Abstract
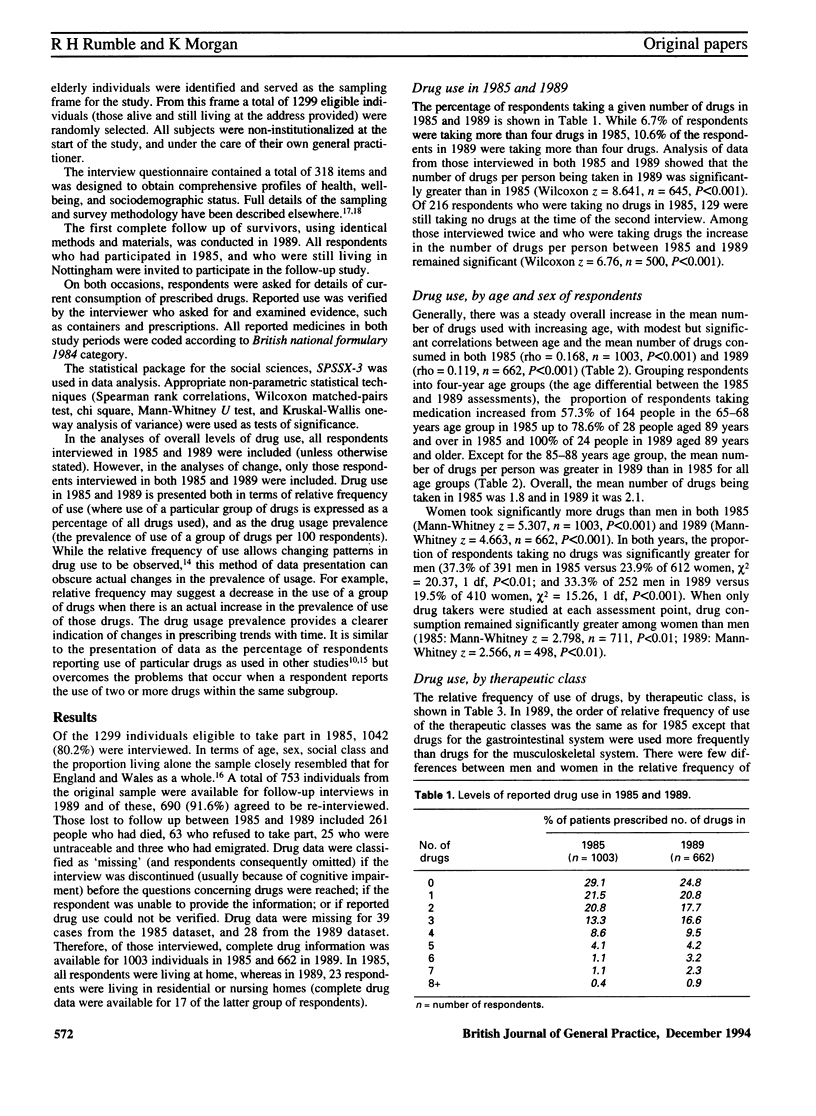
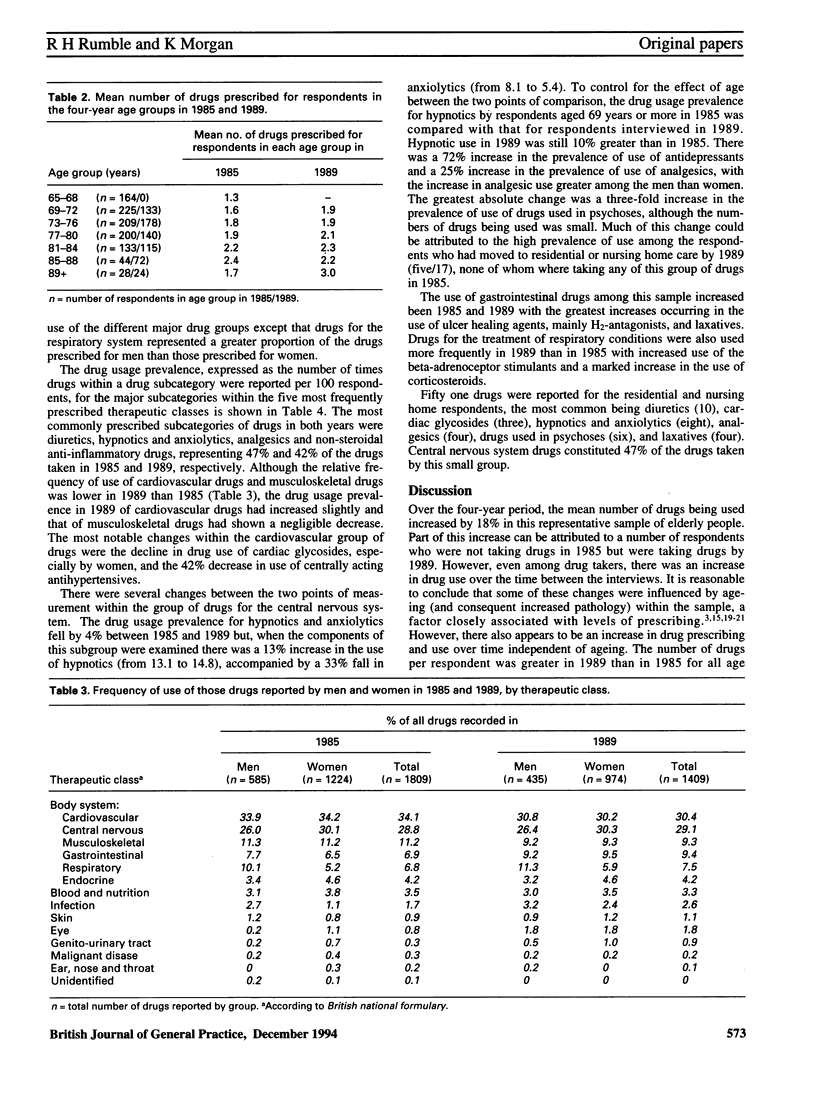
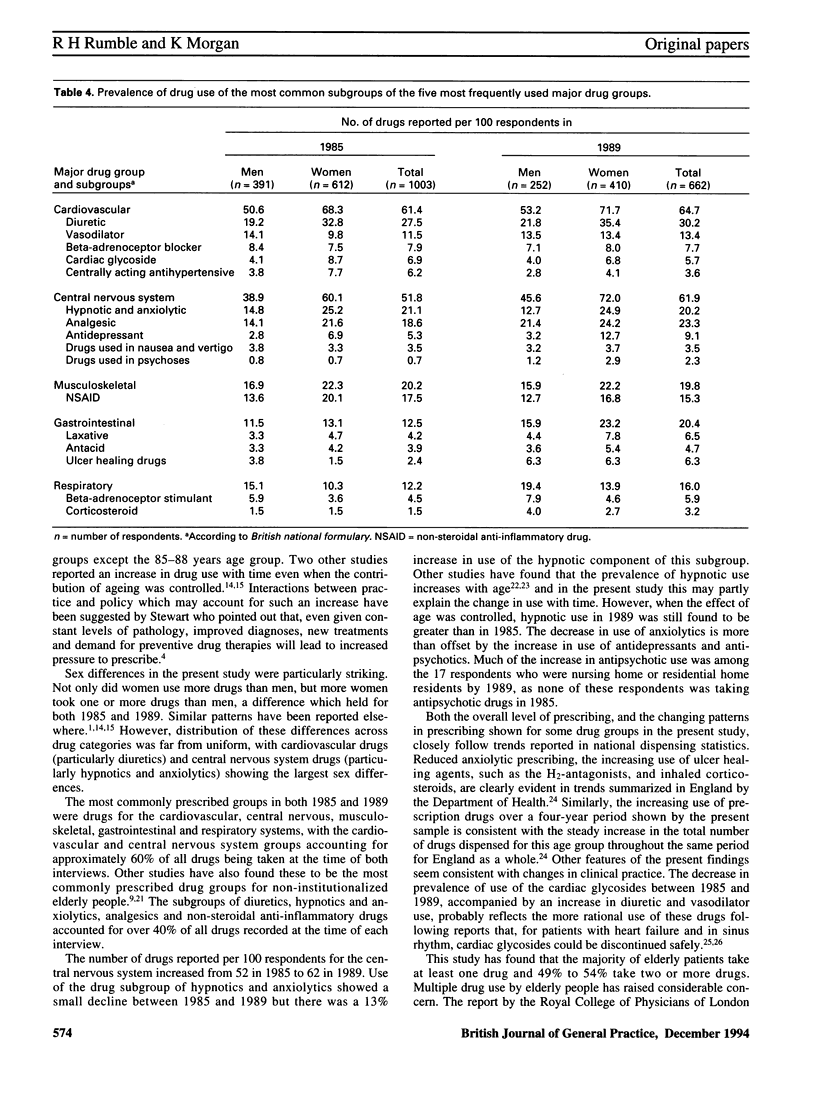
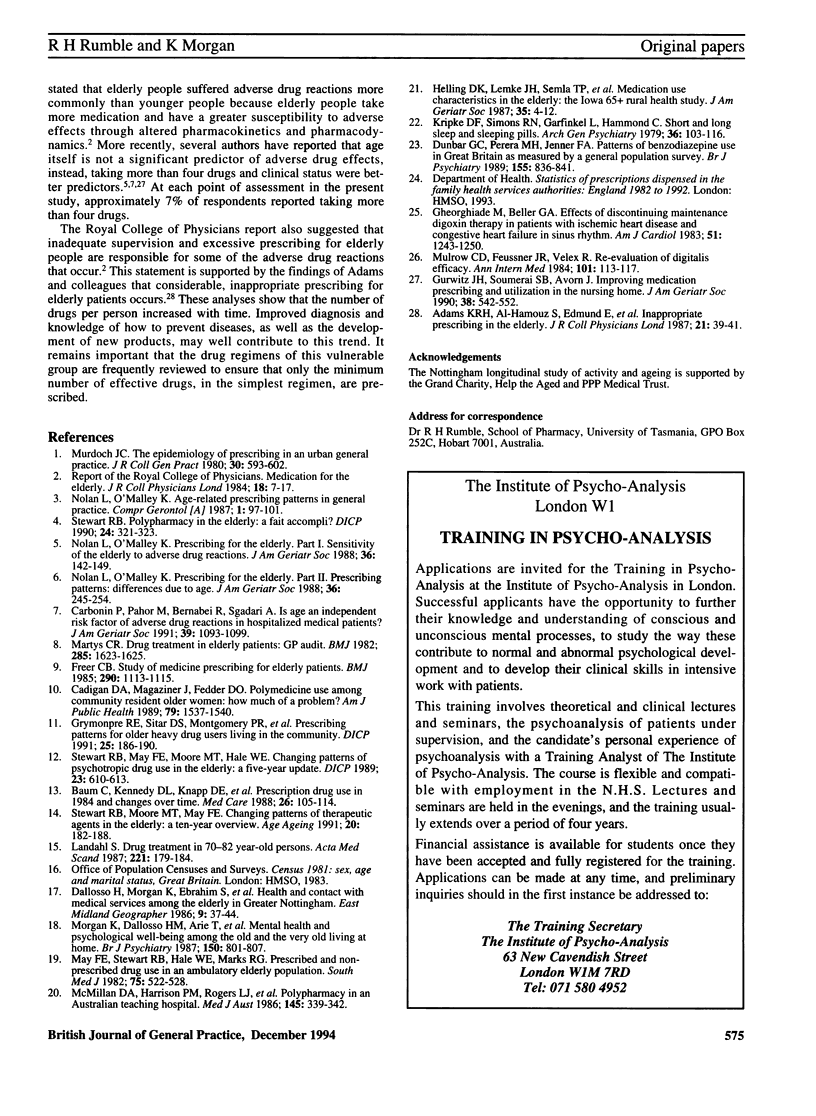
BACKGROUND. Elderly people are prescribed more drugs than younger people. The consequences of excessive or unwise prescribing, such as drug interactions, are well known. AIM. A longitudinal study was undertaken to examine levels and patterns of prescribed drug use among a group of elderly people. METHOD. Use of prescribed drugs by a sample of elderly people in Nottingham aged 65 years and over was assessed on two occasions four years apart, in 1985 and 1989. RESULTS. Complete drug data were available for 1003 respondents in 1985 and 662 respondents in 1989 (with attrition due mainly to mortality). Drug use increased significantly with age. Women took significantly more drugs than men. Approximately half of respondents were taking at least two drugs. The overall number of drugs per person being taken in 1989 was significantly greater than in 1985. This difference remained significant when age and mortality were controlled, suggesting that changes in drug use over time within this sample may reflect genuine changes in prescribing practice (rather than simply the effects of ageing). The most commonly prescribed drug classes on each occasion were drugs for the cardiovascular system, central nervous system, musculoskeletal system, gastrointestinal tract and respiratory system. The subgroups of drugs most commonly reported at each