Abstract
Respiratory infections are a major cause of mortality among young children and adults, particularly the elderly or those with underlying medical conditions. Many respiratory infections, including influenza, COVID-19, pneumococcal disease, and respiratory syncytial virus (RSV), have available vaccines and antiviral agents. However, vaccine coverage rates remain low. Experts representing a broad spectrum of medical specialties from the United Arab Emirates (UAE) made evidence-based recommendations on treating patients considered high risk for respiratory infections, highlighting gaps in current practices and suggesting strategies for improved communication between healthcare professionals and patients. To effectively manage respiratory infections, the experts emphasized the importance of adhering to guidelines, considering all vaccines and antiviral treatments, and strictly following vaccination schedules. Early testing upon recognition of symptoms was also encouraged. Improving vaccine uptake was considered crucial and could be achieved by educating patients about disease prevention through vaccines and the role of antiviral treatments for COVID-19. Addressing knowledge gaps and combating vaccine hesitancy among both patients and healthcare professionals were also essential steps. Recommendations for future initiatives include healthcare professionals educating the public on precautionary measures to reduce the spread of respiratory infections. Additionally, the experts agreed that clinical management guidelines for chronic diseases should be updated to include preventative strategies such as vaccines, prophylaxis, and counselling. Monitoring the performance of healthcare facilities using key performance indicators is also recommended to ensure effective management and continuous improvement of vaccination programs. Patient populations in the UAE who are considered at high risk of serious disease from respiratory infections have diverse medical needs and may access healthcare across a wide range of settings and specialisms. Therefore, it is vital that all healthcare professionals across specialisms who may engage with these individuals are able to provide appropriate advice on managing the risk through vaccination, prompt testing, and treatments as needed.
Keywords: Antiviral agents, Influenza, COVID-19, Pneumococcal infections, Respiratory syncytial virus, Vaccines, Management, Prevention
Key Summary Points
| Respiratory infections pose a significant health risk, particularly for young children, the elderly, and those with underlying conditions, yet vaccine coverage remains low |
| This study aimed to identify gaps in current vaccination and treatment practices for patients at high risk in the United Arab Emirates and propose expert-driven recommendations for improving prevention and management |
| Experts emphasized the need for adherence to vaccination guidelines, early testing, and better patient education to improve vaccine uptake and reduce severe disease outcomes |
| Addressing vaccine hesitancy among both patients and healthcare professionals, alongside integrating vaccines and prophylaxis into chronic disease management, is essential for better prevention |
| Implementing performance monitoring and updating clinical guidelines will help optimize vaccination programs and enhance respiratory infection management in high-risk populations |
Introduction
Respiratory infections are responsible for significant mortality, morbidity, and economic burden worldwide [1, 2]. They can affect all individuals in the population, but the highest rates are seen in adults older than 70 years and children younger than 5 years. Between 2019 and 2021, there were substantial decreases in global influenza and respiratory syncytial virus (RSV) incidence and deaths during the COVID-19 pandemic following the introduction of non-pharmaceutical interventions, such as face mask usage and mobility restrictions, which have been linked to the decreased transmission of respiratory viruses [1]. Nevertheless, in 2021, upper and lower respiratory infections had an estimated global incidence of 12.8 billion and 344 million, respectively. In 2021, there were 11.3 million deaths worldwide from respiratory infections, of which 2.18 million deaths were due to lower respiratory infections [1, 3].
The global incidence of and number of deaths caused by respiratory infections have increased following the pandemic, despite the availability of vaccines for influenza, COVID-19, pneumococcal disease, and RSV and antiviral treatments for COVID-19 and influenza [2]. The rebound in vaccine-preventable respiratory infections across all age groups and levels of socio-economic status may be at least partly due to immunity gaps that arose due to a decline in vaccine coverage rates during the COVID-19 pandemic. The World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) on Immunization has identified that despite integrated outreach efforts to minimize missed vaccination opportunities, there are other challenges that remain to be overcome, including identifying unvaccinated and undervaccinated children, promoting behavior change among health workers and caregivers to enhance vaccine uptake, ensuring accurate data recording and reporting, dealing with uncertainties regarding vaccine supply, addressing instability and insecurity in certain countries, and bridging resource gaps [4]. This group has suggested several approaches in the Eastern Mediterranean region to address these challenges, such as advocacy, use of technology, enhanced training for health workers, and improved surveillance of vaccine-preventable diseases.
Patient populations at high risk of serious disease from respiratory infections include individuals with chronic diseases, such as uncontrolled cardio-metabolic-renal diseases; those with impaired immune function (due to advanced age, chronic diseases impacting immune function, or the use of immunosuppressive therapies); and individuals with cancer [5]. Therefore, primary focus should be directed toward these vulnerable groups to ensure they receive the necessary care and preventative measures. Patients at high risk of serious disease from respiratory infections have diverse medical needs and may access healthcare across a wide range of settings and specialisms. Therefore, it is vital that all healthcare professionals (HCPs) who may engage with an individual at high risk of serious disease from respiratory infections are able to provide appropriate counselling and advice on managing the risk of serious respiratory infections through vaccination, prompt testing, and treatment as needed.
This article presents an in-depth assessment by an expert group of multidisciplinary medical leaders from the United Arab Emirates (UAE), offering cross-disciplinary guidance and evidence-based recommendations on the vaccination and treatment of patients who are considered high risk for serious influenza, COVID-19, pneumococcal, and RSV infections. We address the impact of respiratory infections, the perceived value of vaccination, and the guidelines currently informing vaccination, diagnosis, and treatment practices; gaps in day-to-day healthcare practices; and the training needs of HCPs to enhance patient care. We also discuss strategies for optimizing communication between HCPs and patients who are considered at high risk, focusing on the prevention, diagnosis, and treatment of respiratory infections.
Methods
A group of expert leaders from diverse medical specialties across the UAE convened with the aim of developing best practice guidance on the prevention and management of respiratory infections in patients at high risk and providing practical recommendations for protecting this population from adverse outcomes. The focus of discussions was on those respiratory infections for which vaccines are available: COVID-19, influenza, pneumococcal disease, and RSV. Experts from the following fields were included: cardiology, endocrinology, family medicine, internal medicine, obstetrics and gynecology, oncology, pediatric infectious diseases, public health, and pulmonary medicine.
