Abstract
Context
As the availability of and demand for genetic testing for hereditary cancers increases in primary care and other clinical settings, alternative or adjunct educational methods to traditional genetic counseling will be needed.
Objective
To compare the effectiveness of a computer-based decision aid with standard genetic counseling for educating women about BRCA1 and BRCA2 genetic testing.
Design
Randomized controlled trial conducted from May 2000 to September 2002.
Setting and Participants
Outpatient clinics offering cancer genetic counseling at 6 US medical centers enrolled 211 women with personal or family histories of breast cancer.
Interventions
Standard one-on-one genetic counseling (n=105) or education by a computer program followed by genetic counseling (n=106).
Main Outcome Measures
Participants’ knowledge, risk perception, intention to undergo genetic testing, decisional conflict, satisfaction with decision, anxiety, and satisfaction with the intervention. Counselor group measures were administered at baseline and after counseling. Computer group measures were administered at baseline, after computer use, and after counseling. Testing decisions were assessed at 1 and 6 months. Outcomes were analyzed by high vs low risk of carrying a BRCA1 or BRCA2 mutation.
Results
Both groups had comparable demographics, prior computer experience, medical literacy, and baseline knowledge of breast cancer and genetic testing, and both counseling and computer use were rated highly. Knowledge scores increased in both groups (P<.001) regardless of risk status, and change in knowledge was greater in the computer group compared with the counselor group (P=.03) among women at low risk of carrying a mutation. Perception of absolute risk of breast cancer decreased significantly after either intervention among all participants. Intention to undergo testing decreased significantly after either intervention among low-risk but not high-risk women. The counselor group had lower mean scores on a decisional conflict scale (P=.04) and, in low-risk women, higher mean scores on a satisfaction-with-decision scale (P=.001). Mean state anxiety scores were reduced by counseling but were within normal ranges for both groups at baseline and after either intervention, regardless of risk status.
Conclusions
An interactive computer program was more effective than standard genetic counseling for increasing knowledge of breast cancer and genetic testing among women at low risk of carrying a BRCA1 or BRCA2 mutation. However, genetic counseling was more effective than the computer at reducing women’s anxiety and facilitating more accurate risk perceptions. These results suggest that this computer program has the potential to stand alone as an educational intervention for low-risk women but should be used as a supplement to genetic counseling for those at high risk.
IN RECENT YEARS, GENETIC TESTING for inherited cancer predisposition has become widely available.1–3 Initially, the use of such testing was limited to those enrolled in research studies at specialized medical centers. However, developments in testing technology and widespread publicity in the news media have led to increased testing for conditions such as breast cancer susceptibility4,5 in primary care6–8 and other settings, raising questions about how to adequately inform patients about their personal breast cancer risk and the pros and cons of genetic testing.9–11 Professional organizations advise that people who want to learn about their options and alternatives regarding genetic testing should be referred to specialists such as genetic counselors.12–14 However, there are only about 400 genetic counselors in the United States who identify themselves as specializing in cancer genetics,15 and cancer genetic counselors are not available in some regions of the United States, especially outside of major urban areas. Consequently, the demand for education and counseling about inherited cancer risk is likely to outstrip the supply of cancer genetics specialists,16,17 and there is a pressing need to find effective ways to deliver factual information about breast cancer risk and genetic testing in light of the limited access to these services.
A variety of educational materials help address this informational need,18 including brochures and booklets,19,20 Web sites,21,22 and videotapes,23 but few have been rigorously evaluated for their effectiveness in educating their target audience, and none can replicate a detailed discussion between a counselor and client. In response to this information gap, a group led by the first author (M.J.G.) developed an interactive, multimedia, computer-based decision aid (“Breast Cancer Risk and Genetic Testing”) to educate individuals and help facilitate informed decision making about genetic testing for breast cancer susceptibility.24 This computer program has undergone extensive peer review,25–28 and it was evaluated in a small randomized trial, in which it was found to be acceptable to cancer genetic counselors and their clients29 and effective at increasing clients’ knowledge about breast cancer risk and genetic testing.30
As a follow-up to the initial reviews and evaluation, we revised and updated the program and conducted a larger multicenter randomized trial among women with family or personal histories of breast cancer. In this study, we directly compared our interactive computer program with standard one-on-one counseling, assessing the impact of each on women’s knowledge, perception of risk, decisions about genetic testing, postintervention decisional conflict, and satisfaction with the educational method. We also determined whether these outcomes differed between women at high vs low risk of carrying a BRCA1 or BRCA2 mutation and whether these 2 risk groups derived different benefits from the computer-based intervention.
METHODS
Study Participants
Participants were recruited between May 2000 and September 2002 at 6 study sites (Penn State College of Medicine, Hershey, Pa; Lehigh Valley Hospital and Health Network, Allentown, Pa; University of Pittsburgh Medical Center, Pittsburgh, Pa; The University of Texas M. D. Anderson Cancer Center, Houston; Baylor College of Medicine, Houston; and Evanston Northwestern Healthcare, Evanston, Ill). The research protocol received institutional review board (IRB) approval at each of the participating sites and was monitored by each local IRB. Women were eligible to participate if they were 18 years or older; able to read, write, and speak English; referred for genetic counseling for evaluation of personal or family history of breast cancer; and able to give informed consent. Women who previously had undergone genetic counseling or testing for inherited breast cancer susceptibility were excluded. Potential participants were identified by counselors or other staff when clients scheduled counseling appointments. All women meeting eligibility criteria were invited to participate by mail, telephone, or in-person contact and were informed that using the computer program and/or meeting with a counselor could take up to 3 hours. Anyone who was unable or unwilling to allot this amount of time was excluded. All eligible women who agreed to participate provided written informed consent. Participants received a small gift in recognition of their participation.
Randomization and Study Design
To ensure balance in each arm of the study, we used separate computer-generated randomization lists for low-risk and high-risk individuals at each study site. Low risk was defined as less than 10% chance of carrying a deleterious BRCA1 or BRCA2 mutation, and high risk was defined as 10% or higher chance, as calculated by using the BRCAPRO model.31 Participants were assigned to the intervention groups using the appropriate randomization list for their risk category. Those enrolled in the counselor group received standard genetic counseling, including education and risk assessment. Those in the computer group used the interactive computer-based educational program about breast cancer risk and genetic testing and then received standard genetic counseling.
Procedures
All participants first completed a baseline questionnaire on or just before the day of their counseling appointments. Participants who were randomized to the counselor group proceeded directly to their genetic counseling appointments after completing the baseline questionnaire and, after counseling, completed an additional questionnaire. Participants assigned to the computer group were introduced to the computer program after completing their baseline questionnaire. Individuals who were unfamiliar with interactive computer programs were directed to the optional instructions and guidance at the beginning of the program. Aside from this introduction, staff did not assist participants as they used the program. Women proceeded through the program at their own pace. Immediately after using the program and before their counseling appointments, computer group participants completed a subset of postintervention measures identical to those completed by the counselor group. They then proceeded to their counseling appointments and completed additional measures after counseling. At 1 and 6 months after the study visit, we contacted participants by telephone and collected information about their genetic testing decisions.
