ABSTRACT
Objective
The purpose of this study is to better understand the prognostic implications for a patient's hospital course, chances for ventilator liberation and decannulation, functional status, and mortality based on the indication for tracheostomy.
Methods
A retrospective analysis was performed at a single tertiary‐care institution for 106 adult patients who underwent a tracheostomy from January 2022 to March 2023 and were followed for 6 months post‐tracheostomy placement. Demographics, clinical intervals, and clinical outcomes were compared based on the indication for tracheostomy: Airway Obstruction or Ventilator‐Dependent Respiratory Failure (VDRF).
Results
In the study group, 29 patients received a tracheostomy for airway obstruction, and 77 patients received a tracheostomy for VDRF. The VDRF group had more than three times longer hospital stays, more than three times the duration from first intubation to tracheostomy placement, six times the duration of mechanical ventilation post‐tracheostomy, and increased rates of hospital mortality (23.4% vs. 3.4%) and mortality at 6 months post‐tracheostomy placement (42.4% vs. 10.5%) compared to the Airway Obstruction group (p's < 0.05). The VDRF group was less likely to be discharged home (6.5% vs. 44.8%). At discharge, the majority of patients were liberated from mechanical ventilation (82.8%) and speaking (77.0%). Most surviving patients were not decannulated during their admission (65.5%). There were no significant differences in diet or time interval to decannulation.
Conclusion
Our analysis suggests that consideration of clinical indicators pertaining to tracheostomy placement may facilitate improved conversations with patients, families, and healthcare teams regarding the nuances of the functional and logistical course after receiving a tracheostomy.
Level of Evidence
3.
Keywords: decannulation, disposition, indication, tracheostomy
This study seeks to evaluate the prognostic significance of the initial indication for tracheostomy placement, airway obstruction versus ventilator‐dependent respiratory failure (VDRF), impacts the patient's hospital course, likelihood of ventilator weaning and tracheostomy tube removal, post‐discharge functional recovery, and overall mortality. We anticipate that the topics discussed in this paper should be of wide interest to those performing tracheostomies as well as caring for patients with tracheostomies following discharge. The VDRF group had more than three times longer hospital stays, more than three times the duration from first intubation to tracheostomy placement, six times the duration of mechanical ventilation post‐tracheostomy, and increased rates of hospital mortality and mortality at 6 months post‐tracheostomy placement.

1. Introduction
A tracheostomy is a common procedure performed in patients to exteriorize the trachea to the skin of the neck in order to bypass upper airway obstruction or to facilitate mechanical ventilation [1]. Although a tracheostomy is one of the most commonly performed surgical procedures in adults, with over 100,000 tracheostomies performed per year in the United States alone [2, 3], significant knowledge gaps persist regarding patient‐centered outcomes such as vocalization, oral intake, quality of life, and mortality [4]. The American Academy of Otolaryngology—Head and Neck Surgery Foundation created a 2013 Clinical Consensus Statement (CCS) regarding day‐to‐day tracheostomy care for both adult and pediatric patients [5]. Of the 77 statements that reached consensus, 13 statements were considered the most essential, of which the importance of providing comprehensive education to the patient and/or caregiver(s) both prior to performing a tracheostomy and prior to discharge was emphasized [5]. However, this requires an understanding of factors that may influence morbidity and mortality related to tracheostomy placement—a gap in the research emphasized by the 2013 CCS [5].
In order to provide a more comprehensive assessment of outcomes following tracheostomy placement, the Global Tracheostomy Collaborative (GTC) was formed in 2012 [4]. For adult patients undergoing first tracheostomy placement over an 8‐month period from 2018 to 2019 across six countries, the GTC found that among this cohort, 92% were admitted to the intensive care unit (ICU), resulting in a prolonged hospitalization of 34 days, with only 39% of patients being discharged home following their hospitalization [4]. Furthermore, the GTC found that increased length of stay and mortality following tracheostomy placement were associated with an increased number of medical comorbidities and if the tracheostomy placement was deemed emergent [4]. However, patients with head and neck cancer and upper airway obstruction were noted to have significantly decreased length of hospital stay and mortality [4]. Building off of these findings by the GTC, a multitude of studies have attempted to better predict outcomes following tracheostomy placement with increased age [6], unknown partner status [7], increased BMI [8], low Glasgow Coma Scores [6, 9], increased number of comorbidities/frailty [6, 7, 10], and the timing of decannulation [8] shown to be associated with either prolonged hospitalization or increased mortality.
