Abstract
This study examined the utility of cognitive and behavioral constructs (AIDS information, motivation, and behavioral skills) in explaining sexual risk taking among 172 12–20–year-old ethnically diverse urban youths in outpatient psychiatric care. Structural equation modeling revealed only moderate support for the model, explaining low to moderate levels of variance in global sexual risk taking. The amount of explained variance improved when age was included as a predictor in the model. Findings shed light on the contribution of AIDS information, motivation, and behavioral skills to risky sexual behavior among teens receiving outpatient psychiatric care. Results suggest that cognitive and behavioral factors alone may not explain sexual risk taking among teens whose cognitive and emotional deficits (e.g., impaired judgment, poor reality testing, affect dysregulation) interfere with HIV preventive behavior. The most powerful explanatory model will likely include a combination of cognitive, behavioral, developmental, social (e.g., family), and personal (e.g., psychopathology) risk mechanisms.
HIV continues to spread among young people despite a decreased incidence of AIDS cases nationwide. HIV infection doubles every 14 months in adolescents, and teenagers account for 25% of new sexually transmitted diseases (STDs) reported annually (Centers for Disease Control and Prevention, 2000). Teens are most likely to acquire HIV through risky sexual behavior (e.g., sex without a condom), but risk is not uniform across youths. Adolescents receiving mental health services are especially vulnerable to HIV because they engage in the same risk behaviors as their school–aged peers but at higher rates (Brown, Danovsky, Lourie, DiClemente, & Ponton, 1997; Donenberg, Emerson, Bryant, Wilson, & Weber–Shifrin, 2001). In a recent study, teens in psychiatric care reported high rates of unprotected sexual intercourse (55%), sex while using drugs/alcohol (49%), sex with a high–risk partner (43%), and being currently sexually active (45%) (Donenberg et al., 2001). Cognitive deficits associated with mental health problems, such as impaired decision making, poor judgment, impulsivity, and inaccurate assessment of risk exacerbate the health risks for these youths, but their unique risk mechanisms are not well understood. The current study tested a cognitive–behavioral model of HIV risk among youths in psychiatric care based on the constructs of the information–motivation–behavioral skills (IMB) model (Fisher & Fisher, 1992).
THE INFORMATION–MOTIVATION–BEHAVIORAL SKILLS (IMB) MODEL
Most theories of health behavior implicate cognitive determinants of HIV risk and prevention, such as AIDS knowledge, personal attitudes, and behavioral intentions to practice prevention (Ajzen & Fishbein, 1980). Among these theories, the IMB model (Fisher & Fisher, 1992) stands out as an integrative framework to explain AIDS risk reduction. The IMB model posits two cognitive and one behavioral factor as determinants of AIDS prevention behavior: (a) information, or knowledge about transmission and prevention; (b) motivation to reduce risk, or personal attitudes about preventive behavior, perceived normative support for HIV prevention, and behavioral intentions; and (c) behavioral skills to practice prevention, including perceived self–efficacy and the ability to negotiate AIDS prevention with a partner. Perceptions of HIV prevention self–efficacy have been used as an indicator of behavioral skills in a number of studies testing the IMB model, including those involving adolescents (Fisher, Fisher, Bryan, & Misovich, 2002; Fisher, Williams, Fisher, & Molloy, 1999).
The IMB model is innovative in its suggested linkages among these key constructs. Information and motivation are unrelated to each other (e.g., a teenager may know how to protect herself from HIV but feel little motivation to do so, or a highly motivated adolescent may not be well informed), but both influence risk reduction behavior directly and indirectly through behavioral skills. Behavioral skills directly influence preventive behavior, and information and motivation influence and function through behavioral skills (Fisher & Fisher, 1992). The strength of the relationships of information, motivation, behavioral skills, and behavior, and the specific causal paths, vary as a function of the status of the study population (e.g., age, mental health) and the specific HIV preventive behavior at focus. Variations reflect the dynamic causes of HIV preventive behavior among different groups and behaviors of interest. Identifying patterns of causal links for different populations is essential to developing tailored interventions that fit the needs of particular groups.
There is empirical support for the model among adults, gay men, and nonclinical samples of youths when AIDS prevention behavior is the outcome variable (e.g., safer sex discussions, condom use, getting an HIV test) (Fisher & Fisher, 1992). Fisher and Fisher (1995) found that motivation to prevent AIDS was associated with behavioral skills and prevention behavior among teens. The model has explained 46–75% of the variance in risk reduction behavior among adolescents (Fisher & Fisher, 2000; Fisher et al., 1999). By contrast, the IMB model explained only 10% of the variance among young adults (Fisher & Fisher, 2000). Boyer et al. (2000) tested cognitive and behavioral constructs in relation to STD risk behavior (i.e., actions that increase risk of STD exposure), but they did not test the IMB structural model. HIV/STD information, motivation, and behavioral skills together explained 22% of the variance in engagement in STD risk behavior among sexually active urban youths. Consistent with Boyer et al. (2000), the current study examined cognitive and behavioral mechanisms associated with sexual risk taking behavior (as opposed to HIV preventive behavior studied by Fisher and colleagues), but we applied these constructs to youths with mental health problems.
Most tests of the IMB constructs have not examined the effects of age, despite widespread evidence that age, a proxy for development, influences adolescents’ cognitive, emotional, social, and sexual behavior. Older youths are more likely to be sexually active and less likely to use condoms than younger teens (Kotchick, Shaffer, Miller, & Forehand, 2001), yet there has been no systematic comparison of different statistical treatments of age in testing IMB model constructs. The present study examined the role of age in three ways (ignoring age, controlling age, and including age as a predictor) because of the wide age range among participants. We expected age to explain a significant portion of the variance, potentially underscoring the need to consider age in testing key cognitive and behavioral risk mechanisms.
Ample evidence suggests that gender plays an important role in sexual risk taking. For example, Donenberg, Wilson, Emerson, and Bryant (2002) found that girls in psychiatric care reported less consistent condom use than boys. Previous research also documents important sex differences associated with cognitive and behavioral risk determinants (Donenberg et al., 2002; Kotchick et al., 2001). Fisher et al. (1999) found that the IMB pathways were different for boys and girls. For girls, the path from information to behavioral skills was significant, but for boys the path from motivation to safer sex was significant. The current study tested the fit of the model separately for boys and girls in psychiatric care, but the absence of previous research warranted no specific predictions.