Interventions
Breast Cancer Genetics Computer Program
The computer program, “Breast Cancer Risk and Genetic Testing”, has been described in detail elsewhere.24,32 It is an interactive, multimedia CD-ROM–based decision aid designed to educate women about breast cancer, heredity, and the benefits and limitations of genetic testing. The program’s main purpose is to help women make informed decisions about genetic testing for breast cancer susceptibility by addressing topics such as who is at risk of breast cancer, how genes affect cancer risk, and the pros and cons of testing. The program is easy to use, requires no prior experience with computers, and has been designed for women of various ages and educational levels. Since it is self-paced and user-driven, each user determines the order and sequence of accessing various sections, as well as the amount of time spent in each section. In this study, participants used the program for an average of 45 to 60 minutes.
Genetic Counseling
Genetic counseling was provided by 12 genetic counselors and 1 advanced practice nurse with specialty training in cancer genetics. All were experienced in counseling clients about cancer susceptibility and either had received instruction in cancer genetics as part of their formal training or had obtained additional continuing education through short courses, conferences, and other educational opportunities. Since cancer genetic counseling is individualized to meet the needs of persons with varying degrees of inherited cancer risk, it was not feasible to develop a common script for counselors. To ensure that counseling sessions contained similar content across counselors and study sites, the investigators and participating counselors identified a standard set of topics to be covered that was consistent with current practice guidelines33 and also with the information presented in the computer program.24 At some centers, physicians were available to clients at the end of the counseling session to reinforce medical management recommendations provided during the session and to answer questions.
Two features of the counseling sessions differed from the computer program. First, counselors (but not the computer program) provided individualized risk estimates for the likelihood of carrying a genetic mutation and of developing breast cancer. Second, the counseling included a psychosocial component to address emotional concerns if they were raised during discussions of breast cancer risk and genetic testing.34,35
Measures
Demographics
At baseline, participants were asked to provide demographic information (age, race/ethnicity, educational level, religion/religiosity) and to rate their degree of experience with computers and awareness of genetic testing.
Medical Literacy
Medical literacy was measured at baseline using the Rapid Estimate of Adult Literacy in Medicine (REALM), a reliable and valid measure of reading ability with regard to medical terminology.36 REALM consists of 66 medical words that a participant reads aloud to an interviewer. Each correctly pronounced word receives 1 point, for a maximum score of 66.
Knowledge
Knowledge about breast cancer, heredity, and genetic testing was measured at baseline and after the educational intervention. The knowledge measure was a 20-item multiple choice and true/false questionnaire modified from a core instrument used by the Cancer Genetics Studies Consortium of the National Human Genome Research Institute and National Cancer Institute.37 Similar versions have been used successfully in prior research.30,38,39
Perceived Risk
Perceived risk was assessed at baseline and after each intervention using 3 items. Perceived relative or comparative risk of developing breast cancer was assessed with a single item from the Cancer Genetics Studies Consortium core instruments: “In your opinion, compared to other women your age, what are your chances of developing breast cancer in the future?” Responses ranged from 1 (much lower) to 5 (much higher). Perceived absolute risk of developing breast cancer was assessed using the question, “What do you think your chances of getting breast cancer are on a scale of 0 to 100, where 0 is no chance of getting breast cancer and 100 means that you will definitely get it?” Perceived risk of having a genetic susceptibility to breast cancer was assessed with a single item modeled after questions developed by Weinstein40: “In your opinion, how likely is it that you have an inherited gene mutation for breast cancer susceptibility?” Responses ranged from 1 (not at all likely) to 4 (definitely).
Objective Mutation Carrier Risk
Counselors used the BRCAPRO model41 to calculate each participant’s estimated risk of carrying a BRCA1 or BRCA2 germline mutation. This model uses information from a woman’s family history of breast and ovarian cancer to determine her risk42 and is a widely accepted method for determining the probability of carrying mutations in BRCA1 and BRCA2 genes.31,43
Intention to Undergo Genetic Testing
Intention to undergo genetic testing was assessed at baseline, after each intervention, and after 1 and 6 months with a single item: “At the present time, which of the following statements describes your thoughts about having genetic testing for susceptibility to breast cancer?” Responses ranged from 1 to 6 and included, respectively, “(1) I haven’t thought about it; (2) I definitely will not get tested; (3) I probably will not get tested; (4) I probably will get tested; (5) I definitely will get tested; and (6) I was already tested (used at study visit to confirm that women already tested were excluded from the study).” For analysis, responses 2 through 5 were collapsed into 2 categories (“likely” and “unlikely” to be tested).
Decisional Conflict and Satisfaction With Decision
Decisional conflict was measured after the intervention in both groups using a validated 6-item scale with a 5-point Likert response format44 to assess the level of conflict women felt about their decisions regarding genetic testing. This scale measures perceptions of personal uncertainty in making a choice about health care options, the modifiable factors contributing to uncertainty, and the quality of the decision made. Items are summed and averaged to obtain scores ranging from 1 (low decisional conflict) to 5 (high decisional conflict). Satisfaction with decision regarding genetic testing was assessed after the intervention using the 6-item Satisfaction With Decision Scale.45 Scores on this validated instrument range from 6 (low satisfaction) to 30 (high satisfaction).
Anxiety
State anxiety was measured at baseline and after computer use and genetic counseling using the State Anxiety subscale of the Spielberger State-Trait Anxiety Inventory,46,47 a validated and widely used measure. The subscale includes 20 items and yields scores ranging from 20 (low anxiety) to 80 (high anxiety).
Evaluation of Computer Intervention and Genetic Counseling
Participants’ assessments of the strengths and weaknesses of both the computer intervention and genetic counseling were measured after the educational component with a 9-item scale developed for this study. Using a 4-point Likert response format (excellent, good, fair, and poor), participants assessed attributes such as how well each method presented factual information, dealt with emotional concerns, and tailored the intervention to the specific needs of the learners.
Statistical Analysis
Descriptive statistics were computed for all variables. Results of the 20-item knowledge measure were summarized as the percentage of correct responses. The decisional conflict, satisfaction with decision, and state anxiety instruments were summarized according to recommended algorithms.44–47 Knowledge was chosen as the primary outcome measure because informed decision making cannot take place without sufficient understanding of key factual information.48–50 Group differences in continuous outcomes were assessed by t test (cross-sectional outcomes) and repeated-measures analysis of variance (longitudinal outcomes). Group differences in categorical and ordinal outcomes were assessed by χ2 test or Fisher exact test (cross-sectional outcomes) and by ordinal or binary logistic regression using the generalized estimating equations approach (longitudinal outcomes). Four-and 5-point Likert scale responses were analyzed as ordinal outcomes. These responses were collapsed into a smaller number of categories when 1 or more levels had fewer than 5 responses. All P values reported were associated with 2-tailed tests of significance, and all analyses were carried out using SAS statistical software, version 8.1 (SAS Institute, Cary, NC). The study sample size (210 targeted enrollment) was chosen to provide 90% power (at the .05 significance level) to detect a 10% difference between groups with respect to knowledge scores.