We conducted a comprehensive literature review using PubMed and Google Scholar from 1 January 2020 to 1 August 2024 to identify relevant studies, clinical trials, and guidelines using the search terms “COVID”, “RSV”, “pneumococcal”, “influenza”, “United Arab Emirates”, “vaccine”, and other related keywords. The selected articles were searched against the topics of interest, and duplicates, non-English language, and preclinical studies were excluded (Fig. 1). The remaining articles were reviewed and used to develop recommendations based on evidence (Table 1). Given the limited number of relevant articles identified, no formal grading of the evidence was carried out.
Fig. 1.
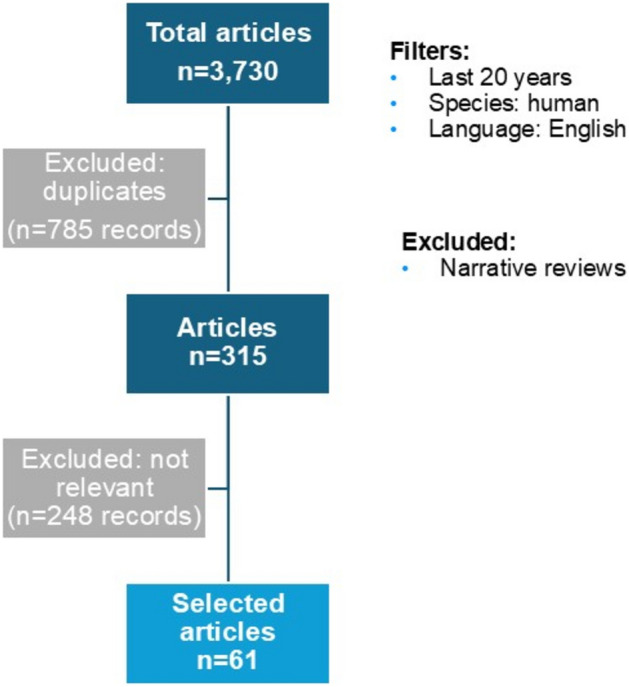
Literature analysis
Table 1.
Positioning and recommendations on prevention and management strategies for respiratory infections in the UAE.
| Prevalence |
Influenza and COVID-19 are currently considered more critical to manage than pneumococcal disease and RSV The prevalence of influenza and RSV may be shifting, with outbreaks noted in the off-season |
| Key populations considered at high risk for respiratory infections |
Respiratory infections are a key concern in the UAE for: Individuals with uncontrolled cardio-metabolic-renal diseases Pediatric patients Patients with cancer Those who are unvaccinated |
| Effective management of respiratory infections |
Management of respiratory infections involves: Referring to discipline-specific guidelines Understanding the available vaccines and antiviral treatment options Adhering to varying vaccine schedules Awareness of differing durations of immunity provided by vaccines Patients at high risk should be tested upon presentation with symptoms of any respiratory infection Patients should be encouraged to get tested as soon as symptoms of a respiratory infection are noticed |
| Educational needs of patients and healthcare professionals |
Educating patients at high risk and their families/caregivers about the impact of respiratory infections, the importance of vaccines for prevention, and the management of COVID-19 with antiviral treatments is crucial Addressing the knowledge gap among healthcare professionals regarding available vaccines and antiviral treatments is imperative to ensure best-practice patient care Tackling vaccine hesitancy among both patients and healthcare professionals is crucial to improving vaccination rates, enhancing public health outcomes, and building trust in medical interventions post pandemic |
| Future initiatives |
Healthcare professionals can play an important role in educating the public and dispelling myths about COVID-19 and other respiratory infections It is recommended to integrate clinical preventative services, such as vaccines, prophylaxis, and patient counselling, into the clinical management guidelines for chronic disease The performance of each facility should be monitored using clear key performance indicators, with a particular emphasis on vaccination coverage for patients at high risk |
RSV respiratory syncytial virus, UAE United Arab Emirates
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Burden of Respiratory Infections in the UAE
What is the Burden of These Infections on Patients in Day-to-Day Clinical Practice in the UAE?
From a cross-disciplinary perspective, experts identified respiratory infections as a significant concern for patients at high risk in the UAE. Among these, influenza and COVID-19 were considered the most critical.
In the UAE, the mortality rate from respiratory infections was 11.2 per 100,000 population in 2020, of which 6.7 per 100,000 population were due to COVID-19 [6]. Furthermore, the incidence of influenza, invasive pneumococcal disease (IPD), community-acquired pneumonia, and RSV increased following the COVID-19 pandemic [7].
Streptococcus pneumoniae accounted for the largest share of lower respiratory infection (LRI) episodes and deaths worldwide from 1990 to 2021, with an estimated 97.9 million episodes and 505,000 deaths. During the pandemic, the number of pneumococcal disease cases decreased. This reduction could be linked to the lower spread of other respiratory viruses, such as influenza and RSV, which often co-infect individuals and contribute to the incidence of pneumococcal disease [1]. An unmet need exists for data on the evolving pattern of pneumococcal disease in the UAE since the pandemic.
COVID-19 has evolved from a novel threat necessitating an emergency response to an infectious disease that populations must now manage and live with [8]. Since the onset of the pandemic, there have been approximately 777 million COVID-19 cases and 7.1 million deaths globally [9, 10]. In contrast, the UAE reported 1,067,030 cases and 2349 deaths [9, 10].
The following patient populations at high risk for severe respiratory infections were highlighted by the expert group: individuals with uncontrolled cardio-metabolic-renal diseases, patients with cancer, children, and those who are unvaccinated. It was also noted that respiratory infections are often not considered a priority for patients under obstetrics and gynecology care, despite their elevated risk.
In a single-center analysis at Sheikh Khalifa Specialty Hospital, Ras Al Khaimah, UAE, in 2019, prior to the COVID-19 pandemic, a total of 28.5% of patients presenting with acute respiratory infection were admitted, independent of the confirmation of any respiratory virus. The admission rate for all-cause acute respiratory infection and virus-positive cases was significantly higher among the elderly population compared to the pediatric and adult populations (p < 0.01) [11]. However, in the UAE there has been a substantial rise in severe acute respiratory infections among children aged ≤ 4 years, with reported cases increasing from 0–3 per week in 2021 to 12–97 per week in 2022, and further increasing to 19–142 per week in 2023 [7]. Furthermore, prior to the pandemic (January 2018 to January 2020), the percentage of infants < 2 years old presenting to University Hospital Sharjah, UAE, diagnosed with acute respiratory tract infections who tested positive for RSV was 18.8% [12]. In an analysis of Dubai insurance claims from January 2014 to September 2023, it was found that of 28,011 patients with RSV aged < 18 years, 49.3% were aged < 2 years, of which 39.1% required hospitalization [13].
