasound monitoring [18–20]. These techniques are highly effective and can significantly reduce the necessity for surgical intervention [21]. In this context, a study from Japan reported a 77.5% success rate for hydrostatic enema reduction of intussusception on the first attempt [22]. However, in cases where non-surgical reduction fails, or if there is evidence of bowel perforation, peritonitis, or hemodynamic instability, surgical intervention becomes necessary [23, 24]. Surgical approaches include manual reduction of the intussuscepted segment or, in cases of necrotic or nonviable bowel, resection with anastomosis [25, 26].
While several studies have investigated the epidemiology, diagnosis, and treatment of intussusception [3, 27–30], few studies have specifically examined the clinical and paraclinical characteristics of children who ultimately require surgery. The clinical presentation of intussusception can vary significantly, and delays in diagnosis can increase the risk of complications. Additionally, laboratory markers such as leukocytosis and CRP elevation may provide valuable insights into disease severity and the need for surgical management. A detailed analysis of clinical and paraclinical features in surgically treated intussusception cases can help improve early recognition, optimize preoperative assessment, and guide clinical decision-making. Identifying factors associated with failed non-surgical reduction may also aid in developing predictive models for surgical intervention. This retrospective study aimed to compare clinical and paraclinical characteristics between pediatric patients treated surgically and those managed non-surgically for intussusception.
Materials and methods
Study design and setting
This retrospective study was conducted by reviewing the medical records of patients admitted with intussusception at the Children’s Medical Center, affiliated with Tehran University of Medical Sciences, Tehran, Iran, from April 2018 to March 2020. The Children’s Medical Center is a referral hospital that provides care for pediatric patients from across Iran. The diverse population referring to this hospital provides a representative sample from various regions, ensuring a broad and comprehensive dataset for this study.
Participants
The study population included all pediatric patients diagnosed with intussusception who were admitted to the Children’s Medical Center. The inclusion criteria were patients with a confirmed diagnosis of intussusception through clinical evaluation and imaging results, such as ultrasound. Patients were excluded if their medical records were incomplete.
Sample size
To assess the differences between pediatric patients receiving surgical and non-surgical interventions for intussusception, continuous variables were considered as the primary variables. The sample size calculation was performed using G*Power software version 3.1, based on Cohen’s d for effect size, with a power of 0.80 (β = 0.80) and a significance level of 0.05 (α = 0.05). Assuming a medium effect size of 0.5, the minimum sample size required in each group was calculated to be 63 participants [31]. However, the surgical intervention group had 55 participants. To ensure sufficient statistical power, the non-surgical treatment group was increased to 110 participants. With a 1:2 ratio between the surgical and non-surgical groups, the study design provided adequate power to detect meaningful differences between the groups. The power analysis for the final sample size showed an achieved power of approximately 0.85, which is above the acceptable threshold of 0.80.
Data collection
The data collection process was conducted by two trained researchers (BG and ZS) to ensure consistency and minimize potential errors. Any discrepancies were resolved through discussion with two additional researchers (ZZ and HA). To better assess the differences between patients requiring surgical and non-surgical interventions, data from patients prior to surgery and at admission were collected. This allowed for a more comprehensive understanding of the clinical and paraclinical differences between the two groups.
The data collected for this study included patient demographics such as age and gender. Clinical data encompassed the location of the intussusception (determined by sonographic results), and the presence of clinical symptoms, including abdominal pain, fever, vomiting, and bloody stools. Paraclinical data collected included laboratory results such as white blood cell count (WBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels.
The data were entered into Microsoft Excel 2007. After collecting data from all patients, it was found that 55 patients had received surgical interventions. These patients were considered the surgical intervention group. Additionally, 110 patients who did not receive surgical interventions were randomly selected using Excel. These patients were considered the non-surgical intervention group. Non-surgical interventions included hydrostatic or pneumatic reduction techniques, and monitoring with nil per os (NPO) status.