RESULTS
Patient Enrollment and Characteristics
A total of 432 eligible women were invited to participate in the study and 288 (67%) agreed (Figure). Of these, 77 canceled or failed to keep their counseling appointments, and we enrolled 211 women into the study, distributing them equally between the counselor and computer groups. There were no statistically significant differences across the 6 study sites with respect to any outcomes reported herein.
Figure.
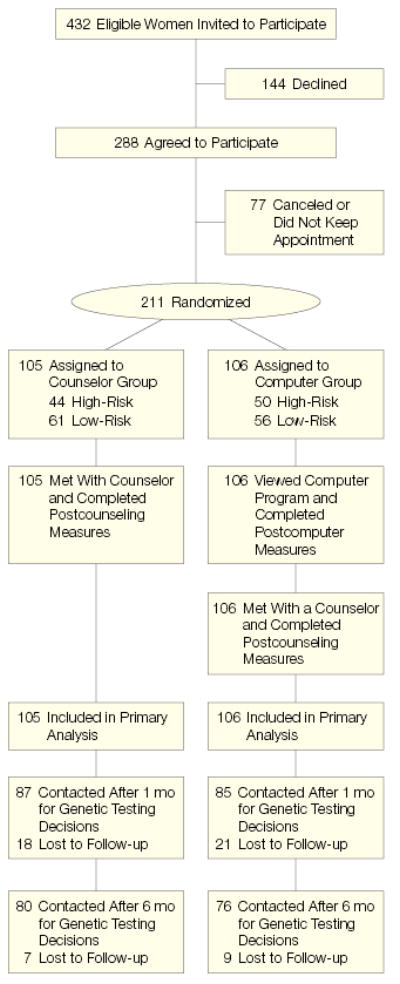
Flow of Study Participants
Baseline data are summarized in Table 1. The 2 groups were similar with respect to age, race/ethnicity, education, religion, religiosity, experience with computers, and personal history of breast cancer. High-risk and low-risk participants were evenly distributed across groups. Overall, 74% of the 211 participants were younger than 50 years, 56% had completed college or beyond, and 93% were white. A high proportion reported using a computer “often” or “sometimes” at home (63%) or at work (77%). The mean score on the REALM assessment of medical literacy was very high (65 on a scale of 1–66). Based on BRCAPRO estimates, 55% of participants had less than a 10% chance of carrying a BRCA1/2 mutation (low risk) and 45% of participants had a 10% chance or higher (high risk). Furthermore, 30% of participants had a personal history of breast cancer (excluding lobular carcinoma in situ or ductal carcinoma in situ). Those at high and low risk were similar with respect to most demographic characteristics, but high-risk individuals were younger (42 vs 47 years; P=.003) and more familiar with genetic testing (50% vs 36% reported reading or hearing “a fair amount” or “a lot” about genetic testing; P=.04).
Table 1.
Baseline Participant Characteristics*
| Characteristics | Counselor Group (n = 105) | Computer Group (n = 106) | P Value |
|---|---|---|---|
| Age, mean (range), y | 44 (24–71) | 45 (23–77) | .33 |
| Race/ethnicity | |||
| White | 95 (90) | 100 (95) | ].28 |
| African American | 6 (6) | 2 (2) | |
| Hispanic | 4 (4) | 2 (2) | |
| Education | |||
| ≥College degree | 53 (50) | 65 (62) | ].10 |
| <College degree | 52 (50) | 40 (38) | |
| Religion | |||
| Catholic | 27 (26) | 38 (37) | ].52 |
| Protestant or other Christian | 52 (50) | 45 (44) | |
| Jewish | 7 (7) | 7 (7) | |
| Other | 11 (11) | 7 (7) | |
| None | 6 (6) | 6 (6) | |
| “Very strong” religious or spiritual faith | 53 (50) | 47 (44) | .37 |
| Uses computer at work | |||
| Often or sometimes | 71 (72) | 83 (82) | ].40 |
| Rarely or never | 27 (28) | 18 (18) | |
| Uses computer to manage personal affairs | |||
| Often or sometimes | 63 (61) | 68 (65) | ].12 |
| Rarely or never | 40 (39) | 36 (35) | |
| Very confident with computer skills | 39 (37) | 44 (42) | .78 |
| “How much have you read or heard about genetic testing?” | |||
| Fair amount or a lot | 44 (42) | 45 (42) | ].98 |
| Almost nothing or relatively little | 60 (58) | 61 (58) | |
| REALM health literacy score, mean (range)† | 65 (55–66) | 65 (38–66) | >.99 |
| Calculated risk of carrying a BRCA1/2 mutation | |||
| High risk (≥10% chance) | 44 (42) | 50 (47) | ].40 |
| Low risk (<10% chance) | 61 (58) | 56 (53) | |
| Personal history of breast cancer | 29 (28) | 35 (33) | .37 |
Data are expressed as No. (%) unless otherwise indicated.
Rapid Estimate of Adult Literacy in Medicine (REALM) scale ranges from 0 to 66.36
Knowledge
Both genetic counseling and the interactive computer program were highly successful at increasing knowledge scores, and mean postintervention scores were significantly higher than baseline scores in both groups (P<.001), regardless of risk status (Table 2 and Table 3). Women in the computer group correctly answered significantly more knowledge questions than those in the counselor group for 12 of the 20 items (Table 4). Among low-risk women, the mean increase in knowledge scores was significantly higher in the computer group compared with the counselor group (38 vs 29; P=.03). However the increase was not significantly different between groups among high-risk women (34 vs 29; P=.22). Changes in knowledge scores were not affected by self-reported computer literacy but they were affected by educational level. Specifically, women with higher educational levels had smaller changes in their knowledge scores because they started out with higher baseline scores and therefore had less room for improvement. However, since the effect of education was identical in both groups, the overall group comparison was not confounded.
Table 2.
Measures of Knowledge, Risk Perception, Intent to Test, and Anxiety for Women at Low Risk of Carrying a BRCA1/2 Mutation*
|
Counselor Group (n = 61) |
Computer Group (n = 56) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measures† | Before Counseling | After Counseling | Change | PValue‡ | Before Computer Use | After Computer Use | Change | PValue§ | After Computer Use and Counseling | PValue|| | PValue, Counselor vs Computer Group¶ |
| Knowledge, % correct responses | 50 | 80 | 29 | <.001 | 53 | 91 | 38 | <.001 | . . .# | . . .# | .03 |
| Relative risk perception, % | 90 | 78 | −12 | .05 | 82 | 83 | 1 | >.99 | 83 | >.99 | .18 |
| Absolute risk perception, mean (range) | 58 (0–100) | 42 (0–100) | −16 | <.001 | 59 (10–100) | 51 (10–90) | −8 | .001 | 42 (10–90) | <.001 | .02 |
| Genetic risk perception, % | 46 | 7 | −39 | <.001 | 41 | 34 | −7 | .16 | 11 | <.001 | .002 |
| Intent to test, % | 80 | 36 | −44 | <.001 | 82 | 67 | −15 | .05 | 42 | <.001 | .07 |
| State anxiety, mean (range) | 34 (20–72) | 30 (20–61) | −3 | .007 | 33 (20–52) | 33 (20–48) | 0 | .90 | 29 (20–47) | <.001 | .04 |
Low risk was defined as less than 10% chance of carrying a mutation.