Most patients with pneumococcal disease were ≤ 18 years of age, and those with IPD had a significantly higher mortality rate of 2.2%, compared to 0.7% for patients with non-IPD (p < 0.001) [14]. There was a high occurrence of penicillin-resistant S. pneumoniae, suggesting that these isolates are now endemic in the UAE and underlining the importance of continued surveillance, the implementation of effective antibiotic stewardship programs, and the vaccination of vulnerable populations. These data highlight the vulnerability of both elderly and pediatric populations in the UAE to respiratory infections.
The experts noted that since the COVID-19 pandemic, the prevalence of influenza and RSV has shifted, with outbreaks observed clinically during the off-season. This change may be partially attributed to delays in national immunization programs during the pandemic.
In 2019, the incidence of all respiratory viruses in the UAE was highest in December and lowest in September, with peaks in influenza observed in August and December [11]. Globally, the incidence of RSV and influenza declined during 2020 and 2021 due to the use of non-pharmaceutical interventions, such as stay-at-home orders, school and community closures, and facemask requirements [1]. However, once these interventions were relaxed, outbreaks of RSV and influenza were observed during the off-seasons [1], similar to the pattern observed by experts in the UAE.
A retrospective analysis of the UAE antimicrobial resistance surveillance program from 2010 to 2021 reported an increasing burden of pneumococcal disease over time until the pandemic, followed by a sharp decrease, potentially attributable to social distancing and other non-pharmacological interventions, though it may also have resulted from decreased testing during the pandemic [14].
Improving the Management and Mitigation of Respiratory Infections in Patients at High Risk
What Are the Licensed Vaccines and Antiviral Treatment Options for Influenza, COVID-19, RSV, and Pneumococcal Disease in the UAE?
Effective prevention and management of respiratory infections in patients at high risk in the UAE involve several considerations. These include adhering to discipline-specific guidelines, understanding the available vaccines and antiviral treatment options, following varying vaccine schedules, and accounting for the differing durations of immunity provided by vaccines.
Vaccines against COVID-19 are available and free of charge for medically eligible UAE citizens and residents, and several antiviral treatment options for COVID-19 are also available. Remdesivir was approved in July 2020 as an emergency treatment for severe COVID-19 in patients who have been hospitalized [15]. Despite the availability of PAXLOVID® (nirmatrelvir + ritonavir) as an antiviral treatment approved for patients at high risk of severe COVID-19 [16], not all eligible patients are receiving it [17]. This may, in part, be due to the need for prompt and accurate testing before administration [16, 17].
The prophylactic use of an RSV vaccine and RSV monoclonal antibody was recently approved in the UAE and is recommended for high-risk infants (aged < 1 year) and children (aged < 2 years) [18]. All patients aged ≥ 65 years who are susceptible to complications from RSV or have existing medical conditions are eligible to receive an RSV vaccine in the UAE. Similarly, the US Centers for Disease Control and Prevention (CDC) recommends RSV vaccination for all adults aged ≥ 75 years and for adults aged 60–74 years who are at increased risk of severe RSV (Table 1) [19]. The CDC also recommends the use of a bivalent RSVpreF vaccine in pregnant women during 32–36 weeks of gestation to protect their newborns from severe RSV illness [19].
The UAE has a formal national influenza vaccination policy in both the public and private sectors based on WHO recommendations [20]. Vaccines against seasonal influenza are available for children aged ≥ 6 months old, adults, and those considered at high risk. Pneumococcal conjugate vaccines (PCV) against pneumococcal disease have been included in the national immunization schedule for routine services in the UAE since 2007 [21]. PCV-13, PCV-20, and pneumococcal polysaccharide 23 valent (PPV-23) are available for patients at high risk [21, 22]. In 2023, the national vaccine coverage for pneumococcal conjugate vaccines was estimated at 94% [21].
What Gaps Exist in Education, Knowledge, or Best-Practice Management of Patients at High Risk?
A majority of experts noted that in their clinical practice, patients who died or experienced severe symptoms from respiratory infections, such as myocardial infarction following COVID-19, were often unvaccinated.
The UAE approved the emergency use of the BBIBP-CorV inactivated COVID-19 vaccine in September 2020, followed by the approval of the BNT162b2 vaccine. It was one of the first countries to achieve early vaccine coverage, with over 70% of the population vaccinated early on. By the end of November 2021, nearly 90.4% of the UAE population had been fully vaccinated, and 99% had received at least their first dose [23].
Several studies have shown that COVID-19 vaccination status significantly influences hospital admissions, symptom severity, and mortality rates [23–26]. In the UAE, high COVID-19 vaccination coverage during the pandemic was demonstrated to have significantly reduced COVID-19-related hospitalizations, intensive care unit (ICU) admissions, and mortality (p < 0.001) in a study involving 2277 patients [23]. The mortality rate was also significantly higher among patients who had not been vaccinated compared with those who were partially or fully vaccinated (p > 0.001) [23, 24].
A cross-sectional study conducted in Algeria, Egypt, Iraq, Lebanon, Libya, Tunisia, and the UAE found that being aged ≥ 65 years, having chronic diseases or obesity, and being unvaccinated were significantly associated with severe COVID-19 symptoms [24]. Cardiovascular complications were common in patients with COVID-19 [25]. Additionally, a retrospective cohort study of 231,037 patients infected with COVID-19 found that severe or critical cases were more prevalent among patients who had not been vaccinated. The risk of acute myocardial infarction and ischemic stroke was also significantly higher in patients not vaccinated [26]. A systematic review of eight studies from the USA, the UK, Turkey, China, and Singapore, involving a total of 8,736,943 patients, demonstrated that COVID-19 was an independent risk factor for poor prognosis in patients with myocardial infarction [25]. These studies underscore the importance of COVID-19 vaccination in managing outbreaks of COVID-19 and protecting patients considered vulnerable.
