Abstract
Background:
Carpometacarpal (CM) joint osteoarthritis of the thumb is characterized by pain and impaired thumb function in terms of pinch and range of motion. Here, we newly adopted a trapeziectomy with a graft-augmented ligament reconstruction procedure, in which the reconstructed ligament is reinforced using a half-slip extensor carpi radialis longus (ECRL) tendon.
Methods:
From 2015 to 2022, 101 hands of 95 patients with CM joint osteoarthritis of the thumb underwent trapeziectomy with graft-augmented ligament reconstruction using the half-slip ECRL tendon to reconstruct the ligament. The reconstructed ligament was reinforced by wrapping 3 times with the half-slip ECRL tendon. All patients underwent a 1-year assessment, and 29 hands of 26 patients were followed up for >4 years postoperatively.
Results:
Motion pain, as assessed by visual analogue scale, was significantly improved from 56.9 ± 20.6 preoperatively to 4.2 ± 10.1 at the 1-year assessment (p < 0.001). Radial and palmar abduction also increased significantly from 46.0° ± 11.0° and 49.7° ± 8.8° preoperatively, respectively, to 58.4° ± 6.4° (p < 0.001) and 59.5° ± 6.3° (p < 0.001), respectively, at 12 months postoperatively. Both male and female tip pinch increased significantly from 4.2 ± 1.8 and 3.0 ± 1.4 preoperatively, respectively, to 6.1 ± 1.9 (p = 0.002) and 4.3 ± 1.4 (p < 0.001) at the 1-year postoperative evaluation. We observed no impingement of the first metacarpal and scaphoid bones due to sinking of the first metacarpal bone, and repeat surgery due to rupture of the reconstructed ligament or fractures at the bone hole, was not needed for the 101 hands followed for approximately 1 year and the 29 hands followed over 4 years.
Conclusions:
Trapeziectomy combined with graft-augmented ligament reconstruction, using a reinforced half-slip ECRL tendon wrapped 3 times, may serve as an effective treatment option for primary thumb carpometacarpal osteoarthritis. This approach offers significant pain relief, improved range of motion and pinch strength, and prevents postoperative impingement of the first metacarpal across all Eaton stages in the short - medium term.
Level of Evidence:
Therapeutic Level Ⅳ. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Carpometacarpal (CM) joint osteoarthritis of the thumb is the second most common degenerative arthritis of the hand1. Treatment modalities for osteoarthritis of the thumb CM joint include arthrodesis2-4, artificial joint replacement5,6, metacarpal osteotomy7, and ligament reconstruction using various tendons following trapeziectomy8-11. Recently, ligament reconstruction using new materials has also been described12,13. CM joint arthrodesis is a popular method that provides good pain relief, is durable, and improves pinch force; however, thumb range of motion becomes limited, and peritrapezial degenerative changes are occasionally observed postoperatively2-4. Since Burton et al. first reported a trapeziectomy with ligament reconstruction and tendon interposition (LRTI) in 1986, alternative approaches have been reported, but the LRTI method remains the most popular14. However, the most concerning drawback of post-trapeziectomy ligament reconstruction is proximal migration of the first metacarpal bone. To address these concerns, a surgical method using the extensor carpi radialis longus (ECRL) tendon has been developed to reconstruct ligaments between the first and second metacarpals at the shortest distance11. However, questions remain about strength, because the ECRL is half-slipped. The purpose of this study was to assess clinical outcomes and verify effectiveness of graft reinforcement in patients who underwent our modified surgical procedure.
Materials and Methods
Study Design
Written informed consent was obtained from all patients before enrollment. All patients were Japanese. This study conformed to the principles outlined in the Declaration of Helsinki, was approved by the Institutional Review Board and Ethics Committee of Kumamoto University Hospital (approval number: 2,999) and was carried out in accordance with clinical study guidelines.
In principle, surgical procedures were considered only for patients not responding satisfactorily to conservative treatments for at least 3 to 6 months, and patients with rheumatoid arthritis, previous wrist and hand fractures, and adjunct or previous hand surgery were excluded.