Data for the measures are based on the following: relative risk perception: % indicating “much higher” or “a little higher” for the item, “Compared with other women your age, what are your chances of developing breast cancer in the future?”; absolute risk perception: mean response values (range) for the item, “What do you think your chances of getting breast cancer are on a scale from 0 to 100?”; genetic risk perception: % indicating “very likely” or “definitely” for the item, “In your opinion, how likely is it that you have an inherited gene mutation for breast cancer susceptibility?”; intent to test: % indicating “probably” or “definitely” will get tested for the item, “Present thoughts about having genetic testing for suceptibility to breast cancer”; and state anxiety: mean scores (range) on a scale from 20 to 80.
P values are for difference in outcomes between baseline and after counseling among counselor group.
P values are for difference in outcomes between baseline and after computer among computer group.
P values are for difference in outcomes between baseline and after counseling among computer group.
P values are for difference in change scores between counselor group and computer group.
Ellipses indicate data not applicable.
Table 3.
Measures of Knowledge, Risk Perception, Intent to Test and Anxiety for Women at High Risk for Carrying a BRCA1/2 Mutation*
|
Counselor Group (n = 44) |
Computer Group (n = 50) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measures† | Before Counseling | After Counseling | Change | PValue‡ | Before Computer Use | After Computer Use | Change | PValue§ | After Computer Use and Counseling | PValue|| | PValue, Counselor vs Computer Group¶ |
| Knowledge, % correct responses | 58 | 86 | 29 | <.001 | 56 | 90 | 34 | <.001 | . . .# | . . .# | .22 |
| Relative risk perception, % | 83 | 86 | 3 | .65 | 85 | 84 | −1 | >.99 | 86 | .74 | .70 |
| Absolute risk perception, mean (range) | 62 (0–100) | 54 (10–90) | −8 | .002 | 67 (10–100) | 59 (10–100) | −9 | .03 | 56 (10–90) | .006 | .85 |
| Genetic risk perception, % | 68 | 56 | −12 | .17 | 67 | 58 | −9 | .10 | 61 | .48 | .80 |
| Intent to test, % | 89 | 95 | 7 | .08 | 96 | 89 | −6 | .32 | 85 | .18 | .13 |
| State anxiety, mean (range) | 38 (20–72) | 33 (20–75) | −5 | .001 | 33 (20–60) | 31 (20–52) | −2 | .08 | 30 (20–53) | .02 | .04 |
High risk was defined as 10% or higher chance of carrying a mutation.
Data for the measures are based on the following: relative risk perception: % indicating “much higher” or “a little higher” for the item, “Compared with other women your age, what are your chances of developing breast cancer in the future?”; absolute risk perception: mean response values (range) for the item, “What do you think your chances of getting breast cancer are on a scale from 0 to 100?”; genetic risk perception: % indicating “very likely” or “definitely” for the item, “In your opinion, how likely is it that you have an inherited gene mutation for breast cancer susceptibility?”; intent to test: % indicating “probably” or “definitely” will get tested for the item, “Present thoughts about having genetic testing for suceptibility to breast cancer”; and state anxiety: mean scores (range) on a scale from 20 to 80.
P values are for difference in outcomes between baseline and after counseling among counselor group.
P values are for difference in outcomes between baseline and after computer among computer group.
P values are for difference in outcomes between baseline and after counseling among computer group.
P values are for difference in change scores between counselor group and computer group.
Ellipses indicate data not available.
Table 4.
Postintervention Knowledge Scores: Percentage of Correct Responses by Group
| Question | Correct Answer | Counselor Group (n = 105) | Computer Group (n = 106) | Difference | PValue |
|---|---|---|---|---|---|
| If a woman has a BRCA1 or BRCA2 gene mutation, the chance of passing it down to her child is | 1 in 2 | 73 | 96 | 23 | <.001 |
| Having one’s ovaries removed will definitely prevent ovarian cancer | False | 59 | 80 | 21 | .001 |
| About 1 in 10 women have an altered BRCA1 or BRCA2 gene | False | 50 | 71 | 21 | .002 |
| For a woman in the general population, the chance (or risk) of getting breast cancer at some time during her life is about 12% (1 in 8) | True | 84 | 99 | 15 | <.001 |
| Most women with breast cancer have a BRCA1 or BRCA2 gene mutation | False | 80 | 93 | 13 | .005 |
| A father can pass down a BRCA1 or BRCA2 gene mutation to his daughter | True | 87 | 99 | 12 | .001 |
| All women who have an altered (defective) BRCA1 or BRCA2 gene will get breast cancer | False | 94 | 99 | 5 | .05 |
| A woman who has a sister with an altered BRCA1 gene has a 50% chance (1 in 2) of also having this altered BRCA1 gene | True | 82 | 94 | 12 | .006 |
| About one half of all cases of breast cancer in the United States are related to mutations in the BRCA1 or BRCA2 genes | False | 73 | 85 | 12 | .04 |
| A woman who has her breasts removed can still get breast cancer | True | 78 | 90 | 12 | .02 |
| The purpose of a genetic test for breast cancer susceptibility is to detect breast cancer when it is too small to be detected through other methods, such as breast examination or mammography | False | 82 | 92 | 10 | .04 |
| Genetic testing for breast cancer susceptibility involves which of the following? | None of the above | 90 | 97 | 7 | .04 |
| Prophylactic mastectomy is an operation to remove: | Healthy breast tissue without tumor | 81 | 88 | 7 | .20 |
| A woman who does NOT have a BRCA1 or BRCA2 gene mutation can still get breast cancer | True | 96 | 99 | 3 | .17 |
| A person with a negative BRCA1 or BRCA2 test result may still have a mutation in a breast cancer susceptibility gene | True | 88 | 89 | 1 | .81 |
| A woman who does NOT have an altered BRCA1 or BRCA2 gene can still get breast or ovarian cancer | True | 98 | 99 | 1 | .56 |
| For a woman with a BRCA1 or BRCA2 gene mutation, the chance (or risk) of getting breast cancer at some time during her life is about 1% (1 in 100) | False | 73 | 74 | 0 | .97 |
| A woman who has an altered BRCA1 or BRCA2 gene has a higher risk of ovarian cancer | True | 95 | 95 | 0 | .96 |
| Compared with a woman in the general population, what is the chance (or risk) of getting breast cancer for a woman with a BRCA1 or BRCA2 gene mutation? | Higher | 96 | 92 | −4 | .25 |
| A woman who gets breast cancer at age 70 y is more likely to have an altered BRCA1 or BRCA2 gene than a woman who gets breast cancer at age 40 y | False | 88 | 83 | −5 | .26 |
Perceived Risk
Participants’ overall perception of their relative risk of developing breast cancer was high at baseline (>82% believed they had a higher risk of developing breast cancer than other women their age) and was significantly lowered after education only among low-risk women in the counselor group (Table 2). Participants’ perception of their absolute risk of developing breast cancer decreased significantly after either counseling or computer use among both high-risk and low-risk women. The reduction in risk perception was greatest among low-risk women in the counselor group (Table 2), whose mean self-estimated probability of getting breast cancer (on a scale of 0–100) dropped from 58 to 42 (P<.001). Participants’ perceived likelihood of carrying a gene mutation in BRCA1 or BRCA2 also differed by risk status (Tables 2 and 3). Among high-risk women, the percentage who indicated that they “very likely” or “definitely” had a mutation was high at baseline and did not change significantly after counseling or computer use. Among low-risk women, whose baseline risk perceptions were lower than those of high-risk women (P<.001), the percentage who indicated a higher likelihood of carrying a mutation decreased dramatically after counseling (from 46% to 7%; P<.001), and slightly (though not significantly) after computer use (from 41% to 34%; P=.16). However, after low-risk women in the computer group underwent counseling, the percentage who indicated that they likely had a mutation declined significantly (to 11%; P<.001).
