Abstract
The triage classification and diagnosis of eye diseases in primary care patients through teleophthalmology were performed by ophthalmologists, optometrists, and family physicians. The agreement in triage classification and diagnosis between observers, as well as the quality of referrals from primary care to ophthalmology, were evaluated. Study to compare methods using a non-inferiority method approach. The sample comprised 220 patients with suspected ocular problems evaluated by family physicians. These patients were examined by an optometrist (observer 1) using a Visionix VX650 multi-diagnostic platform. The optometrist provided a suspected diagnosis and a referral. The tests were forwarded electronically to an ophthalmologist (observer 2), who provided a diagnosis and referral. Subsequently, they were reviewed in person by an ophthalmologist (observer 3) who provided a diagnosis and referral. The observers worked independently and at different times, without knowledge of each other’s evaluations, ensuring the objectivity of the analysis. We analyzed interobserver agreement in triage referrals and diagnosis using the Kappa index. The triage classification of patients by teleophthalmology coincides with that of in-person ophthalmology in 91.2% of the cases (Kappa = 0.819). The optician’s triage classification coincided with in-person ophthalmology in 91.3% (Kappa = 0.858) and with teleophthalmology in 92.3% (Kappa = 0.851). The diagnostic categories, teleophthalmology and in-person ophthalmology coincided in 84.61% of the cases (Kappa = 0.80). The optician coincided with in-person ophthalmology in 90.65% (Kappa = 0.88) and with teleophthalmology in 90.9% of the diagnoses (Kappa = 0.87). There was a very high level interobserver agreement for both triage classification and diagnostic categories. This validates our teleophthalmology approach, conducted in a primary care setting by optometrists, family physicians, and ophthalmologists, for an effective triage classification of patients referred to ophthalmology services. This telemedicine also accurately categorizes patients based on their conditions, optimizing resources, reducing waiting times and waiting lists.
Keywords: referrals, optometry, primary care, ophthalmology, teleophthalmology, triage
Highlights.
● Our teleophthalmology system reveals a high level of agreement in triage classification and diagnostic categories between teleophthalmology an in-personal care.
● A collaborative teleophthalmology system that links optometrists and ophthalmologists is valid, allowing efficient triage classification of patinets and referrals form primary care.
● This teleophthalmology framework effectively categorizes patients according to their specific pathologies and significantly reducing wait times for consultations.
● The optometrist perfomed a comprehensive optometric examination using the Visionix VX650 multiple diagnostic platform.
Introduction
Teleophthalmology has been widely implemented in many parts of the world for years, with opticians serving as a key access point for providing care to individuals in remote or underserved areas.1,2 In Scotland and England, optometrists refer patients to hospitals by sending patient reports, along with retinal images, to primary care physicians and ophthalmologists via an online platform.3 -5 Similarly, Denmark has recently adopted teleophthalmology, where opticians also refer patients to ophthalmology services. 6 The COVID-19 pandemic has significantly accelerated the use of teleophthalmology and teleconsultations worldwide.7,8
In Spain, the population is aging rapidly, which will challenge the public healthcare system. 9 This will lead to increasing delays in access to specialist consultations due to the high demand and low number of specialist physicians.10,11 Ophthalmology, in particular, is a highly sought-after specialty in both outpatient and hospital settings. 12 Therefore, exploring new methods to optimize the available healthcare resources is essential.
Optometrists are well-trained professionals, specializing in refraction and skilled in the use of ocular diagnostic equipment. With the right tools, they can perform comprehensive eye exams. Notably, multi-diagnostic platforms, which conduct several tests in a single session, allow for safe online sharing of diagnostic data with ophthalmologists. This makes the creation of a teleophthalmology system in Spain not only feasible but also a valuable support to both primary and specialized healthcare.
We hypothesized that patients with vision problems who visit a primary healthcare center and are examined by a trained optometrist at an optician using multi-diagnostic platforms, could be correctly prioritized for specialist ophthalmology consultations in 80% of cases. This prioritization would reduce wait times between primary care and specialist consultations, enabling earlier screening and diagnosis of most common ocular conditions.
This study aimed to assess whether a teleophthalmology model supported by optometrists in primary care achieves sufficient diagnostic agreement and appropriate triage decisions when compared to face-to-face ophthalmologic evaluation across a wide range of consultation types. To this end, ocular conditions in patients presenting with visual impairment at primary care centers were prioritized and diagnosed through a collaborative model involving an ophthalmologist, an optometrist, and a primary care physician. Additionally, we aimed to assess the concordance between triage classification and diagnosis through optometrist assessment, teleophthalmology, and in-person ophthalmic evaluation. Furthermore, we analyzed the percentage of patients correctly prioritized for the most significant conditions, the reduction in referrals for in-person ophthalmology consultations, and the overall impact on healthcare and society.