Clinical Data Collection
We collected data from all patients at 8-weeks, 12-weeks, 6-months, 1-year, and from 29 hands (26 patients) at 4 or more years postoperatively. The following parameters were evaluated: 1, visual analog scale (VAS) for pain15; 2, postoperative active range of motion in radial and palmar abduction; 3, tip pinch collected by gender; and 4, patient-reported upper extremity disability based on the Japanese Society for Surgery of the Hand version of the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire16.
The distance from the center of the proximal end of the first metacarpal to the center of the distal end of the scaphoid was measured by x-ray at 12-weeks, 6-months, 1-year for all patients, and at 4 or more years (average 64.3 months) for 27 hands (25 patients). Patients were enrolled under a standardized protocol strictly followed throughout the 7-year period of data collection.
Surgical Methods
We devised a novel surgical approach to treat osteoarthritis of the thumb CM joint by trapeziectomy coupled with ligament reconstruction utilizing a reinforced half-slip of the ECRL tendon. Surgery was performed on an outpatient basis. Patients were anesthetized with intravenous regional block using 15–18-mL 2% intravenous xylocaine diluted two-fold, and a double tourniquet was applied on the forearm17.
An approximately 3.5-cm first incision through the area near the metacarpal bone to the dorsal side of the trapezium was made between the extensor pollicis longus and extensor pollicis brevis (Fig. 1A). A second incision of approximately 3 cm was then made to expose the ECRL tendon and create an approximately 8-cm half-slip by half-slipping the ECRL tendon from the ECRL tendon attachment of the second metacarpal bone (M2) and cutting it at approximately 8 cm from the ECRL tendon attachment of M2 (Fig. 1-A and Video 1). Then, the trapezium was completely removed, piece by piece (Fig. 1-B). Using a 3.5-mm drill, a hole was drilled at the center of the metacarpal thumb CM joint surface through the central dorsal base of the first metacarpal bone. After drilling, a half-slip ECRL tendon was created as a graft, as shown in Fig. 1-C and Video 1, and the distal site of the pedicled half-slip of the ECRL tendon was passed through a subcutaneous tunnel between the remaining ECRL tendon and subcutis, and then looped around the remaining ECRL tendon at the trapeziectomy gap, so that the remaining ECRL tendon could serve as a pulley (Fig. 1-D and Video 1). The graft end was then pulled out from the bony hole in the joint surface of the M1 to the dorsal side (Fig. 1-E and Video 1). With the thumb in ample palmar abduction, a 1.5-mm diameter Kirschner wire was inserted through the M1 and M2 for fixation. Next, the half-slip of the ECRL tendon graft was drawn to the dorsal side of the first metacarpal bone and folded back into the gap made by the trapeziectomy (Fig. 1-F) and then wound around the remaining half-slip ECRL tendon located between M1 and M2 tightly, and mattress-sutured 3 times (Figs. 1-F and 1-G, and Video 1). Two additional tight wraps around the remaining half-slip ECRL tendon with the half-slip ECRL tendon graft, each secured with 3 mattress sutures, were made (Video 1). A bone peg and a 3-mm diameter (7-mm long) TJ screw18 were inserted into the hole to crimp the ECRL half-slip, and the wound was closed (Video 1).
Fig. 1.
Surgical procedures. An approximately 3.5-cm first incision from the metacarpal bone to the dorsal side of the trapezium was made, followed by a second incision of approximately 3 cm (Fig. 1-A). The trapezium was then completely removed (Fig. 1-B). The ECRL tendon insertion and approximately 8 cm proximal to the ECRL tendon from that insertion were dissected. (Fig. 1-C). A distal-based pedicled half-slip of the ECRL tendon was then inserted into the trapeziectomy gap by passing it under the remaining half-slip of the ECRL tendon using it as a pulley (Fig. 1-D). The distal-based pedicled half-slip of the ECRL tendon was then pulled out from the bone hole made in the joint surface of the first metacarpal bone to the dorsal side (Fig. 1-E). The distal-based half-slip of the ECRL tendon drawn to the dorsal side of the first metacarpal bone was folded back into the gap made by the trapeziectomy and woven to reinforce the reconstructed ligament (Fig. 1-F). Illustration showing how the ECRL tendon was woven 3 times (Fig. 1-G). ECRL = extensor carpi radialis longus.