Intention to Undergo Genetic Testing
At baseline, participants’ intention to undergo testing was high in both groups, with more than 80% indicating that they “probably” or “definitely” will get tested. After counseling or the computer intervention, the percentage of women indicating that they intended to get tested declined significantly among low-risk but not high-risk women (Tables 2 and 3). Among low-risk women in the counselor group, 80% indicated at baseline that they would get tested; after counseling, this declined to 36% (P<.001). The decline among low-risk women in the computer group was also significant (but less dramatic) after computer use, from 82% to 67% (P=.05). After these participants underwent counseling, their testing intention declined even further (to 42%; P<.001).
One and 6 months after participants’ study visits, we collected data about actual testing decisions. After 1 month, 21% of contacted participants (36/172) had undergone genetic testing (4% of low-risk and 39% of high-risk women). After 6 months, a cumulative total of 39% (61/156) had been tested (19% of low-risk and 62% of high-risk women). Testing decisions did not differ significantly between computer group and counselor group participants (Table 5).
Table 5.
Cumulative Number of Women Who Underwent Genetic Testing by 1 and 6 Months
|
Low Risk |
High Risk |
|||||
|---|---|---|---|---|---|---|
| Counselor Group | Computer Group | PValue, Counselor vs Computer Group | Counselor Group | Computer Group | PValue, Counselor vs Computer Group | |
| 1 mo after study visit | n = 47 | n = 42 | n = 40 | n = 43 | ||
| No. (%) who underwent testing | 3 (6.4) | 1 (2.4) | .62 | 13 (32.5) | 19 (44.2) | .27 |
| 6 mo after study visit | n = 44 | n = 39 | n = 36 | n = 37 | ||
| No. (%) who underwent testing | 9 (20.5) | 7 (17.9) | .77 | 19 (52.8) | 26 (70.3) | .12 |
Postintervention Decisional Conflict and Satisfaction With Decision
Overall mean scores on the decisional conflict measure were low in both groups and were somewhat lower in the counselor group compared with the computer group (1.9 and 2.1, respectively, on a scale of 1–5; P=.04). However, when analyzed by high and low risk status, there was no significant difference in decisional conflict between the counselor and computer groups. Additionally, overall mean scores on the satisfaction-with-decision measure were high for both groups, with mean scores of at least 23 (on a scale of 6–30). Among low-risk women, those in the counselor group had slightly higher mean satisfaction scores compared with those in the computer group (26 vs 24; P=.001), but there was no difference in satisfaction among high-risk women.
State Anxiety
On the whole, mean state anxiety scores were within normal ranges for the general population both at baseline and after either intervention. Scores for the counselor group decreased significantly after counseling among high-risk (P=.001) and low-risk (P=.007) participants. For computer group participants, anxiety did not change significantly after computer use but did decline after subsequent counseling among both high-risk and low-risk women (Tables 2 and 3).
Evaluation of the Educational Interventions
Participants rated both interventions highly. More than 83% rated counseling and computer use as “excellent” or “good” on all 9 measured attributes, and more than 95% in both groups indicated that the amount of information provided was “about right.” The overall mean evaluation score (on a scale of 1–4) was 3.7 in the counselor group and 3.5 in the computer group (P<.001). The percentage of “excellent” or “good” responses for each attribute is shown for low- and high-risk women in Table 6. There were no significant differences between groups on 6 of the 9 attributes. However, among high-risk women, more counselor group than computer group participants gave an excellent or good rating to the attribute “providing enough information for you to make a decision about genetic testing” (P=.01). Among low-risk women, more counselor group than computer group participants gave an excellent or good rating to “providing reassurance” (P=.02), but more computer group than counselor group participants gave excellent or good responses to “making good use of your time” (P=.03).
Table 6.
Participants’ Evaluation of Educational Interventions: Responses of “Excellent” or “Good”
|
Excellent or Good Rating, No. (%) |
||||
|---|---|---|---|---|
|
Low Risk |
High Risk |
|||
| Attributes | Counselor Group (n = 59) | Computer Group (n = 53) | Counselor Group (n = 43) | Computer Group (n = 50) |
| Being easy to understand | 58 (98) | 53 (100) | 43 (100) | 50 (100) |
| Providing adequate explanation | 59 (100) | 53 (100) | 42 (98) | 47 (94) |
| Enough information to decide* | 57 (97) | 46 (87) | 43 (100) | 42 (86) |
| Respecting privacy | 57 (98) | 51 (98) | 42 (98) | 49 (98) |
| Helping to understand options | 57 (97) | 52 (98) | 41 (98) | 47 (96) |
| Addressing emotional concerns | 53 (96) | 46 (90) | 42 (98) | 46 (96) |
| Learning at own pace | 58 (98) | 53 (100) | 40 (3) | 46 (94) |
| Providing reassurance† | 56 (97) | 43 (83) | 41 (95) | 45 (92) |
| Making good use of time‡ | 54 (92) | 53 (100) | 42 (98) | 44 (88) |
Counselor group had significantly more excellent or good responses than computer group in high-risk women (P = .01).
Counselor group had significantly more excellent or good responses than computer group in low-risk women (P = .02).
Computer group had significantly more excellent or good responses than counselor group in low-risk women (P = .03).
COMMENT
Increasing use of genetic testing for breast cancer susceptibility and increasing awareness of hereditary cancer risk have placed great demands on genetic counseling services.51 As more women seek information about breast cancer risk, there may be too few genetic counselors to meet their informational needs. Health care professionals (particularly those in primary care) who would ordinarily refer to genetic counselors are likely to seek alternative or adjunct methods for educating some of their patients. Interactive computer programs are such an alternative, but questions have been raised as to whether these programs can effectively educate about breast cancer risk and help women make informed decisions about genetic testing. This study sought to measure the effectiveness of a computer-based intervention, comparing its use with genetic counseling. In doing so, we also sought to determine if it can be used alone and when it should be used in conjunction with genetic counseling.