While a multitude of studies have assessed factors related to the immediate postoperative outcomes following tracheostomy placement, fewer studies have assessed both patient‐ and caregiver‐specific quality of life outcomes. In a scoping review by Newman et al. assessing patient‐specific quality of life outcomes following tracheostomy placement, the importance of maintaining autonomy and establishing goals of care was emphasized, with voice restoration given the highest priority [11]. However, professional support in achieving these quality‐of‐life goals has been shown to be inadequate for both the patient and their caregivers [12].
In an effort to better align goals of care and provide more specific information to healthcare teams, patients, and families regarding the possible course following tracheostomy placement, we assessed the prognostic implications that the initial indication for tracheostomy placement has on a patient's hospital course, chances for ventilator liberation and tracheostomy tube removal, postdischarge functional status, and overall mortality.
2. Materials and Methods
2.1. Study Design
We performed a retrospective cohort study at a single tertiary‐care institution of adult patients who were treated in the ICU and underwent a tracheostomy between January 1, 2022, and March 31, 2023. Institutional Review Board approval was obtained (IRB # 0282‐23‐EP). An automated data pull combined with manual chart review was used to obtain patient characteristics and key hospital and postdischarge dates. A chart review was performed from the date of hospital admission resulting in tracheostomy placement until 6 months post‐tracheostomy placement. Inclusion criteria consisted of adults (≥ 19 years) who underwent tracheostomy. Patients were then manually stratified by indication for tracheostomy placement: coded as upper airway obstruction or a different condition resulting in ventilator‐dependent respiratory failure (VDRF). Patients were stratified into the Airway Obstruction group if the indication for tracheostomy included conditions such as head and neck cancer, bilateral vocal cord paralysis, subglottic stenosis, and angioedema. Patients were stratified into the VDRF group if the indication for tracheostomy included conditions such as shock, stroke, and encephalopathy, resulting in prolonged mechanical ventilation.
2.2. Patient Characteristics
Demographic variables collected included age at tracheostomy placement, sex, ethnicity, race, primary language spoken, and the distance of the patient's residence to the hospital in which the tracheostomy was performed. Social history included tobacco use, alcohol use, insurance status, and the patient's primary caregiver.
2.3. Hospital Course
The specialty of the provider performing the tracheostomy was collected. The following dates were collected: admission, first intubation prior to tracheostomy placement, tracheostomy placement, liberation from mechanical ventilation, decannulation, and discharge. These dates were used to determine the following intervals: hospital length of stay, first intubation to tracheostomy placement, tracheostomy placement to mechanical ventilator liberation, and tracheostomy placement to decannulation. If applicable, the deceased date was also collected and categorized as prior to discharge, death at ≤ 7 days, and ≤ 182 days (6 months) following tracheostomy placement. Patients who were lost to follow‐up before 7 days or 6 months had missing values for the 7‐day and 6‐month mortality variables, respectively. At discharge, information regarding oral intake status, vocalization status, mechanical ventilation requirements, decannulation status, and discharge disposition was collected; these variables were only documented for patients alive at discharge (except for disposition). For patients documented to be alive at 6 months and not lost to follow‐up, documentation of tracheostomy status was collected by indicating if they were still tracheostomy tube dependent, had been decannulated, or had a laryngectomy.
2.4. Statistical Analysis
Descriptive statistics for continuous data are given as medians and interquartile ranges (IQRs). Associations between categorical variables of interest and tracheostomy indication status were assessed using chi‐square tests, or Fisher's exact tests when expected cell counts were low. Wilcoxon rank‐sum tests were used to examine differences in distributions of numeric variables of interest between tracheostomy indication status groups. For significant chi‐square tests with variables having more than two groups, all possible 2 × 2 tables were run and assessed using chi‐square or Fisher's exact tests, and associated p‐values were Bonferroni adjusted to account for multiple comparisons. A p‐value < 0.05 was considered statistically significant. All analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC).
3. Results
3.1. Patient Characteristics
This study included 106 patients who underwent a tracheostomy, with 29 patients receiving a tracheostomy for airway obstruction and 77 patients receiving a tracheostomy for VDRF (Table 1). The median age of the patient cohort at tracheostomy placement was 61 years (IQR: 43, 68 years), with the majority of patients being non‐Hispanic (90.5%), white (68.9%), males (56.6%) who indicated that English was their primary spoken language (89.6%). The majority of patients indicated that they were not currently (36.7%) or did not use (36.7%) alcohol. Most patients indicated that they never smoked tobacco (43.0%) or were former smokers (40.0%). Furthermore, most patients never used smokeless tobacco (88.3%). The primary caregiver for the majority of patients was a relative or a friend (96.2%). Medicare was the most common insurance plan (34.0%). The median distance from the patient's residence to the hospital in which the tracheostomy was performed was 11.6 miles (IQR: 4.8, 47.1 miles). There were no significant differences between patient age at tracheostomy placement, gender, ethnicity, race, primary language, smoking status, smokeless tobacco use, alcohol, primary caregiver, medical insurance, and distance to the hospital between the Airway Obstruction and VDRF groups.