Patient Perspective
The experts noted that educating patients at high risk and their families or caregivers about the impact of respiratory infections, the importance of vaccines in prevention, and the management of COVID-19 using antiviral treatments is crucial to delivering best-practice care for patients at high risk.
In a cross-sectional survey conducted by Jirjees et al. between June and August 2021, over 40% of people in the UAE sought information about medical topics, such as COVID-19, from HCPs, including physicians and pharmacists [24]. However, the majority of participants obtained their information from family, friends, media, and social media [24, 27, 28]. Therefore, there is an urgent need to offer trusted sources of information about respiratory infections to address misconceptions and curb the spread of false information. Furthermore, in the Jirjees et al. study, more than half of patients in the UAE used non-pharmacological therapies, such as vitamins, dietary supplements, and herbs, either prophylactically or during COVID-19 infection [24]. Another cross-sectional survey conducted by Radwan et al. in the UAE in May 2020 reported that among respondents who used non-prescription diets and dietary supplements (e.g., citrus fruits and herbal teas) for the prevention or treatment of COVID-19, only 21% received advice about these regimens from HCPs, while 40% obtained the information from social media and 29% from family and friends [27]. Given the limited evidence supporting the use of non-prescription diets and supplements for COVID-19 [24, 27], physicians play a crucial role in raising awareness about their proper value and potential limitations. Furthermore, many studies have shown that direct recommendations and information from HCPs are the most important factors influencing an individual’s decision to accept a vaccine [29].
Educational needs exist even among individuals with good general education. For example, a cross-sectional survey of 467 students studying medical and non-medical subjects at Ajman University in the UAE was conducted between March and August 2021. The study revealed that 81% of respondents were aware that individuals with serious medical conditions are more likely to experience severe health effects from COVID-19. However, participants were not always aware of the available vaccine options, eligibility criteria, or which schedules were recommended. In addition, many participants believed that antibiotics are an effective treatment for COVID-19 and that vitamins or vaccines against pneumonia offer protection against the virus [30].
HCP Perspective
Addressing knowledge gaps among HCPs regarding available vaccines and antiviral treatments is essential for improving the prevention and management of respiratory infections.
For HCPs to effectively counsel patients on vaccines, they must first have confidence in the vaccines’ safety and effectiveness. A cross-sectional survey of UAE physicians’ attitudes toward vaccines was conducted before (June to October 2020) and after (November 2022 to March 2023) the availability of COVID-19 vaccines [29]. Around a third of participants were family physicians or internists, while two-thirds were physicians working in governmental hospitals. Although investigators reported a high level of vaccine acceptance (95%) in both cohorts, they also identified doubts regarding safety, effectiveness, and necessity, as well as a general level of complacency and lack of ownership regarding patients’ vaccination status. For example, 74.4% reported not having enough time to advise patients about vaccines [29].
One of the first studies in the UAE assessing attitudes toward COVID-19 vaccines among healthcare workers, including consultants/specialists, general practitioners, medical residents, nurses, pharmacy/laboratory staff, paramedics, radiology technicians, and other ancillary staff, was conducted prior to the vaccine’s availability (from November 2020 to January 2021). Investigators reported that 58% of healthcare workers were willing to take the vaccine and administer it to their family members, but a considerable proportion were hesitant to take the vaccine immediately. Reasons for refusal included concerns about side effects [31].
In a cross-sectional survey of physiotherapy students at Gulf Medical University, UAE, conducted from January to December 2022, 28.7% of respondents questioned the safety of COVID-19 vaccines [31, 32]. Furthermore, 30% believed that the COVID-19 vaccine could cause various issues, such as headaches and fever. A smaller group held misconceptions that COVID-19 might lead to infertility, paralysis, and cancer, although they were unable to provide scientific evidence to support these beliefs [32].
HCPs would benefit from increased awareness of the differences between various infectious pathogens and vaccine technologies, which result in varying recommended schedules. Many physicians are still unaware of the availability of RSV vaccines and may have a limited understanding of the frequency and potential impact of RSV among high-risk adults, as this is an evolving area of scientific knowledge currently.
There exists a noticeable gap in awareness of strategies for managing respiratory infections across diverse medical specialties. Bridging this gap requires the implementation of guidelines that integrate specialized care pathways across the different specialties, ensuring improved management and mitigation of respiratory infection risks across all patient groups. A comprehensive educational strategy is essential, targeting both physicians and patients at high risk, alongside their families or caregivers.
What Challenges Exist that Prevent Appropriate Vaccination and/or Treatment for Respiratory Viral Infections Among Patients at High Risk?
Tackling vaccine hesitancy among both patients and HCPs is crucial for improving vaccination rates, enhancing public health outcomes, and building trust in medical interventions.
Vaccination remains the most effective prophylactic measure for significantly reducing the severity of COVID-19 symptoms. However, vaccine hesitancy continues to be a key challenge among both patients and HCPs in the UAE [24]. Addressing barriers to vaccination acceptance is a prominent issue globally [33–38].
Vaccine hesitancy may stem from economic, social, or political sources. During the COVID-19 pandemic, it was recognized that vaccine hesitancy would have a major impact on the uptake of the newly developed vaccines, with initial studies indicating acceptance rates as low as 30.4% [29]. Notably, COVID-19 vaccine hesitancy has led to increased reluctance to vaccinate against other vaccine-preventable diseases, such as diphtheria, measles, and mumps [29]. Concerns about vaccine costs (whether genuine or because of misperceptions) may be a barrier to uptake in UAE [39]. For example, in a survey of 815 UAE residents conducted in 2020, concerns about a lack of insurance coverage or lack of affordability of influenza vaccines was one of the reasons cited by unvaccinated individuals for not being immunized [40]. Access to vaccine services for non-national residents regardless of insurance status was a crucial policy in UAE to reduce cases and transmission during the COVID-19 pandemic [39].
HCPs in the UAE have reported receiving minimal training and expressed feeling ill-equipped to address vaccine hesitancy among their patients. Another challenge to appropriate vaccination, reported by physicians, is the limited time and lack of resources to effectively counsel patients and discuss their concerns [29].