interview were diuretics, hypnotics and anxiolytics, analgesics and non-steroidal anti-inflammatory drugs. Drugs within the category 'hypnotics and anxiolytics' showed clear and differential trends over time, with the use of anxiolytics falling, while the use of hypnotics increased. Among those respondents admitted to residential care during the course of the study higher levels of psychotropic drug use, and an increase in antipsychotic medication, were observed. CONCLUSION. It is important that the drug regimens of elderly people are frequently reviewed to ensure that only the minimum number of effective drugs, in the simplest regimen, are prescribed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams K. R., Al-Hamouz S., Edmund E., Tallis R. C., Vellodi C., Lye M. Inappropriate prescribing in the elderly. J R Coll Physicians Lond. 1987 Jan;21(1):39–41. [PMC free article] [PubMed] [Google Scholar]
- Baum C., Kennedy D. L., Knapp D. E., Juergens J. P., Faich G. A. Prescription drug use in 1984 and changes over time. Med Care. 1988 Feb;26(2):105–114. doi: 10.1097/00005650-198802000-00002. [DOI] [PubMed] [Google Scholar]
- Cadigan D. A., Magaziner J., Fedder D. O. Polymedicine use among community resident older women: how much a problem? Am J Public Health. 1989 Nov;79(11):1537–1540. doi: 10.2105/ajph.79.11.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonin P., Pahor M., Bernabei R., Sgadari A. Is age an independent risk factor of adverse drug reactions in hospitalized medical patients? J Am Geriatr Soc. 1991 Nov;39(11):1093–1099. doi: 10.1111/j.1532-5415.1991.tb02875.x. [DOI] [PubMed] [Google Scholar]