TABLE 1.
Characteristics of the patient cohort: Adults (≥ 19 years) undergoing a tracheostomy by indication.
| Airway | VDRF | Total | p | |
|---|---|---|---|---|
| (n = 29) | (n = 77) | (n = 106) | ||
| Age at tracheostomy placement, median (IQR) | 61.0 (54.0, 70.0) | 59.0 (42.0, 67.0) | 61.0 (43.0, 68.0) | 0.243 a |
| Sex, n (%) | 0.855 b | |||
| Female | 13 (44.8%) | 33 (42.9%) | 46 (43.4%) | |
| Male | 16 (55.2%) | 44 (57.1%) | 60 (56.6%) | |
| Ethnicity, n (%) | 0.278 c | |||
| Hispanic or Latino | 1 (3.4%) | 9 (11.8%) | 10 (9.5%) | |
| Not Hispanic or Latino | 28 (96.6%) | 67 (88.2%) | 95 (90.5%) | |
| Race, n (%) | 0.503 c | |||
| Black or African American | 2 (6.9%) | 12 (15.6%) | 14 (13.2%) | |
| Other | 6 (20.7%) | 13 (16.9%) | 19 (17.9%) | |
| White or Caucasian | 21 (72.4%) | 52 (67.5%) | 73 (68.9%) | |
| Language, n (%) | 0.224 c | |||
| English | 25 (86.2%) | 70 (90.9%) | 95 (89.6%) | |
| Other | 3 (10.3%) | 2 (2.6%) | 5 (4.7%) | |
| Spanish | 1 (3.4%) | 5 (6.5%) | 6 (5.7%) | |
| Smoking, n (%) | 0.094 c | |||
| Former | 16 (57.1%) | 24 (33.3%) | 40 (40.0%) | |
| Never | 8 (28.6%) | 35 (48.6%) | 43 (43.0%) | |
| Yes | 4 (14.3%) | 13 (18.1%) | 17 (17.0%) | |
| Smokeless tobacco, n (%) | 0.729 c | |||
| Current | 1 (3.6%) | 1 (1.5%) | 2 (2.1%) | |
| Former | 2 (7.1%) | 7 (10.6%) | 9 (9.6%) | |
| Never | 25 (89.3%) | 58 (87.9%) | 83 (88.3%) | |
| Alcohol, n (%) | 0.846 b | |||
| No | 10 (40.0%) | 23 (35.4%) | 33 (36.7%) | |
| Not currently | 8 (32.0%) | 25 (38.5%) | 33 (36.7%) | |
| Yes | 7 (28.0%) | 17 (26.2%) | 24 (26.7%) | |
| Caregiver | 1.000 c | |||
| Facility | 1 (3.4%) | 3 (4.0%) | 4 (3.8%) | |
| Relative/friends | 28 (96.6%) | 72 (96.0%) | 100 (96.2%) | |
| Insurance status, n (%) | 0.473 c | |||
| Medicaid | 3 (10.3%) | 4 (5.2%) | 7 (6.6%) | |
| Medicare | 8 (27.6%) | 28 (36.4%) | 36 (34.0%) | |
| Military | 1 (3.4%) | 4 (5.2%) | 5 (4.7%) | |
| Other government | 4 (13.8%) | 17 (22.1%) | 21 (19.8%) | |
| Private | 9 (31.0%) | 20 (26.0%) | 29 (27.4%) | |
| Uninsured | 4 (13.8%) | 4 (5.2%) | 8 (7.5%) | |
| Distance to hospital, median (IQR) | 18.6 (4.8, 48.4) | 11.0 (5.0, 46.8) | 11.6 (4.8, 47.1) | 0.924 a |
Abbreviation: IQR = interquartile range.
Wilcoxon rank‐sum p‐value.
Chi‐square p‐value.
Fisher's exact p‐value.
