Abstract
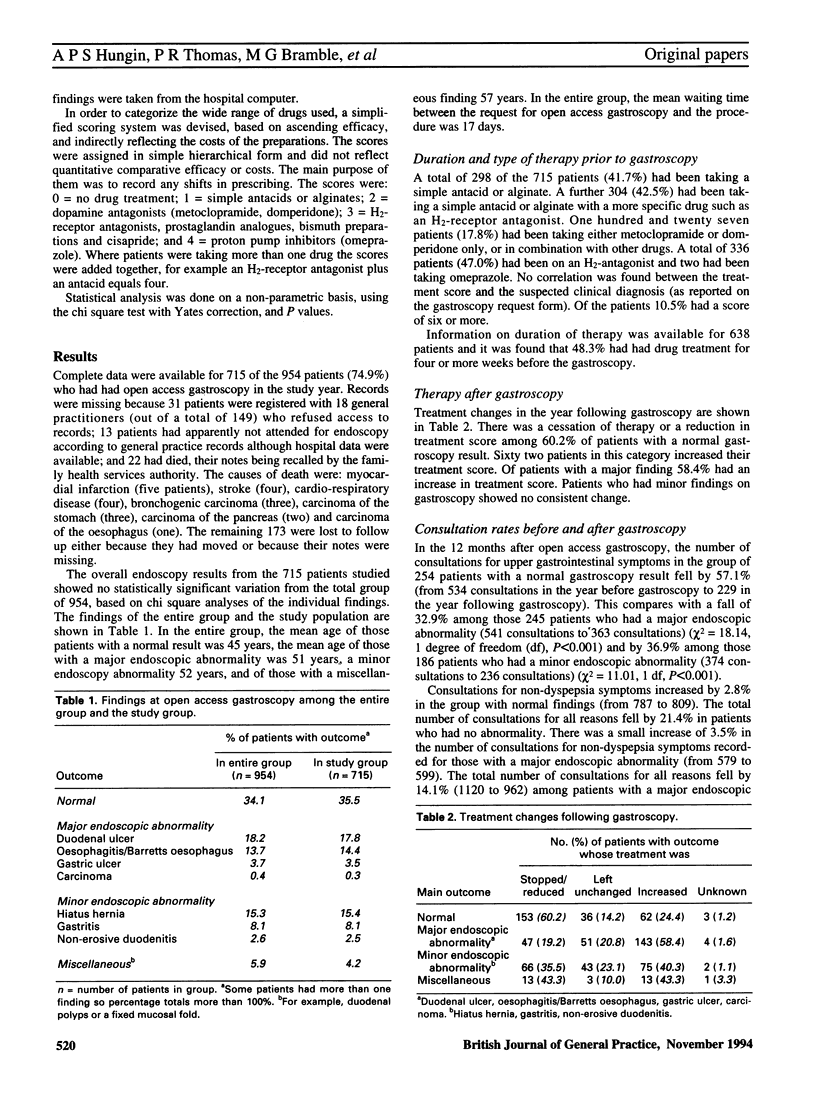
BACKGROUND. Open access gastroscopy allows general practitioners to request a gastroscopy without prior referral to a specialist. The effect of open access gastroscopy upon patient management is poorly explored. Most studies have been hospital based and have focused on diagnostic yields and on means of tightening requests to reduce inefficient use. A user evaluation can only be made by measuring outcomes in primary care. AIM. A study was undertaken to determine the impact of open access gastroscopy in general practice and in particular, the value of a normal result. METHOD. All general practices in South Tees District Health Authority were asked to participate. Any of their patients who had had open access gastroscopy in the year prior to July 1990 were identified from the hospital computer and their general practitioner notes examined. Patient management during the year prior to the open access gastroscopy was compared with the year after. The main outcome measures were: detection rate and grade of lesion, change in graded score of prescribed drugs, consultation rate for dyspepsia and non-dyspepsia problems, and further hospital referral and investigations. Outcomes among those with normal and abnormal gastroscopy results were compared. RESULTS. The study sample comprised 715 patients, 36% of whom had a normal gastroscopy result, 34% a major abnormality and 26% a minor abnormality (4% of patients had miscellaneous diagnoses). It was found that 39% of all patients, and 60% of those with normal findings on open access gastroscopy had their drug treatment stopped or reduced in grade after the investigation. Of those with a major endoscopic abnormality 58% increased their treatment score. Consultations for dyspepsia in the year before and after gastroscopy fell by 57% overall among those with a normal gastroscopy result, by 37% among those with a minor finding and by 33% in those with a major finding. There was a 21% fall in consultations for all reasons among those with a normal gastroscopy result but those with a minor abnormality had a 23% increase in non-dyspepsia consultations. Of all patients 19% were referred to hospital subsequently. CONCLUSION. Open access gastroscopy has a major effect upon patient management in general practice, and a normal endoscopy result has an important an impact as an abnormal one. Open access gastroscopy is associated with a rationalization of drug therapy, reduced consultations and a low hospital referral rate.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bramble M. G., Cooke W. M., Corbett W. A., Cann P. A., Clarke D., Contractor B., Hungin A. S. Organising unrestricted open access gastroscopy in South Tees. Gut. 1993 Mar;34(3):422–427. doi: 10.1136/gut.34.3.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gear M. W., Wilkinson S. P. Open-access upper alimentary endoscopy. Br J Hosp Med. 1989 May;41(5):438, 440, 442-4. [PubMed] [Google Scholar]
- Hansen J. M., Bytzer P., Bondesen S., Schaffalitzky de Muckadell O. B. Efficacy and outcome of an open access endoscopy service. Dan Med Bull. 1991 Jun;38(3):288–290. [PubMed] [Google Scholar]
- Holdstock G., Wiseman M., Loehry C. A. Open-access endoscopy service for general practitioners. Br Med J. 1979 Feb 17;1(6161):457–459. doi: 10.1136/bmj.1.6161.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hungin A. S. Use of an open-access gastroscopy service by a general practice: findings and subsequent specialist referral rate. J R Coll Gen Pract. 1987 Apr;37(297):170–171. [PMC free article] [PubMed] [Google Scholar]
- Jones R. H., Lydeard S. E., Hobbs F. D., Kenkre J. E., Williams E. I., Jones S. J., Repper J. A., Caldow J. L., Dunwoodie W. M., Bottomley J. M. Dyspepsia in England and Scotland. Gut. 1990 Apr;31(4):401–405. doi: 10.1136/gut.31.4.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. What happens to patients with non-ulcer dyspepsia after endoscopy? Practitioner. 1988 Jan;232(1441):75-6, 78. [PubMed] [Google Scholar]
- MacIntyre I. M. Open-access endoscopy for general practitioners. Practitioner. 1988 Mar 22;232(1445):348–351. [PubMed] [Google Scholar]
- Mann J., Holdstock G., Harman M., Machin D., Loehry C. A. Scoring system to improve cost effectiveness of open access endoscopy. Br Med J (Clin Res Ed) 1983 Oct 1;287(6397):937–940. doi: 10.1136/bmj.287.6397.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy M. Somatisation: embodying the problem. BMJ. 1989 May 20;298(6684):1331–1332. doi: 10.1136/bmj.298.6684.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]