In general, the computer program was well-received by participants, who considered it to be a good use of their time and adaptable to their own learning pace. We demonstrated that the program was particularly effective at improving knowledge about hereditary breast cancer and genetic testing among women at low risk of carrying a BRCA1/2 mutation, and that this process of self-directed learning did not increase users’ anxiety. In fact, the program was more effective at increasing knowledge than was genetic counseling among low-risk women, the group who may have the least familiarity with the topic and, thus, the greatest informational needs. One possible explanation for this finding is that the computer program maximizes comprehension by presenting and repeating difficult concepts in engaging ways, using multiple formats and simple examples. It allows users to obtain information at their own pace and to review material as needed, thus promoting reflection and assimilation of complex concepts18,52–54 while averting the “information overload” that sometimes occurs during face-to-face counseling.55 Although less likely, it is also possible that the knowledge test was biased in favor of our program. However, the instrument we used was adapted from measures validated in previous studies, and all test items addressed standard topics that counselors and other genetics professionals believe necessary for informed decision making.50 An even more remote possible explanation of our finding is that our computer program was more “knowledgeable” than the counselors. Several things make this highly unlikely: all counselors had specialized training in cancer genetics, all were well-versed in the factual material, all were rated highly by the clients, and the content for the computer program was itself modeled after accepted standard content for a genetic counseling session. Further research could help clarify these issues.
The computer program was also effective in reducing low-risk women’s perceived risk of getting breast cancer and their intention to undergo genetic testing (although these outcomes were affected more after counseling). As in other studies,56–58 most women in our study initially estimated their breast cancer risks to be quite high, a misperception that can lead to increased concerns about one’s cancer risk as well as inappropriate or unnecessary genetic testing.
Although we have demonstrated the effectiveness of the computer program as an educational method, it is important to note that one-on-one genetic counseling was superior in affecting risk perception and anxiety. This is not surprising since the computer program does not provide individualized risk assessments or psychological counseling. Although a computer could be designed to give risk estimates, presenting that information without the guidance of a trained health care professional can give rise to misunderstandings and confusion due to the complexity and limitations of risk models. The program also does not address emotional issues as thoroughly as or with any of the accompanying psychological support of individualized counseling, both of which may be needed by those considering genetic testing.34,35,59,60
Counseling also increased knowledge, but not as much as the computer for low-risk individuals. However, for this group, counseling was perceived to be better than the computer at providing reassurance. Yet, high-risk women rated the counselors as better at providing them with sufficient information to make a decision. This may be because many women at high risk access information about breast cancer risk before their visit and may have sought counseling specifically to obtain personal risk assessments and guidance about testing from a genetics professional.
What is the appropriate niche for the computer program? For the majority of women who are at low risk of carrying BRCA1/2 mutations, the computer program is likely to be an effective way to improve knowledge and address most questions about hereditary cancer risk and genetic testing. The program may be particularly useful in primary care settings, where many women may have questions about their inherited cancer risk and the need for genetic testing but don’t have immediate access to genetic counseling services. Given the growing demand for education and testing in primary care61 and the limited knowledge of genetics by primary care practitioners,10,11,62 the use of our computer program by low-risk women can help reduce unnecessary referrals to genetic counselors and reserve one-on-one counseling for those who most need it, namely, high-risk women.
For women at high risk or those in need of additional psychosocial support, the computer is best used as a supplement to rather than a replacement for genetic counseling. When used in advance of counseling sessions, it can increase women’s basic knowledge of breast cancer, heredity, and genetic testing and thereby help prepare them for their meetings with counselors. With a higher knowledge base, women are more likely to comprehend the personalized risk assessments that take place in counseling sessions and to focus on the implications of pursuing genetic testing.
An additional noteworthy finding in both groups was that women’s actual uptake of genetic testing was lower than one might expect from their previously stated intentions. Greater than 80% of participants in both risk groups indicated at baseline that they were likely to undergo genetic testing. After receiving genetic counseling (with or without the computer program), the percentage of high-risk women who indicated that they were likely to undergo genetic testing did not change; however, the percentage of low-risk women who intended to have testing declined significantly, to approximately 40%. At 6 months after the intervention, 62% of high-risk women and 19% of low-risk women had undergone testing. These findings are consistent with other studies that have demonstrated that genetic testing intentions frequently differ from actual behaviors,63 especially among persons who are at lower risk of carrying a mutation. The findings also illustrate the dissuading influence that education and counseling may have on testing decisions among low-risk women, for whom genetic testing is less likely to be helpful.
The generalizability of our findings to other populations may be limited for several reasons. First, the computer program focuses only on genetic testing for breast cancer susceptibility. Other inherited cancer predisposition syndromes may have different test limitations, psychological effects, and implications for medical management. Thus, separate programs would need to be developed and evaluated for other conditions. Second, the study was conducted in 6 specialty settings offering cancer risk assessment by counselors experienced in cancer genetics. Most medical environments lack such specialty services; hence, the present findings may significantly underestimate our program’s ability to outperform various health care professionals in increasing women’s knowledge about breast cancer risks. Third, 77 individuals did not keep their counseling appointments after initially agreeing to participate in the study; these women may differ from participants who completed the study. Although it was not feasible to collect detailed information about nonparticipants, we can speculate that those who did not keep their appointments may have been less motivated or more ambivalent about obtaining information about their risks and less open to considering genetic testing. If these individuals had been in our study, we may have seen lower mean knowledge scores, perceived risk of developing breast cancer, and intention to undergo testing. Still, since randomization did not occur until after participants arrived at their study visits, any differences would likely have affected both groups equally and, hence, had no significant impact on our results.
Perhaps the most important limitation to the generalizability of our findings is that this study included only women who could read, write, and speak English, and most were white, well-educated, medically literate, and comfortable using computers. Thus, our study population is not representative of the US population at large or of women at risk of breast cancer. Nonetheless, the women included in this study do represent a typical cross section of women who seek genetic counseling for breast cancer susceptibility. Clearly, further study is needed to determine the usefulness of our computer program in more diverse populations, including minorities, those with lower educational levels, and those in primary care settings.
In conclusion, these findings support the use of an interactive computer program to educate women about breast cancer risk and genetic testing. For those at high risk of hereditary breast cancer, our computer program can effectively supplement standard genetic counseling by providing factual information before genetic counseling sessions. For women at low risk, the computer program has the potential to stand alone as an educational method when accompanied by appropriate follow-up with a qualified health care professional.
Acknowledgments
We thank the genetic counselors and study coordinators involved in this study and Norm Fost, MD, MPH, Andrew Baum, PhD, Benjamin Levi, MD, PhD, June Peters, MS, and Joanne Caulfield, MS, MEd, for their contributions to the article and to the project.
Footnotes
Financial Disclosure: Dr Green has received royalty payments from sales of the CD-ROM decision aid.
Author Contributions: Dr Green had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Green, Mauger.
Acquisition of data: Green, Peterson, Wagner-Baker, Harper, Friedman, Rubinstein.
Analysis and interpretation of data: Green, Peterson, Harper, Mauger.
Drafting of the manuscript: Green.
Critical revision of the manuscript for important intellectual content: Green, Peterson, Wagner-Baker, Harper, Friedman, Rubinstein, Mauger.