- Dunbar G. C., Perera M. H., Jenner F. A. Patterns of benzodiazepine use in Great Britain as measured by a general population survey. Br J Psychiatry. 1989 Dec;155:836–841. doi: 10.1192/bjp.155.6.836. [DOI] [PubMed] [Google Scholar]
- Freer C. B. Study of medicine prescribing for elderly patients. Br Med J (Clin Res Ed) 1985 Apr 13;290(6475):1113–1115. doi: 10.1136/bmj.290.6475.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheorghiade M., Beller G. A. Effects of discontinuing maintenance digoxin therapy in patients with ischemic heart disease and congestive heart failure in sinus rhythm. Am J Cardiol. 1983 May 1;51(8):1243–1250. doi: 10.1016/0002-9149(83)90293-x. [DOI] [PubMed] [Google Scholar]
- Grymonpre R. E., Sitar D. S., Montgomery P. R., Mitenko P. A., Aoki F. Y. Prescribing patterns for older heavy drug users living in the community. DICP. 1991 Feb;25(2):186–190. doi: 10.1177/106002809102500214. [DOI] [PubMed] [Google Scholar]
- Gurwitz J. H., Soumerai S. B., Avorn J. Improving medication prescribing and utilization in the nursing home. J Am Geriatr Soc. 1990 May;38(5):542–552. doi: 10.1111/j.1532-5415.1990.tb02406.x. [DOI] [PubMed] [Google Scholar]
- Helling D. K., Lemke J. H., Semla T. P., Wallace R. B., Lipson D. P., Cornoni-Huntley J. Medication use characteristics in the elderly: the Iowa 65+ Rural Health Study. J Am Geriatr Soc. 1987 Jan;35(1):4–12. doi: 10.1111/j.1532-5415.1987.tb01312.x. [DOI] [PubMed] [Google Scholar]
