Abstract
Fractures of the trapezium occur infrequently, accounting for only 3.5 % of all carpal fractures. Trapezium fractures with concomitant Bennett’s fracture-dislocations are exceedingly rare without a consensus on treatment recommendations. Here, we present a case of a simultaneous Bennett’s fracture with a trapezium fracture in a pediatric patient. Our patient was treated with open reduction and internal fixation. Clinically, the patient was pain free with range of motion comparable to his uninjured side and without joint instability. A review of the literature reveals only twelve other cases reported in adult patients all of which were male with an average age of twenty-eight at the time of injury. Open reduction is the most popular treatment approach, but closed reduction can also be utilized with success in these injuries. While there is a large degree of heterogeneity of outcome reporting methodology, most patients have satisfactory outcomes and return to function comparable to their contralateral side.
Keywords: Bennett’s fracture, Trapezium fracture, Rare hand fractures, Fracture-Dislocation
Introduction
Bennett’s fractures account for 1–2 % of all hand fractures.1,2 First described by Dr. Edward Bennett in 1882, they involve a fracture at the base of the first metacarpal, typically with a volar ulnar fragment and dislocation of the carpometacarpal (CMC) joint.3,4 This pattern of injury is classically caused by axial loading on an abducted or extended thumb and often occurs with other injuries.5, 6, 7, 8 Accepted treatment options include open reduction with internal fixation (ORIF) or closed reduction with percutaneous Kirschner-wire pinning (CRPP).9 Although both treatment methods are effective and show no significant differences in clinical outcomes or subsequent incidence of radiographic arthritis, the standard of care remains a subject of active debate.4
Isolated fractures of the trapezium are rare, accounting for only 3.5 % of all carpal fractures.10 These injuries typically result from high-energy forces, such as those sustained during motor vehicle accidents, falls, and contact sports.5,11 Due to their low incidence and poor radiographic diagnostic sensitivity, standard of care practices remain debated.12
The inherent mobility of the first trapeziometacarpal joint predisposes it to instability, especially in the setting of a Bennett’s fracture with the avulsion of the anterior oblique ligament.6,13 Proper treatment is critical to optimize patient outcomes, minimize arthritis risk, and preserve hand function. Since there is no consensus on the optimal management for either Bennett’s fractures or trapezium fractures individually, concomitant injuries pose a particularly complex therapeutic challenge. The purpose of this study is to present a rare care of Bennett’s fracture associated with fracture of the trapezium in a pediatric patient and review current literature regarding treatment options and patient outcomes.
Case report
A 17-year-old right hand-dominant male presented to the emergency department after falling onto his outstretched left hand while riding his bicycle. Plain radiographs revealed skeletal maturity with a comminuted trapezium fracture, a displaced fracture through the ulnar base of the first metacarpal, and dislocation of the first CMC joint (Figure 1). Closed reduction was performed in the emergency department, and the patient was placed in a thumb spica splint. Approximately 2 weeks later, ORIF was performed. A curvilinear incision was made over the left thenar eminence at the junction of the glabrous and non-glabrous skin. Dissection proceeded down to the first CMC joint, and the trapezium fracture was temporarily reduced and fixated with three 0.028 Kirschner wires. One wire was then removed, and a 1 mm screw was placed. Next, the Bennett’s fracture-dislocation was reduced using traction, pronation, and abduction. Reduction was maintained by fixating the first metacarpal to the second metacarpal using two 0.045 Kirschner wires (Figure 2). Orthogonal fluoroscopic views demonstrated adequate bony reduction and proper hardware placement.
Figure 1.
Oblique view of the left hand demonstrating a comminuted fracture of the trapezium with associated dislocation of the first carpometacarpal joint, and fracture of the first metacarpal base.
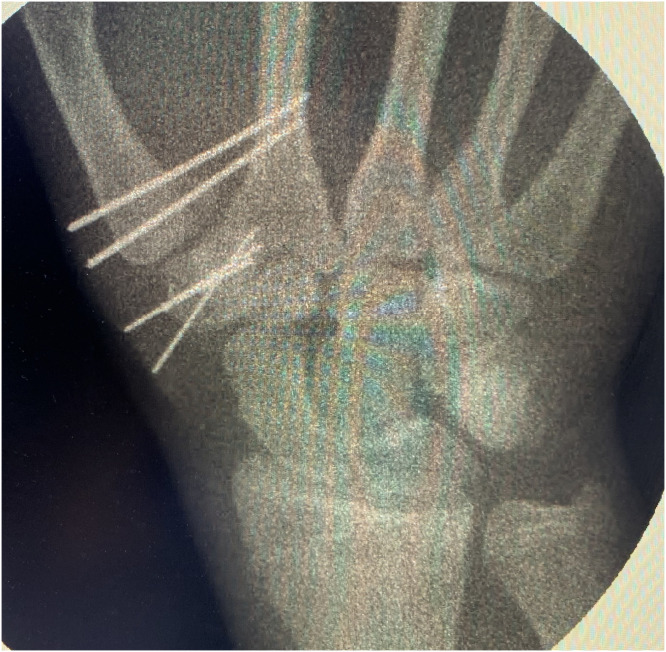
Figure 2.