The choice of reduction method was made on a case-by-case basis by the attending physicians. This decision often involved consultation with members of the care team, particularly pediatric surgeons and radiologists. It was based on clinical judgment and the patient’s overall condition. Although non-surgical reduction is generally preferred as a first-line treatment, there were no standardized or universally accepted criteria in the research setting to guide the selection between hydrostatic and pneumatic methods.
Statistical analysis
All statistical analyses were performed using SPSS version 24 (IBM Corp., Armonk, NY, USA). The normality of continuous variables was assessed and confirmed using the Kolmogorov-Smirnov test. Descriptive statistics were used to summarize the data, with continuous variables reported as mean ± standard deviation and categorical variables presented as frequencies and percentages. To compare continuous variables between the two groups, an independent t-test was used. For categorical variables, the chi-square test was applied to examine the association between group categories. In cases where the expected frequency was less than 5, Fisher’s exact test was used. The significance level was set at P < 0.05.
Results
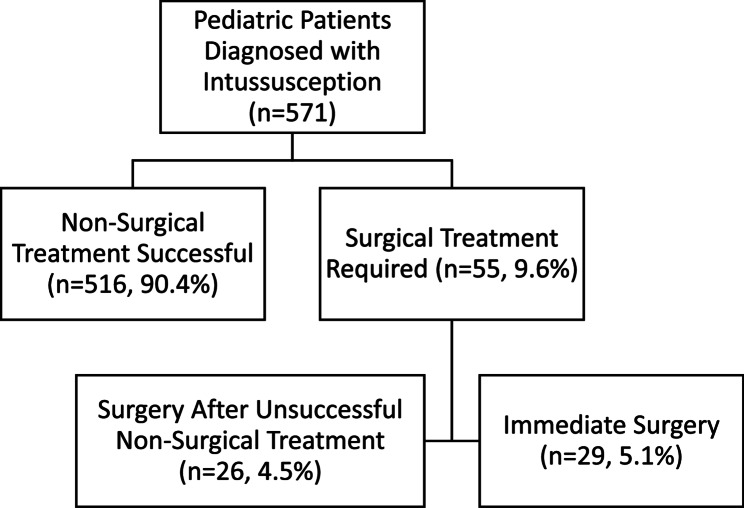
During the study period, 571 pediatric patients were diagnosed with intussusception. Among them, 516 (90.4%) were successfully treated with non-surgical methods, while 55 (9.6%) required surgical intervention. Of the surgical group, 29 underwent immediate surgery following diagnosis, and 26 underwent surgery after unsuccessful non-surgical treatment (Fig. 1).
Fig. 1.
Treatment approach for pediatric patients with intussusception
The mean age was 2.68 ± 1.65 years in the surgical group and 3.88 ± 3.51 years in the non-surgical group, with a statistically significant difference (P < 0.001), indicating that younger patients were more likely to require surgery. A significantly higher proportion of patients in the surgical group were under 1 year of age compared to the non-surgical group (P = 0.004). Gender distribution was similar between groups: 69.1% males in the surgical group versus 70.9% in the non-surgical group (P = 0.81).
Laboratory test results showed no significant differences between groups. The mean white blood cell count was 11.86 × 10³ ± 4.60 cells/mm³ in the surgical group and 11.47 × 10³ ± 3.89 cells/mm³ in the non-surgical group (P = 0.53). The mean ESR was 17.17 ± 9.48 mm/hr versus 16.34 ± 11.27 mm/hr (P = 0.69), and the mean CRP was 20.86 ± 17.87 mg/L versus 28.41 ± 14.66 mg/L (P = 0.55) in the surgical and non-surgical groups, respectively.
Symptom analysis revealed no significant difference in the incidence of fever (25.5% vs. 29.1%, P = 0.62) or vomiting (69.1% vs. 60.9%, P = 0.30) between surgical and non-surgical groups. However, a significantly higher proportion of patients in the surgical group reported bloody stools compared to the non-surgical group (38.2% vs. 10.0%, P < 0.001).