- Kripke D. F., Simons R. N., Garfinkel L., Hammond E. C. Short and long sleep and sleeping pills. Is increased mortality associated? Arch Gen Psychiatry. 1979 Jan;36(1):103–116. doi: 10.1001/archpsyc.1979.01780010109014. [DOI] [PubMed] [Google Scholar]
- Landahl S. Drug treatment in 70-82-year-old persons. A longitudinal study. Acta Med Scand. 1987;221(2):179–184. doi: 10.1111/j.0954-6820.1987.tb01264.x. [DOI] [PubMed] [Google Scholar]
- Martys C. R. Drug treatment in elderly patients: GP audit. Br Med J (Clin Res Ed) 1982 Dec 4;285(6355):1623–1625. doi: 10.1136/bmj.285.6355.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May F. E., Stewart R. B., Hale W. E., Marks R. G. Prescribed and nonprescribed drug use in an ambulatory elderly population. South Med J. 1982 May;75(5):522–528. doi: 10.1097/00007611-198205000-00004. [DOI] [PubMed] [Google Scholar]
- McMillan D. A., Harrison P. M., Rogers L. J., Tong N., McLean A. J. Polypharmacy in an Australian teaching hospital. Preliminary analysis of prevalence, types of drugs and associations. Med J Aust. 1986 Oct 6;145(7):339–342. [PubMed] [Google Scholar]
- Morgan K., Dallosso H. M., Arie T., Byrne E. J., Jones R., Waite J. Mental health and psychological well-being among the old and the very old living at home. Br J Psychiatry. 1987 Jun;150:801–807. doi: 10.1192/bjp.150.6.801. [DOI] [PubMed] [Google Scholar]