Postoperative therapy consisted of immobilizing the thumb for 6 weeks with a thumb spica splint. The Kirschner wire was removed during postoperative week 3. For postoperative weeks 6 to 12, patients were allowed free movement without restrictions on activities-of-daily-living while wearing an orthosis.
Statistical Analyses
All results are presented as means ± standard deviations. Student's t-test was used to compare preoperative and postoperative data relevant to each examination item if the data was parametric. If the data was nonparametric, the Friedman test, non-parametric statistical tests, was used to evaluate overall differences, and Wilcoxon signed rank test with Bonferroni correction was performed as a post-hoc analysis. Statistical significance was considered as a p value < 0.05.
Results
Patient Series
From February 2015 to March 2022, 101 hands (80 from females, 21 from males) from 95 patients underwent our newly developed trapeziectomy with graft-augmented ligament reconstruction procedure for thumb CM joint osteoarthritis. Age at surgery ranged from 45 to 87 years, with a mean of 66.9 (21 hands of 19 men; 80 hands of 77 women). All patients were assessed at for at least 1 year after surgery (12-100 months, average 31.4 months). Of the 101 hands, 51 (49 patients) were followed up for 1 to 2 years, 16 (16 patients) for 2 to 3 years, 5 (5 patients) for 3 to 4 years, and 29 (26 patients) for more than 4 years after surgery, thus 49.5% of patients were followed up for more than 2 years postoperatively. The range of time for follow-up for hands observed at or before 4 years was 12 to 46 months (average 18.3). Relevant to Eaton classification19, 29, 60, and 12 hands were classified as being at stages II, III, and Ⅳ, respectively.
VAS Score at Rest or Motion
The average preoperative VAS score gradually decreased over time (Fig. 2-A). Relative to preoperative conditions, pain at rest was significantly decreased by 8 weeks after surgery (p < 0.001; Fig. 2-A). Pain at rest continued to gradually improve and reached zero in all but 8 of 101 patients by 1 year postoperatively (Fig. 2-A). All 27 hands assessed 4 years after surgery had a VAS score at rest of 0 (Fig. 2-B).
Fig. 2.
Pain at the thumb CM joint at rest (Figs. 2-A and 2-C) or in motion (Figs. 2-B and 2-D) is significantly improved by surgery. Pain at the thumb CM joint at rest (Figs. 2-A and 2-C) or in motion (Figs. 2-B and 2-D) was evaluated by the VAS prior to and then at 8 weeks, 12 weeks, 6 months, 1 year and final (average 31.3 months) after surgery. 29 (26 patients) were assessed at more than 4 years after surgery (average 64.3 months). Data represents mean VAS at rest or in motion ± SD (n = 101 in Figs. 2-A and 2-C, 27 in Figs. 2-B and 2-D respectively, *p < 0.05). VAS = visual analogue scale.
Relative to preoperative values, the average VAS score at motion post-surgery gradually decreased over time, exhibiting a significant decrease by 8 weeks after surgery (p < 0.001; Fig. 2-C). A VAS score at motion of 0 was recorded in 39 (38.6%), 58 (57.4%), and 77 (76.2%) patients at 12 weeks, 6, and 12 months postoperatively, respectively. In patients assessed at >4 years postoperatively, 26 of 27 hands evaluated were free of pain on movement, with a VAS score at motion of 0 (Fig. 2-D).
Radial Abduction and Palmar Abduction
The average preoperative value of radial abduction in 101 hands improved significantly by 8 weeks postoperatively (p < 0.001; Fig. 3-A). Range of motion of radial abduction was improved in patients who were followed over 4 years (Fig. 3-B).
Fig. 3.