Few studies capture the complexity of teen sexual risk taking. Risky sexual behavior has been alternatively defined by specific indicators (e.g., number of partners, condom use, sexual debut) (Blum et al., 2000; Smith, 1997), composite scores (Boyer et al., 2000; Donenberg et al., 2001), or both (Doljanac & Zimmerman, 1998; Pinkerton et al., 1998). We assessed adolescent self–reported global risky sexual behavior, a composite score consisting of four high–risk behaviors that have been linked to HIV risk in previous research: multiple partners (Fisher et al., 1999; Kalichman et al., 2002), sex while using drugs and alcohol (Devieux et al., 2002), sex with someone whose history is not well known and therefore could be a high–risk partner (Eiser & Ford, 1995; Metzler, Noell, Biglan, Ary, & Smolkowski, 1994; Rickman, Lodico, DiClemente, & Morris, 1994), and sex without a condom (Fisher et al., 1999; Kalichman et al., 2002).
APPLYING THE IMB MODEL TO YOUTHS RECEIVING PSYCHIATRIC TREATMENT
Different factors likely influence HIV–risk behavior for unique subgroups of teens. Few studies have tested the structural components or pathways of the IMB constructs with adolescents, and none have evaluated the utility of these mechanisms for teens in psychiatric care. Compared with their peers, youths receiving mental health services have greater cognitive deficits (e.g., poor reality testing, impaired judgment), more negative attitudes about prevention (Brown, Danovsky, et al., 1997), and low perceived vulnerability to HIV (Katz, Mills, Singh, & Best, 1995). Mental health problems introduce unique barriers to behavior change that further reduce motivation to prevent AIDS, such as low self–esteem and a negative view of the future (Carey, Carey, & Kalichman, 1997). Less is known about the influence of peer norms on youths in psychiatric care because their social networks are more complicated and less intimate than those of their peers (McFarlane, Bellisimo, & Norman, 1995). Adolescents with mental health problems lack essential interpersonal and social skills to negotiate safe sex, including assertiveness and effective communication (Brown, Danovsky, et al., 1997). Low perceived self–efficacy is related to risky behavior among teens in psychiatric care, and these youths report an inability to refuse sex without a condom (Brown, Reynolds, & Lourie, 1997).
This study tested the central cognitive and behavioral constructs of the IMB model with teens in mental health care. Using structural equation modeling procedures, we examined the linkages proposed in the IMB model for teens’ risky sexual behavior. Consistent with previous research, we expected the strongest relationships to occur between motivation and risky sex, motivation and behavioral skills, and behavioral skills and risky sex. We hypothesized that low motivation would be related to low perceived behavioral skills and more risky sex. We expected a nonsignificant relationship between information and risky sex or behavioral skills directly, but we hypothesized that low behavioral skills would predict greater risk taking. Understanding the role of cognitive and behavioral factors in sexual risk behavior for these teens will yield new insight into the specific and potentially unique causal mechanisms of risky sexual behavior among youths in psychiatric care and offer guidelines for developing specially tailored interventions to reduce HIV risk this vulnerable population.
METHOD
OVERVIEW OF PROCEDURES
This study grows out of a larger longitudinal project of HIV risk behavior among youths in psychiatric care. Youths and caregivers (hereafter referred to as “parents”) were recruited from three hospitals in Chicago. Families were reassured that their participation would have no impact on their medical or psychiatric care. At two clinics, a staff member called eligible families to inform them of the study and invite them to participate. At the third clinic, data were collected as part of the hospital’s routine intake procedure, and research staff asked youths and parents for permission to use the data for research. Sixty percent of the families contacted agreed to participate (N = 227/380), but consent rates differed for the third clinic where data were collected as part of the intake procedure (159/192, or 83%) versus the two clinics where a staff member invited eligible families to participate (68/188, or 36%). We examined site differences among model variables in the preliminary analyses (see below). Consenters and refusers did not differ significantly by child gender (p = .676) or by child age (p = .082). Because of restrictions in access to private health information beyond child age and gender among non–participants, we were unable examine ethnic differences. Parents and youths separately completed self–report measures and interviews. They were compensated for their participation, and each received an informational pamphlet about AIDS transmission and prevention. Total testing time was approximately 3 hours. The current study analyzed youths’ reports of HIV/AIDS knowledge, attitudes, beliefs, and behavioral skills and their associations with teens’ high–risk sexual behavior.
PARTICIPANTS
Participants (N = 172) are a subset of the larger sample for whom complete data were available. Participants included in this sample and participants with incomplete data did not differ significantly by age, gender, or ethnicity. Moreover, there were no differences between samples for the IMB–related constructs and risk behavior outcomes, except for AIDS behavioral skills (p = .043; excluded participants had lower self–efficacy to practice prevention). Youths ranged in age from 12 to 20 years (M = 15.29; SD = 1.87), and 44.8% were female. Teens were ethnically diverse (45.3% African/African American, 34.9% Caucasian, 10.5% Latino, 7.0% biracial, 2.3% Asian) and 47.6% scored in the first three levels of the Hollingshead (1975) index, indicating that slightly less than half of the subjects were from low to middle income families. Youths were excluded from the study if they (a) were mentally retarded or had known organic impairment that might limit their ability to understand the questions or the assent process (n = 40), (b) were wards of the Department of Child and Family Services because their institutional review board denied approval for the study (n = 47), (c) did not speak English (measures are normed for English speakers) (n = 20), and (d) did not live with a guardian or caretaker (n = 5).
Teens qualified for a range of psychiatric disorders based on the Computerized Diagnostic Interview Schedule for Children 4.0 (CDISC; Shaffer, Fisher, Piacentini, Schwab–Stone, & Wiks, 1991). Diagnoses are based on a smaller sample because 36 adolescents (20.9%) and 42 caregivers (24.4%) did not complete the CDISC. Of the teens who completed at least one section of the interview, 20% qualified for a mood disorder, 23% met criteria for an anxiety disorder, 12% qualified for conduct disorder, and 37% met criteria for at least one disorder. According to parents who completed at least one section of the CDISC, 22% of youths qualified for a mood disorder, 26% met criteria for an anxiety disorder, 41% qualified for a disruptive behavior disorder, and 62% met criteria for at least one disorder. The relatively low association between parent and youth reports of child psychopathology are consistent with previous reports (Achenbach, McConaughy, & Howell, 1987).
MEASURES
Family Demographics
Parents provided information about the adolescent’s age, gender, and ethnicity, and the family’s socioeconomic status (Hollingshead, 1975).
Information
AIDS knowledge was assessed using a 37–item true–false self–report instrument that combines and modifies previously published measures of transmission routes, misconceptions about transmission, and risk reduction strategies (Brown, DiClemente, & Beausoleil, 1992). The original measure was modified to be developmentally and linguistically appropriate for use with adolescents (Brown et al., 1992). We computed two scales: knowledge about prevention consisting of 10 items (e.g., “Condoms reduce the risk of getting the AIDS virus”), and knowledge about transmission consisting of 20 items. Items were scored as 0 (incorrect) or 1 (correct). Scale reliabilities for all measures are reported below.