Fluoroscopic view following trapezium fixation and reduction of the thumb metacarpal base with transfixation to the second metacarpal.
Six weeks later, the patient was brought back to the operating room for pin removal. Passive movement testing confirmed stability of the joint without subluxation (Figure 3). Three months from date of injury, the patient was pain free with excellent range of motion (ROM) and strength comparable to the contralateral side. The one-year follow-up appointment was canceled as he was asymptomatic with excellent functional status.
Figure 3.
Fluoroscopic PA view demonstrating maintained bony alignment with increased bone density along the fracture margins.
Discussion
Simultaneous Bennett’s fracture with an associated trapezium fracture is rare, with only twelve cases reported in the English literature.5,8,14, 15, 16, 17, 18 Patient demographics, mechanisms of injury, treatment methods, and outcomes are summarized (Table 1). All patients were male and between the ages of 18–47 (average age 28). Mechanisms of injury included motorcycle accidents (n = 4), motorized vehicle accidents (n = 3), road accidents (n = 2), a fall from a motorcycle (n = 1), bicycle accident (n = 1), and an unspecified fall (n = 1). The injuries occurred on both the left (n = 7) right hands (n = 5). In eleven cases that reported hand dominance, the non-dominant hand was injured eight times. The mean final follow-up time was 30 months with a range of 2 - 108 months.
Table 1.
Demographics, treatment methodology, and outcomes of patients with a concomitant Bennett’s fracture and trapezium fracture.
| Case | Age | Sex | Mechanism of injury | Dominant hand | Injured hand | Treatment | Follow up (months) | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 114 | 25 | Male | Motorcycle Accident | Right | Right | OR and pinning with Kirschner wires; 6 weeks immobilization | 7 | Decreased range of motion to 25 % of the contralateral side |
| 214 | 27 | Male | Road Accident | Right | Left | OR and pinning with Kirschner wires; 5 weeks immobilization | 108 | Normal range of motion and pain free |
| 314 | 33 | Male | Motor Vehicle Accident | Right | Left | OR with percutaneous fixation with two lag screws; 3 weeks immobilization and subsequent active rehabilitation | 7 | "Fully satisfied" No significant limitations in strength or motion |
| 415 | 30 | Male | Road Accident | Not Reported | Right | CR with percutaneous Kirschner wire pinning; 6 weeks immobilization | 8 | Painless range of motion; palmar abduction 75°, radial abduction 55°; pinch power was symmetric bilaterally |
| 58 | 47 | Male | Fall From Motorbike | Right | Right | OR with a 2 mm screw and Kirschner wires; 8 weeks of immobilization | 12 | Pain free, normal range of motion; QuickDASH score was 3.9/100 |
| 616 | 27 | Male | Motor Vehicle Accident | Right | Left | OR with Kirschner wire pinning; 6 weeks of immobilization | 2 | Regained Full movement of thumb, lost to follow up after 2 months |
| 717 | 24 | Male | Motorcycle Accident | Right | Left | OR with 1.5 mm screws, 2.8 mm mini-anchor, and Kirschner wire pinning; cast immobilization for 2 weeks and pins removed after 6 weeks | 12 | Quick Dash Score of 3.5; No mobility limitations and recovered grip strength |
| 818 | 19 | Male | Fall off bicycle | Right | Right | OR with a 2 mm screw, Kirschner wire pinning, and suture; 2 weeks immobilization, pins removed at 4 weeks | 12 | Regained full range of motion by eight weeks and asymptomatic at one year follow up |
| 95 | 23 | Male | Motorcycle Accident | Left | Right | OR with minifragment screw | 30 | satisfied |
| 105 | 37 | Male | Motorcycle Accident | Right | Left | OR and pinning | 80 | very satisfied |
| 115 | 18 | Male | Motor Vehicle Accident | Right | Left | OR with minifragment screws | 53 | very satisfied |
| 125 | 28 | Male | Fall | Right | Left | CR and pinning | 34 | very satisfied |
OR, open reduction; CR, closed reduction.
Of the twelve reported cases, two fractures underwent CRPP, and ten cases underwent ORIF. While the reported outcome measures were heterogeneous, only one case noted a significant reduction in ROM. Two cases reported QuickDash disability scores of 3.5 and 3.9. Four cases reported patient satisfaction outcomes, including three patients as “very satisfied” and one as “satisfied.” These injuries predominantly affected young males and often arose from motorized vehicle or bicycle accidents.
To our knowledge, the current case represents the thirteenth reported and the first in the pediatric population reported in the literature. Despite the paucity of treatment guidelines, most treatment paradigms have shown acceptable outcomes and see patients return to function comparable to their uninjured hand. The majority of the cases, including that presented herein, were treated with ORIF, though CRPP showed equivalent patient outcomes in n = 2 cases. Garcia-Elias and colleagues reported one patient with a particularly poor outcome in their case series of three patients.14 The injury occurred in the dominant hand of a twenty-five-year-old patient after a motorcycle accident. Despite treatment with open reduction, pinning, and six weeks of immobilization, the ROM of the first carpometacarpal joint was reduced to 25 % when compared to his contralateral side in flexion-extension and adduction-abduction at 7 months. Interestingly, the authors treated another 27-year-old patient similarly and reported normal ROM at 108 months postoperatively.