Range of the motion of the thumb CM joint is significantly improved by surgery. Radial (Figs. 3-A and 3-C) or palmar (Figs. 3-B and 3-D) abduction was evaluated prior to and then at 8 weeks, 12 weeks, 6 months, 1 year, and final (average 31.3 months) after surgery. 29 (26 patients) were assessed at more than 4 years after surgery (average 64.3 months). Data represents mean radial or palmar abduction ± SD (n = 101 in both Figs. 3-A and 3-C, 27 in both Figs. 3-B and 3-D, respectively, *p < 0.05).
Average preoperative palmar abduction values improved significantly by 8 weeks postoperatively in 101 hands (p < 0.001; Fig. 3-C). Range of motion of palmar abduction further improved in patients followed over 4 years (Fig. 3-D).
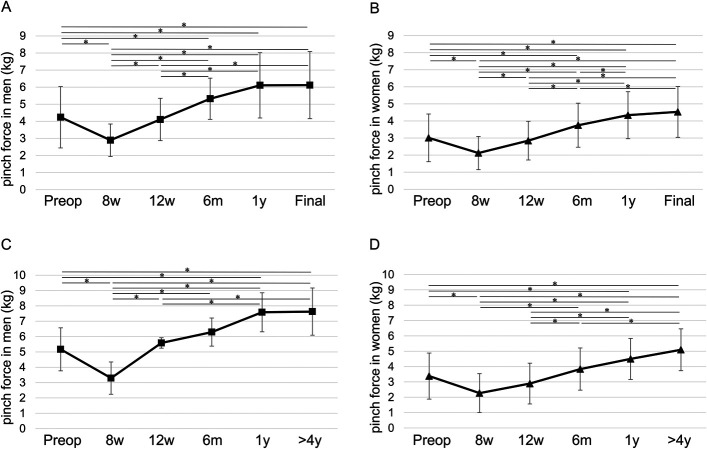
Tip Pinch
Average values of preoperative pinch force in men and women were 4.2 ± 1.8 kg and 3.0 ± 1.4 kg, respectively. By 1 year postoperatively, pinch force in men and women had significantly increased to 6.1 ± 1.9 and 4.3 ± 1.4, respectively (p = 0.002 and p < 0.001, Figs. 4-A and 4-B). For hands followed over 4 years, pinch force in 7 hands of men and 20 hands of women improved further to 7.5 ± 1.8 and 5.1 ± 1.3 kg, respectively (Figs. 4-C and 4-D).
Fig. 4.
Tip pinch force is significantly improved by surgery. Tip pinch force was evaluated in men (Figs. 4-A and 4-C) and women (Figs. 4-B and 4-D) prior to and then at 8 weeks, 12 weeks, 6 months, 1 year, and final (average 31.3 months) after surgery. 29 (26 patients) were assessed at more than 4 years after surgery (average 64.3 months). Data represents mean tip pinch force ± SD (n = 21 (Fig. 4-A), 80 (Fig. 4-B), 7 (Fig. 4-C) and 20 (Fig. 4-D), respectively, *p < 0.05).
Three Finger (Thumb, Index and Middle) Pinch
Similar to tip pinch, 3 finger (thumb, index and middle) pinch force also significantly improved following surgery. Those values in men and women were 6.1 ± 2.1 kg and 4.0 ± 1.8 kg, respectively, and significantly improved to 8.0 ± 1.7 and 5.2 ± 1.6, respectively, by 1 year postoperatively (p = 0.002 and p < 0.001, Figs. 5-A and 5-B). For the 27 hands assessed at more than 4 years, 3 finger pinch force in 7 hands of men and 20 hands of women improved further to 9.3 ± 2.5 and 6.3 ± 1.6 kg, respectively (Figs. 5-C and 5-D).
Fig. 5.
Three finger (thumb, index and middle) pinch is significantly improved by surgery. Three finger pinch force was evaluated in men (Figs. 5-A and 5-C) and women (Figs. 5-B and 5-D) prior to and then at 8w, 12w, 6 m, 1 y, and final (average 31.3 m) after surgery. 29 (26 patients) were assessed at more than 4 years after surgery (average 64.3 months). Data represents mean 3 finger pinch force ± SD (n = 21 (Fig. 5-A), 80 (Fig. 5-B), 7 (Fig. 5-C) and 20 (Fig. 5-D), respectively, *p < 0.05).