- Mulrow C. D., Feussner J. R., Velez R. Reevaluation of digitalis efficacy. New light on an old leaf. Ann Intern Med. 1984 Jul;101(1):113–117. doi: 10.7326/0003-4819-101-1-113. [DOI] [PubMed] [Google Scholar]
- Murdoch J. C. The epidemiology of prescribing in an urban general practice. J R Coll Gen Pract. 1980 Oct;30(219):593–602. [PMC free article] [PubMed] [Google Scholar]
- Nolan L., O'Malley K. Age-related prescribing patterns in general practice. Compr Gerontol A. 1987 Sep;1(3):97–101. [PubMed] [Google Scholar]
- Nolan L., O'Malley K. Prescribing for the elderly. Part I: Sensitivity of the elderly to adverse drug reactions. J Am Geriatr Soc. 1988 Feb;36(2):142–149. doi: 10.1111/j.1532-5415.1988.tb01785.x. [DOI] [PubMed] [Google Scholar]
- Nolan L., O'Malley K. Prescribing for the elderly: Part II. Prescribing patterns: differences due to age. J Am Geriatr Soc. 1988 Mar;36(3):245–254. doi: 10.1111/j.1532-5415.1988.tb01809.x. [DOI] [PubMed] [Google Scholar]
- Stewart R. B., May F. E., Moore M. T., Hale W. E. Changing patterns of psychotropic drug use in the elderly: a five-year update. DICP. 1989 Jul-Aug;23(7-8):610–613. doi: 10.1177/1060028089023007-821. [DOI] [PubMed] [Google Scholar]
- Stewart R. B., Moore M. T., May F. E., Marks R. G., Hale W. E. Changing patterns of therapeutic agents in the elderly: a ten-year overview. Age Ageing. 1991 May;20(3):182–188. doi: 10.1093/ageing/20.3.182. [DOI] [PubMed] [Google Scholar]
- Stewart R. B. Polypharmacy in the elderly: a fait accompli? DICP. 1990 Mar;24(3):321–323. doi: 10.1177/106002809002400320. [DOI] [PubMed] [Google Scholar]