Regarding intussusception location, a significant difference was observed (P < 0.001). Ileocolic intussusception was more common in the surgical group (80.0%) compared to the non-surgical group (61.9%). The non-surgical group had a higher proportion of cases in the right lower quadrant (10.9% vs. 0%) and right upper quadrant (15.5% vs. 3.6%) (Table 1).
Table 1.
Comparison of demographic and clinical characteristics between surgical and Non-Surgical groups
| Variable | Surgical intervention (Mean ± SD) |
Non-Surgical intervention (Mean ± SD) |
P value |
|---|---|---|---|
| Age (years) | 2.68 ± 1.65 | 3.88 ± 3.51 | < 0.001* |
| WBC (×103 cells/mm3) | 11.86 ± 4.60 | 11.47 ± 3.89 | 0.53* |
| ESR (mm/hr) | 17.17 ± 9.48 | 16.34 ± 11.27 | 0.69* |
| CRP (mg/L) | 20.86 ± 17.87 | 28.41 ± 14.66 | 0.55* |
| N (%) | N (%) | ||
| Gender | |||
| Male | 38 (69.1%) | 78 (70.9%) | 0.81** |
| Female | 17 (30.9%) | 32 (29.1%) | |
| Age Subgroups | |||
| > 1 year | 22 (40.0%) | 21 (19.1%) | 0.004** |
| < 1 year | 33 (60.0%) | 89 (80.9%) | |
| Location of the intussusception | |||
| Ileo-Ileal | 3 (5.5%) | 5 (4.5%) | < 0.001*** |
| Ileocolic | 44 (80.0%) | 68 (61.9%) | |
| Colocolic | 0 (0.0%) | 2 (1.8%) | |
| Right Lower Quadrant (RLQ) | 0 (0.0%) | 12 (10.9%) | |
| Right Upper Quadrant (RUQ) | 2 (3.6%) | 17 (15.5%) | |
| Left Lower Quadrant (LLQ) | 1 (1.8%) | 2 (1.8%) | |
| Left Upper Quadrant (LUQ) | 0 (0.0%) | 1 (0.9%) | |
| Jejunojenunal | 0 (0.0%) | 3 (2.7%) | |
| Jejuno-Ileal | 1 (1.8%) | 0 (0.0%) | |
| Multiple | 4 (7.3%) | 0 (0.0%) | |
| Abdominal pain | |||
| Yes | 55 (100.0%) | 110 (100.0%) | 1*** |
| No | 0 (0.0%) | 0 (0.0%) | |
| Fever | |||
| Yes | 14 (25.5%) | 32 (29.1%) | 0.62** |
| No | 41 (74.5%) | 78 (70.9%) | |
| Vomiting | |||
| Yes | 38 (69.1%) | 67 (60.9%) | 0.30** |
| No | 17 (30.9%) | 43 (39.1%) | |
| Bloody stools | |||
| Yes | 21 (38.2%) | 11 (10.0%) | < 0.001** |
| No | 34 (61.8%) | 99 (90.0%) | |
SD Standard deviation
*Independent samples t-test
**Chi-squared test
***Fisher’s exact test
Discussion
This study examined clinical and paraclinical differences between pediatric patients with intussusception who underwent surgical versus non-surgical treatment. The findings provide insights that may support early clinical decision-making and reduce unnecessary delays in treatment.
Age and need for surgery
The results showed that patients in the surgical group were younger than those in the non-surgical group. This suggests that younger age is associated with a higher likelihood of requiring surgery. The immature intestinal structure in younger children may contribute to the lower success rate of non-surgical reduction [32]. Consistent with our findings, previous studies from Thailand [23], China [33, 34], and Saudi Arabia [32] have reported higher surgical intervention rates among younger children and greater failure of enema reductions in those under one year of age.
Laboratory markers
Our analysis found no significant difference in WBC, ESR, or CRP levels between the two groups. A possible reason for this finding is that these inflammatory markers are non-specific and may be elevated in various conditions, reducing their diagnostic value in predicting the need for surgery. Supporting evidence from studies in China [34] and South Korea [35] also reported no association between these markers and hydrostatic or pneumatic reduction failure.
