Abstract
Subjective quality of life can be compromised in individuals with psychosis-risk symptoms, with poorer quality of life being associated with worse functioning and later transition to psychosis. Individuals who experience psychosis-related symptoms also tend to endorse more internalized (or self-) mental health stigma when compared to controls, potentially contributing to delays in seeking treatment and increased duration of untreated psychosis, as well as interfering with treatment engagement and retention in those already receiving care. Despite these findings, and the growing recognition for prevention in earlier phases of psychotic illness, few studies have examined the relation between psychosis-risk symptoms, internalized stigma, and subjective quality of life in a younger, help-seeking sample. The present study examined whether internalized stigma mediates the relation between psychosis-risk symptoms and subjective quality of life in a transdiagnostic sample of youth (M age = 17.93, SD = 2.90) at clinical high-risk for psychosis (CHR), with early psychosis, or with non-psychotic disorders (N = 72). Psychosis-risk symptom severity was assessed using the Structured Interview for Psychosis-Risk Syndromes (SIPS). Internalized stigma was assessed using the Internalized Stigma of Mental Illness Inventory (ISMI), and subjective quality of life was assessed using the Youth Quality of Life Instrument – Short Form (YQOL-SF). Internalized stigma fully mediated the relation between psychosis-risk symptoms and subjective quality of life across the full sample (p < .05, f2 = 0.06). Findings suggest that internalized stigma may be an important target in efforts to improve quality of life for individuals in early stages of psychosis.
Keywords: Clinical high risk, Early psychosis spectrum, Internalized stigma, Quality of life
1. Introduction
1.1. Subjective quality of life in psychosis-related disorders
Subjective quality of life (SQOL) can be broadly conceptualized as an individual’s overall perception of wellbeing and life satisfaction across a variety of psychosocial domains, within the context of cultural and personal goals, expectations, and values (Malla and Payne, 2005; WHOQOL-Group, 1995). When compared with healthy controls, people with psychosis spectrum disorders consistently report poorer SQOL, which has been linked to a number of adverse clinical and functional outcomes within this population (Bechdolf et al., 2005; Bobes et al., 2007; Galuppi et al., 2010). There is also evidence that SQOL can be compromised in those with psychosis-risk symptoms and is associated with poor outcomes at this early stage of illness (Fusar-Poli et al., 2015; Heinze et al., 2018; Hui et al., 2013). Multiple studies have also demonstrated negative associations between SQOL and attenuated psychosis symptoms (Bechdolf et al., 2005; Domínguez-Martínez et al., 2015; Svirskis et al., 2007), and decreased SQOL has been shown to predict conversion to psychosis in longitudinal studies with clinical high-risk (CHR) samples (Strobl et al., 2012).
Interestingly, Bechdolf et al. (2005) found that individuals with psychosis-risk symptoms reported worse SQOL even when compared to those who met criteria for first-episode psychosis. These findings suggest that those in the earliest phases of the psychosis continuum may experience reduced subjective wellbeing in multiple areas of life, and that some aspects of SQOL may actually be more vulnerable for individuals in the psychosis-risk stage than in those already diagnosed with a formal psychotic disorder. Given that attenuated symptoms often emerge during adolescence and young adulthood, a transition-age period already characterized by multiple developmental challenges and role changes (Jalbrzikowski et al., 2014; Ruhrmann et al., 2008), it may be especially informative to examine SQOL and its determinants in the earlier phases of illness.
1.2. Internalized stigma across the psychosis spectrum
SQOL also appears to be related to stigma across the psychosis spectrum (Gerlinger et al., 2013; Vrbova et al., 2017), with psychosis being one of the most highly stigmatized mental health conditions (Pescosolido et al., 2019; Thornicroft et al., 2009; Wood et al., 2014). Compared to those with other mental health concerns, people diagnosed with schizophrenia are more likely to be perceived as dangerous, violent, and unpredictable (Angermeyer and Matschinger, 2003), as well as experience discrimination and social marginalization (Crisp et al., 2000). These findings seem to follow suit for those with ‘psychosis-risk’ labels (Yang et al., 2013).
As adolescence is a period associated with identity formation and heightened sensitivity to socioemotional stimuli (Albert and Steinberg, 2011), youth in the earliest phases of psychosis may be especially vulnerable to societal messages and peer attitudes surrounding psychosis and mental illness. Research suggests that youth at CHR may internalize negative stereotypes related to psychosis, which may explain the increased levels of self-stigma observed within this population (Yang et al., 2015, 2010). Among this group, internalized stigma has also been associated with a host of negative correlates and outcomes (Colizzi et al., 2020; Pyle et al., 2015; Rüsch et al., 2015; Rüsch et al., 2014; Stowkowy et al., 2015; Xu et al., 2016a, 2016b) including delays in seeking treatment (Byrne and Morrison, 2010; Franz et al., 2010) and poorer treatment engagement and retention in those already receiving care (Ben-David et al., 2018). Some studies have also found that internalized stigma is more robustly related to psychosis-related symptoms than formal diagnostic labels in early psychosis (Denenny et al., 2015; Pyle et al., 2015; Yang et al., 2015), and it is possible that internalized stigma may lead to the underreporting of symptoms and may undermine diagnostic accuracy even among youth already receiving mental health treatment for non-psychosis-related concerns. Gaining a better understanding of the mechanisms such as stigma that contribute to reduced SQOL in the early phases of psychosis may elucidate potential targets for treatment and inform early intervention efforts aimed at helping youth with psychosis-risk symptoms lead personally fulfilling and meaningful lives. Based on the extant literature on psychosis and stigma, it is possible that psychosis-risk symptoms affect SQOL through the way in which someone assigns meaning to these experiences, within the context of their social environment, prior experiences, and expectations.
1.3. The current study
The current study aimed to examine associations between psychosis-risk symptoms, internalized stigma, and SQOL in a sample of help-seeking youth. As psychosis-related experiences are transdiagnostic phenomena and are thought to exist on a continuum of severity (Moreno-Küstner et al., 2018; Van Os et al., 2009), and internalized mental health stigma appears to be more closely tied to symptoms than formal diagnoses, we opted to examine these relations across a combined sample of individuals with varying degrees of psychosis-risk symptoms. We hypothesized that within our sample, greater psychosis-risk symptom severity would be associated with both greater internalized stigma and poorer SQOL, and internalized stigma would mediate the relation between psychosis-risk symptom severity and SQOL. We also explored whether a) hypothesized relations would remain present when controlling for demographic covariates (age, binary gender, and race); b) distinct psychosis-risk symptoms (i.e., unusual thought content, suspiciousness, grandiosity, perceptual abnormalities/hallucinations, and disorganized communication) would be uniquely related to internalized stigma and/or SQOL; and c) distinct domains of internalized stigma (i.e., alienation, stereotype endorsement, discrimination experience, social withdrawal, and stigma resistance) would be uniquely related to psychosis-risk symptom severity and/or SQOL.