DASH Disability and Work Scores
Preoperative DASH disability and work scores decreased over time (Figs. 6-A and 6-B). Both scores significantly improved by 12 weeks postoperatively (each p < 0.001; Figs. 6-A and 6-B). DASH disability and work scores continued to improve through the first postoperative year. In the 27 hands assessed at more than 4 years, although not statistically significant, both scores were better at 4 years after surgery than they were at 1 year after surgery.
Fig. 6.

DASH disability and work scores are significantly improved by surgery. DASH disability (Fig. 6-A) and work (Fig. 6-B) scores were evaluated prior to and then at 8 weeks, 12 weeks, 6 months, 1 year, and final (average 31.3 months) after surgery. 29 (26 patients) were assessed at more than 4 years after surgery (average 64.3 months). Data represents mean DASH disability and work scores ± SD (n = 101, *p < 0.05). DASH = disabilities of the arm, shoulder, and hand.
Migration of the First Metacarpal
Because patients had undergone trapeziectomy, we measured the distance from the center of the central end of the first metacarpal to the center of the distal end of the scaphoid radiographically in 27 hands (25 patients) to determine whether the first metacarpal had migrated into the space left by removal of the trapezium after removal of the trapezium. At 12 weeks postoperatively, this distance had indeed shortened to an average of 56.3% (31.4%-71.4%) of its preoperative value, but was maintained at 55.7% (34.1%-73.6%) at 6 months postoperatively, at 56.4% (37.2%-81.1%) at 1 year postoperatively, and at 52.9% (26.2%-70.5%) in the group assessed more than 4 years later (Supplementary Table 1). As a result, we observed no impingement of the first metacarpal and scaphoid bones due to sinking of the first metacarpal bone.
Discussion
To date, various surgical procedures including trapeziectomy with intermetacarpal ligament reconstruction have been proposed to treat thumb CM joint arthritis in patients who do not respond to conservative therapy for more than 3 to 6 months20,21. Overall, we feel that our procedure has several advantages over previous surgical methods used to treat thumb CM joint arthritis. One of those is arthrodesis, which has been an effective method to eliminate pain in the CM joint. However, arthrodesis limits activity of daily life due to limited range of motion of the thumb. Trapezium removal relieves pain by eliminating bone impingement, while subsequent ligament reconstruction stabilizes the first and second metacarpal bones. In the context of pain relief, meta-analysis suggests that LRTI outcomes seen following trapeziectomy are not superior to trapeziectomy alone at up to 1 year postoperative follow-up22,23. While these findings do not demonstrate a clear advantage of LRTI over simple trapeziectomy in the short term, a small population of patients undergoing trapeziectomy alone have been reported to develop significant CM joint instability and some degeneration22. Simple trapeziectomy was also reported caused secondary metacarpo-scaphoid arthritis in the long term resulting from proximal migration of the first metacarpal bone, necessitating secondary revision surgery24. Thus, trapeziectomy alone has the risk of postoperative pain and revision due to impingement caused by migration of the first metacarpal bone after surgery25. In contrast, none of patients treated with our surgical procedure developed CM joint instability during follow-up more than 4 years. Moreover, no patient experienced pain or required revision surgery due to postoperative impingement by migration of the first metacarpal bone (Supplementary Table 1). Ligament reconstruction with Flexor Carpi Radialis (FCR) was first developed to prevent first metacarpal instability after partial or total trapeziectomy to treatment thumb CM joint arthritis8,9. While suspension arthroplasty using the FCR tendon shows generally good results26, rupture has been reported in FCR used for suspension arthroplasty or ligament reconstruction27-29. Artificial materials such as TightRope used for ligament reconstruction or suspension arthroplasty also have their limitations, such as potential damage to that