Gender
No association was found between gender and treatment type. Although intussusception is more common in males [32], gender did not influence the likelihood of requiring surgery. This is in line with previous studies from Poland [19] and China [34, 36] that also reported no significant role of gender in reduction success or recurrence rates.
Location of intussusception
Ileocolic intussusception was the most common type across both groups. However, patients with masses in the RUQ or RLQ were more likely to undergo non-surgical management, while ileocolic cases more frequently required surgery. These findings are consistent with reports from China [34] indicating better outcomes with hydrostatic reduction when the mass is located on the right side of the abdomen.
Clinical symptoms
Abdominal pain and vomiting were common in both groups, with no significant differences. Fever was rare and also showed no association with treatment type. However, bloody stools were significantly more frequent in the surgical group. This symptom may serve as a clinical marker of disease severity and predict the need for surgery. Studies from China [34] and India [37] have similarly identified rectal bleeding as a predictor of failed non-surgical reduction. Similarly, Alsinan et al. (2024) found that fever was not linked to the failure of enema reduction [32].
Implications of findings
This study found that younger age and the presence of bloody stools may suggest a higher risk of surgical intervention. These indicators should be considered during early assessment to prioritize surgical consultation. Recognizing that RUQ and RLQ intussusceptions are more amenable to non-surgical treatment may help guide the initial approach. Additionally, reliance on WBC, ESR, and CRP as decision-making tools should be reconsidered, as these markers lack discriminatory power in this context.
Strengths and limitations
This study offers several strengths that support the reliability of its findings. First, it was conducted at a pediatric referral center, which provided a diverse sample from different regions of Iran and enhanced the generalizability of the results. Second, data were collected through a rigorous process by trained researchers, reducing errors and improving data accuracy. Third, the study included a wide range of clinical and paraclinical variables—such as demographic characteristics, sonographic findings, laboratory markers, and clinical symptoms—offering a comprehensive view of factors associated with surgical versus non-surgical management of intussusception. Furthermore, the 1:2 ratio between surgical and non-surgical groups increased the statistical power to detect meaningful differences.
Despite these strengths, several limitations should be noted. As a retrospective study, it was limited by the quality and completeness of medical records, which may have led to inconsistent data. For example, some sonographic reports described only the region (e.g., “RLQ mass”), while others specified the type (e.g., “ileocolic intussusception”). This variation in reporting limited the uniformity of data classification and analysis. The study was also conducted at a single center, which may affect the generalizability of the results to other settings with different treatment practices. In addition, the study relied on general inflammatory markers (WBC, ESR, CRP) rather than more specific biomarkers, which may have limited its ability to identify stronger predictors of surgical need. Finally, although the sample size was statistically adequate, the relatively small number of surgical cases (n = 55) may have limited the ability to detect smaller effects.
Future research
Future research should focus on prospective multicenter studies to validate the findings in diverse healthcare settings and reduce the limitations of retrospective data collection. Additionally, studies should explore more advanced biomarkers or imaging techniques to improve early prediction of surgical intervention. Investigating long-term outcomes of different treatment strategies could provide valuable insights into optimizing management approaches for pediatric intussusception. Finally, machine learning and predictive modeling approaches could be utilized to develop risk stratification tools based on a combination of clinical and laboratory parameters.
Conclusion
In this study, younger age was associated with a higher likelihood of surgical intervention, which may reflect greater clinical severity or anatomical factors. Gender showed no significant association with treatment type. Laboratory markers such as WBC, ESR, and CRP did not differentiate between surgical and non-surgical cases. Bloody stools were significantly more common in patients who needed surgery. The location of intussusception was also linked to treatment: ileocolic cases were more frequent in the surgical group, while right upper and right lower quadrant intussusceptions were more often treated non-surgically. These findings can help guide clinical decisions. Future research should focus on improving imaging for early diagnosis and testing new non-surgical treatments to enhance patient outcomes.
Acknowledgements
The authors would like to sincerely thank the authorities at the Children's Medical Center Hospital for their invaluable support and collaboration throughout the study. We also wish to express our deep appreciation to Mrs. Mirzakhani and all others who contributed to the development and publication of this article.
