Abstract
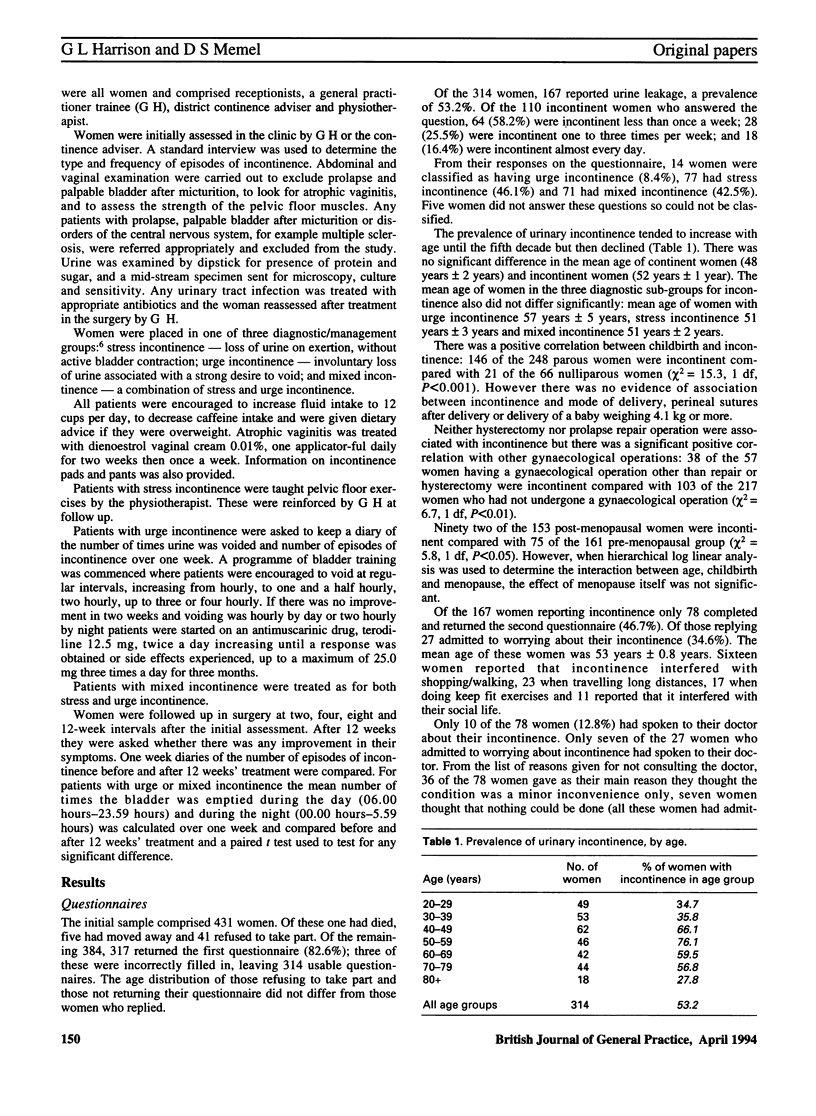
BACKGROUND. It has been suggested that regular clinics might improve the management of urinary incontinence in general practice. AIM. A study was undertaken to determine the prevalence of urinary incontinence among women in one general practice and the feasibility of using a health promotion clinic in its management. METHOD. Questionnaires were sent to a 10% sample of women aged 20 years and over on the practice register. Pregnant women were excluded. RESULTS. Of 384 questionnaires sent to eligible women, 314 were completed correctly (82%). The overall reported prevalence of urinary incontinence was 53%; 8% of these women had urge incontinence, 46% had stress incontinence and 43% had mixed incontinence. Incontinence was positively correlated with parity and with gynaecological operation other than hysterectomy and repair of prolapse but not with perineal suturing after childbirth, delivery of a baby weighing 9 lb (4.1 kg) or more or mode of delivery. Twenty seven out of 78 incontinent women (35%) who completed a second questionnaire admitted to worrying about their incontinence but only 10 (13%) had consulted their doctor about the problem. The main reason given for not consulting was that incontinence was a minor inconvenience only. The 167 incontinent women were offered an appointment at a women's clinic but only 13 attended. Of these, 10 were entered into a 12 week treatment trial. Various treatments were offered, such as the women being taught bladder training and pelvic floor exercises. One woman was lost to follow up, and for eight out of nine women their continence had improved, both subjectively and objectively. CONCLUSION. Urinary incontinence in women is a common problem. It can be successfully diagnosed and treated in general practice but low attendance makes the health promotion clinic setting an inefficient means of achieving this.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brocklehurst J. C. Urinary incontinence in the community--analysis of a MORI poll. BMJ. 1993 Mar 27;306(6881):832–834. doi: 10.1136/bmj.306.6881.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FRANCIS W. J. Disturbances of bladder function in relation to pregnancy. J Obstet Gynaecol Br Emp. 1960 Jun;67:353–366. doi: 10.1111/j.1471-0528.1960.tb07013.x. [DOI] [PubMed] [Google Scholar]
- Holst K., Wilson P. D. The prevalence of female urinary incontinence and reasons for not seeking treatment. N Z Med J. 1988 Nov 9;101(857):756–758. [PubMed] [Google Scholar]
- Jolleys J. V. Diagnosis and management of female urinary incontinence in general practice. J R Coll Gen Pract. 1989 Jul;39(324):277–279. [PMC free article] [PubMed] [Google Scholar]
- Jolleys J. V. Reported prevalence of urinary incontinence in women in a general practice. Br Med J (Clin Res Ed) 1988 May 7;296(6632):1300–1302. doi: 10.1136/bmj.296.6632.1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagro-Janssen T. L., Smits A. J., Van Weel C. Women with urinary incontinence: self-perceived worries and general practitioners' knowledge of problem. Br J Gen Pract. 1990 Aug;40(337):331–334. [PMC free article] [PubMed] [Google Scholar]
- Snooks S. J., Setchell M., Swash M., Henry M. M. Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet. 1984 Sep 8;2(8402):546–550. doi: 10.1016/s0140-6736(84)90766-9. [DOI] [PubMed] [Google Scholar]
- Stanton S. L., Kerr-Wilson R., Harris V. G. The incidence of urological symptoms in normal pregnancy. Br J Obstet Gynaecol. 1980 Oct;87(10):897–900. doi: 10.1111/j.1471-0528.1980.tb04444.x. [DOI] [PubMed] [Google Scholar]
- Williams D. R., Munroe C., Hospedales C. J., Greenwood R. H. A three-year evaluation of the quality of diabetes care in the Norwich community care scheme. Diabet Med. 1990 Jan;7(1):74–79. doi: 10.1111/j.1464-5491.1990.tb01312.x. [DOI] [PubMed] [Google Scholar]