material and metacarpal bone fracture, as reported previously30-32. Additionally, CM joint replacement, while offering anatomical reconstruction, is associated with higher costs and potential risks of implant failure and loosening33,34. Arthroscopic debridement has demonstrated superiority over conventional nonoperative management in terms of pain relief, however, its indication is limited to early-stage disease, Eaton stages I and II35. We applied our procedure to stage II–IV cases, but half-slipped ECRL raised concerns about reconstructed ligament strength. Indeed, we observed impingement of the first metacarpal on the scaphoid in 1 of 7 individuals who underwent the procedure with a half-slipped ECRL tendon without wrapping 3 times, likely due to graft rupture or dysfunction (Supplementary Fig. 1). We concluded it was necessary to increase strength of the reconstructed ligament, which is the half-slip ECRL tendon, in order to maintain it over the long term. To do so, we reinforced the reconstructed ligament by creating a pulley with a half-slip ECRL tendon and by wrapping the reconstructed ligament 3 times with the half-slip ECRL tendon. As a result, in the 101 hands evaluated for 1 year, and in 29 hands that were followed for >4 years, clinical outcomes after our surgical procedure did not greatly differ from results seen in previously reported methods9,16,36. We also observed no rupture of the reconstructed ligament and no impingement of M1 and scaphoid bones resulting from migration of M1. These significantly improved clinical outcomes were maintained for at least 1 year postoperatively.
Patients in this study had a tip pinch of 6.1 (men) and 4.3 kg (women) at 1 year postoperatively. Moreover, in 29 hands followed postoperatively for over 4 years, tip pinch of men and women was at 7.5 and 5.1 kg, respectively. Since tip pinch of 60-year-old healthy individuals is approximately 7 kg for men and 4.5 kg for women37, we conclude that our method represents an improvement in pinch-strength.
The 101 hands observed postoperatively included 29 hands classified at Stage II based on the Eaton classification. In this series, we observed the articular surfaces of Eaton classification Stage II hands intraoperatively, and they showed cartilage degeneration or partial loss and osteosclerosis. Nevertheless, surgical outcomes following our procedure were positive for all hands at different classifications. Thus, we feel that in Stage-II cases involving mild osteophyte formation and articular surface dislocation, the new method is indicated in cases of obstinate pain.
Surgery requiring drilling of a hole in the M1 and M2 requires caution when performed on older patients with osteoporosis, as they are at a higher risk of metacarpal bone fracture. Since our method does not involve transversal drilling of the M1, fracture risk is less likely, as evidenced by the fact that none of the patients in our study experienced fractures. Illarramendi A et al. reported fixation for 6-weeks postoperatively with a K-wire following trapeziectomy and intermetacarpal ligament reconstruction with ECRL11. We fixed the M1 and M2 with K-wires for 3 weeks, allowing reconstructed ligaments to be firmly tensed and to prevent ligament rupture after surgery.
Although a limitation to this study is that we did not directly compare postoperative clinical outcomes with other methods, we do report those surgical outcomes for at least one-year following after use of our method. Longer-term follow-up may be needed to confirm that the reconstructed tendon is maintained, that there are no fractures at bone holes, and that good clinical outcomes are preserved.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A882, http://links.lww.com/JBJSOA/A883, https://avs.jbjs.org/video/6367613861112). This content was not copyedited or verified by JBJS.
Footnotes
T. Kato and K. Ideo contributed equally to this work.
Investigation performed at the Kato Orthopedic Clinic, Okazaki, Japan and Kumamoto University Hospital, Kumamoto, Japan
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A881).
Contributor Information
Teiji Kato, Email: kteiji@yahoo.co.jp.
Katsumasa Ideo, Email: kacofkac@kuh.kumamoto-u.ac.jp.