Authors’ contributions
ZS: Sampling and data interpretation; SM: Study design and drafting; MMR: Study design, data analysis, data interpretation, and drafting; ZZ: Study design and data analysis; HA: Study design and data analysis; BG: Corresponding author, Study design, data analysis, data interpretation, and drafting; All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
The data generated and analyzed during the current study is not publicly available but is available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval for this study was granted by the Ethics Committee of Tehran University of Medical Sciences (Approval No. IR.TUMS.CHMC.REC.1399.177). The research adhered to the ethical principles outlined in the Declaration of Helsinki. The requirement for informed consent was waived by the Ethics Committee of Tehran University of Medical Sciences due to the retrospective nature of the study. To ensure confidentiality, all patient data were anonymized, and no personal identifying details were collected or recorded.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bradshaw CJ, Johnson P, Intussusception. Surg (Oxford). 2022;40(5):311–5. 10.1016/j.mpsur.2022.03.001. [Google Scholar]
- 2.Mazzotta E, Lauricella S, Carannante F, Mascianà G, Caricato M, Capolupo G. Ileo-ileal intussusception caused by small bowel leiomyosarcoma: a very rare case report. Int J Surg Case Rep. 2020;72. 10.1016/j.ijscr.2020.05.049. [DOI] [PMC free article] [PubMed]
- 3.Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg. 2017;30(1):30–9. 10.1055/s-0036-1593429. PubMed PMID: 28144210; PubMed Central PMCID: PMC5179276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charles T, Penninga L, Reurings J, Berry M. Intussusception in children: A clinical review. Acta Chir Belg. 2015;115:327–33. 10.1080/00015458.2015.11681124. [DOI] [PubMed] [Google Scholar]
- 5.Zhu J, Cheng W, Xu Y, Guo Y, Shi L. Two cases of small bowel necrosis due to intussusception secondary to abnormal proliferation of intestinal peyer’s patches in infants after MMR vaccination. BMC Pediatr. 2024;24:147. 10.1186/s12887-024-04618-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu N, Yen C, Huang T, Cui P, Tate JE, Jiang B, et al. Incidence and epidemiology of intussusception among children under 2 years of age in Chenzhou and kaifeng, china, 2009–2013. Vaccine. 2018;36(51):7862–7. 10.1016/j.vaccine.2018.02.032. Epub 20180210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Zhou Q, Liu C, Sun C, Sun H, Li X, Zhang L. Epidemiology, clinical characteristics, and treatment of children with acute intussusception: a case series. BMC Pediatr. 2023;23(1):143. 10.1186/s12887-023-03961-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang WC, Chen CY, Wu HP. Etiology of non-traumatic acute abdomen in pediatric emergency departments. World J Clin Cases. 2013;1(9):276–84. 10.12998/wjcc.v1.i9.276. PubMed PMID: 24364022; PubMed Central PMCID: PMC3868711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strobel S, Ben-Yakov M, Tessaro MO, Boutis K, Intwosusception. Case report of 2 sisters presenting simultaneously with intussusception. Can Fam Physician. 2017;63(11):863–5. PubMed PMID: 29138157; PubMed Central PMCID: PMC5685448. [PMC free article] [PubMed] [Google Scholar]
- 10.Oh YR, Je BK, Oh C, Cha JH, Lee JH. Pediatr Gastroenterol Hepatol Nutr. 2021;24(2):135–44. 10.5223/pghn.2021.24.2.135. Epub 20210304. Suspecting Intussusception and Recurrence Risk Stratification Using Clinical Data and Plain Abdominal Radiographs. [DOI] [PMC free article] [PubMed]