2. Method
2.1. Participants
Adolescents and young adults were recruited through the Strive for Wellness (SFW) clinic, a treatment and research program specializing in early identification and intervention for individuals at CHR for psychosis. The SFW clinic is affiliated with the Youth FIRST laboratory at the University of Maryland, Baltimore County (UMBC) and the Division of Child and Adolescent Psychiatry at the University of Maryland, School of Medicine (UMSOM).
Given our interest in the dimensional nature of psychosis, recruitment strategies were aimed at yielding participants with a wide range of psychosis-related experiences and concerns. Participants were recruited through community providers, clinics, hospitals, and schools in central Maryland and surrounding areas, and referred for either potential signs of early psychosis or other psychiatric concerns.1 In order to be eligible for the study, participants needed to be engaged in mental health services at the time of participation and/or suspected of experiencing attenuated psychosis symptoms, between the ages of 12 and 25 years old, and able to provide informed consent (or written assent, if under the age of 18). Participants under the age of 18 were accompanied by a consenting parent or legal guardian throughout all study procedures.
In addition to youth with non-psychotic disorders, the current study included both individuals at CHR and those with early psychosis to better represent the dimensional nature of the psychosis spectrum. To limit the sample to youth experiencing attenuated or very early-course psychosis symptoms, individuals who had previously been diagnosed with a psychotic disorder were excluded from study participation on the premise that they were more likely to be further along in their course of illness, to have been exposed to antipsychotic medication and other specialty treatments for psychosis, and to have had different stigma experiences compared to the help-seeking youth in our sample. Participants with early psychosis therefore represented youth who were accepted into the study based on suspected psychosis-risk symptoms or other mental health concerns and were discovered as meeting threshold for first-episode psychosis through the course of their study participation.
2.2. Procedure
All study procedures were approved by the Institutional Review Boards at UMBC and UMSOM. Upon initial entry into the SFW clinic, and following the eligibility screening and consent process, all participants completed a series of self-report questionnaires and clinician-administered psychodiagnostic interviews. All interviews were administered in-person by graduate-level study staff (who were supervised by licensed mental health professionals) and were conducted prior to participant receipt of any formal assessment feedback or other clinical services. All study data was collected between October 2014 and January 2020.
2.3. Measures
2.3.1. Structured Interview for Psychosis-Risk Syndromes (SIPS)
The SIPS is a clinician-administered, semi-structured interview designed to measure attenuated psychosis symptoms and assess for the presence of three separate psychosis-risk syndromes, schizotypal personality disorder, and psychosis (Miller et al., 2003). The SIPS measures 19 total symptoms, which are divided into positive (5 items), negative (6 items), disorganized (4 items), and general symptom (4 items) subscales. Each symptom is rated on a scale of 0 to 6, with higher scores reflecting greater severity. Participants met criteria for either CHR status or early psychosis based on their scores on any of the positive symptoms (unusual thought content, suspiciousness, grandiosity, perceptual abnormalities/hallucinations, and disorganized communication), or if they had experienced a significant decline in functioning accompanied by either a diagnosis of schizotypal personality disorder or a first-degree relative with psychosis. Participants who did not meet criteria for either CHR status or early psychosis were categorized as youth with non-psychotic disorders. A total psychosis-risk symptom severity score ranging from 0 to 30 was calculated by summing scores on the five individual positive symptom items (P1 through P5).
All SIPS interviewers completed a rigorous, standardized training protocol and reliability testing. Each participant case was also reviewed in weekly supervision meetings to establish diagnostic consensus among research team members.
2.3.2. Internalized Stigma of Mental Illness Inventory (ISMI)
The ISMI is a 29-item self-report questionnaire designed to assess subjective feelings of stigma in individuals experiencing mental health concerns (Ritsher et al., 2003). The ISMI is composed of five subscales measuring alienation, stereotype endorsement, perceived discrimination, social withdrawal, and stigma resistance associated with mental illness. Participants are instructed to consider their “mental health problems” or “whatever you feel is the best term for it” while responding to each item. All items are present-oriented and rated on a 4-point Likert scale, with response options ranging from “Strongly Disagree” to “Strongly Agree”, and higher scores representing greater self-stigma. In order to maximize response choices, we also included a “don’t know” response option for each item, which was subsequently excluded from analyses. A total score and summary scores for each subscale, each ranging from 1 to 4, were calculated; data were considered missing for participants with valid data on fewer than approximately 80% of the items (i.e., 23 items). The total ISMI scale proved to be highly reliable in our study sample (α = 0.94). The individual subscales ranged in reliability – Cronbach’s alphas for the alienation, stereotype endorsement, discrimination experience, social withdrawal, and stigma resistance items were 0.92, 0.67, 0.83, 0.85, and 0.54, respectively.
2.3.3. Youth Quality of Life Instrument – Short Form (YQOL-SF)
The YQOL-SF is 15-item self-report questionnaire adapted from the original 41-item Youth Quality of Life Instrument – Research Version (YQOL-R) and designed to measure perceived quality of life in adolescents (Patrick et al., 2002). The YQOL-SF is comprised of four domains: sense of self (five items), social relationships (five items), environment (four items), and general quality of life (one item). All items are rated on a 10-point Likert scale, with response options ranging from “Not At All” (0) to “Very Much” (10), and higher scores representing better perceived quality of life. A total score ranging from 0 to 100 was obtained by first converting all individual item scores to T-scores on a 100-point scale, and then calculating the mean of the 15 transformed items; data were considered missing for participants with valid data on less than 80% of the items. Although the YQOL-SF has not yet been empirically validated, the measure demonstrated good reliability in our study sample (α = 0.89). In addition, the original YQOL-R has been shown to have good reliability and validity in diverse clinical and community samples (Patrick et al., 2002; Salum et al., 2012; Topolski et al., 2004).
3. Results
3.1. Preliminary analyses
N = 112 participants were consented into the study. Data were generated from the SIPS positive symptom subscale, ISMI, and YQOL-SF, and participants were excluded from the analysis sample if they were missing data related to any of the psychosis-risk symptom variables, or if they answered less than 80% of the items on the ISMI and YQOL-SF scales. The final analysis sample included 72 participants, ranging in age from 12 to 23 years old (M = 17.93, SD = 2.90). Participants in the analysis sample were approximately 56% female (n = 40). Approximately 54% of participants self-identified as White (n = 39), 19% as Black or African American (n = 14), 13% as either biracial or multiracial (n = 9), and 11% as Asian (n = 8); 3% of participants identified as either “Other” or “Unknown” (n = 2). In terms of clinical status (as determined by SIPS diagnostic criteria), 54% of the sample (n = 39) met criteria for CHR, 21% (n = 15) met criteria for early/first-episode psychosis, and 25% (n = 18) were classified as youth with non-psychotic disorders. Descriptive statistics and correlations among study variables are presented in Table 1. Additionally, to help characterize the sample for contextual reasons, descriptive statistics by clinical status are presented in Table 2.