Statistical analysis: Green, Mauger.
Obtained funding: Green, Peterson, Rubinstein.
Administrative, technical, or material support: Green, Wagner-Baker, Harper, Friedman, Rubinstein.
Supervision: Green, Friedman, Rubinstein.
Funding/Support: This research was supported by grants R03CA70638 and R01CA84770 from the National Cancer Institute and the National Human Genome Research Institute, National Institutes of Health, Bethesda, Md.
Role of the Sponsor: The authors carried out the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript without the sponsor’s participation. The distributor of the program had no role in the study design or implementation.
References
- 1.Eng C, Hampel H, de la Chapelle A. Genetic testing for cancer predisposition. Annu Rev Med. 2001;52:371–400. doi: 10.1146/annurev.med.52.1.371. [DOI] [PubMed] [Google Scholar]
- 2.Collins F. Shattuck lecture—medical and societal consequences of the Human Genome Project. N Engl J Med. 1999;341:28–37. doi: 10.1056/NEJM199907013410106. [DOI] [PubMed] [Google Scholar]
- 3.Petersen GM. Genetic testing. Hematol Oncol Clin North Am. 2000;14:939–952. doi: 10.1016/s0889-8588(05)70320-8. [DOI] [PubMed] [Google Scholar]
- 4.Miki Y, Swensen J, Shattuck-Eidens D, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266:66–71. doi: 10.1126/science.7545954. [DOI] [PubMed] [Google Scholar]
- 5.Wooster R, Bignell G, Lancaster J, et al. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995;378:789–792. doi: 10.1038/378789a0. [DOI] [PubMed] [Google Scholar]
- 6.Touchette N, Holtzman NA, Davis JG, Feetham S. Toward the 21st Century: Incorporating Genetics Into Primary Health Care Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press; 1997.
- 7.Fry A, Campbell H, Gudmunsdottir H, et al. GPs’ views on their role in cancer genetics services and current practice. Fam Pract. 1999;16:468–474. doi: 10.1093/fampra/16.5.468. [DOI] [PubMed] [Google Scholar]
- 8.Friedman LC, Cooper HP, Webb JA, Weinberg AD, Plon SE. Primary care physicians’ attitudes and practices regarding cancer genetics: a comparison of 2001 with 1996 survey results. J Cancer Educ. 2003;18:91–94. doi: 10.1207/S15430154JCE1802_11. [DOI] [PubMed] [Google Scholar]
- 9.Geller G, Tambor WS, Chase GA, Hofman KJ, Faden RR, Holtzman NA. Incorporation of genetics in primary care practice—will physicians do the counseling and will they be directive? Arch Fam Med. 1993;2:1119–1125. doi: 10.1001/archfami.2.11.1119. [DOI] [PubMed] [Google Scholar]
- 10.Hofman KJ, Tambor ES, Chase GA, Geller G, Faden RR, Holtzman NA. Physicians’ knowledge of genetics and genetic tests. Acad Med. 1993;68:625–632. doi: 10.1097/00001888-199308000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Freedman AN, Wideroff L, Olson L, et al. US physicians’ attitudes toward genetic testing for cancer susceptibility. Am J Med Genet. 2003;120A:63–71. doi: 10.1002/ajmg.a.10192. [DOI] [PubMed] [Google Scholar]
- 12.Secretary’s Advisory Committee on Genetic Testing. Enhancing the Oversight of Genetic Tests: Recommendations of the SACGT. Bethesda, Md: National Institutes of Health; 2000.
- 13.American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol. 2003;21:2397–2406. doi: 10.1200/JCO.2003.03.189. [DOI] [PubMed] [Google Scholar]
- 14.Klimberg VS, Galandiuk S, Singletary ES, et al. Committee on Issues and Governmental Affairs of the Society of Surgical Oncology. Society of Surgical Oncology: statement on genetic testing for cancer susceptibility. Ann Surg Oncol. 1999;6:507–509. doi: 10.1007/s10434-999-0507-4. [DOI] [PubMed] [Google Scholar]
- 15.National Society of Genetic Counselors Familial Cancer Risk Counseling Special Interest Group Directory. Wallingford, Pa: National Society of Genetic Counselors; 2003.
- 16.Andrews LB, Fullarton JE, Holtzman NA, Motulsky AG. Assessing Genetic Risks: Implications for Health and Social Policy. Washington, DC: National Academy Press; 1994. [PubMed]
- 17.Holtzman NA, Watson MS. Promoting Safe and Effective Genetic Testing in the United States: Final Report of the Task Force on Genetic Testing Baltimore, Md: Johns Hopkins University Press; 1998. [PubMed]
- 18.Green MJ, Fost N. Who should provide genetic education prior to gene testing? computers and other methods for improving patient understanding. Genet Test. 1997;1:131–136. doi: 10.1089/gte.1997.1.131. [DOI] [PubMed] [Google Scholar]
- 19.Understanding Gene Testing. Bethesda, Md: National Cancer Institute; 1995. NIH publication 96–3905.
- 20.National Action Plan on Breast Cancer and National Cancer Institute. Genetic Testing for Breast Cancer Risk: It’s Your Choice. Washington, DC: US Dept of Health and Human Services; 1997.
- 21.FORCE: Facing Our Risk of Cancer Empowered home page. Available at: http://www.facingourrisk.org/ Accessed March 30, 2004.
- 22.National Cancer Institute and National Action Plan on Breast Cancer. Genetic testing for breast cancer risk. Available at: http://www.cancer.gov/cancertopics/genetic-testing-breast/DetailedTOC Accessed March 30, 2004.
- 23.Cull A, Miller H, Porterfield T, et al. The use of videotaped information in cancer genetic counselling: a randomized evaluation study. Br J Cancer. 1998;77:830–837. doi: 10.1038/bjc.1998.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green MJ, Fost N. An interactive computer program for educating and counseling patients about genetic susceptibility to breast cancer. J Cancer Educ. 1997;12:204–208. doi: 10.1080/08858199709528490. [DOI] [PubMed] [Google Scholar]
- 25.Baty BJ. Counseling by computer: breast cancer risk and genetic testing. Am J Med Genet. 1999;86:93–94. [Google Scholar]
- 26.Crowe JP. CD-ROM review: counseling by computer: breast cancer risk & genetic testing. J Womens Health. 1999;8:25–26. [Google Scholar]
- 27.Dabney MK, Huelsman K. Software review: counseling by computer: breast cancer risk and genetic testing. Genet Test. 2000;4:43–44. doi: 10.1089/109065700316453. [DOI] [PubMed] [Google Scholar]
- 28.McGee G. Breast cancer counseling. JAMA. 1999;281:1652. [Google Scholar]
- 29.Green MJ, McInerney AM, Biesecker BB, Fost N. Education about genetic testing for breast cancer susceptibility: patient preferences for a computer program or genetic counselor. Am J Med Genet. 2001;103:24–31. doi: 10.1002/ajmg.1501. [DOI] [PubMed] [Google Scholar]
- 30.Green MJ, Biesecker BB, McInerney AM, Mauger D, Fost N. An interactive computer program can effectively educate patients about genetic testing for breast cancer susceptibility. Am J Med Genet. 2001;103:16–23. doi: 10.1002/ajmg.1500. [DOI] [PubMed] [Google Scholar]
- 31.Berry DA, Iversen ES, Jr, Gudbjartsson DF, et al. BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2, and prevalence of other breast cancer susceptibility genes. J Clin Oncol. 2002;20:2701–2712. doi: 10.1200/JCO.2002.05.121. [DOI] [PubMed] [Google Scholar]
- 32.McGee G. Beyond Genetics: Putting the Power of DNA to Work in Your Life New York, NY: HarperCollins; 2003:96–99.