Motivation
AIDS attitudes and beliefs were assessed using a 38–item self–report measure based on IMB model constructs (Fisher & Fisher, 1992) and social cognitive theory (Bandura, 1994). Items were developed for use with pre–adolescents and adolescents. We computed four scores: (a) perceived threat of acquiring AIDS, (b) personal attitudes about AIDS, (c) peer norms for AIDS prevention, and (d) intentions to prevent AIDS. Tests of the measurement model revealed that only the latter two subscales, peer norms and intentions to prevent AIDS, were sufficiently correlated to function as indicators of the latent variable so they were retained for future analyses. Although this narrowed the breadth of the motivation construct, it enhanced scale reliability. Peer norms and prevention intentions have been widely used as indicators of motivation in tests of the IMB model (Fisher et al., 1999; Fisher et al., 2002). Peer norms consisted of six items scored on a scale from 1 (Very untrue) to 5 (Very true), with higher scores indicating stronger peer support for HIV prevention. Scores ranged from 6 to 30. A sample item is “Friends whom I respect think I should use condoms every time, if I have sex, during the next 2 months.” Intentions to prevent AIDS consisted of three items scored on the same 5–point scale described above with higher scores indicating stronger intentions to have safe sex. Scores ranged from 3 to 15. A sample item is “If I have sex during the next 2 months, I’m planning to use condoms every time.”
Behavioral Skills
AIDS behavioral skills (S. J. Misovich, personal communication, October 24, 1998) measured perceptions of self–efficacy to prevent HIV transmission (assertive, performance, and refusal self–efficacy) and negotiate AIDS prevention with a partner. Questions were modified for use with adolescents. The scale consisted of 7 items with a total score ranging from 7 to 35. Response choices ranged from 1 (very hard to do) to 5 (very easy to do) with low scores indicating less self–efficacy to practice prevention. A sample item is “If you have sex, how hard or easy would it be for you to make sure you and your partner use a condom every time?” We divided the total scale into two separate item “parcels” (the four odd–numbered items summed into one parcel, the three even–numbered items into a second parcel) to serve as indicators of the behavioral skills latent variable.
HIV–Risk Behavior
The AIDS Risk Behavior Assessment (ARBA; Donenberg et al., 2001) is a self–administered computerized interview designed specifically for use with adolescents to assess their sexual behavior, drug/alcohol use, and needle use associated with HIV infection. The ARBA is derived from five well–established measures of sexual behavior and drug/alcohol use (Dowling, Johnson, & Fisher, 1994; Institute for Behavioral Science, 1991; National Institute of Drug Abuse, 1995; Needle et al., 1995; Watters, 1994; Weatherby, Needle, & Cesari, 1994) and assesses sexual behavior in the past 30 days and the past 3 months. The ARBA uses a skip structure so that more detailed items do not follow initial screening questions answered in the negative. Youths self–administered the ARBA using a voice directed computer (n = 84) or they used a portable cassette tape player and recorded their responses on a questionnaire (n = 88). In both cases, an interviewer remained in the room to answer questions and to ensure item comprehension. Controlling for age, the rates of risk behavior for the two outcome variables were not statistically different across the two methods of interview administration. Sexually inactive adolescents were given scores of 0 on the measures of risky sexual behaviors, to indicate the absence of risk for these participants. This approach allowed us to include all participants—whether sexually active or not—in all of our analyses. Including sexually active and nonsexually active teens in the analyses is consistent with previous research (Donenberg et al., 2001; Donenberg et al., 2002).
We created a composite score of the sum of four high–risk behaviors that have been examined in previous research, including (a) number of sexual partners in the past 3 months; (b) whether one (1) or no (0) teens ever had sex while using drugs/alcohol; (c) whether one (1) or no (0) adolescents ever had sex with a high–risk partner (i.e., whose sexual history was unknown); (d) whether one (1) or no (0) youths ever had sex without a condom. To avoid weighting the first of these indicators more strongly than the others, we standardized each of the four separate measures before summing them.
RELIABILITY ANALYSIS OF LATENT VARIABLE COMPOSITE MEASURES
We formed dual indicators by computing separate percentages of correct transmission knowledge and prevention knowledge (αs = .53 and .40, respectively). When combined into a single, unit–weighted average score, the two knowledge indicators provided an acceptably reliable summary measure of Information (α = .74). The average score on the combined information scales was 79% correct (SD = 16%). Motivation was comprised of two measured indicators: (a) perceptions of peer norms about abstaining from sex and using condoms (α = .82) and (b) behavioral intentions to reduce risk behavior (α = .71). The mean score of peer norms was 23.41 (SD = 5.33; range = 6–30), and the mean score of behavioral intentions was 12.66 (SD = 2.79; range = 3–15). When combined into a single, unit–weighted average score, the two composite indicators provided a reasonably reliable measure of motivation (α = .77). For behavioral skills, we constructed two item parcels (odd- versus even–numbered items) representing perceived self–efficacy and negotiation with a partner (α = .63). They provided a reliable measure of behavioral skills when combined into a single, unit–weighted average score (α = .80). The mean score on the overall measure of behavioral skills was 26.50 (SD = 4.99; range = 7–35).
Consistent with earlier research, we used four measures of sexual risk taking (see above) as indicators of risky sex (α for standardized components = .75). We minimized the number of measured variables in the structural model by parceling standardized versions of the four measures into two composite indicators (number of partners plus sex with a high–risk partner; sex without a condom plus sex while using drugs or alcohol), which when combined provided a reliable summary measure of risky sex (α = .79). Table 1 presents the means, standard deviations, and correlations among the variables.
TABLE 1.
Means, Standard Deviations, and Intercorrelations Between Subscales
| Subscales | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Adolescents (n = 172) | ||||||||||
| 1. AIDS prevention knowledge | .60 | −.16 | −.03 | −.25 | .18 | .08 | .31 | .41 | .54 | |
| 2. AIDS transmission knowledge | −.09 | −.01 | −.13 | .14 | .04 | .17 | .29 | .43 | ||
| 3. Peer norms about AIDS prevention | .70 | .59 | .20 | .23 | −.19 | −.27 | −.33 | |||
| 4. Intentions to prevent AIDS parcel 1 | .39 | .37 | .31 | −.12 | −.19 | −.08 | ||||
| 5. Intentions to prevent AIDS parcel 2 | .11 | .11 | −.30 | −.41 | −.40 | |||||
| 6. Behavioral skills parcel 1 | .68 | −.08 | −.09 | .10 | ||||||
| 7. Behavioral skills parcel 2 | −.04 | −.06 | −.01 | |||||||
| 8. Risky sexual behavior parcel 1 | .66 | .34 | ||||||||
| 9. Risky sexual behavior parcel 2 | .47 | |||||||||
| 10. Age | ||||||||||
| Mean | 0.58 | 0.79 | 23.41 | 9.02 | 3.64 | 15.53 | 10.97 | 0.00 | 0.00 | 15.29 |
| SD | 0.21 | 0.16 | 5.33 | 1.89 | 1.44 | 3.01 | 2.42 | 1.67 | 1.80 | 1.89 |
Note. Tabled are Pearson correlation coefficients. |rs| ≥ .13 are statistically significant at p <.05, one–tailed. |rs| ≥ .15 are statistically significant at p <.05, two–tailed.