Table 1.
Bivariate correlations and descriptive statistics for primary study variables, age, binary gender, and race.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| 1. SQOL | |||||||||||||||
| 2. PSUM | −0.30* | ||||||||||||||
| 3. ISMI | −0.67** | 0.25* | |||||||||||||
| 4. P1 | −0.26* | 0.68** | 0.35** | ||||||||||||
| 5. P2 | −0.19 | 0.74** | 0.03 | 0.35** | |||||||||||
| 6. P3 | −0.03 | 0.54** | 0.08 | 0.25* | 0.33** | ||||||||||
| 7. P4 | −0.28* | 0.79** | 0.26* | 0.41** | 0.42** | 0.30** | |||||||||
| 8. P5 | −0.17 | 0.51** | 0.09 | 0.20 | 0.21 | 0.12 | 0.29* | ||||||||
| 9. Alienation | −0.66** | 0.32** | 0.89** | 0.41** | 0.04 | 0.10 | 0.32** | 0.17 | |||||||
| 10. Stereotype | −0.48** | 0.09 | 0.78** | 0.16 | −0.01 | 0.10 | 0.09 | −0.05 | 0.57** | ||||||
| 11. Discrim | −0.46** | 0.09 | 0.79** | 0.17 | −0.03 | −0.01 | 0.10 | 0.08 | 0.63** | 0.63** | |||||
| 12. Withdraw | −0.55** | 0.30* | 0.87** | 0.33** | 0.07 | 0.08 | 0.30* | 0.18 | 0.75** | 0.56** | 0.64** | ||||
| 13. Resistance | −0.40** | 0.01 | 0.51** | 0.12 | −0.05 | 0.04 | 0.05 | −0.15 | 0.33** | 0.47** | 0.19 | 0.30* | |||
| 14. Age | −0.14 | −0.01 | 0.00 | 0.04 | 0.06 | −0.04 | −0.07 | −0.02 | 0.01 | −0.02 | 0.07 | 0.01 | 0.11 | ||
| 15. Gendera | 0.16 | 0.14 | −0.19 | 0.13 | 0.09 | 0.10 | 0.02 | 0.18 | −0.30* | 0.00 | −0.21 | −0.18 | −0.09 | −0.13 | |
| 16. Raceb | 0.02 | 0.05 | −0.10 | 0.00 | 0.10 | −0.04 | −0.03 | 0.14 | −0.05 | −0.09 | −0.01 | −0.16 | 0.13 | 0.12 | 0.17 |
| M | 59.91 | 11.13 | 1.98 | 2.92 | 2.57 | 0.79 | 2.89 | 1.96 | 2.28 | 1.52 | 1.84 | 2.21 | 2.86 | 17.93 | |
| SD | 19.49 | 4.96 | 0.54 | 1.46 | 1.75 | 1.05 | 1.93 | 1.17 | 0.88 | 0.44 | 0.67 | 0.77 | 0.62 | 2.90 | |
p < .05,
p < .01, N = 72. SQOL = subjective quality of life; PSUM = psychosis-risk symptom severity; ISMI = internalized stigma; P1 = unusual thought content; P2 = suspiciousness; P3 = grandiosity; P4 = hallucinations; P5 = disorganized communication; Stereotype = stereotype endorsement; Discrim = perceived discrimination; Withdraw = social withdrawal; Resistance = stigma resistance.
Coded as (0 = female, 1 = male).
Coded as (0 = non-White, 1 = White). N = 71 for all correlations involving this variable.
Table 2.
Descriptive statistics by clinical status.
| Non-psychotic disorders (N = 18) |
CHR (N = 39) |
EP ( N = 15) |
||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
|
| ||||||
| SQOL | 63.26 | 18.14 | 57.54 | 21.14 | 62.04 | 16.71 |
| PSUM | 6.11 | 2.65 | 11.92 | 3.70 | 15.07 | 5.34 |
| ISMI | 1.94 | 0.57 | 2.02 | 0.59 | 1.95 | 0.37 |
3.2. Primary analyses
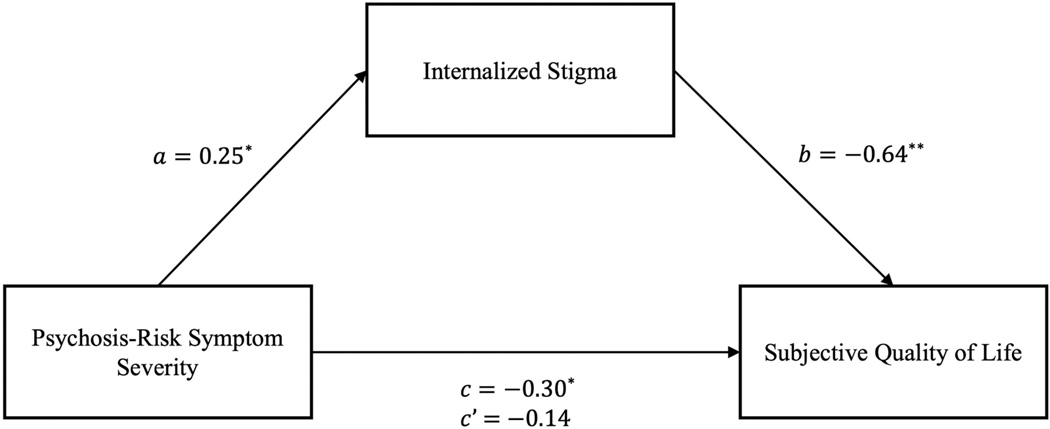
Bivariate correlations revealed significant relations between psychosis-risk symptom severity and both internalized stigma (r = 0.25) and SQOL (r = − 0.30). The mediational hypothesis was tested via regression analyses using the PROCESS Macro for SPSS v26.0 (Hayes, 2013). Evidence of an indirect effect was observed to the extent that a 95% confidence interval of 5000 bootstrapped estimates did not overlap zero (MacKinnon et al., 2004; O’Rourke and Mackinnon, 2018). Results demonstrated a significant indirect (mediating) effect of psychosis-risk symptom severity on SQOL through internalized stigma (see Fig. 1). In other words, greater psychosis-risk symptom severity (the primary predictor) was associated with worse SQOL (the outcome variable) and higher levels of internalized stigma (the mediator), and internalized stigma had a unique effect on SQOL when controlling for psychosis-risk symptoms, with higher levels of internalized stigma being associated with worse SQOL – b = − 0.64, t(69) = − 7.04, p < .001, f2 = 0.72. Accordingly, Sobel’s test of the indirect effect was significant, ab = − 0.16, t(69) = − 2.10, p = .04, f2 = 0.06, 95% CI [− 0.30, − 0.03]. Internalized stigma accounted for 54% of the total effect of psychosis-risk symptoms on SQOL. Additionally, the model supported the presence of complete mediation as psychosis-risk symptoms no longer predicted SQOL once the effects of internalized stigma were accounted for – b = − 0.14, t(69) = − 1.50, p = .138, f2 = 0.03.