Discussion
Expert Recommendations
Which Patients Are at High Risk of Serious Influenza, COVID-19, Pneumococcal, and RSV Infections, and How Should They Be Prevented in the UAE?
The patient populations at high risk of respiratory infections, and the guidelines currently employed across various disciplines in the UAE to manage influenza, COVID-19, pneumococcal disease, and RSV, are outlined in Table 2. The patient groups identified to be at high risk within cardiology, endocrinology, internal medicine, oncology, and primary care were consistent across influenza, COVID-19, and pneumococcal disease.
Table 2.
International recommendations and the specific patient populations that could benefit from vaccination against respiratory infections in the UAE
| Specialism | Which patients should be vaccinated? | What guidelines on vaccination use are used? | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Influenza | COVID-19 | Pneumococcal | RSV vaccine | RSV prophylaxis | Influenza | COVID-19 | Pneumococcal | RSV | |
| Cardiology | All cardiac event cases (high risk) with MI, CHF, and CRS | All patients ≥ 65 years that are susceptible to complication from RSV | Infants with CHD (< 1 years) [18] | ACC [52]; ESC [53] | Not stated | ||||
| Endocrinology | Patients with diabetes (with or without risk factors) | No | AACE [54]; CDCa [55] | N/A | |||||
| Internal medicine | All adults; patients at high risk | No | US and local UAE guidelines | N/A | |||||
| Obstetrics and gynecology | All pregnant women during high season | Patients at risk | Not sure | Individuals with medical conditions [51] | High-risk patients during high season [18] | ACOG; RCOG | ACOG; RCOG [49] | No | ACOG [42], RCOG |
| Oncologyb | All immunocompromised patients with cancer; patients who have not been vaccinated | No | ESMO; NCCN [5] | ||||||
| Pediatrics | All > 6 months | If available, for all patients at high risk | All children (PPSV23 for high-risk group) |
High-risk (< 2 years), preterm infants (< 1 years) Infants with CHD (< 1 years) Immunocompromised infants during the RSV season (< 2 years) [18] |
ACIP [55]; IDSA [56] | ACIP [55] | Local and regional guidelines adapted from AAP [41] | ||
| Primary care | Everyone (very low uptake) | Patients at high risk | None | None | |||||
| Public health | All patients at high risk | Not recommended by national authority | Children and elderly | Not recommended by national authority | National guidelines (MOHP) | N/A | National guideline (MOHP) | N/A | |
AACE American Association of Clinical Endocrinology, AAP American Academy of Pediatrics, ACC American College of Cardiology, ACOG American College of Obstetricians and Gynecologists, ACIP Advisory Committee on Immunization Practices, CDC Centers for Disease Control and Prevention, CHD chronic heart disease, CHF chronic heart failure, CKD chronic kidney disease, CRS cardio-renal syndrome, ESC European Society of Cardiology, ESMO European Society for Medical Oncology, FDA Food and Drug Administration, IDSA Infectious Diseases Society of America, MI myocardial infarction, MOHP Ministry of Health & Prevention, N/A not applicable, NCCN National Comprehensive Cancer Network, PPSV23 23-valent pneumococcal polysaccharide vaccine, RCOG Royal College of Obstetricians and Gynaecologists, UAE United Arab Emirates, US United States
aOn June 27, 2024, the CDC adopted the ACIP’s recommendations for use of 2024–2025 COVID-19 vaccines in people aged ≥ 6 months as approved or authorized by FDA [57]
bInfluenza vaccine recommended annually in oncology specialism
The US CDC recommends maternal immunization with the RSVpreF vaccine Abrysvo™ for pregnant mothers between 32 and 36 weeks 6 days of gestation, during the peak season from September through January. A prophylactic RSV monoclonal antibody, nirsevimab, is also available in the UAE for preterm infants and children aged < 2 years of age [41]. RSV vaccination is also available for people aged ≥ 60 years [42]. However, there is still a need to clarify recommendations for the use of RSV vaccination across specialties in some healthcare settings in the UAE.
The UAE benefits from several advantages in planning, monitoring, and managing immunizations. The UAE has updated routine immunization micro-plans in seven districts to boost vaccination coverage, a technical advisory group that reviews monitoring and evaluation data and provides recommendations for improving program performance, and a national research agenda on immunization. Additionally, there is an annual workplan for immunization activities, and evaluation results are effectively communicated between national and subnational levels [43].
How Should Respiratory Infections Be Managed in Patients at High Risk in the UAE?
Acute Management
Early in the pandemic, a mass testing strategy for SARS-CoV-2 was implemented throughout the UAE [44]. As of August 2024, over 200 million polymerase chain reaction (PCR) tests had been conducted, diagnosing over one million cases of COVID-19 [45]. As a result of the overlap of symptoms in presentation, we recommend that patients at high risk be tested upon presentation with symptoms of any respiratory infection, regardless of severity. Furthermore, patients should be encouraged to seek testing for respiratory infections as soon as symptoms are noticed. Early antiviral treatment is recommended according to the patient’s risk profile in advance of receipt of test results in order to minimize the risk of severe disease.
For patients who are at high risk, ambulatory, and who are identified as having a positive case of COVID-19, the antiviral treatment nirmatrelvir/ritonavir is recommended (Table 3). Therefore, educating patients and their families or caregivers about how respiratory infections impact their health, strategies for prevention through vaccines, and methods for managing conditions with antiviral treatment (for COVID-19) will help improve vaccine uptake.
Table 3.
International recommendations and the specific patient populations that could benefit from antiviral therapies in the UAE
| Specialism | Which patients would you treat? | What guideline(s) do you follow? |
|---|---|---|
| Cardiology | Patients at high risk | ACC [52]; ESC [53] |
| Endocrinology | Patients at high risk with (uncontrolled) diabetes | CDC [55] and UAE guidelines |
| Internal medicine |
Patients with a moderate to severe infection Patients at high risk with mild to moderate symptoms |
US and local UAE guidelines |
| Obstetrics and gynecology | Case-by-case decision made with an infectious disease specialist during the second and third trimester | Local guidelines RCOG, and WHO recommendation [49] |
| Oncology | All patients with cancer who are immunocompromised | NCCN [5]; ESMO |
| Pediatrics | High risk > 28 days | Local guideline |
| Primary care | Patients at high risk | Not stated |
| Public health | N/A | N/A |
ACC American College of Cardiology, CDC Centers for Disease Control and Prevention, ESC European Society of Cardiology, ESMO European Society for Medical Oncology, N/A not applicable, RCOG Royal College of Obstetricians and Gynaecologists, UAE United Arab Emirates, US United States
Long-Term Prevention
Navigating the care journey can be complex for patients at high risk and associated with challenges such as access to specialized care and delays in diagnosis. Therefore, there is a need for specialty physicians to not only provide counselling and education to patients about their risks and treatment options but also ensure that patients identified to be at high risk receive timely and effective care, which improves health outcomes and reduces the burden of disease.