3.2. Hospital Course
The median hospital stay for all patients was 32.0 days (IQR: 18.0, 55.0 days). The Airway Obstruction group had a significantly shorter median hospital stay of 11.0 days (IQR: 7.0, 19.0 days) compared to the VDRF group's median hospital stay of 38.0 days (IQR: 27.0, 72.0 days; p < 0.001; Figure 1). The median time from the date of the first intubation to the date of the tracheostomy placement was 12.0 days (IQR: 8.0, 17.0 days). Excluding patients who underwent a local or scheduled tracheostomy without ventilator dependence prior to the procedure (n = 19), the time from the first intubation to tracheostomy placement was significantly shorter for the remaining 10 patients in the Airway Obstruction group (3.5 days; IQR: 2.0, 4.0 days) compared to the VDRF group (13.0 days; IQR: 10.0, 17.0 days; p = 0.002). The majority of patients had their tracheostomy performed by an otolaryngologist (84.9%), with no significant differences between the two groups regarding the specialty of the provider who performed the tracheostomy.
FIGURE 1.

Hospital course based on indication for tracheostomy. Dispositional differences were significant for hospital length of stay, intubation to tracheostomy placement, and tracheostomy placement to ventilator liberation via Wilcoxon rank‐sum p‐value (p's < 0.05).
Following tracheostomy placement, the median time from tracheostomy placement to mechanical ventilator liberation was 4.0 days (IQR: 2.0, 11.0 days), and the median time from tracheostomy placement to decannulation was 44.5 days (IQR: 21.5, 91.5 days). The time from tracheostomy placement to mechanical ventilator liberation was significantly shorter for the Airway Obstruction group (1.0 days; IQR: 1.0, 2.0 days) compared to the VDRF group (6.0 days; IQR: 3.0, 16.5 days; p < 0.001). However, there was no significant difference between the median time from tracheostomy placement to decannulation for the Airway Obstruction and VDRF groups.
3.3. Discharge
At the time of discharge, the majority of patients were not on mechanical ventilation (82.8%) and were effectively vocalizing (77.0%; Table 2). However, most were not tolerating oral intake (51.7%) and were deemed strictly nothing by mouth (NPO) at discharge. The majority of patients were not decannulated at discharge (65.5%). Of the patients alive at discharge, all who received a tracheostomy for airway obstruction were liberated from mechanical ventilation (100.0%). This was significantly greater than the 74.6% of patients who were liberated from mechanical ventilation in the VDRF group (p = 0.002). However, there were no significant differences between the Airway Obstruction or the VDRF groups in the percentages of patients tolerating PO intake, speaking, or being decannulated at discharge.
TABLE 2.
Discharge functional status. Excludes 19 total patients who died during hospitalization (1 patient in the Airway Obstruction group, 18 patients in the VDRF group).
| Airway (n = 28) | VDRF (n = 59) | Total (n = 87) | p | |
|---|---|---|---|---|
| Mechanical ventilation at discharge | 28 (100%) | 44 (74.6%) | 72 (82.8%) | 0.002 a |
| Speaking on discharge (Y), n (%) | 25 (89.3%) | 42 (71.2%) | 67 (77.0%) | 0.100 a |
| PO on discharge (Y), n (%) | 15 (53.6%) | 27 (45.8%) | 42 (48.3%) | 0.496 b |
| PO status, n (%) | 0.147 a | |||
| NPO at discharge | 13 (46.4%) | 32 (54.2%) | 45 (51.7%) | |
| PO with PEG at discharge | 3 (10.7%) | 13 (22.0%) | 16 (18.4%) | |
| PO without PEG at discharge | 12 (42.9%) | 14 (23.7%) | 26 (29.9%) | |
| Decannulated at discharge (Y), n (%) | 6 (21.4%) | 24 (40.7%) | 30 (34.5%) | 0.078 b |
Abbreviations: NPO = nothing per mouth; PEG = percutaneous endoscopic gastrostomy tube; PO = per mouth.
Fisher's exact p‐value.
Chi‐square p‐value.
The minority of patients were discharged to a home (17.0%), with the majority being discharged to a facility (61.3%). However, there were significant differences in discharge disposition between the Airway Obstruction and VDRF groups (p < 0.001). Patients in the VDRF group were significantly more likely to be discharged to a facility (66.2%), with only 6.5% discharged home, in comparison to the Airway Obstruction group, where 44.8% were discharged home and 48.3% were discharged to a facility (p < 0.001; Figure 2). Out of patients who were alive and had follow‐up data at 6 months, the majority were decannulated (75.4%). However, tracheostomy status at 6 months significantly differed between the two groups (p < 0.001). Patients alive at 6 months in the VDRF group were significantly more likely to be decannulated at 6 months (89.5%) with 10.5% tracheostomy dependent in comparison to the Airway Obstruction group, where 42.1% were tracheostomy dependent at 6 months and 47.4% were decannulated at 6 months (p < 0.01; Table 3).
FIGURE 2.