Fig. 1.
Estimated mediation model.
Note. * p < .05, ** p < .01.
Estimates provided are standardized regression coefficients.
3.3. Exploratory analyses
As age, binary gender, and race were not related to the primary predictors of interest, exploratory analyses with these variables were not considered. Two separate multiple regressions were estimated to address research question 1 (distinct psychosis-risk symptoms may be uniquely associated with internalized stigma and/or subjective quality of life). Each regression tested the direct effects of five different types of psychosis-risk symptoms on internalized stigma and SQOL, respectively (Tables 3 and 4). A significant positive relation was observed between unusual thought content and internalized stigma, b = 0.12, t(66) = 2.54, p = .014, f2 = 0.10. No other individual psychosis-risk symptoms uniquely predicted internalized stigma. The overall model estimating the effects of psychosis-risk symptom types on SQOL was not significant, and no individual psychosis-risk symptoms were uniquely associated with SQOL.
Table 3.
Types of psychosis-risk symptoms predicting internalized stigma.
| Internalized stigma | ||||
|---|---|---|---|---|
|
| ||||
| Overall model | R 2 | F | df | p |
| 0.16 | 2.51 | 5, 66 | 0.039 | |
| Predictors | b (sb) | t | p | f 2 |
| Unusual thought content | 0.12 (0.32) | 2.54 | 0.014 | 0.10 |
| Suspiciousness | −0.05 (−0.16) | −1.25 | 0.217 | 0.02 |
| Grandiosity | 0.00 (−0.01) | −0.05 | 0.960 | 0.00 |
| Hallucinations | 0.06 (0.20) | 1.49 | 0.141 | 0.03 |
| Disorganized communication | 0.00 (0.00) | −0.01 | 0.988 | 0.00 |
Table 4.
Types of psychosis-risk symptoms predicting subjective quality of life.
| Subjective quality of life | ||||
|---|---|---|---|---|
|
| ||||
| Overall model | R 2 | F | df | p |
| 0.12 | 1.78 | 5, 66 | 0.129 | |
| Predictors | b (sb) | t | p | f 2 |
| Unusual thought content | −2.17 (−0.16) | −1.24 | 0.218 | 0.02 |
| Suspiciousness | −0.72 (−0.06) | −0.48 | 0.632 | 0.00 |
| Grandiosity | 1.79 (0.10) | 0.77 | 0.444 | 0.01 |
| Hallucinations | −1.99 (−0.20) | −1.42 | 0.159 | 0.03 |
| Disorganized communication | −1.25 (−0.07) | −0.62 | 0.540 | 0.01 |
Two multiple regressions were estimated to address research question 2 (distinct domains of internalized stigma may be uniquely associated with psychosis-risk symptom severity and/or subjective quality of life). Each regression tested the direct effects of five different forms of internalized stigma on psychosis-risk symptom severity and SQOL, respectively (Tables 5 and 6). The overall model estimating the effects of specific forms of stigma on psychosis-risk symptom severity was significant, suggesting that together, the five different forms of stigma accounted for a significant proportion of the variance in psychosis-risk symptom severity. However, there were no unique associations between any individual forms of stigma and psychosis-risk symptom severity. The overall model estimating the effects of specific forms of stigma on SQOL was also significant, with increased feelings of alienation uniquely predicting worse SQOL - b = − 11.02, t(66) = − 3.48, p = .001, f2 = 0.18. No other forms of stigma were uniquely associated with SQOL.
Table 5.
Types of internalized stigma predicting psychosis-risk symptom severity.
| Psychosis-risk symptom severity | ||||
|---|---|---|---|---|
|
| ||||
| Overall model | R 2 | F | df | p |
| 0.15 | 2.39 | 5, 66 | 0.047 | |
| Predictors | b (sb) | t | p | f 2 |
| Alienation | 1.91 (0.34) | 1.85 | 0.069 | 0.05 |
| Stereotype endorsement | −0.58 (−0.05) | −0.30 | 0.764 | 0.00 |
| Perceived discrimination | −1.66 (−0.22) | −1.32 | 0.193 | 0.03 |
| Social withdrawal | 1.58 (0.25) | 1.35 | 0.182 | 0.03 |
| Stigma resistance | −0.86 (−0.11) | −0.81 | 0.420 | 0.01 |
Table 6.
Types of internalized stigma predicting subjective quality of life.
| Subjective quality of life | ||||
|---|---|---|---|---|
|
| ||||
| Overall model | R 2 | F | df | p |
| 0.48 | 12.29 | 5, 66 | < 0.001 | |
| Predictors | b (sb) | t | p | f 2 |
| Alienation | −11.02 (−0.50) | −3.48 | 0.001 | 0.18 |
| Stereotype endorsement | −1.39 (−0.03) | −0.24 | 0.813 | 0.00 |
| Perceived discrimination | −1.27 (−0.04) | −0.33 | 0.744 | 0.00 |
| Social withdrawal | −1.77 (−0.07) | −0.49 | 0.625 | 0.00 |
| Stigma resistance | −6.27 (−0.20) | −1.93 | 0.058 | 0.06 |
4. Discussion
This study sought to examine the relation between psychosis-risk symptoms, internalized stigma, and subjective quality of life in a sample of youth that included individuals in the CHR and early stages of psychosis, as well as help-seeking individuals who endorsed varying levels of psychosis-risk symptoms below the CHR range. Results supported the primary hypotheses – within the sample, psychosis-risk symptom severity was negatively associated with SQOL, and internalized stigma completely mediated this effect (f2 = 0.06).
4.1. Relations between psychosis-risk symptoms, internalized stigma, and SQOL
Our findings are consistent with prior research demonstrating that youth who experience attenuated symptoms of psychosis endorse both greater feelings of internalized stigma and reduced SQOL when compared to those who do not. It also appears that internalized stigma may be a key mechanism through which psychosis-risk symptoms ultimately influence a person’s emotional wellbeing. In other words, results from this study provide support for the idea that it is an individual’s interpretation of mental health symptoms, and not the symptoms themselves, that is ultimately implicated in SQOL.