OVERVIEW OF ANALYSES
Data analyses unfolded in two stages. In Stage 1, we tested the goodness–of–fit of the four–factor structure presumed to underlie the set of measured variables in the model. Following a two–step approach to model testing (Anderson & Gerbing, 1988), we evaluated the model in the form of a correlated–factors measurement model and then as a latent–variable path model. Next, we tested hypotheses about the structural coefficients in the model. We also compared three approaches to handling the effects of age when testing the latent variable model (see above). In Stage 2, we explored the role of gender as a moderator of the structural coefficients in the model. Given the focused nature of our predictions, we used one–tailed tests to increase power and precision and limit Type I error. Following standard practice, we report one–tailed p values when observed effects are in the predicted direction, but we report two–tailed p values when observed effects are opposite to the predicted direction.
RESULTS
PRELIMINARY ANALYSES
We examined potential site differences among participants and found that youths were significantly older at one site (n = 108, M = 15.96, SD = 1.68) than the other two sites (n = 42, M = 14.48, SD = 1.83 and n = 22, M = 13.56, SD = 1.16), which also differed significantly from each other. After controlling for age, there were no other significant site differences among the independent or dependent variables. Age was considered in all further analyses. We also examined potential ethnic differences among model constructs. There was a main effect for adolescent knowledge about HIV transmission, F(4,167) = 4.47, p < .05. Conservative post–hoc comparisons (Scheffe and Tukey) indicated that Caucasians were significantly more knowledgeable about HIV transmission than African Americans.
Consistent with earlier reports (Brown, Danovsky, et al., 1997; Donenberg, Bryant, Emerson, Wilson, & Pasch, 2003), teens reported high rates of sexual behavior; 40% reported ever having vaginal, anal, and/or oral sex. Youths reported a range from 0 to 5 sexual partners in the past 3 months (M = .48; SD = .90). Among sexually active teens (n = 68), 41% reported sex with a high–risk partner, 51% reported sex while using drugs/alcohol, and 66% reported sex without a condom. Sixty (39%) teens reported vaginal and/or anal sex, and among them, 46% reported sex with a high–risk partner, and 62% had sex without a condom.
STAGE 1: TESTING THE MODEL
We evaluated the goodness–of–fit of the intended structural model when specified as a measurement model consisting of four correlated latent variables. We assessed absolute model fit using the root mean square error of approximation (RMSEA; Steiger, 1990) and the goodness–of–fit index (GFI; Joreskog & Sorbom, 1996). We used two measures to assess relative model fit, the comparative fit index (CFI; Bentler, 1990), and the Tucker–Lewis coefficient (TLC; Tucker & Lewis, 1973). These fit indices are relatively robust with respect to sample size, distributional violations, and model misspecification (Hu & Bentler, 1998). Mardia (1970) statistics revealed significant departures from univariate normality for seven of the nine measures, with significant multivariate skewness and kurtosis. Accordingly, we used maximum–likelihood estimation to compute the Satorra–Bentler scaled chi–square (Satorra & Bentler, 1994) to adjust goodness–of–fit statistics for inflation due to nonnormality (Kline, 1998). This is the most common approach to handling nonnormality in structural equation modeling (West, Finch, & Curran, 1995).
The intended four–factor model for risky sexual behavior initially produced an inadmissible solution due to a negative unique variance (i.e., “Heywood case”) for the measured variable of “behavioral intentions.” Consistent with Wothke (1993), we eliminated the Heywood case by including an additional measured variable in the model; we split “behavioral intentions” into two indicators: (a) the mean of two items assessing plans to use condoms (α = .87) and (b) a single continuous–scale item assessing intentions to abstain from sex during the next 2 months. The respecified four–factor model produced an admissible solution that provided an acceptable fit to the data for the nine measured variables, χ2(21, n = 172) = 39.80, RMSEA = .072, GFI = .95, CFI = .96, TLC = .94. All factor loadings and factor correlations were significantly different from zero. Table 2 reports the goodness–of–fit statistics for the latent variable models.
TABLE 2.
Goodness–of–Fit Statistics for Latent Variable Path Model Predicting Risky Sexual Behavior (n = 172)
|
Measures of Absolute Fit |
Measures of Relative Fit |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | Treatment of Age in the Analysis | Number of Variablesa | χ2 | df | RMSEA | GFI | CFI | TLC | R2 |
| Risky sex | Ignore age | 9 | 39.80 | 21 | .072 | .95 | .96 | .93 | .30 |
| Residualize for age | 9 | 34.95 | 21 | .062 | .95 | .96 | .94 | .10 | |
| Include age | 10 | 51.10 | 27 | .072 | .94 | .95 | .92 | .35 | |
Note. RMSEA = root mean square error of approximation (Browne & Cudeck, 1989; Steiger, 1990). GFI = goodness–of–fit index (Joreskog & Sorbom, 1996). CFI = comparative fit index (Bentler, 1990). TLC = Tucker–Lewis coefficient (Tucker & Lewis, 1973). The four–factor model for risky sexual behavior contained 24 estimated parameters (9 loadings, 6 factor correlations, and nine unique variances). Given the total sample size of 172, the ratio of participants to estimated model parameters (7.2) was within the recommended range of 5 to 10 (Kline, 1998).
Number of variables refers to the number of measured variables in the latent variable model.
Next we evaluated the goodness–of–fit and structural coefficients of the hypothesized model considering age in three ways: First, consistent with most studies of the IMB model, we ignored the effects of age. Second, based on evidence that sexual behavior varies according to child age and our sample spans a wide age range (12–20 years), we tested the model controlling for age in two ways: (a) We partialled out the effects of age by regressing risky sex on age and saving the unstandardized residual for use as a measured variable in our structural model (Donenberg et al., 2001), and (b) we included age as a third exogenous latent variable in the model, allowing it to correlate with information and motivation, and estimating its direct effect on the outcome measure. We examined the magnitude of the direct and indirect effects in the model and the proportion of variance explained in risky sex across the three approaches to handling age.