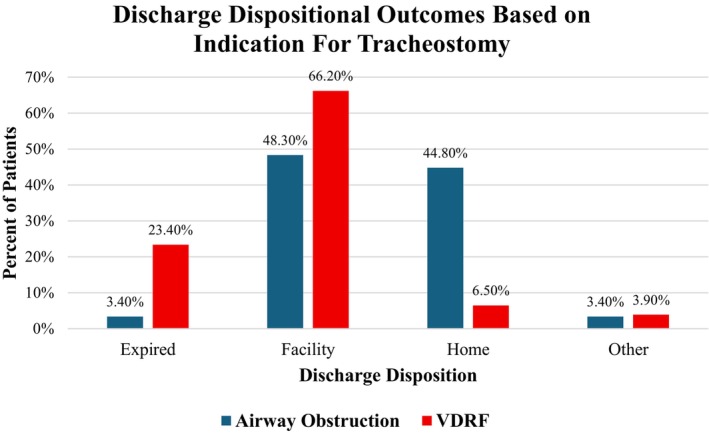
Discharge dispositional outcomes based on indication for tracheostomy. Dispositional differences were significant via Fisher's exact p‐value.
TABLE 3.
Outcomes for patients with documentation of being alive 6 months post‐tracheostomy placement. Excludes deceased patients. Ten patients from the Airway Obstruction group and 39 patients from the VDRF group were lost to follow‐up at 6 months post‐tracheostomy.
| Airway (n = 19) | VDRF (n = 38) | Total (n = 57) | p | |
|---|---|---|---|---|
| Decannulated | 9 (47.4%) | 34 (89.5%) | 43 (75.4%) | < 0.001 a |
| Laryngectomy | 2 (10.5%) | 0 (0.0%) | 2 (3.5%) | |
| Tracheostomy dependent | 8 (42.1%) | 4 (10.5%) | 12 (21.1%) |
Fisher's exact p‐value.
3.4. Mortality
Following tracheostomy, 17.8% of all patients died during their hospitalization stay, with 3.8% of patients dying within 7 days of placement and 35.3% of patients dying within 6 months. While the percentage of deceased patients at 7 days post‐tracheostomy placement was not significantly different between the two groups, the Airway Obstruction group was significantly less likely to have died during the hospital stay (3.4%) compared to the VDRF group (23.4%; p = 0.021; Figure 3). Furthermore, the Airway Obstruction group was significantly less likely to have died within 6 months of tracheostomy placement (10.5%) compared to the VDRF group (42.4%; p = 0.013).
FIGURE 3.

Mortality during hospitalization, 7 days post‐tracheostomy, and 6 months (182 days) post‐tracheostomy. Hospital stay: Airway Obstruction n = 29; VDRF = 77; total = 106. Seven days post‐tracheostomy: Airway Obstruction n = 28; VDRF = 77; total = 105. Six months post‐tracheostomy: Airway Obstruction n = 19; VDRF n = 66; total n = 85. Differences between death during hospital stay and within 6 months between the Airway Obstruction and VDRF groups were statistically significant according to Fisher's exact p‐value (p's < 0.05).
4. Discussion
In an effort to better characterize differences in the hospital course and outcomes following tracheostomy placement, we categorized patients based on the indication for tracheostomy placement: Airway Obstruction and VDRF. In comparing hospital courses between the two groups, patients who received a tracheostomy for VDRF had more than triple the length of hospital stay, more than triple the time from first intubation to tracheostomy placement, and six times the duration from tracheostomy placement to mechanical ventilator liberation. At discharge, the VDRF group was significantly more likely to require mechanical ventilation. However, there were no significant differences in patients tolerating oral intake, vocalizing, or being decannulated at discharge between the two groups. Upon discharge, only 6.5% of patients in the VDRF group were discharged home. Patients who received a tracheostomy for VDRF were significantly more likely to die during their hospitalization or die within 6 months of tracheostomy placement, with only 57.6% documented to be alive 6 months post‐tracheostomy (among patients who had follow‐up of at least 6 months). For patients with follow‐up of at least 6 months, 42.1% of patients in the Airway Obstruction group remained tracheostomy dependent compared to 10.5% of patients in the VDRF group.