Prior research has established a link between symptoms and quality of life through internalized stigma in the broader psychosis literature. For instance, Chan and Mak (2014) reported that internalized stigma mediated the relation between symptom severity and SQOL in a sample of outpatients with schizophrenia. Negative appraisals of psychotic symptoms are common in people with schizophrenia (Moritz et al., 2018; Moritz et al., 2014), and greater symptom severity has been associated with an increased tendency to attribute negative events to internal causes (Mizrahi et al., 2008). In youth with psychosis-risk symptoms, negative beliefs about psychosis (e.g., perceiving psychosis as stigmatizing or believing that symptoms may lead to social rejection) has also been associated with greater symptom-related distress and higher levels of depression and anxiety (Morrison et al., 2006; Ropaj et al., 2021). Though no other studies to-date have looked explicitly at the relation between psychosis-risk symptoms, internalized stigma, and SQOL in a sample of help-seeking youth, these prior findings support the idea that internalized stigma represents an important mediating factor in the relation between symptoms and overall wellbeing within this group.
4.2. Relations between specific psychosis-risk symptoms and internalized stigma
Unusual thought content – which encompasses a range of experiences that represent subthreshold delusional ideation (e.g., magical thinking, non-persecutory ideas of reference, and other atypical or overvalued beliefs) – emerged as a unique predictor of internalized stigma when controlling for other psychosis-risk symptom domains. This finding is consistent with prior research demonstrating that unusual thought content and other forms of attenuated delusions are associated with internalized stigma in youth at CHR, above and beyond the effects of other psychosis-risk symptoms (DeLuca et al., 2021a; Pyle et al., 2015; Stowkowy et al., 2015), and that unusual thought content is associated with negative self-evaluations (e.g., seeing oneself as “weak”, “bad”, or “worthless”; Addington and Tran, 2009). It is possible that these types of experiences are more strongly associated with stigmatizing notions of personal responsibility (Corrigan and Watson, 2002) or otherwise viewed as less ‘acceptable’ than other types of psychosis-risk symptoms. Additionally, some research has demonstrated that delusional ideation in psychosis is associated with certain cognitive biases (Broome et al., 2007; Langdon et al., 2010; Lysaker and Hammersley, 2006; Moritz et al., 2014; Werner et al., 2014) which may perpetuate feelings of shame, social exclusion, and self-blame that then lead to impaired quality of life. One study has also found that experiences such as unusual thought content may contribute to a longer duration of untreated psychosis-risk symptoms (Zhang et al., 2018), potentially through a pathway of stigma.
Other than the few studies previously mentioned, there has generally been limited investigation into relations between distinct psychosis-risk symptoms and stigma. This represents an important area to explore further, particularly given the clinical heterogeneity in CHR and psychosis populations (Millman and Schiffman, 2018; Picardi et al., 2012). Our findings suggest that youth who endorse unusual thought content may be especially vulnerable to the experience of internalized stigma.
4.3. Relations between specific forms of internalized stigma and SQOL
We also found that alienation – a form of internalized stigma involving feelings of inferiority, status loss, and social exclusion due to mental illness – had moderate effects on SQOL, with greater feelings of alienation predicting poorer quality of life in the sample. Alienation has been described as a feeling of being “less than a full member of society” (Drapalski et al., 2013, p. 265), and appears to be one of the most common forms of internalized stigma experienced by people with schizophrenia (Brohan et al., 2010; Gerlinger et al., 2013; Holubova et al., 2016; Koschorke et al., 2014; Lv et al., 2013). In addition, feelings of alienation are thought to be exacerbated through social comparison processes and have been associated with reduced frequency of social contacts in those with psychosis (Koschorke et al., 2014; Lysaker et al., 2010). For young people in the earlier phases of psychosis who are in a developmental stage where peer relationships and social comparison processes are particularly salient, these feelings may be particularly detrimental to wellbeing (Jalbrzikowski et al., 2014; Ruhrmann et al., 2008).
It is also possible that relations between individual forms of stigma and SQOL may change depending on stage of illness or degree of exposure to public stigma over time. For example, individuals with early psychosis spectrum symptoms may initially be shielded from certain types of stigma because these symptoms may be easier to conceal than full-scale psychotic symptoms (Link et al., 1989). It could be that feelings of alienation precede other forms of internalized stigma that are associated with greater symptom severity and/or visibility in a more chronic population. Similarly, anticipated stigma may be of particular concern among those with “concealable stigmatized identities” (Quinn and Chaudoir, 2009, p. 634). Though not directly assessed in the current study, anticipated stigma refers to the degree to which a person expects to be stigmatized if a certain identity (i.e., mental health status) is revealed to others, and may be linked to feelings of alienation (DeLuca, 2020; Moses, 2011; Quinn and Chaudoir, 2009). As stigma is a multidimensional construct, future research should continue to explore how different forms of internalized stigma, as well as anticipated stigma, may impact wellbeing within this unique population.
4.4. Limitations
The cross-sectional nature of the study did not allow for the assessment of temporal order between variables. This raises the possibility of reverse causality, or alternative explanations for the observed relations (e.g., underlying third variables). Although the literature supports the hypothesized ordering of variables in this study, it could also be the case that worse SQOL leads to increased symptom severity and/or greater internalized stigma, or that greater internalized stigma exacerbates psychosis-risk symptoms. Relations between these variables may also be cyclical in nature. Future longitudinal research could help establish causal pathways by examining psychosis-risk symptoms, internalized stigma, and SQOL at different time points.
There may have been some conceptual overlap between individual items used to assess internalized stigma and items used to assess SQOL, which could have exaggerated the strength of relations among study variables or the size of the indirect effect. Although our internalized stigma measure aimed to assess subjective experiences directly associated with mental health concerns whereas our SQOL measure aimed to assess life experiences more broadly, both constructs are complex, socially constructed phenomena and may be interpreted similarly by some individuals. Future studies should examine whether the observed relations in this study hold true across different measures of internalized stigma and SQOL.
Our recruitment procedures were biased such that our findings may not precisely generalize to all clinical settings. Specifically, some participants who were referred for suspected psychosis-risk symptoms, but did not end up meeting CHR criteria, were subsequently classified as youth with non-psychotic disorders. This may have resulted in this group more closely resembling participants at CHR/early psychosis than help-seeking youth with non-psychotic disorders outside the context of psychosis specialty clinics. Nonetheless, for the purposes of this study, our sample provided an appropriate distribution of psychosis spectrum experiences and symptoms and is likely representative of youth in specialty clinics similar to ours.
Missing data was relatively high in this sample. Nonetheless, analyses did not reveal any systematic differences between participants with missing data versus those included in the final analyses that would call into question the validity or generalizability of our findings.
4.5. Clinical implications and future directions
In light of growing recognition for prevention in earlier phases of illness, findings from this study indicate that internalized mental health stigma may be an important target in early intervention efforts along the psychosis spectrum and beyond. Albeit speculative given the aforementioned limitations, psychosocial interventions aimed at reducing internalized stigma may lead to improved quality of life for help-seeking adolescents and young adults experiencing psychosis-risk symptoms, over and above interventions targeting symptoms alone (DeLuca et al., 2021b). Stigma-reduction interventions also represent a low-risk treatment option with few – if any – harmful side effects.