References
- 1.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, Pols HA, Hazes JM, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. 2005;64(5):682-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hattori Y, Doi K, Dormitorio B, Sakamoto S. Arthrodesis for primary osteoarthritis of the trapeziometacarpal joint in elderly patients. J Hand Surg. 2016;41(7):753-9. [DOI] [PubMed] [Google Scholar]
- 3.Fulton DB, Stern PJ. Trapeziometacarpal arthrodesis in primary osteoarthritis: a minimum two-year follow-up study. J Hand Surg. 2001;26(1):109-14. [DOI] [PubMed] [Google Scholar]
- 4.Rizzo M, Moran SL, Shin AY. Long-term outcomes of trapeziometacarpal arthrodesis in the management of trapeziometacarpal arthritis. J Hand Surg. 2009;34(1):20-6. [DOI] [PubMed] [Google Scholar]
- 5.Huang K, Hollevoet N, Giddins G. Thumb carpometacarpal joint total arthroplasty: a systematic review. J Hand Surg Eur. 2015;40(4):338-50. [DOI] [PubMed] [Google Scholar]
- 6.Cooney WP, Linscheid RL, Askew LJ. Total arthroplasty of the thumb trapeziometacarpal joint. Clin Orthop Relat Res. 1987;220:35-45. [PubMed] [Google Scholar]
- 7.Hobby JL, Lyall HA, Meggitt BF. First metacarpal osteotomy for trapeziometacarpal osteoarthritis. The J Bone Joint Surg Br. 1998;80-B(3):508-12. [DOI] [PubMed] [Google Scholar]
- 8.Burton RI, Pellegrini VD, Jr. Surgical management of basal Joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplast. J Hand Surg. 1986;11(3):324-32. [DOI] [PubMed] [Google Scholar]
- 9.Tomaino MM, Pellegrini VD, Jr., Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg. 1995;77(3):346-55. [DOI] [PubMed] [Google Scholar]
- 10.Diao E. Trapezio-metacarpal arthritis. Trapezium excision and ligament reconstruction not including the LRTI arthroplasty. Hand Clin. 2001;17(2):223-36. [PubMed] [Google Scholar]
- 11.Illarramendi AA, Boretto JG, Gallucci GL, De Carli P. Trapeziectomy and intermetacarpal ligament reconstruction with the extensor carpi radialis longus for osteoarthritis of the trapeziometacarpal joint: surgical technique and long-term results. J Hand Surg. 2006;31(8):1315-21. [DOI] [PubMed] [Google Scholar]
- 12.Yao J, Song Y. Suture-button suspensionplasty for thumb carpometacarpal arthritis: a minimum 2-year follow-up. J Hand Surg. 2013;38(6):1161-5. [DOI] [PubMed] [Google Scholar]
- 13.Endress RD, Kakar S. Double tightrope for basilar thumb arthritis. J Hand Surg. 2014;39(12):2512-6. [DOI] [PubMed] [Google Scholar]
- 14.Yuan F, Aliu O, Chung KC, Mahmoudi E. Evidence-based practice in the surgical treatment of thumb carpometacarpal joint arthritis. J Hand Surg. 2017;42(2):104-12.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huskisson EC. Measurement of pain. Lancet. 1974;304(7889):1127-31. [DOI] [PubMed] [Google Scholar]
- 16.Imaeda T, Toh S, Nakao Y, Nishida J, Hirata H, Ijichi M, Kohri C, Nagano A. Validation of the Japanese society for surgery of the hand version of the disability of the Arm, shoulder, and hand questionnaire. J Orthop Sci. 2005;10(4):353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tucker GT, Boas RA. Pharmacokinetic aspects of intravenous regional anesthesia. Anesthesiology. 1971;34(6):538-49. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka J, Yanagida H. Reconstruction of the ligament using an interference screw (tendon junction screw). Tech Hand Upper Extremity Surg. 2001;5(1):57-62. [DOI] [PubMed] [Google Scholar]
- 19.Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg. 1973;55(8):1655-66. [PubMed] [Google Scholar]
- 20.Spaans AJ, van Minnen LP, Kon M, Schuurman AH, Schreuders AR, Vermeulen GM. Conservative treatment of thumb base osteoarthritis: a systematic review. J Hand Surg. 2015;40(1):16-21.e6. [DOI] [PubMed] [Google Scholar]