Nearly half of the patients who received a tracheostomy for airway obstruction were discharged home compared to only 6.5% of patients who received a tracheostomy for VDRF. Although the GCS found that only 39% of patients who received a tracheostomy were discharged home [4], our findings predict significantly different dispositional outcomes based on the indication for tracheostomy placement. This difference in discharge disposition outcomes is especially important given the value patients place on autonomy following tracheostomy placement [11]. Additionally, while the majority of our cohort were speaking on discharge, a functional outcome of utmost importance to patients undergoing a tracheostomy [11], nearly a quarter of our patient cohort were unable to vocalize by the time of discharge, regardless of the indication for tracheostomy placement. The use of dedicated interprofessional tracheostomy teams, shown to significantly increase speaking valve use following tracheostomy placement [13], can help patients meet their voicing goals regardless of the indication for tracheostomy. However, challenges reaching discharge dispositional goals remain, with Abril et al. finding a significant increase in the proportion of patients being discharged to intermediate care facilities following tracheostomy from 2002 to 2017 [2]. With the CCS emphasizing the importance of providing comprehensive patient education prior to performing a tracheostomy [5], our results suggest the importance of considering the indication for tracheostomy prior to counseling patients in order to effectively advise patients on where they might be living after discharge and the likelihood of speaking and eating by mouth following the procedure.
Almost a quarter of patients who received a tracheostomy for VDRF died during their hospital stay. This is in contrast to the one patient (3.4%) who underwent a tracheostomy for airway obstruction and expired before discharge. Furthermore, for patients with documentation at an interval of 6 months, over a third died within 6 months of undergoing a tracheostomy, 93.3% of which were from the VDRF group. Patients within our VDRF group undoubtedly had an increased number of comorbidities and elevated frailty scores, both of which have been associated with worsening mortality following tracheostomy placement [7, 10]. The proportion of patients undergoing a tracheostomy for VDRF is not only increasing in the United States [14], but the risk for mortality among this cohort has also proportionally increased [2]. Furthermore, recent studies have advocated for earlier tracheostomy placement in an effort to decrease rates of mortality [15], ventilator‐associated pneumonia [16], duration of mechanical ventilation [16], and lengths of ICU stays [15, 17]. Despite the purported benefits of early tracheostomy placement for patients in the ICU, concerns arise regarding the current process for determining tracheostomy candidacy and the need for pre‐tracheostomy multidisciplinary teams to improve patient selection [18]. The recent increase in the proportion of patients undergoing tracheostomy for VDRF illustrates the need to not only better educate patients and caregivers regarding expected mortality following tracheostomy placement in the context of a critical illness but also suggests the need to establish a multidisciplinary approach to align patients goals of care in the context of the circumstances prompting the discussion of tracheostomy placement.
Almost two‐thirds of our patient cohort remained tracheostomy dependent at discharge. Furthermore, of the patients documented to be alive at 6 months, nearly a quarter of our patient cohort remained tracheostomy dependent or underwent laryngectomy. While the implementation of multidisciplinary tracheostomy teams has been shown to significantly improve the rates of decannulation [13, 19, 20], a significant portion of patients who are discharged with a tracheostomy are left feeling unsupported, unprepared, and overwhelmed with the task of providing appropriate tracheostomy care [12]. Despite similar rates of patients being decannulated at discharge between both groups, the significant number of patients remaining tracheostomy or laryngectomy tube dependent at 6 months within our Airway Obstruction group highlights the need for improved counseling when setting appropriate expectations for the probability of decannulation based on the indication for tracheostomy placement.
This study highlights several differences in the hospital course and functional outcomes following tracheostomy placement for airway obstruction or VDRF. Otolaryngologists are significantly more likely to be consulted to perform tracheostomies for medically complex patient populations with airway obstruction compared to other surgical specialties [21]. Despite the familiarity otolaryngologists have with providing post‐tracheostomy care for patients with airway obstruction [21], this patient population is still left feeling misinformed and unprepared about the prognostic implications of receiving a tracheostomy [22]. This sentiment extends beyond just this airway obstruction patient population and is pervasive among all tracheostomized patients and their caregivers [12, 23]. Furthermore, while much of the current research regarding patient‐centered outcomes following tracheostomy placement focuses on the tertiary care hospital setting, there is limited attention to the management of tracheostomized patients without access to specialized, multidisciplinary care [24]. By highlighting the prognostic differences between these two distinct patient populations within the present study, we aim to equip patients with an improved knowledge and understanding of what to expect following tracheostomy placement.