Concomitant Bennett’s fracture and trapezium fractures remain challenging to manage given their rarity and lack of consensus on treatment protocols. Herein, we report the successful management of this injury in a 17-year-old male patient via ORIF. While open reduction is the most common treatment approach with good patient outcomes, CRPP has also been used with success. While there is a large degree of heterogeneity in outcome measures reported, most patients return to normal function with either treatment modality. Further comparative studies are needed to determine the optimal approach to treating these complex injuries.
Statement of human rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of informed consent
Informed consent was obtained from all patients for being included in the study.
IRB approval
Local IRB considers case reports involving three or fewer patients exempt and does not require IRB review if the interaction with patients was solely for treatment purposes.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
None.
References
- 1.Hove L.M. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993;27(4):317–319. [PubMed] [Google Scholar]
- 2.Dobyns J.H., Linscheid R.L., Cooney W.P. Fractures and dislocations of the wrist and hand, then and now. J Hand Surg Am. 1983;8(5 Pt 2):687–690. doi: 10.1016/s0363-5023(83)80247-0. [DOI] [PubMed] [Google Scholar]
- 3.Bennett E.H. Fracture of the metacarpal bones. Dublin J Med Sci. 1883;73:72–75. [Google Scholar]
- 4.Carlsen B.T., Moran S.L. Thumb trauma: bennett fractures, Rolando fractures, and ulnar collateral ligament injuries. J Hand Surg Am. 2009;34(5):945–952. doi: 10.1016/j.jhsa.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 5.McGuigan F.X., Culp R.W. Surgical treatment of intra-articular fractures of the trapezium. J Hand Surg Am. 2002;27(4):697–703. doi: 10.1053/jhsu.2002.33705. [DOI] [PubMed] [Google Scholar]
- 6.Roger J., Mathieu L., Mottier F., et al. Trapeziometacarpal joint dislocation complicated by a trapezium fracture: a case report and literature review. Hand Surg Rehabil. 2016;35(4):288–291. doi: 10.1016/j.hansur.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Papp S Carpal bone fractures. Hand Clin. 2010;26(1):119–127. [DOI] [PubMed]
- 8.Goyal T. Bennett's fracture associated with fracture of trapezium - A rare injury of first carpo-metacarpal joint. World J Orthop. 2017;8(8):656–659. doi: 10.5312/wjo.v8.i8.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rivlin M., Fei W., Mudgal C.S. Bennett fracture. J Hand Surg Am. 2015;40(8):1667–1668. doi: 10.1016/j.jhsa.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 10.Borgeskov S., Christiansen B., Kjaer A., et al. Fractures of the carpal bones. Acta Orthop Scand. 1966;37(3):276–287. doi: 10.3109/17453676608989415. [DOI] [PubMed] [Google Scholar]
- 11.Garneti N., Tuson C.E. Sagittally split fracture of trapezium associated with subluxated carpo-metacarpal joint of thumb. Injury. 2004;35(11):1172–1175. doi: 10.1016/j.injury.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Gibney B., Murphy M.C., Ahern D.P., et al. Trapezium fracture: a common clinical mimic of scaphoid fracture. Emerg Radiol. 2019;26(5):531–540. doi: 10.1007/s10140-019-01702-2. [DOI] [PubMed] [Google Scholar]
- 13.Van Brenk B., Richards R.R., Mackay M.B., et al. A biomechanical assessment of ligaments preventing dorsoradial subluxation of the trapeziometacarpal joint. J Hand Surg Am. 1998;23(4):607–611. doi: 10.1016/s0363-5023(98)80045-2. [DOI] [PubMed] [Google Scholar]
- 14.Garcia-Elias M., Henríquez-Lluch A., Rossignani P., et al. Bennett's fracture combined with fracture of the trapezium. A report of three cases. J Hand Surg Br. 1993;18(4):523–526. doi: 10.1016/0266-7681(93)90164-b. [DOI] [PubMed] [Google Scholar]
- 15.El Ibrahimi A., Amar F., Chbani B., et al. Dislocation of the carpometacarpal joint of the thumb associated with trapezium and Bennett's fractures. Hand (N Y) 2009;4(2):191–193. doi: 10.1007/s11552-008-9162-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kosagi Sharaph R., Saseendar S., Shanmugasundaram S. Combined Bennett fracture dislocation and trapezium fracture: a rare case report. Cureus. 2019;11(11):e6211. doi: 10.7759/cureus.6211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pina G., Vaz M.R., Vaz A., et al. Trapezium and Bennett fracture - A rare base thumb fracture pattern:a case report. J Orthop Case Rep. 2021;11(5):99–103. doi: 10.13107/jocr.2021.v11.i05.2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radford P.J., Wilcox D.T., Holdsworth B.J. Simultaneous trapezium and Bennett's fractures. J Hand Surg Am. 1992;17(4):621–623. doi: 10.1016/0363-5023(92)90304-8. [DOI] [PubMed] [Google Scholar]