Of note, efforts to address internalized stigma should not detract from work to reduce public stigma (presumably the source of internalized stigma) in society as a whole. Preventative work should therefore consider the influence of both public and personal forms of stigma on the mental health and wellbeing of those in the earlier stages of the psychosis continuum, with the understanding that each has important implications for recovery within this population.
Acknowledgments
The authors would like to thank the participants who generously gave their time, effort, and trust to take part in this study, and without whom this work would not be possible.
Role of the funding source
This work was supported by the National Institute of Mental Health (grant R01MH112612), the Maryland Department of Health and Mental Hygiene, Behavioral Health Administration through the Maryland Center of Excellence on Early Intervention Program (MEIP) (OPASS# 14-13717G/M00B4400241), and the Substance Abuse and Mental Health Services Administration (Community Intervention for those at Clinical High Risk for Psychosis, vis a vis MD State Dept of Health, SM081092-01). Joseph S. DeLuca is supported by a National Institute of Mental Health T32 Fellowship (1T32MH122394-01). The funding sources did not have a role in the writing of this manuscript.
Footnotes
CRediT authorship contribution statement
Authors Akouri-Shan and Schiffman designed and ran the study, with assistance from authors DeLuca, Jay, Redman, Petti, Bridgwater, Rakhshan Rouhakhtar, Klaunig, Chibani, and Reeves. Author Akouri-Shan managed the literature searches. Authors Akouri-Shan and Pitts undertook the statistical analysis. Author Akouri-Shan wrote the manuscript with conceptual and written assistance from authors DeLuca, Petti, Bridgwater, Martin, and Schiffman.
Declaration of competing interest
All authors declare that they have no conflicts of interest.
Some recruitment strategies were designed to be more likely to yield either potential CHR participants or youth with non-psychotic disorders. For example, members of our research team regularly engaged in outreach activities (e.g., giving presentations on psychosis-risk to various community organizations). In addition, detailed information about the SFW clinic is publicly available online. Therefore, some of the individuals who contacted us were aware of the nature of our clinic and specialization in psychosis-risk-related concerns. Wording on flyers and internet advertisements, however, was kept relatively non-specific. Individuals were encouraged to contact us if they – or someone they knew – were experiencing any new or unusual symptoms, sudden changes in mood or functioning, sleep difficulties, and/or difficulties managing everyday stressors.
References
- Addington J, Tran L, 2009. Using the brief core schema scales with individuals at clinical high risk of psychosis. Behav. Cogn. Psychother. 37, 227–231. 10.1017/S1352465809005116. [DOI] [PubMed] [Google Scholar]
- Albert D, Steinberg L, 2011. Judgment and decision making in adolescence. J. Res. Adolesc. 21, 211–224. 10.1111/j.1532-7795.2010.00724.x. [DOI] [Google Scholar]
- Angermeyer MC, Matschinger H, 2003. Public beliefs about schizophrenia and depression: similarities and differences. Soc. Psychiatry Psychiatr. Epidemiol. 38, 526–534. 10.1007/s00127-003-0676-6. [DOI] [PubMed] [Google Scholar]
- Bechdolf A, Pukrop R, Köhn D, Tschinkel S, Veith V, Schultze-Lutter F, Ruhrmann S, Geyer C, Pohlmann B, Klosterkötter J, 2005. Subjective quality of life in subjects at risk for a first episode of psychosis: a comparison with first episode schizophrenia patients and healthy controls. Schizophr. Res. 79, 137–143. 10.1016/j.schres.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Ben-David S, Cole A, Brucato G, Girgis RR, Munson MR, 2018. Mental health service use decision-making among young adults at clinical high risk for developing psychosis. Early Interv. Psychiatry 13, 1050–1055. 10.1111/eip.12725. [DOI] [PubMed] [Google Scholar]
- Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousoño M, 2007. Quality of life in schizophrenic patients. Dialogues Clin. Neurosci. 9, 215–226. 10.5294/aqui.2011.11.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brohan E, Elgie R, Sartorius N, Thornicroft G, 2010. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr. Res. 122, 232–238. 10.1016/j.schres.2010.02.1065. [DOI] [PubMed] [Google Scholar]
- Broome MR, Johns LC, Valli I, Woolley JB, Tabraham P, Brett C, Valmaggia L, Peters E, Garety PA, McGuire PK, 2007. Delusion formation and reasoning biases in those at clinical high risk for psychosis. Br. J. Psychiatry 191, s38–s42. 10.1192/bjp.191.51.s38. [DOI] [PubMed] [Google Scholar]
- Byrne R, Morrison AP, 2010. Young people at risk of psychosis: a user-led exploration of interpersonal relationships and communication of psychological difficulties. Early Interv. Psychiatry 4, 162–168. 10.1111/j.1751-7893.2010.00171.x. [DOI] [PubMed] [Google Scholar]
- Chan KKS, Mak WWS, 2014. The mediating role of self-stigma and unmet needs on the recovery of people with schizophrenia living in the community. Qual. Life Res. 23, 2559–2568. 10.1007/s11136-014-0695-7. [DOI] [PubMed] [Google Scholar]
- Colizzi M, Ruggeri M, Lasalvia A, 2020. Should we be concerned about stigma and discrimination in people at risk for psychosis? A systematic review. Psychol. Med. 10.1017/S0033291720000148. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, 2002. The paradox of self-stigma and mental illness. Clin. Psychol. Sci. Pract. 9, 35–53. 10.1093/clipsy/9.1.35. [DOI] [Google Scholar]
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ, 2000. Stigmatisation of people with mental illnesses. Br. J. Psychiatry 177, 4–7. 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- DeLuca JS, 2020. Conceptualizing adolescent mental illness stigma: youth stigma development and stigma reduction programs. Adolesc. Res. Rev. 5, 153–171. 10.1007/s40894-018-0106-3. [DOI] [Google Scholar]
- DeLuca JS, Akouri-Shan L, Jay SY, Redman S, Petti E, Lucksted A, Rakhshan Rouhakhtar P, Klaunig M, Edwards S, Reeves G, Schiffman J, 2021a. Predictors of internalized mental health stigma in a help-seeking sample of youth: the roles of psychosis-spectrum symptoms and family functioning. J. Abnorm. Psychol. 130, 587–593. 10.1037/abn0000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLuca JS, Yang LH, Lucksted AA, Yanos PT, DeVylder J, Anglin DM, Landa Y, Corcoran CM, 2021b. Reducing stigma among youth at risk for psychosis: a call to action. Schizophr. Bull. 10.1093/schbul/sbab098 sbab 098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denenny D, Thompson E, Pitts SC, Dixon LB, Schiffman J, 2015. Subthreshold psychotic symptom distress, self-stigma, and peer social support among college students with mental health concerns. Psychiatr. Rehabil. J. 38, 164–170. 10.1037/prj0000124. [DOI] [PubMed] [Google Scholar]