These findings should be interpreted with the understanding of the limitations of our study being a single‐institution retrospective analysis. Many variables were not listed discretely and required manual chart review. Documentation within the electronic medical records can be vague and inconsistent and can traverse multiple health systems that were not readily accessible during the chart review process. The majority (n = 19) of the Airway Obstruction group underwent a local or scheduled tracheostomy and were subsequently not intubated prior to tracheostomy placement, potentially illustrating differences in acuity and severity of airway obstruction necessitating tracheostomy placement within the Airway Obstruction group. Subsequently, comparisons with the VDRF group between time from first intubation to tracheostomy placement should be interpreted with caution. With 49 patients from our cohort lost to follow‐up 6 months from tracheostomy placement, the postdischarge outcomes of our patient cohort with documented follow‐up by 6 months should be interpreted with caution, as this population could differ from those lost to follow‐up. Furthermore, the sample size of patients undergoing a tracheostomy for airway obstruction within our patient cohort was limited to 29 patients. Moreover, due to our small patient cohort, we are unable to statistically account for further potential confounders such as the diversity of comorbidities or severity of illness within our patient cohort.
5. Conclusion
Our study illustrates similarities and differences in hospital courses, functional outcomes, and mortality for adult patients based on the indication for tracheostomy placement. With longer hospital stays, prolonged intubation, increased mechanical ventilator dependence, decreased likelihood of being discharged home, and increased rates of mortality within 6 months of tracheostomy placement for patients with VDRF, our findings indicate a need to stratify patients by indication before providing informed consent to patients and caregivers. Furthermore, with a substantial portion of patients requiring a tracheostomy tube at discharge, improved patient and caregiver education regarding expectations for daily tracheostomy care is necessary. Further studies stratifying indications for tracheostomy placement, incorporating standardized frailty metrics, and assessing the efficacy of pre‐tracheostomy conferences in improving both patient selection and expectations are necessary.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
All authors aided in the data acquisition, data analysis, manuscript writing, and manuscript revisions. All contributors are listed as authors.
Higgins R. C., Samson K., Works D., and Dowdall J. R., “The Impact of Tracheostomy Indication on Patient Outcomes and Hospital Course,” Laryngoscope Investigative Otolaryngology 10, no. 4 (2025): e70210, 10.1002/lio2.70210.
Funding: The authors received no specific funding for this work.
This study was presented at the Triological Society, 2025 Combined Sections Meeting, Triological Society Paper: 5163, Orlando, Florida, USA, January 23, 2025—January 25, 2025.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- 1. Cheung N. H. and Napolitano L. M., “Tracheostomy: Epidemiology, Indications, Timing, Technique, and Outcomes Discussion,” Respiratory Care 59, no. 6 (2014): 895–919. [DOI] [PubMed] [Google Scholar]
- 2. Abril M. K., Berkowitz D. M., Chen Y., Waller L. A., Martin G. S., and Kempker J. A., “The Epidemiology of Adult Tracheostomy in the United States 2002–2017: A Serial Cross‐Sectional Study,” Critical Care Explorations 3, no. 9 (2021): e0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehta A. B., Syeda S. N., Bajpayee L., Cooke C. R., Walkey A. J., and Wiener R. S., “Trends in Tracheostomy for Mechanically Ventilated Patients in the United States, 1993–2012,” American Journal of Respiratory and Critical Care Medicine 192, no. 4 (2015): 446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brenner M. J., Pandian V., Milliren C. E., et al., “Global Tracheostomy Collaborative: Data‐Driven Improvements in Patient Safety Through Multidisciplinary Teamwork, Standardisation, Education, and Patient Partnership,” British Journal of Anaesthesia 125, no. 1 (2020): e104–e118. [DOI] [PubMed] [Google Scholar]
- 5. Mitchell R. B., Hussey H. M., Setzen G., et al., “Clinical Consensus Statement: Tracheostomy Care,” Otolaryngology‐Head and Neck Surgery 148, no. 1 (2013): 6–20. [DOI] [PubMed] [Google Scholar]
- 6. Alhashemi H., Algarni M., Al‐Hakami H., et al., “An Interdisciplinary Approach to the Management of Individuals With Tracheostomy,” Respiratory Care 67, no. 1 (2022): 34–39. [DOI] [PubMed] [Google Scholar]