HCPs play an important role in educating the public on precautionary measures to mitigate the spread of disease and dispel myths about COVID-19. A survey of 109 healthcare workers in the UAE found that they possessed extensive knowledge about COVID-19 and related viruses. Additionally, they demonstrated good adherence to social distancing, wearing facemasks, and following government guidelines on preventative measures, positioning them as exemplary role models [46].
The UAE has a strong foundation for tackling the increasing challenge of chronic diseases [47]. Therefore, experts recommend integrating clinical preventative services, such as vaccines, prophylaxis, and counselling, into the clinical management guidelines for chronic diseases.
Experts recommend monitoring the performance of each facility using clear key performance indicators, with a particular emphasis on vaccination coverage for patients at high risk. These indicators may include vaccination rates, adherence to vaccine schedules, follow-up rates for subsequent doses, adverse event reporting, and patient satisfaction. This approach ensures the effective management and continuous improvement of vaccination programs.
What is the Role of Specialists with Respect to Vaccination?
In the UAE, primary care physicians handle most vaccinations. Therefore, enhancing education among primary care/family medicine physicians about the importance of ensuring patients receive all recommended vaccinations is essential. Furthermore, streamlining processes to integrate vaccination services across healthcare sectors—including pharmacies, nursing, and specialist care—will generate more opportunities to counsel patients on vaccines against respiratory infections, ultimately ensuring broader and more effective vaccination coverage for those who need it most [42]. Ensuring that vaccination guidelines are implemented across disciplines will increase public trust, enhance vaccine uptake, and ultimately lead to improved patient outcomes. Raising awareness among HCPs across disciplines and specialties about the approved and effective vaccines and antiviral treatments available for patients at high risk in the UAE is a key step toward achieving best practices. In particular, highlighting to obstetrics and gynecologists the availability of recently approved RSV vaccines for maternal immunization. As a key part of a more holistic approach to immunizations, specialists should take ownership of preventing respiratory conditions among patients at high risk under their care through patient counselling and planning for potential infections should they occur.
How Can Vaccine Hesitancy Be Overcome?
Education from trusted sources plays an important role in shaping how people choose to protect and treat themselves before and during an infection. Key information needed to address vaccine hesitancy in the general public includes raising awareness about who is at high risk of serious disease from respiratory infections, the prevalence of these infections in the UAE, and the potential consequences of such infections for high-risk individuals. Additionally, providing balanced, evidence-based, and trustworthy information about available vaccines and antiviral treatments, how they were assessed, and the evidence base supporting their use is essential.
Future vaccine campaign strategies should equip HCPs with clear guidance on counselling patients about the importance of vaccinations and addressing their own challenges and concerns [31, 48, 49]. These strategies should also support public health and educational initiatives to enhance vaccine knowledge [31]. Key elements include dispelling misconceptions about side effects, especially those at high risk who show low intent to receive the vaccine, and recognizing individual preferences for vaccine options [32]. Additionally, leveraging insights from successful vaccination programs with high coverage rates (e.g., 90% of staff at one center received influenza and COVID-19 vaccines through a targeted program) can help reduce vaccine hesitancy and improve overall vaccine uptake [31].
Conclusion
Patients at high risk of respiratory diseases experience significant burden of disease, morbidity, and mortality in the UAE. A range of guidelines are currently being used across specialisms to inform best practices regarding vaccination and antiviral treatment; there is a need for a unified national guideline of best practices regarding the prevention and treatment of respiratory diseases. Vaccine hesitancy and clinical inertia hinder patients from being vaccinated. Patient counseling efforts must be supported by ongoing education for HCPs and investment in the prevention of respiratory diseases. Overall, enhancing coverage requires a comprehensive approach that includes both individual-level interventions and national vaccine requirements. This position paper provides recommendations that reflect the challenges faced by different specialties and the realities of clinical practice in UAE but may also be valuable in other countries in the region and beyond.
Acknowledgments
Medical Writing/Editorial Assistance
Medical writing and editorial support were provided by Innovaacom LLC and were funded by Pfizer Gulf FZ LLC, according to Good Publication Practice guidelines [50]. Authors retain responsibility for the opinions and conclusions.
Author Contributions
All authors (Abdullah Shehab, Huda Al Dhanhani, Omar Alhammadi, Mohamed Badi Hassan, Mohamed Farghaly, Ahmed Hassoun, Bassam Mahboub, Mona Tahlak, Reem Faisal Abutayeh, Hammam Haridy, Ashraf Hassanien, Jean Joury, and Humaid O. Al-Shamsi) contributed to the conceptualization and methodology of the manuscript. The elaboration of recommendations was discussed and agreed upon among the group, and they participated in the drafting and revision of the manuscript. All authors reviewed and approved the final, submitted version.
Funding
Pfizer Gulf FZ LLC provided funding for the expert group meeting, medical writing/editorial support for the development of the manuscript and for the Rapid Service Fee. Neither honoraria nor payments were made for authorship.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed.
Declarations
Conflicts of Interest
Ahmed Hassoun received payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing or educational events from EVA Pharma, and received support for attending meetings and/or travel from AstraZeneca and VIATRIS. Reem Faisal Abutayeh, Hammam Haridy, Ashraf Hassanien, and Jean Joury are Pfizer employees and may hold stock or stock options. Abdullah Shehab, Huda Al Dhanhani, Omar Alhammadi, Mohamed Badi Hassan, Mohamed Farghaly, Bassam Mahboub, Mona Tahlak, and Humaid O. Al-Shamsi have nothing to disclose.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
References
- 1.GBD 2021 Lower Respiratory Infections and Antimicrobial Resistance Collaborators. Global, regional, and national incidence and mortality burden of non-COVID-19 lower respiratory infections and aetiologies, 1990–2021: a systematic analysis from the Global Burden of Disease Study 2021. Lancet Infect Dis. 2024;24:974–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine. 2021;37:100986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IHME. IHME, Global burden of disease—deaths from respiratory infections, 2021. Our World Data. 2024. https://ourworldindata.org/grapher/deaths-from-respiratory-infections. Accessed 2024 Jul 8.