- Domínguez-Martínez T, Kwapil TR, Barrantes-Vidal N, 2015. Subjective quality of life in at-risk mental state for psychosis patients: relationship with symptom severity and functional impairment. Early Interv. Psychiatry 9, 292–299. 10.1111/eip.12111. [DOI] [PubMed] [Google Scholar]
- Drapalski AL, Lucksted A, Perrin PB, Aakre JM, Brown CH, DeForge BR, Boyd JE, 2013. A model of internalized stigma and its effects on people with mental illness. Psychiatr. Serv. 64, 264–269. 10.1176/appi.ps.001322012. [DOI] [PubMed] [Google Scholar]
- Franz L, Carter T, Leiner AS, Bergner E, Thompson NJ, Compton MT, 2010. Stigma and treatment delay in first-episode psychosis: a grounded theory study. Early Interv. Psychiatry 4, 47–56. 10.1111/j.1751-7893.2009.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rocchetti M, Sardella A, Avila A, Brandizzi M, Caverzasi E, Politi P, Ruhrmann S, McGuire P, 2015. Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br. J. Psychiatry 207, 198–206. 10.1192/bjp.bp.114.157115. [DOI] [PubMed] [Google Scholar]
- Galuppi A, Turola MC, Nanni MG, Mazzoni P, Grassi L, 2010. Schizophrenia and quality of life: how important are symptoms and functioning? Int. J. Ment. Heal. Syst. 4, 31. 10.1186/1752-4458-4-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU, 2013. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry 12, 155–164. 10.1002/wps.20040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach. Guilford Press, New York. [Google Scholar]
- Heinze K, Lin A, Nelson B, Reniers RLEP, Upthegrove R, Clarke L, Roche A, Lowrie A, Wood SJ, 2018. The impact of psychotic experiences in the early stages of mental health problems in young people. BMC Psychiatry 18, 1–10. 10.1186/s12888-018-1767-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holubova M, Prasko J, Matousek S, Latalova K, Marackova M, Vrbova K, Grambal A, Slepecky M, Zatkova M, 2016. Comparison of self-stigma and quality of life in patients with depressive disorders and schizophrenia spectrum disorders - a cross-sectional study. Neuropsychiatr. Dis. Treat. 10.2147/NDT.S121556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui C, Morcillo C, Russo DA, Stochl J, Shelley GF, Painter M, Jones PB, Perez J, 2013. Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis. Schizophr. Res. 148, 175–180. 10.1016/j.schres.2013.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalbrzikowski M, Sugar CA, Zinberg J, Bachman P, Cannon TD, Bearden CE, 2014. Coping styles of individuals at clinical high risk for developing psychosis. Early Interv. Psychiatry 8, 68–76. 10.1111/eip.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, Pereira J, Naik S, John S, Dabholkar H, Balaji M, Chavan A, Varghese M, Thara R, Thornicroft G, Patel V, 2014. Experiences of stigma and discrimination of people with schizophrenia in India. Soc. Sci. Med. 123, 149–159. 10.1016/j.socscimed.2014.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langdon R, Ward PB, Coltheart M, 2010. Reasoning anomalies associated with delusions in schizophrenia. Schizophr. Bull. 36, 321–330. 10.1093/schbul/sbn069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP, 1989. A modified labeling theory approach to mental disorders: an empirical assessment. Am. Sociol. Rev. 54, 400–423. 10.2307/2095613. [DOI] [Google Scholar]
- Lv Y, Wolf A, Wang X, 2013. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen. Hosp. Psychiatry 35, 83–88. 10.1016/j.genhosppsych.2012.07.007. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Hammersley J, 2006. Association of delusions and lack of cognitive flexibility with social anxiety in schizophrenia spectrum disorders. Schizophr. Res. 86, 147–153. 10.1016/j.schres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Ringer J, Maxwell C, McGuire A, Lecomte T, 2010. Personal narratives and recovery from schizophrenia. Schizophr. Res. 121, 271–276. 10.1016/j.schres.2010.03.003. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J, 2004. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivar. Behav. Res. 39, 99. 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malla A, Payne J, 2005. First-episode psychosis: psychopathology, quality of life, and functional outcome. Schizophr. Bull. 31, 650–671. 10.1093/schbul/sbi031. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW, 2003. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr. Bull. 29, 703–715. 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Millman ZB, Schiffman J, 2018. False-positives and clinical heterogeneity among youth at clinical high-risk for psychosis: clinical and ethical implications for assessment and treatment. J. Ethics Ment. Health 9, 2014–2016. [Google Scholar]
- Mizrahi R, Addington J, Remington G, Kapur S, 2008. Attribution style as a factor in psychosis and symptom resolution. Schizophr. Res. 104, 220–227. 10.1016/j.schres.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Moreno-Küstner B, Martín C, Pastor L, 2018. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One 13, e0195687. 10.1371/journal.pone.0195687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz S, Andreou C, Schneider BC, Wittekind CE, Menon M, Balzan RP, Woodward TS, 2014. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin. Psychol. Rev. 34, 358–366. 10.1016/j.cpr.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Moritz S, Mahlke CI, Westermann S, Ruppelt F, Lysaker PH, Bock T, Andreou C, 2018. Embracing psychosis: a cognitive insight intervention improves personal narratives and meaning-making in patients with schizophrenia. Schizophr. Bull. 44, 307–316. 10.1093/schbul/sbx072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison AP, French P, Lewis SW, Roberts M, Raja S, Neil ST, Parker S, Green J, Kilcommons A, Walford L, Bentall RP, 2006. Psychological factors in people at ultra-high risk of psychosis: comparisons with non-patients and associations with symptoms. Psychol. Med. 36, 1395–1404. 10.1017/S0033291706007768. [DOI] [PubMed] [Google Scholar]
- Moses T, 2011. Stigma apprehension among adolescents discharged from brief psychiatric hospitalization. J. Nerv. Ment. Dis. 199 10.1097/NMD.0b013e31822fc7be. [DOI] [PubMed] [Google Scholar]