The hypothesized model yielded the same goodness–of–fit measures as the measurement model (see Table 2). Figure 1 presents structural diagrams and standardized parameter estimates of the model when ignoring age, residualizing age, and including age as a predictor. In all three ways of treating age, four of the five hypothesized direct effects were statistically significant. The direct effects of information on behavioral skills and on risky sex and of motivation on behavioral skills were statistically significant. Contrary to our hypothesis, more knowledge was associated with elevated risk. The link between knowledge and risky sex was somewhat smaller when residualizing age (β = .22) than when ignoring age (β = .46). The direct effects of motivation and behavioral skills on risky sex varied depending on the statistical treatment of age. Motivation significantly predicted risky sex when ignoring or including age but not when age was residualized. Behavioral skills significantly predicted risky sex when controlling age (i.e., residualizing and including it as a predictor) but not when ignoring it. As in earlier research, age had a positive direct effect on risky sex, β = .26, one–tailed p <.001. The correlation between information and motivation was −.18 when ignoring age, −.17 when residualizing age, and −.18 when including age as a predictor (all two–tailed ps <.05). Age was more strongly correlated with information (φ = .62) than with motivation (φ = −.33), Δχ2(1) = 13.49, two–tailed p <.001. The indirect effects of information and motivation on risky sex were not statistically significant regardless of how age was treated in the analysis. The model explained 30%, 10%, and 35% when age was ignored, residualized, and included as a predictor, respectively.
FIGURE 1.
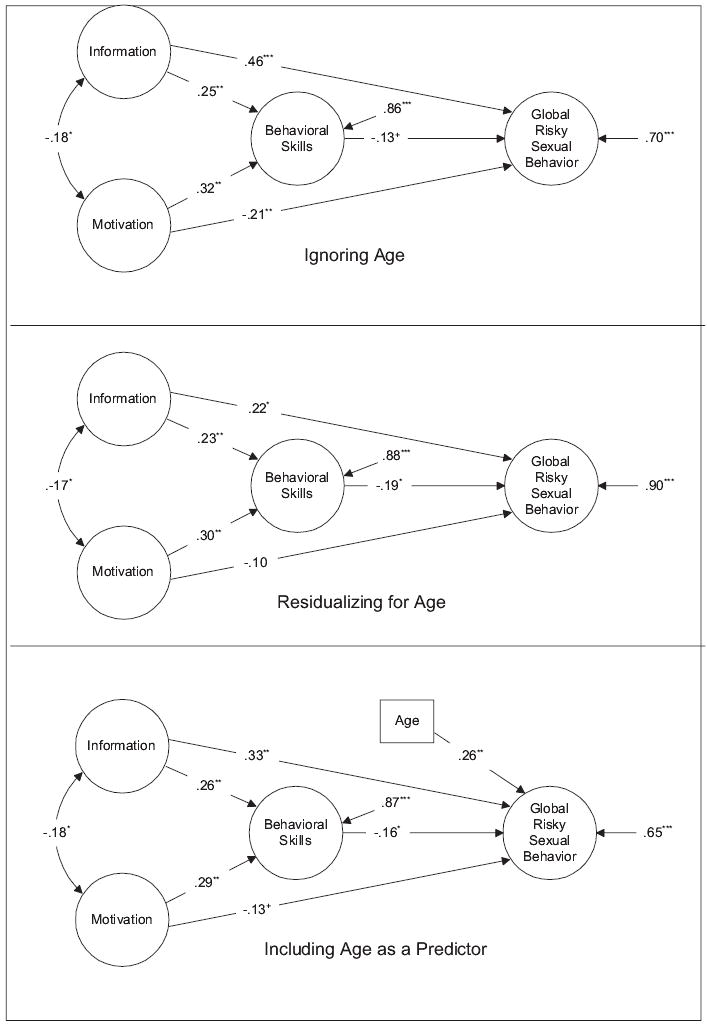
Standardized parameter estimates for the latent variable path model predicting the risky sexual behavior (a) ignoring age (top), (b) residualizing age (center), and (c) including age as a predictor (bottom).
Measured indicators, factor loadings, and item error variances have been omitted for purposes of presentation. The model that included age as an additional predictor also allowed age to correlate with both Information (φ = .62, p < .001) and Motivation (φ = −.33, p < .01). All p values are one-tailed except for that associated with the path coefficient linking information and risky sex, which is two-tailed because it is opposite to the predicted direction. +p < .10. *p < .05. **p < .01. ***p < .001.
STAGE 2: GENDER AS A MODERATOR VARIABLE
Because of sample size limitations (95 males and 77 females), we used multigroup path analysis with measured variables to investigate possible moderating effects of gender on the structural coefficients in the model (Jaccard & Wan, 1996). This minimized the number of estimated parameters to accommodate smaller sample sizes. Using summary measures to represent each latent variable in the model (Bagozzi & Edwards, 1998), we tested for gender differences in the magnitude of the five path coefficients. The path coefficients in the model were equivalent for males and females, regardless of whether we ignored age, Satorra–Bentler Δχ2s(5) < 5.63, ps >.34; residualized age, Satorra–Bentler Δχ2s(5) < 6.17, ps >.29; or included age as a predictor, Satorra–Bentler Δχ2s(5) < 5.21, ps >.40.
DISCUSSION
This is the first study to test the cognitive and behavioral constructs proposed in the IMB model among adolescent boys and girls in psychiatric care. Few studies have tried to elucidate the complex processes underlying sexual risk taking among youths with mental health problems, and this study focused on three cognitive–behavioral mechanisms that have been well documented in the literature. The model provided a reasonable fit to the data and the direct links between the key constructs were supported. Namely, AIDS information and motivation to practice prevention were consistently linked to behavioral skills, and greater behavioral skills were related to less risky sexual behavior. However, the proposed model was only moderately useful when applied to sexual risk taking in this population as underscored by the absence of mediation in all model tests and by the relatively low level of explained variance (i.e., 8–14%) after removing the effects of age on the dependent variables. Child age played a critical role in determining the amount of variance explained by the model. Findings suggest that information, motivation, and behavioral skills alone may be insufficient to understand sexual risk taking in this adolescent subgroup, and yet improving these factors can play a role in reducing risk behavior.
This study revealed unique relationships among the model constructs relative to earlier studies, and these may reflect important characteristics of a psychiatric population. For example, contrary to our hypotheses, more information was associated with greater risk behavior, and motivation was inconsistently related to sexual risk taking. Previous reports have found little relationship between information and risk behavior (DiClemente, Ponton, & Hansen, 1996; Fisher & Fisher, 2000). It is possible that high–risk teens in psychiatric care receive more information about HIV prevention by their health care providers who recognize their increased risk. Alternatively, it is possible that once adolescents engage in high–risk behavior, they seek out and retain information about HIV transmission and prevention because it is relevant to them. Nevertheless, a certain level of intellectual maturity and stability is necessary to apply the knowledge to make safe decisions and implement behavioral skills to reduce risk behavior. Although these abilities have yet to develop in many teens, they are often more delayed among youths with psychiatric impairment. These teens tend to be impulsive and lack key cognitive and behavioral skills (e.g., problem solving, self–reflection, decision making, accurately assess their own risk) to translate their knowledge into HIV preventive behavior, especially when they are emotionally aroused.