- 4.Meeting of the Strategic Advisory Group of Experts on Immunization, March 2024: conclusions and recommendations. https://www.who.int/publications/i/item/WER-9922-285-306. Accessed 2024 Aug 7.
- 5.Prevention and Treatment of Cancer-Related Infections—NCCN Guidelines. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1457. Accessed 2024 Aug 14.
- 6.World Health Organization (WHO). Respiratory infections—deaths by sex and age group for a selected country or area and year—UAE. 2024. https://platform.who.int/mortality/themes/theme-details/topics/topic-details/MDB/respiratory-infections. Accessed 2024 Aug 11.
- 7.World Health Organization (WHO). Influenza surveillance report. Influenza surveillance report in the UAE. 2024. https://app.powerbi.com/view?r=eyJrIjoiYWU4YjUyN2YtMDBkOC00MGI1LTlhN2UtZGE5NThjY2E1ZThhIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9. Accessed 2024 Aug 11.
- 8.GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 cases | WHO COVID-19 dashboard. https://data.who.int/dashboards/covid19/cases?n=c. Accessed 2024 Nov 12.
- 10.COVID-19 deaths | WHO COVID-19 dashboard. https://data.who.int/dashboards/covid19/deaths?n=c. Accessed 2024 Nov 12.
- 11.Jeon J-H, Han M, Chang H-E, et al. Incidence and seasonality of respiratory viruses causing acute respiratory infections in the Northern United Arab Emirates. J Med Virol. 2019;91(8):1378–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saeed BQ, Sharif HA, Adrees AO, et al. Incidence of respiratory syncytial virus among young children in United Arab Emirates. J Nat Sci Biol Med. 2023;8(14):52–8. [Google Scholar]
- 13.Zayed M, Abdelaziz MA, Farghaly M, et al. Evaluation of disease burden (comorbidities, length of hospitalization and healthcare resource utilization) from respiratory syncytial virus (RSV) illness in United Arab Emirates: a retrospective cohort claims database study. Value Health. 2024;27(6):S408. [Google Scholar]
- 14.Senok A, Thomsen J, Abdulrazzaq NM, et al. Antimicrobial resistance in Streptococcus pneumoniae: a retrospective analysis of emerging trends in the United Arab Emirates from 2010 to 2021. Front Public Health. 2023;11:1244357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamb YN. Remdesivir: first approval. Drugs. 2020;80(13):1355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO). WHO recommends highly successful COVID-19 therapy and calls for wide geographical distribution and transparency from originator. 2022. https://www.who.int/news/item/22-04-2022-who-recommends-highly-successful-covid-19-therapy-and-calls-for-wide-geographical-distribution-and-transparency-from-originator. Accessed 2024 Aug 14.
- 17.Pepperrell T, Ellis L, Wang J, Hill A. Barriers to worldwide access for paxlovid, a new treatment for COVID-19. Open Forum Infect Dis. 2022;9(9):ofac174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Department of Health Abu Dhabi. Standard for prophylaxis to reduce the risk of respiratory syncytial virus (RSV) in high risk infants and children. 2023. https://www.doh.gov.ae/-/media/280AE05D53E74F7FB8C06B9CE38D7A14.ashx. Accessed 2024 Aug 14.
- 19.CDC. RSV (respiratory syncytial virus) immunizations | CDC. 2024. https://www.cdc.gov/vaccines/vpd/rsv/index.html#print. Accessed 2024 Sep 23.
- 20.WHO. Influenza vaccination policy. WHO—influenza vaccination policy. 2024. https://immunizationdata.who.int/global/wiise-detail-page/influenza-vaccination-policy?ISO_3_CODE=ARE&YEAR=. Accessed 2024 Aug 14.
- 21.WHO. WHO Immunization Data portal—Eastern Mediterranean region. 2024. https://immunizationdata.who.int/dashboard/regions/eastern-mediterranean-region/ARE. Accessed 2024 Aug 14.
- 22.Zayed M, Joury J, Farghaly M, et al. Budgetary impact of 20-valent pneumococcal conjugate vaccine use for adult expatriates living in Dubai. Curr Ther Res Clin Exp. 2023;14(98):100698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pradhan R, Ahmed LA, Al Kaabi N, El Subki WI, Zaabi AA. Impact of COVID-19 vaccination on the trend of hospital admission and mortality in two tertiary care hospitals in the United Arab Emirates: a retrospective study. NEMJ. 2023. 10.2174/04666230316121757. [Google Scholar]
- 24.Jirjees F, Barakat M, Shubbar Q, Othman B, Alzubaidi H, Al-Obaidi H. Perceptions of COVID-19 symptoms, prevention, and treatment strategies among people in seven Arab countries: a cross-sectional study. J Infect Public Health. 2022;15(10):1108–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rus M, Ardelean AI, Andronie-Cioara FL, Filimon GC. Acute myocardial infarction during the COVID-19 pandemic: long-term outcomes and prognosis-a systematic review. Life (Basel). 2024;14(2):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim Y-E, Huh K, Park Y-J, Peck KR, Jung J. Association between vaccination and acute myocardial infarction and ischemic stroke after COVID-19 infection. JAMA. 2022;328(9):887–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radwan H, Hasan H, Jaafar Z, et al. Diets and dietary supplements used during the COVID-19 pandemic in the United Arab Emirates: a cross-sectional survey. Saudi Pharm J. 2022;30(4):421–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alremeithi HM, Alghefli AK, Almadhani R, Baynouna AlKetbi LM. Knowledge, attitude, and practices toward SARS-COV-2 infection in the United Arab Emirates population: an online community-based cross-sectional survey. Front Public Health. 2021;19(9): 687628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barqawi HJ, Samara KA, Haddad ES, Bakkour LM, Amawi FB. Attitudes and practices to adult vaccination among physicians before and after COVID-19 pandemic in the United Arab Emirates. Vaccine X. 2024;17:100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shahwan M, Suliman A, Abdulrahman Jairoun A, et al. Prevalence, knowledge and potential determinants of COVID-19 vaccine acceptability among university students in the United Arab Emirates: findings and implications. J Multidiscip Healthc. 