- O’Rourke HP, Mackinnon DP, 2018. Reasons for testing mediation in the absence of an intervention effect: a research imperative in prevention and intervention research. J. Stud. Alcohol Drugs 79, 171–181. 10.15288/jsad.2018.79.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick D, Edwards TC, Topolski TD, 2002. Adolescent quality of life, part II: initial validation of a new instrument. J. Adolesc. 25, 287–300. 10.1006/jado.2002.0471. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Manago B, Monahan J, 2019. Evolving public views on the likelihood of violence from people with mental illness: stigma and its consequences. Health Aff. 38, 1735–1743. 10.1377/hlthaff.2019.00702. [DOI] [PubMed] [Google Scholar]
- Picardi A, Viroli C, Tarsitani L, Miglio R, de Girolamo G, Dell’Acqua G, Biondi M, 2012. Heterogeneity and symptom structure of schizophrenia. Psychiatry Res. 198, 386–394. 10.1016/j.psychres.2011.12.051. [DOI] [PubMed] [Google Scholar]
- Pyle M, Stewart SLK, French P, Byrne R, Patterson P, Gumley A, Birchwood M, Morrison AP, 2015. Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Interv. Psychiatry 9, 133–140. 10.1111/eip.12098. [DOI] [PubMed] [Google Scholar]
- Quinn DM, Chaudoir SR, 2009. Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. J. Pers. Soc. Psychol. 97, 634–651. 10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, Grajales M, 2003. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 121, 31–49. 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Ropaj E, Jones A, Dickson JM, Gill Z, Taylor PJ, 2021. Are negative beliefs about psychosis associated with emotional distress in adults and young people with such experiences? A meta-analysis. Psychol. Psychother. Theory Res. Pract. 94, 242–267. 10.1111/papt.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhrmann S, Paruch J, Bechdolf A, Pukrop R, Wagner M, Berning J, Schultze-Lutter F, Janssen B, Gaebel W, Möller HJ, Maier W, Klosterkötter J, 2008. Reduced subjective quality of life in persons at risk for psychosis. Acta Psychiatr. Scand. 117, 357–368. 10.1111/j.1600-0447.2008.01152.x. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Corrigan PW, Heekeren K, Theodoridou A, Dvorsky D, Metzler S, Müller M, Walitza S, Rössler W, 2014. Well-being among persons at risk of psychosis: the role of self-labeling, shame, and stigma stress. Psychiatr. Serv. 65, 483–489. 10.1176/appi.ps.201300169. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Heekeren K, Theodoridou A, Müller M, Corrigan PW, Mayer B, Metzler S, Dvorsky D, Walitza S, Rossler W, 2015. Stigma as a stressor and transition to schizophrenia after one year among young people at risk of psychosis. Schizophr. Res. 166, 43–48. 10.1016/j.schres.2015.05.027. [DOI] [PubMed] [Google Scholar]
- Salum GA, Patrick DL, Isolan LR, Manfro GG, De Almeida Fleck MP, 2012. Youth quality of life instrument-research version (YQOL-R): psychometric properties in a community sample. J. Pediatr. 88, 443–448. 10.2223/JPED.2193. [DOI] [PubMed] [Google Scholar]
- Stowkowy J, Perkins DO, Woods SW, Nyman K, Addington J, 2015. Personal beliefs about experiences in those at clinical high risk for psychosis. Behav. Cogn. Psychother. 43, 669–675. 10.1017/S1352465814000307. [DOI] [PubMed] [Google Scholar]
- Strobl EV, Eack SM, Swaminathan V, Visweswaran S, 2012. Predicting the risk of psychosis onset: advances and prospects. Early Interv. Psychiatry 6, 368–379. 10.1111/j.1751-7893.2012.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svirskis T, Korkeila J, Heinimaa M, Huttunen J, Ilonen T, Ristkari T, Hietala J, Syvälahti E, McGlashan T, Vahlberg T, Salokangas RKR, 2007. Quality of life and functioning ability in subjects vulnerable to psychosis. Compr. Psychiatry 48, 155–160. 10.1016/j.comppsych.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, 2009. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet 373, 408–415. 10.1016/S0140-6736(08)61817-6. [DOI] [PubMed] [Google Scholar]
- Topolski TD, Edwards TC, Patrick DL, Varley P, Way ME, Buesching DP, 2004. Quality of life of adolescent males with attention-deficit hyperactivity disorder. J. Atten. Disord. 7, 163–173. 10.1177/108705470400700304. [DOI] [PubMed] [Google Scholar]
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L, 2009. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med. 39, 179–195. 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- Vrbova K, Prasko J, Ociskova M, Kamaradova D, Marackova M, Holubova M, Grambal A, Slepecky M, Latalova K, 2017. Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr. Dis. Treat. 13, 567–576. 10.2147/NDT.S122483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner JD, Trapp K, Wüstenberg T, Voss M, 2014. Self-attribution bias during continuous action-effect monitoring in patients with schizophrenia. Schizophr. Res. 152, 33–40. 10.1016/j.schres.2013.10.012. [DOI] [PubMed] [Google Scholar]
- WHOQOL-Group, 1995. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc. Sci. Med. 10.1016/0277-9536(95)00112-K. [DOI] [PubMed] [Google Scholar]
- Wood L, Birtel M, Alsawy S, Pyle M, Morrison A, 2014. Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. Psychiatry Res. 220, 604–608. 10.1016/j.psychres.2014.07.012. [DOI] [PubMed] [Google Scholar]
- Xu Z, Mayer B, Müller M, Heekeren K, Theodoridou A, Dvorsky D, Metzler S, Oexle N, Walitza S, Rössler W, Rüsch N, 2016a. Stigma and suicidal ideation among young people at risk of psychosis after one year. Psychiatry Res. 243, 219–224. 10.1016/j.psychres.2016.06.041. [DOI] [PubMed] [Google Scholar]
- Xu Z, Müller M, Heekeren K, Theodoridou A, Dvorsky D, Metzler S, Brabban A, Corrigan PW, Walitza S, Rössler W, Rüsch N, 2016b. Self-labelling and stigma as predictors of attitudes towards help-seeking among people at risk of psychosis: 1-year follow-up. Eur. Arch. Psychiatry Clin. Neurosci. 266, 79–82. 10.1007/s00406-015-0576-2. [DOI] [PubMed] [Google Scholar]
- Yang LH, Wonpat-Borja AJ, Opler MG, Corcoran CM, 2010. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: an empirical question. Schizophr. Res. 120, 42–48. 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang LH, Anglin DM, Wonpat-Borja AJ, Opler MG, Greenspoon M, Corcoran CM, 2013. Public stigma associated with psychosis risk syndrome in a college population: implications for peer intervention. Psychiatr. Serv. 64, 284–288. 10.1176/appi.ps.003782011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang LH, Link BG, Ben-David S, Gill KE, Girgis RR, Brucato G, Wonpat-Borja AJ, Corcoran CM, 2015. Stigma related to labels and symptoms in individuals at clinical high-risk for psychosis. Schizophr. Res. 168, 9–15. 10.1016/j.schres.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T, Xu L, Tang Y, Cui H, Wei Y, Wang Junjie, Tang X, Li C, Wang Jijun, 2018. Duration of untreated prodromal symptoms in a Chinese sample at a high risk for psychosis: demographic, clinical, and outcome. Psychol. Med. 48 10.1017/S0033291717002707. [DOI] [PubMed] [Google Scholar]