- 11.Otero HJ, De Leon Benedetti LS, Applegate KE. Intussusception in children: diagnostic imaging and treatment. In: Otero HJ, Kaplan SL, Medina LS, Blackmore CC, Applegate KE, editors. Evidence-Based imaging in pediatrics: clinical decision support for optimized imaging in pediatric care. Cham: Springer International Publishing; 2024. pp. 623–38. [Google Scholar]
- 12.Yadav Ak, Regmi PR, Koirala B, adhikari B, Panthi B. The double target sign as ultrasonographic finding in a case of double intussusception: A case report. Radiol Case Rep. 2024;19(5):1990–3. 10.1016/j.radcr.2024.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegel MJ, Lee EY. CHAPTER 70 - Paediatric bowel and mesentery. In: Allan PL, Baxter GM, Weston MJ, editors. Clinical ultrasound (Third Edition). Edinburgh: Churchill Livingstone; 2011. pp. 1383–405. [Google Scholar]
- 14.Plut D, Phillips GS, Johnston PR, Lee EY. Practical imaging strategies for intussusception in children. AJR Am J Roentgenol. 2020;215(6):1449–63. 10.2214/ajr.19.22445. Epub 20201021. [DOI] [PubMed] [Google Scholar]
- 15.Guo WL, Wang J, Zhou M, Sheng M, Fang L. The role of plain radiography in assessing intussusception with vascular compromise in children. Arch Med Sci. 2011;7(5):877–81. 10.5114/aoms.2011.25565. Epub 20111108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen B, Cao J, Yan C, Zheng C, Chen J, Guo C. A promising new predictive factor for detecting bowel resection in childhood intussusception: the lymphocyte-C-reactive protein ratio. BMC Pediatr. 2021;21(1):577. 10.1186/s12887-021-03068-2. Epub 20211216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Güney LH, Fakıoğlu E, Acer T, Ötgün İ, Arslan EE, Sağnak Akıllı M, Hiçsönmez A. Is every intussusception treatment an emergency intervention or surgery? Ulus Travma Acil Cerrahi Derg. 2016;22(2):139–44. PubMed PMID: 27193980. [DOI] [PubMed] [Google Scholar]
- 18.Hwang J, Yoon HM, Kim PH, Jung AY, Lee JS, Cho YA. Current diagnosis and image-guided reduction for intussusception in children. Clin Exp Pediatr. 2023;66(1):12–21. 10.3345/cep.2021.01816. Epub 20220704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chrapusta MK, Preinl M, Łubniewska Z, Procháska F, Gruba M, Górecki W. Predictive factors for failure of nonsurgical management of intussusception and its in-hospital recurrence in pediatric patients: a large retrospective single-center study. Egypt Pediatr Association Gaz. 2024;72(1):38. 10.1186/s43054-024-00279-x. [Google Scholar]
- 20.Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. Cochrane Database Syst Rev. 2017;6(6). 10.1002/14651858.CD006476.pub3. Epub 20170601. Cd006476. [DOI] [PMC free article] [PubMed]
- 21.Tang XB, Zhao JY, Bai YZ. Status survey on enema reduction of paediatric intussusception in China. J Int Med Res. 2019;47(2):859–66. Epub 20181216. doi: 10.1177/0300060518814120. PubMed PMID: 30556437; PubMed Central PMCID: PMC6381501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yatabe R, Kishibe S, Akahoshi S, Shimojima N, Sakakibara H. Success rate and predictors of failure of enema reduction of intussusception in children with a water-soluble contrast medium at a height of 120 cm or less. Pediatr Int. 2024;66(1):e15824. 10.1111/ped.15824. [DOI] [PubMed] [Google Scholar]
- 23.Khorana J, Singhavejsakul J, Ukarapol N, Laohapensang M, Siriwongmongkol J, Patumanond J. Prognostic indicators for failed nonsurgical reduction of intussusception. Ther Clin Risk Manag. 2016;12:1231–7. 10.2147/tcrm.S109785. Epub 20160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelley-Quon LI, Arthur LG, Williams RF, Goldin AB, St Peter SD, Beres AL, et al. Management of intussusception in children: A systematic review. J Pediatr Surg. 2021;56(3):587–96. 10.1016/j.jpedsurg.2020.09.055. Epub 20201006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang H, Li H, Xin W, Xu L, Zhang G, Yan Q. Surgical treatment of recurrent intussusception induced by intestinal lymphoid hyperplasia in a child: is bowel resection always necessary? A case report. BMC Surg. 2022;22(1):169. 10.1186/s12893-022-01608-w. Epub 20220510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uddin W, Gupta V, Jabir G, Mohd DA, Rafea MM. Single-center experience of managing childhood intussusception. J Pediatr Adolesc Surg. 2021;2(1):84–8. 10.46831/jpas.v1i2.70. [Google Scholar]