Similarly, cognitive deficits may interfere with safe decision making while distorted perceptions and poor reality testing may affect their ability to see how the information relates to them. In fact, despite high rates of self–reported sexual risk in this study, 81% of the teens reported little to no chance of contracting HIV and 49% reported little to no concern about getting HIV. The inconsistent link between teens’ sexual behavior and motivation (i.e., perceptions of peer norms and intentions to practice prevention) to reduce risk in this study exposes a limitation of using cognitive factors alone to explain HIV risk in this population. Teens with mental health problems often have poor peer relationships, and there is evidence that peer influence is lower among nontraditional youth (Rotheram–Borus, Mahler, & Rosario, 1995). Likewise, their increased impulsivity, poor problem solving, and strained interpersonal relationships likely interfere with their ability to practice safe sex despite positive intentions to do so.
The absence of mediation may also represent something unique about youths in psychiatric care. The findings suggest that behavioral skills do not influence the direct effects of information or motivation on high–risk behavior. For teens in psychiatric care, there is often a split between what they know, think and feel, and how they behave. Psychological characteristics (e.g., low self–esteem, poor affect regulation, fear of rejection, need for intimacy, poor impulse control) may play a larger role in determining risk behavior for these youths than factors like information and motivation. Hence, in addition to cognitive–behavioral mechanisms, sexual risk taking among youths in psychiatric care may be explained more fully by social and personal factors such as parental monitoring, parental permissiveness and control, parental directiveness, peer influence, and concerns about relationship intimacy (Donenberg et al., 2002; Donenberg et al., 2003). Donenberg et al. (2001) found evidence for these important factors. Increased externalizing problems predicted more risky sex but greater peer influence mediated the relationship. Models of risk behavior among teens with mental health problems need to address interpersonal negotiation skills that are necessary for HIV prevention, the social contexts in which sexual behavior takes place, and the unique social/interpersonal deficits among these adolescents. Broadening cognitive–behavioral formulations of health behavior to include relationship–based conceptualizations may enhance our understanding of risk behavior among these high–risk youths. This point is further underscored by the fact that social and interpersonal factors are also important in understanding sexual risk behavior among adolescents without mental health difficulties (Kotchick et al., 2001). Given the greater deficits among the adolescents in the current sample as compared with adolescents without mental health problems, it is possible that these factors may play an even greater role among troubled teens.
Consistent with developmental theory (Lerner & Foch, 1987), age served as a proxy for development in our study because of the rapid physical, cognitive, emotional, and behavioral changes that occur from early to late adolescence and the wide age range of the sample (12–20 years). For conceptual purposes, we examined the effects of age in three ways in the data analyses. When we included age as a predictor, the model explained the most variance in risk behavior. Removing the effects of age from risky sex dramatically reduced explained variance. Lastly, consistent with previous research ignoring age while testing the relationship between risk behavior and AIDS information (Fisher & Fisher, 1992; Fisher & Fisher, 1995; Fisher et al., 1999), motivation (Fisher & Fisher, 1992; Fisher & Fisher, 1995; Jemmott & Jemmott, 1992), and behavioral skills (Fisher & Fisher, 1992; Fisher & Fisher, 1995; Fisher et al., 1999), findings yielded moderate levels of explained variance. These findings suggest that ignoring age overestimates the strength of cognitive and behavioral variables in predicting risky sexual behavior. By contrast, controlling for age may offer greater precision in the actual variance explained by the proposed mechanisms and a determination of the independent effects of information, motivation, skills, and age. Findings underscore the relevance of this developmental period for the acquisition of information, motivation, and behavioral skills in relation to risk behavior, and highlight the importance of carefully considering developmental issues in the application of cognitive–behavioral models of HIV risk and prevention to youths.
Study limitations warrant careful consideration of the results. This is a cross–sectional investigation and longitudinal research is needed to determine the relevance of cognitive–behavioral mechanisms in explaining risk behavior among teens in psychiatric care over time. Findings are restricted to youths in outpatient mental health services and may not generalize to other populations or youths with more severe psychiatric problems. However, these teens represent a uniquely vulnerable population and research is sorely needed to identify the most important factors that increase risk of infection among these youths. Moreover, the absence of mediation in this study, and the knowledge–behavior gap among these teens has been reported in the general population (DiClemente et al., 1996; Fisher & Fisher, 2000), and broader conceptualizations of risk have been applied to other teens (Perrino, Gonzales–Soldevilla, Pantin, & Szapocznik, 2000).
This study relied solely on adolescent self–reports, and rates of teens’ sexual risk taking may reflect biases inherent in this methodology. Recent evidence, however, suggests that self–reports of risk behavior closely approximate actual behavior (Harrison, 1995), especially when questions are administered using computer technology as in this study (Romer, Hornik, & Stanton, 1997). Replication of these findings is necessary to fully understand how cognitive–behavioral factors influence sexual risk behavior among teens in psychiatric care. Our analyses did not address whether the model operates differently for older and younger adolescents or for different ethnic groups. Testing these questions requires larger samples to evaluate the moderating effects of age and ethnicity either by including interaction terms in the model or by using multigroup path analyses to compare path coefficients across different age and ethnic groups. These questions pose important directions for future research. We included sexually active and nonsexually active youth in the analyses to understand sexual risk behavior and this may have posed certain limitations on the findings. For example, there may be less association between cognitive and behavioral constructs and risky sexual behavior because less than half of the sample reported risky sex. Similarly, for sexually naive subjects, the measure of behavioral skills may reflect hypothetical attitudes. Furthermore, if the reasons for sexual initiation are different than the reasons for risky sex, our findings may obscure important differences between these two groups. However, behavior genetics research recently indicated that the same influences are implicated in both the initiation and risk–level of sexual behavior (Mustanski, Viken, Kaprio, & Rose, 2004).
Finally, it is possible that the unique patterns found in this study may be explained by variations in sample composition (e.g., age, ethnic diversity), study methods, or procedures rather than characteristics of youths in psychiatric care. For example, the motivation factor was reduced by two characteristics (perceived threat of HIV and personal attitudes about AIDS) and this might account for the lack of association between motivation and skills. Similarly, age was associated with risky sexual behavior and this may indirectly explain why age was so important in the model. However, compared to previous tests of cognitive–behavioral models with other teen populations, this study yielded similar levels of explained variance. Two earlier studies testing AIDS information, motivation, and behavioral skills explained 22% and 21% of the variance in adolescent STD risk (Boyer et al., 2000; Sieving et al., 1997), and Fisher et al. (1999) reported that the IMB model accounted for 75% and 46% of the variance in AIDS–risk for male and female adolescents respectively. Moreover, with two exceptions (see Fisher, Fisher, Williams, & Malloy, 1994; Fisher et al., 1999), the outcome measures used in the current study were similar to those in other research. Finally, adolescents with incomplete data had lower self–efficacy to practice prevention than teens with complete data. Excluding teens with incomplete data from the analyses may have diminished the relationship between self–efficacy and HIV risk taking behavior.