- 33.American Society of Clinical Oncology. Statement of the American Society of Clinical Oncology: genetic testing for cancer susceptibility. J Clin Oncol. 1996;14:1730–1736. doi: 10.1200/JCO.1996.14.5.1730. [DOI] [PubMed] [Google Scholar]
- 34.Croyle RT, Achilles JS, Lerman C. Psychologic aspects of cancer genetic testing: a research update for clinicians. Cancer. 1997;80:569–575. doi: 10.1002/(sici)1097-0142(19970801)80:3+<569::aid-cncr6>3.3.co;2-9. [DOI] [PubMed] [Google Scholar]
- 35.Lerman C, Croyle R. Psychological issues in genetic testing for breast cancer susceptibility. Arch Intern Med. 1994;154:609–616. [PubMed] [Google Scholar]
- 36.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 37.Wilfond BS, Rothenberg KH, Thomson EJ, Lerman C. Cancer genetic susceptibility testing: ethical and policy implications for future research and clinical practice. J Law Med Ethics. 1997;25:243–251. doi: 10.1111/j.1748-720x.1997.tb01406.x. [DOI] [PubMed] [Google Scholar]
- 38.Lerman C, Narod S, Schulman K, et al. BRCA1 testing in families with hereditary breast-ovarian cancer: a prospective study of patient decision making and outcomes. JAMA. 1996;275:1885–1892. [PubMed] [Google Scholar]
- 39.Lerman C, Biesecker BB, Benkendorf JL, et al. Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst. 1997;89:148–157. doi: 10.1093/jnci/89.2.148. [DOI] [PubMed] [Google Scholar]
- 40.Weinstein ND. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. J Behav Med. 1987;10:481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- 41.Berry DA, Parmigiani G, Sanchez J, Schildkraut J, Winer E. Probability of carrying a mutation of breast-ovarian cancer gene BRCA1 based on family history. J Natl Cancer Inst. 1997;89:227–238. doi: 10.1093/jnci/89.3.227. [DOI] [PubMed] [Google Scholar]
- 42.Parmigiani G, Berry D, Aguilar O. Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet. 1998;62:145–158. doi: 10.1086/301670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Euhus DM, Smith KC, Robinson L, et al. Pretest prediction of BRCA1 or BRCA2 mutation by risk counselors and the computer model BRCAPRO. J Natl Cancer Inst. 2002;94:844–851. doi: 10.1093/jnci/94.11.844. [DOI] [PubMed] [Google Scholar]
- 44.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 45.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: the Satisfaction With Decision Scale. Med Decis Making. 1996;16:58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 46.Spielberger CD, Sydeman SJ, Owen AE, Marsh BJ. Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI). In: Maruish ME, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates Inc; 1999:993–1021.
- 47.Spielberger C. Manual for the State-Trait Anxiety Inventory, STAI (Form Y) Palo Alto, Calif: Consulting Psychologists Press; 1983.
- 48.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136:127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 49.O’Connor AM. A call to standardize measures for judging the efficacy of interventions to aid patients’ decision making. Med Decis Making. 1999;19:504–505. doi: 10.1177/0272989X9901900420. [DOI] [PubMed] [Google Scholar]
- 50.Geller G, Botkin JR, Green MJ, et al. Genetic testing for susceptibility to adult-onset cancer: the process and content of informed consent. JAMA. 1997;277:1467–1474. [PubMed] [Google Scholar]
- 51.Cooksey JA. The Genetic Counselor Workforce. Chicago, Ill: Illinois Center for Health Workforce Studies; February 2000.
- 52.Green MJ. Computers and genetic counseling—time for a dialogue? J Genet Couns. 2000;9:359–361. doi: 10.1023/A:1009462314724. [DOI] [PubMed] [Google Scholar]
- 53.Kahn G. Computer-based patient education: a progress report. MD Comput. 1993;10:93–99. [PubMed] [Google Scholar]
- 54.Strecher VJ, Greenwood T, Wang C, Dumont D. Interactive multimedia and risk communication. J Natl Cancer Inst Monogr. 1999;25:134–139. doi: 10.1093/oxfordjournals.jncimonographs.a024188. [DOI] [PubMed] [Google Scholar]
- 55.Elias S, Annas GJ. Generic consent for genetic screening. N Engl J Med. 1994;330:1611–1613. doi: 10.1056/NEJM199406023302213. [DOI] [PubMed] [Google Scholar]
- 56.Evans DG, Burnell LD, Hopwood P, Howell A. Perception of risk in women with a family history of breast cancer. Br J Cancer. 1993;67:612–614. doi: 10.1038/bjc.1993.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hopwood P, Shenton A, Lalloo F, Evans DG, Howell A. Risk perception and cancer worry: an exploratory study of the impact of genetic risk counselling in women with a family history of breast cancer. J Med Genet. 2001;38:139. doi: 10.1136/jmg.38.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hopwood P. Breast cancer risk perception: what do we know and understand? Breast Cancer Res. 2000;2:387–391. doi: 10.1186/bcr83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bleiker EM, Hahn DE, Aaronson NK. Psychosocial issues in cancer genetics—current status and future directions. Acta Oncol. 2003;42:276–286. doi: 10.1080/02841860310004391. [DOI] [PubMed] [Google Scholar]
- 60.Schwartz MD, Peshkin BN, Hughes C, Main D, Isaacs C, Lerman C. Impact of BRCA1/BRCA2 mutation testing on psychologic distress in a clinic-based sample. J Clin Oncol. 2002;20:514–520. doi: 10.1200/JCO.2002.20.2.514. [DOI] [PubMed] [Google Scholar]
- 61.Armstrong K, Weber B, Ubel PA, Guerra C, Schwartz JS. Interest in BRCA1/2 testing in a primary care population. Prev Med. 2002;34:590–595. doi: 10.1006/pmed.2002.1022. [DOI] [PubMed] [Google Scholar]
- 62.Escher M, Sappino AP. Primary care physicians’ knowledge and attitudes towards genetic testing for breast-ovarian cancer predisposition. Ann Oncol. 2000;11:1131–1135. doi: 10.1023/a:1008319114278. [DOI] [PubMed] [Google Scholar]
- 63.Lerman C, Croyle RT, Tercyak KP, Hamann H. Genetic testing: psychological aspects and implications. J Consult Clin Psychol. 2002;70:784–797. doi: 10.1037//0022-006x.70.3.784. [DOI] [PubMed] [Google Scholar]


