Abstract
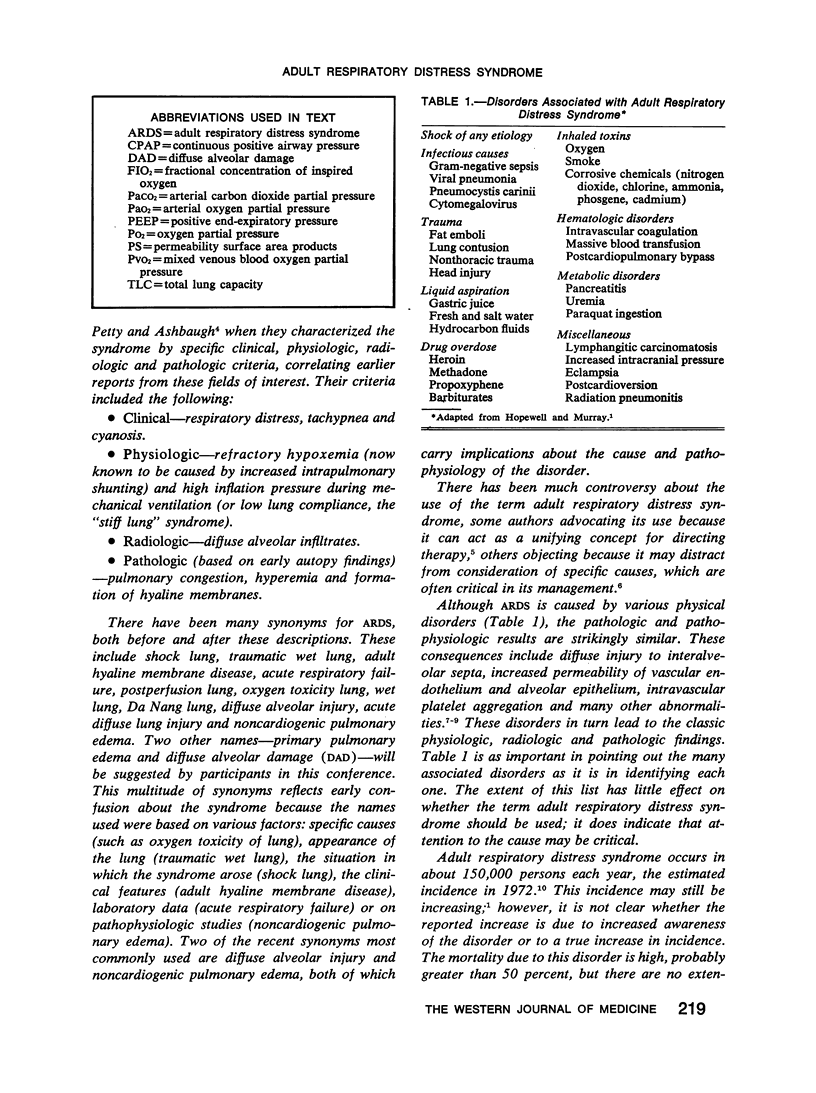
Many causes for the adult respiratory distress syndrome (ARDS) have been reported, all with common pathologic, pathophysiologic and biochemical end results. The final common pathway may involve changes in lung content of a critical enzyme, superoxide dismutase, or alterations in surfactant metabolism, or both. The early assumption that the disorder is partially due to oxygen toxicity from inspired oxygen concentrations greater than 60 percent is consistent with findings of recent biochemical studies. Although the lung normally maintains its alveoli dry, during ARDS increased permeability of small pulmonary vessels results in primary pulmonary edema, in contrast to edema from increased vascular pressure. These data have been obtained mainly in animals; whether they apply to humans with ARDS is not certain. Tissue oxygenation is improved by increasing end-expiratory pressure in an animal model of ARDS, more effectively during spontaneous breathing than during mechanical ventilation. During spontaneous breathing, adverse ventilatory effects were caused by stimulation of pulmonary reflexes.
Full text
PDF