- 21.Tsehaie J, Porsius JT, Rizopoulos D, Slijper HP, Feitz R, Hovius SER, Selles RW. Response to conservative treatment for thumb carpometacarpal osteoarthritis is associated with conversion to surgery: a prospective cohort study. Phys Ther. 2019;99(5):570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosales RS, Gonzalez-Garcia A, Dorta-Fernandez A, Heras-Palou C. A meta-analysis of the outcomes of ligament reconstruction compared to No reconstruction with or without tendon interposition following trapeziectomy for thumb carpometacarpal joint osteoarthritis. The J Hand Surg Asian Pac Vol. 2022;27(01):22-31. [DOI] [PubMed] [Google Scholar]
- 23.Wilcke MK, Evans K, Franko MA, Arner M. Trapeziectomy with or without a tendon-based adjunct: a registry-based study of 650 thumbs. J Hand Surg Eur Vol. 2022;47(7):728-33. [DOI] [PubMed] [Google Scholar]
- 24.Liu Q, Xu B, Lyu H, Lee JH. Differences between simple trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition for the treatment of trapeziometacarpal osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2022;142(6):987-96. [DOI] [PubMed] [Google Scholar]
- 25.Rouveyrol M, de Villeneuve Bargemon JB, Levet P, Mattéi JC, Legré R, Jaloux C. Revision of trapeziectomy failures in thumb base osteoarthritis: retrospective analysis of ten cases and review of the literature. Hand Surg Rehabil. 2021;40(4):464-71. [DOI] [PubMed] [Google Scholar]
- 26.Altissimi M, Pataia E, Rampoldi M, Azzarà A, Braghiroli L. Trapeziectomy and suspension arthroplasty with the flexor carpi radialis tendon for treatment of trapeziometacarpal osteoarthritis. Hand Surg Rehabil. 2021;40(2):162-6. [DOI] [PubMed] [Google Scholar]
- 27.Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg. 2000;25(4):350-6. [DOI] [PubMed] [Google Scholar]
- 28.DelSignore JL, Zambito K, Ballatori SE. Suture suspension arthroplasty for thumb carpometacarpal arthritis reconstruction: 12- to 14-year follow-up. Hand (N Y). 2023;18(1):105-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kawamura D, Funakoshi T, Iwasaki N. Trapeziectomy with ligament reconstruction and interposition arthroplasty using the palmaris longus tendon: an average 5-year follow-up. Clin Orthop Surg. 2019;11(4):453-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khalid M, Jones ML. Index metacarpal fracture after tightrope suspension following trapeziectomy: case report. J Hand Surg. 2012;37(3):418-22. [DOI] [PubMed] [Google Scholar]
- 31.Mufty S, Peters SJ. Fracture of the index metacarpal after TightRope suspension for carpometacarpal instability of the thumb. J Hand Surg (European Volume). 2016;41(9):1000-1. [DOI] [PubMed] [Google Scholar]
- 32.Ruff LR, Delgadillo BE, El-Bahri GF. Management of a traumatic collapse of the first carpometacarpal joint after trapeziectomy with suture suspensionplasty: a case report. Cureus. 2024;16(5):e60216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shintaku T, Nakayama M, Ishii H, Yagi M, Ikegami H. Long-term outcome over 15 Years of prosthesis for thumb carpometacarpal joint arthritis: a case series. Cureus. 2024;16(11):e73480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holme TJ, Karbowiak M, Clements J, Sharma R, Craik J, Ellahee N. Thumb CMCJ prosthetic total joint replacement: a systematic review. EFORT Open Rev. 2021;6(5):316-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Furia JP. Arthroscopic debridement and synovectomy for treating basal joint arthritis. Arthrosc. 2010;26(1):34-40. [DOI] [PubMed] [Google Scholar]
- 36.Uriburu IJ, Olazábal AE, Ciaffi M. Trapeziometacarpal osteoarthritis: surgical technique and results of “stabilized resection-arthroplasty”. J Hand Surg. 1992;17(4):598-604. [DOI] [PubMed] [Google Scholar]
- 37.Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66(2):69-74. [PubMed] [Google Scholar]