- 27.Kolar M, Pilkington M, Winthrop A, Theivendram A, Lajkosz K, Brogly SB. Diagnosis and treatment of childhood intussusception from 1997 to 2016: A population-based study. J Pediatr Surg. 2020;55(8):1562–9. 10.1016/j.jpedsurg.2020.01.049. Epub 20200212. [DOI] [PubMed] [Google Scholar]
- 28.Glover-Addy H, Ansong D, Enweronu-Laryea C, Tate JE, Amponsa-Achiano K, Sarkodie B, et al. Epidemiology of intussusception in infants less than one year of age in ghana, 2012–2016. Pan Afr Med J. 2021;39(Suppl 1):8. 10.11604/pamj.supp.2021. Epub 20210729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsolenyanu E, Akakpo-Numado K, Akolly DE, Mwenda J, Tate J, Boko A, et al. Epidemiology of intussusception among infants in togo, 2015–2018. Pan Afr Med J. 2021;39(Suppl 1):7. 10.11604/pamj.supp.2021. Epub 20210729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Das MK, Arora NK, Mathai J, Sam CJ, G R. Profile and epidemiology of intussusception in children Under-Two years of age: A prospective surveillance. Indian J Pediatr. 2021;88(12):1187–94. 10.1007/s12098-021-03776-8. Epub 20210531. [DOI] [PubMed] [Google Scholar]
- 31.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. Epub 20131126. doi: 10.3389/fpsyg.2013.00863. PubMed PMID: 24324449; PubMed Central PMCID: PMC3840331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alsinan T, Altokhais T, Alshayeb F, Hajja A, Al Boukai M, Alsalameh S, et al. Risk factors for failure of enema reduction of intussusception in children. Sci Rep. 2024;14(1):20786. 10.1038/s41598-024-71289-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsu W-L, Lee H-C, Yeung C-Y, Chan W-T, Jiang C-B, Sheu J-C, et al. Recurrent intussusception: when should surgical intervention be performed?? Pediatr Neonatology. 2012;53(5):300–3. 10.1016/j.pedneo.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Xiaolong X, Yang W, Qi W, Yiyang Z, Bo X. Risk factors for failure of hydrostatic reduction of intussusception in pediatric patients: A retrospective study. Med (Baltim). 2019;98(1):e13826. 10.1097/md.0000000000013826. PubMed PMID: 30608396; PubMed Central PMCID: PMC6344150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Younes A, Lee S, Lee JI, Seo JM, Jung SM. Factors Associated with Failure of Pneumatic Reduction in Children with Ileocolic Intussusception. Children (Basel). 2021;8(2). Epub 20210212. 10.3390/children8020136. PubMed PMID: 33673183; PubMed Central PMCID: PMC7918438. [DOI] [PMC free article] [PubMed]
- 36.Lee DH, Kim SJ, Lee HJ, Jang HJ. Identifying predictive factors for the recurrence of pediatric intussusception. Pediatr Gastroenterol Hepatol Nutr. 2019;22(2):142–51. 10.5223/pghn.2019.22.2.142. Epub 20190307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gadgade BD, Radhakrishna V, Kumar N. Factors associated with a failed nonoperative reduction of intussusception in children. J Indian Assoc Pediatr Surg. 2021;26(6):421–6. Epub 20211112. doi: 10.4103/jiaps.JIAPS_297_20. PubMed PMID: 34912140; PubMed Central PMCID: PMC8637975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated and analyzed during the current study is not publicly available but is available from the corresponding author on reasonable request.