2022;11(15):81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saddik B, Al-Bluwi N, Shukla A, et al. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: a cross-sectional study from the United Arab Emirates. Hum Vaccines Immunother. 2022;18(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Almheiri S, Hazari A, Kumar P, Kumar S, Girish S. A comprehensive survey on the beliefs, perceptions, and clinical manifestations of pre and post Covid-19 vaccinations among physiotherapy students in the United Arab Emirates. PLoS ONE. 2023;18(4):e0282385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.AlKetbi LMB, Elharake JA, Memari SA, et al. COVID-19 vaccine acceptance among healthcare workers in the United Arab Emirates. IJID Reg. 2021;1:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alsuwaidi AR, Elbarazi I, Al-Hamad S, Aldhaheri R, Sheek-Hussein M, Narchi H. Vaccine hesitancy and its determinants among Arab parents: a cross-sectional survey in the United Arab Emirates. Hum Vaccines Immunother. 2020;16(12):3163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alsuwaidi AR, Hammad HAA-K, Elbarazi I, Sheek-Hussein M. Vaccine hesitancy within the Muslim community: Islamic faith and public health perspectives. Hum Vaccines Immunother. 2023;19(1):2190716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andrade G, Bedewy D, Bani I. Motivational factors to receive the COVID-19 vaccine in the United Arab Emirates: a cross-sectional study. J Community Health. 2022;47(3):530–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elbarazi I, Al-Hamad S, Alfalasi S, Aldhaheri R, Dubé E, Alsuwaidi AR. Exploring vaccine hesitancy among healthcare providers in the United Arab Emirates: a qualitative study. Hum Vaccines Immunother. 2021;17(7):2018–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rahbeni TA, Satapathy P, Itumalla R, et al. COVID-19 vaccine hesitancy: umbrella review of systematic reviews and meta-analysis. JMIR Public Health Surveill. 2024;30(10):e54769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koksal I, Al Awaidy S, Assiri AM, et al. Adult vaccination in three Eastern Mediterranean countries: current status, challenges and the way forward. Expert Rev Vaccines. 2024;23(1):1068–84. [DOI] [PubMed] [Google Scholar]
- 40.Saeed B, Imtiaz B, Alhaj S, et al. Knowledge, attitudes, behaviors and risk perception towards seasonal influenza and vaccination among adult population of UAE. Periodicals Eng Nat Sci. 2022;10(2):30–40. [Google Scholar]
- 41.Immunization Schedules | Red Book Online | American Academy of Pediatrics. https://publications.aap.org/redbook/pages/Immunization-Schedules?autologincheck=redirected. Accessed 2024 Aug 14.
- 42.ACOG. Maternal respiratory syncytial virus vaccination. 2023. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2023/09/maternal-respiratory-syncytial-virus-vaccination. Accessed 2024 Aug 14.
- 43.WHO. WHO Planning, managing and monitoring immunization systems. WHO Planning, managing and monitoring immunization systems. 2024. https://immunizationdata.who.int/global/wiise-detail-page/planning-management-and-monitoring?ISO_3_CODE=ARE&YEAR=. Accessed 2024 Aug 14.
- 44.Al-Hosani F, Al-Mazrouei S, Al-Memari S, Al-Yafei Z, Paulo MS, Koornneef E. A review of COVID-19 mass testing in the United Arab Emirates. Front Public Health. 2021;12(9):661134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Home | UAE coronavirus (COVID-19) updates. https://covid19.ncema.gov.ae/en. Accessed 2024 Aug 14.
- 46.Al Marzouqi AM, Otim ME, Kehail LS, Kamal RA. Knowledge, attitudes, and practices of healthcare workers towards COVID-19 patients in the United Arab Emirates: a cross-sectional study. BMC Health Serv Res. 2023;23(1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paulo MS, Loney T, Lapão LV. The primary health care in the emirate of Abu Dhabi: are they aligned with the chronic care model elements? BMC Health Serv Res. 2017;17(1):725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fadl N, Al Awaidy ST, Elshabrawy A, et al. Determinants of parental seasonal influenza vaccine hesitancy in the Eastern Mediterranean region: a cross-sectional study. Front Public Health. 2023;28(11):1132798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Coronavirus (COVID-19), infection in pregnancy | RCOG. https://www.rcog.org.uk/guidance/coronavirus-covid-19-pregnancy-and-women-s-health/coronavirus-covid-19-infection-in-pregnancy/. Accessed 2024 Aug 14.
- 50.DeTora LM, Toroser D, Sykes A, et al. Good publication practice (GPP) guidelines for company-sponsored biomedical research: 2022 update. Ann Intern Med. 2022;175(9):1298–304. [DOI] [PubMed] [Google Scholar]
- 51.Emirates Hospitals Group. RSV vaccination in Dubai | RSV vaccination clinic near me. 2021. https://emirateshospitals.ae/services/family-medicine/adult-vaccinations-clinic/rsv-vaccination-clinic/. Accessed 2024 Sep 23.
- 52.Writing Committee Members, Virani SS, Newby LK, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology joint committee on clinical practice guidelines. J Am Coll Cardiol. 2023;82(9):833–955. [DOI] [PubMed] [Google Scholar]
- 53.McDonagh TA, Metra M, Adamo M, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24(1):4–131. [DOI] [PubMed] [Google Scholar]
- 54.Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology Clinical practice guideline for the diagnosis and management of nonalcoholic fatty liver disease in primary care and endocrinology clinical settings: co-sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract. 2022;28(5):528–62. [DOI] [PubMed] [Google Scholar]
- 55.ACIP vaccine recommendations and schedules | CDC. https://www.cdc.gov/acip/vaccine-recommendations/index.html. Accessed 2024 Aug 14.
- 56.Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68(6):e1-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vaccines for moderately to severely immunocompromised people | COVID-19 | CDC. https://www.cdc.gov/covid/vaccines/immunocompromised-people.html. Accessed 2024 Aug 14.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed.