This study underscores the complexity of sexual risk taking among youths in psychiatric care. The proposed model proved to be somewhat useful for this population by illuminating important relationships among information, motivation, and behavioral skills in relation to sexual risk behavior and pointing to specific cognitive and behavioral mechanisms that may help reduce risk behavior, namely improving behavioral skills. However, other social and personal factors may be critical to enhance our understanding of risk taking among these teens. Findings shed light on the contribution of AIDS information, motivation and behavioral skills to sexual risk behavior among teens in psychiatric care, and they suggest that HIV prevention efforts go beyond cognitive–behavioral factors to include developmental considerations. It is likely that the most powerful explanatory model of sexual behavior for these youths will involve a combination of cognitive, behavioral, social, and personal risk mechanisms.
Acknowledgments
The authors gratefully acknowledge Keryn Pasch, Eryn Weber–Shifrin, Ginger Page, Maura Vodopivec, Hilary Lee, Josefina De Anda, Lisa Gerber, Eddy Borrayo, Marcus Hummings, John Baker, Eric Houston, Molly Roebuck, Jamie Eisenberg, and numerous others who assisted in data collection for this study. They also appreciate the valuable technical advice of Gerhard Mels and the insightful feedback of the editor and anonymous reviewers. Finally, they thank the administrators and clinical staff at Northwestern Memorial Hospital, Children’s Memorial Hospital, and the Institute for Juvenile Research at the University of Illinois at Chicago, and the participating parents and adolescents, without whose help this study would not have been possible.
Footnotes
This research was supported by the NIMH (Grant R01 MH58545), the Warren Wright Adolescent Center at Northwestern Memorial Hospital, and Northwestern Memorial Hospital’s Intramural Grants Program.
References
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross–informant correlations for situational specificity. Psychological Bulletin. 1987;101(2):213–232. [PubMed] [Google Scholar]
- Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice–Hall.
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two–step approach. Psychological Bulletin. 1988;103:411–423. [Google Scholar]
- Bagozzi RP, Edwards JR. A general approach for representing constructs in organizational research. Organizational Research Methods. 1998;1:45–87. [Google Scholar]
- Bandura, A. (1994). Social cognitive theory and exercise of control over HIV infection. In R.J. DiClemente & J.L. Petersen (Eds.), Preventing AIDS: Theories and methods of behavioral interventions. AIDS prevention and mental health (pp. 25–59). New York: Plenum Press.
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blum RW, Beuhring R, Shew M, Bearinger LH, Sieving RE, Resnick MD. The effects of race/ethnicity, income, and family structure on adolescent risk behaviors. American Journal of Public Health. 2000;90:1879–1884. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyer CB, Shafer M, Wibbelsman CJ, Seeberg D, Teitle E, Lovell N. Associations of sociodemographic, psychosocial, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. Journal of Adolescent Health. 2000;27:102–111. doi: 10.1016/s1054-139x(99)00113-5. [DOI] [PubMed] [Google Scholar]
- Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:316–322. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- Brown LK, DiClemente RJ, Beausoleil N. Comparison of HIV–related knowledge, attitudes, intentions and behaviors among sexually active and abstinent young adolescents. Journal of Adolescent Health. 1992;13:140–145. doi: 10.1016/1054-139x(92)90081-l. [DOI] [PubMed] [Google Scholar]
- Brown LK, Reynolds LA, Lourie KJ. A pilot HIV prevention program for adolescents in a psychiatric hospital. Psychiatric Services. 1997;48(4):531–533. doi: 10.1176/ps.48.4.531. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Single–sample cross–validation indices for covariance structures. Multivariate Behavioral Research. 1989;24:445–455. doi: 10.1207/s15327906mbr2404_4. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Kalichman SC. Risk for HIV infection among persons with severe mental illnesses. Clinical Psychology Review. 1997;17.3:271–291. doi: 10.1016/s0272-7358(97)00019-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2000). Cumulative AIDS cases; exposure categories; ten states/territories and cities reporting the highest number of AIDS cases; international statistics. Retrieved October 27, 2001, from http://www.cdc.gov/hiv/stats/
- Devieux J, Malow R, Stein JA, Jennings TE, Lucenko BA, Averhart C, et al. Impulsivity and HIV risk among adjudicated alcohol– and other drug–abusing adolescent offenders. AIDS Education and Prevention. 2002;14(Suppl B):24–35. doi: 10.1521/aeap.14.7.24.23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente, R.J., Ponton, L.E., & Hansen, W.B. (1996). New directions for adolescent risk prevention and health promotion research and interventions. In R.J. DiClemente, W.B. Hansen, & L.E. Ponton (Eds.), Handbook of adolescent health risk behavior (pp. 413–420). New York: Plenum Press.
- Doljanac RF, Zimmerman MA. Psychological factors and high–risk sexual behavior: Race differences among urban adolescents. Journal of Behavioral Medicine. 1998;21:451–467. doi: 10.1023/a:1018784326191. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Bryant FB, Emerson E, Wilson H, Pasch K. Tracing the roots of early sexual debut among adolescents in psychiatric care. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:594–608. doi: 10.1097/01.CHI.0000046833.09750.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber–Shifrin E. Understanding AIDS–risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Wilson HW, Emerson E, Bryant FB. Holding the line with a watchful eye: Parental monitoring, parental permissiveness, and risky sexual behavior among adolescents in psychiatric care. AIDS Education and Prevention. 2002;14:138–157. doi: 10.1521/aeap.14.2.138.23899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling S, Johnson ME, Fisher DG. Reliability of drug users’ self–report of recent drug use. Assess. 1994;1:382–392. [Google Scholar]
- Eiser JR, Ford N. Sexual relationships on holiday: A case of situational disinhibition? Journal of Social and Personal Relationships. 1995;12(3):323–339. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher, J.D., & Fisher, W.A. (2000). Theoretical approaches to individual–level change in HIV risk behavior. In J.L. Peterson, R.J. DiClemente (Eds.), Handbook of HIV prevention. AIDS prevention and mental health (pp. 3–55). New York: Kluwer Academic/Plenum.