- 7. Park C., Bahethi R., Yang A., Gray M., Wong K., and Courey M., “Effect of Patient Demographics and Tracheostomy Timing and Technique on Patient Survival,” Laryngoscope 131, no. 7 (2021): 1468–1473. [DOI] [PubMed] [Google Scholar]
- 8. Martinez G. H., Fernandez R., Casado M. S., et al., “Tracheostomy Tube in Place at Intensive Care Unit Discharge is Associated With Increased Ward Mortality,” Respiratory Care 54, no. 12 (2009): 1644–1652. [PubMed] [Google Scholar]
- 9. Mpe M. J. and Mphahlele B. V., “In‐Hospital Outcome of Patients Discharged From the ICU With Tracheostomies,” South African Medical Journal 95, no. 3 (2005): 184–186. [PubMed] [Google Scholar]
- 10. Fernando S. M., McIsaac D. I., Rochwerg B., et al., “Frailty and Invasive Mechanical Ventilation: Association With Outcomes, Extubation Failure, and Tracheostomy,” Intensive Care Medicine 45, no. 12 (2019): 1742–1752. [DOI] [PubMed] [Google Scholar]
- 11. Newman H., Clunie G., Wallace S., Smith C., Martin D., and Pattison N., “What Matters Most to Adults With a Tracheostomy in ICU and the Implications for Clinical Practice: A Qualitative Systematic Review and Metasynthesis,” Journal of Critical Care 72 (2022): 154145. [DOI] [PubMed] [Google Scholar]
- 12. Nakarada‐Kordic I., Patterson N., Wrapson J., and Reay S. D., “A Systematic Review of Patient and Caregiver Experiences With a Tracheostomy,” Patient 11, no. 2 (2018): 175–191. [DOI] [PubMed] [Google Scholar]
- 13. Ninan A., Grubb L. M., Brenner M. J., and Pandian V., “Effectiveness of Interprofessional Tracheostomy Teams: A Systematic Review,” Journal of Clinical Nursing 32, no. 19–20 (2023): 6967–6986. [DOI] [PubMed] [Google Scholar]
- 14. Mehta M. M., Garg R. K., Rizvi I., et al., “The Multiple Cranial Nerve Palsies: A Prospective Observational Study,” Neurology India 68, no. 3 (2020): 630–635, 10.4103/0028-3886.289003. [DOI] [PubMed] [Google Scholar]
- 15. Patel A. M., Patel R., Revercomb L., et al., “Association of Early Tracheostomy With Length of Stay and Mortality in Critically Ill Patients,” Journal of Laryngology and Otology 138, no. 9 (2024): 921–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chorath K., Hoang A., Rajasekaran K., and Moreira A., “Association of Early Vs Late Tracheostomy Placement With Pneumonia and Ventilator Days in Critically Ill Patients: A Meta‐Analysis,” JAMA Otolaryngology. Head & Neck Surgery 147, no. 5 (2021): 450–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu C. C., Livingstone D., Dixon E., and Dort J. C., “Early Versus Late Tracheostomy: A Systematic Review and Meta‐Analysis,” Otolaryngology‐Head and Neck Surgery 152, no. 2 (2015): 219–227. [DOI] [PubMed] [Google Scholar]
- 18. Raynor T., Marcet‐Gonzalez J., Roy K., et al., “Development and Implementation of a Pre‐Tracheostomy Multidisciplinary Conference: An Initiative to Improve Patient Selection,” International Journal of Pediatric Otorhinolaryngology 158 (2022): 111135. [DOI] [PubMed] [Google Scholar]
- 19. Mah J. W., Staff I. I., Fisher S. R., and Butler K. L., “Improving Decannulation and Swallowing Function: A Comprehensive, Multidisciplinary Approach to Post‐Tracheostomy Care,” Respiratory Care 62, no. 2 (2016): 137–143. [DOI] [PubMed] [Google Scholar]
- 20. Mussa C. C., Gomaa D., Rowley D. D., Schmidt U., Ginier E., and Strickland S. L., “AARC Clinical Practice Guideline: Management of Adult Patients With Tracheostomy in the Acute Care Setting,” Respiratory Care 66, no. 1 (2021): 156–169. [DOI] [PubMed] [Google Scholar]
- 21. Alfonso K. P., Kaufman M. R., Dressler E. V., Liu M., and Aouad R. K., “Otolaryngology Consultation Tracheostomies and Complex Patient Population,” American Journal of Otolaryngology 38, no. 5 (2017): 551–555. [DOI] [PubMed] [Google Scholar]
- 22. Rogers S. N., Russell L., and Lowe D., “Patients' Experience of Temporary Tracheostomy After Microvascular Reconstruction for Cancer of the Head and Neck,” British Journal of Oral and Maxillofacial Surgery 55, no. 1 (2017): 10–16. [DOI] [PubMed] [Google Scholar]
- 23. McCormick M. E., Ward E., Roberson D. W., Shah R. K., Stachler R. J., and Brenner M. J., “Life After Tracheostomy: Patient and Family Perspectives on Teaching, Transitions, and Multidisciplinary Teams,” Otolaryngology‐Head and Neck Surgery 153, no. 6 (2015): 914–920. [DOI] [PubMed] [Google Scholar]
- 24. Paul F., “Tracheostomy Care and Management in General Wards and Community Settings: Literature Review,” Nursing in Critical Care 15, no. 2 (2010): 76–85. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