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information–motivation–behavioral skills model–based HIV risk behavior change intervention for inner–city high school youth. Health Psychology. 2002;21:177–186. [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Williams S, Malloy TE. Empirical tests of an information–motivation–behavioral skills model of AIDS–preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13(3):238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Fisher JD. Understanding and promoting AIDS–preventive behavior: Insights from the theory of reasoned action. Health Psychology. 1995;14:255–264. doi: 10.1037//0278-6133.14.3.255. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Williams SS, Fisher JD, Malloy TE. Understanding AIDS risk behavior among sexually active urban adolescents: An empirical test of the information–motivation–behavioral skills model. AIDS and Behavior. 1999;3(1):13–23. [Google Scholar]
- Harrison LD. The validity of self–reported data on drug use. Journal of Drug Issues. 1995;25:91–111. [Google Scholar]
- Hollingshead, A.B. (1975). Four factor index of social status Unpublished manuscript, Yale University, New Haven, CT.
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Institute for Behavioral Science. (1991). Denver Youth Survey Youth Interview Schedule. University of Colorado: Boulder.
- Jaccard, J., & Wan, C.K. (1996). LISREL approaches to interaction effects in multiple regression Thousand Oaks, CA: Sage.
- Jemmott LS, Jemmott JB. Increasing condom–use intentions among sexually active black adolescent women: Effects of an AIDS prevention program. Nursing Research. 1992;41:273–279. [PubMed] [Google Scholar]
- Joreskog, K.G., & Sorbom, D.G. (1996). LISREL 8: User’s reference guide Chicago: Scientific Software International.
- Kalichman S, Stein JA, Malow R, Averhart C, Devieux J, Jennings T, et al. Predicting protected sexual behavior using the Information–Motivation–Behavior skills model among adolescent substance abusers in court–ordered treatment. Psychology, Health and Medicine. 2002;7:327–338. doi: 10.1080/13548500220139368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz RC, Mills K, Singh NN, Best AM. Knowledge and attitudes about AIDS: A comparison of public high school students, incarcerated delinquents, and emotionally disturbed adolescents. Journal of Youth and Adolescence. 1995;24:117–131. [Google Scholar]
- Kline, R.B. (1998). Principles and practice of structural equation modeling. New York: Guilford Press.
- Kotchick B, Shaffer A, Miller K, Forehand R. Adolescent sexual risk behavior: A multisystem perspective. Clinical Psychology Review. 2001;21(4):493–519. doi: 10.1016/s0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- Lerner, R. M., & Foch, T. T. (1987). Biological–psychosocial interactions in early adolescence: An overview of the issues. In Lerner, R. M., & Foch, T. T. (Eds.), Biological–psychosocial interactions in early adolescence (pp. 1–6). Hillsdale, NJ: Erlbaum.
- Mardia KV. Measures of multivariate skewness and kurtosis with applications. British Journal of Mathematical and Statistical Psychology. 1970;28:205–214. [Google Scholar]
- McFarlane AH, Bellisimo A, Norman GR. The role of family and peers in self–efficacy: Links to depression in adolescence. American Journal of Orthopsychiatry. 1995;65:402–410. doi: 10.1037/h0079655. [DOI] [PubMed] [Google Scholar]
- Metzler CW, Noell J, Biglan A, Ary D, Smolkowski K. The social context for risky sexual behavior among adolescents. Journal of Behavioral Medicine. 1994;17:419–438. doi: 10.1007/BF01858012. [DOI] [PubMed] [Google Scholar]
- Mustanski, B. S., Viken, R. J., Kaprio, J., & Rose, R. J. (2004). Sexual experience in young adulthood: A population–based twin study. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed]
- National Institute of Drug Abuse. (1995). Prevalence of drug use in the dc metropolitan area adult and juvenile offender populations: 1991. Rockville, MD: U.S. Department of Health and Human Services.
- Needle R, Fisher DG, Weatherby N, Chitwood D, Brown B, Cesari H, et al. Reliability of self–reported HIV risk behaviors of drug users. Psychological Addict Behavior. 1995;9:242–250. [Google Scholar]
- Perrino T, Gonzales–Soldevilla A, Pantin H, Szapocznik J. The role of families in adolescent HIV prevention: A review. Clinical Child and Family Psychology Review. 2000;3(2):81–96. doi: 10.1023/a:1009571518900. [DOI] [PubMed] [Google Scholar]
- Pinkerton SD, Holtgrave DR, Leviton LC, Wagstaff DA, Cecil H, Abramson PR. Toward a standard sexual behavior data set for HIV prevention evaluation. American Journal of Health Behavior. 1998;22(4):259–266. [Google Scholar]
- Rickman RL, Lodico M, DiClemente RJ, Morris R. Sexual communication is associated with condom use by sexually active adolescents. Journal of Adolescent Health. 1994;15(5):383–388. doi: 10.1016/1054-139x(94)90261-5. [DOI] [PubMed] [Google Scholar]
- Romer D, Hornik R, Stanton B. “Talking" computers: An efficient and private method to conduct interviews on sensitive health topics”. Journal of Sex Research. 1997;34:3–9. [Google Scholar]
- Rotheram–Borus MJ, Mahler KA, Rosario M. AIDS prevention with adolescents. AIDS Education and Prevention. 1995;7(4):320–336. [PubMed] [Google Scholar]
- Satorra, A., & Bentler, P.M. (1994). Corrections to test statistics and standard errors in covariance structure analysis. In A. von Eye & C.C. Clogg (Eds.), Latent variables analysis (pp. 399–419), Thousand Oaks, CA: Sage.
- Shaffer, D., Fisher, P., Piacentini, J., Schwab–Stone, M., & Wiks, J. (1991). Diagnostic Interview for Children (DISC 2.3)—Child Version. New York: Columbia University.
- Sieving R, Resnick MD, Bearinger L, Remafedi G, Taylor BA, Harmon B. Cognitive and behavioral predictors of sexually transmitted disease risk behavior among sexually active adolescents. Archives of Pediatrics and Adolescent Medicine. 1997;151(3):243–251. doi: 10.1001/archpedi.1997.02170400029006. [DOI] [PubMed] [Google Scholar]
- Smith C. Factors Associated with Early Sexual Activity among Urban Adolescents. Social Work. 1997;42(4):334–346. doi: 10.1093/sw/42.4.334. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A coefficient of reliability for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Watters, J.K. (1994). Street youth at risk for AIDS. Rockville, MD: National Institute on Drug Abuse.
- Weatherby NL, Needle R, Cesari H. Validity of self–reported drug use among injection drug users and crack cocaine users recruited through street outreach. Education Program Plan. 1994;17:347–355. [Google Scholar]
- West, S.G., Finch, J.F., & Curran, P.J. (1995). Structural equation models with nonnormal variables: Problems and remedies. In R.H. Hoyle (Eds.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Thousand Oaks, CA: Sage.
- Wothke, W. (1993). Nonpositive definite matrices in structural modeling. In K.A. Bollen & J.S. Long (Eds.), Testing structural equation models (pp. 256–293). Newbury Park, CA: Sage.