Methodology
Patients and Methods
A cross-sectional observational study was conducted to compare methods using a noninferiority approach. 13
In order for kappa statistic, and therefore our conclusions, to be statistically valid, it was necessary to determine the minimum necessary sample size based on certain assumptions. The works of Flack et al 14 and Bujang and Baharum 15 provide the method to calculate this size, which requires: first, assigning a percentage to the studied pathologies to be diagnosed and assuming these percentages are the same for both observers and second, providing an initial estimated accuracy value. Regarding the first point, we conducted a review of 220 referrals from primary care to the ophthalmology service at HU Virgen Macarena. We classified the diagnoses issued by the ophthalmologist and calculated their frequency percentages. The results yielded 7 diagnostic categories with the following frequencies: cataracts (27.3%), refractive errors (19.5%), anterior segment (18.2%), posterior segment (14.1%), normal examination (18.6%), strabismus (1.4%), and others (0.9%). For the second point, estimating a kappa value, we based our estimate on published studies.16 -27 We believe the accuracy will be high, and assign an estimated kappa value of 0.7, potentially exceeding 0.8. This corresponds to a substantial level of agreement. 28 Under these considerations, it is determined that the minimum required sample size for the index to be statistically significant was 168 patients. For this, we used the N2.cohen.kappa function within R Project software, which returns the optimal sample size according to the method defined in 14, considering a specified power (in this case, 80%) and assuming that the probabilities associated with each category are the same for all observers.
Finally, 220 patients were examined, thus covering the minimum size required to ensure the reliability of the analyses.
The patients included in the sample met the following inclusion criteria: patients over 18 years of age, whose primary reason for consultation was vision loss (decreased vision), with no prior known ocular disease, and who had provided informed consent freely and consciously.
The study involved patients visiting a primary care physician for vision loss who were being referred to the ophthalmology service. Before the referral, these patients were examined by an optometrist (observer 1) who conducted a series of diagnostic tests. The optometrist then transmitted the results electronically to the teleophthalmology ophthalmologist (observer 2), who provided a diagnosis and determined the appropriate referral pathway. Referral options included urgent, scheduled, or no referral. Subsequently, the patient was seen by an ophthalmologist in person, the gold standard comparator (observer 3), who provided a diagnosis and the appropriate referral. Two independent ophthalmologists acted as observers: one evaluated the cases remotely via teleophthalmology using the clinical data and images collected by the optometrist, while the second assessed the same patients in a traditional face-to-face setting. The in-person ophthalmologic evaluation served as the reference standard for assessing diagnostic and triage agreement. This process allowed for a comparison between the teleophthalmology-based diagnosis and referral and the in-person consultation.
Of the 220 enrolled patients, only 10 (5.5%) were classified as urgent or non-urgent but should be seen on a preferential. After obtaining the images through telemedicine and sending them, it was requested that their in-person consultation be carried out immediately. These patients were treated without delay, but the clinical data obtained could still be used for the study.
Primary care physicians at a health center in Seville, Spain, were responsible for recruiting patients and ensuring they met the inclusion criteria. Patients were not selected based on sex; however, sex was recorded to disaggregate results. Sex was classified as male or female. 29 Patient age was categorized into age groups to provide more meaningful insights: 18 to 40 years (a period of more stable refractions and lower incidence of disease), 41 to 65 years (the onset of presbyopia), 30 and 66 to 100 years (when conditions such as cataracts, glaucoma, and AMD become more prevalent).31 -34
Patient recruitment was conducted anonymously to protect privacy, with each patient assigned a numerical code so that investigators did not have access to personal data. The study complied with Spanish data protection laws and the Declaration of Helsinki. Ethical approval was obtained from the ethics committees.
The optometrist scheduled appointments for the recruited patients within 3 days and conducted a comprehensive optometric examination using the VISIONIX VX650 multi-diagnostic platform. With this VISIONIX VX650 the following tests were performed: objective refraction, tonometry, pachymetry, anterior segment tomography, cataract analysis, corneal topography, fundus photography. In addition, the following tests were performed: distance and near visual acuity, subjective refraction for both distance and near, Amsler grid test, and anterior pole photography with fluorogram.
The optometrist provided a preliminary diagnosis and triage classification for each patient. An anonymized report containing the patient’s test results was generated and securely transmitted to the teleophthalmology ophthalmologist within 1 day. The teleophthalmologist then issued a diagnosis and referral within a maximum of 1 week. Subsequently, the patient was scheduled for an in-person ophthalmology consultation within 1 month, during which the ophthalmologist also provided a diagnosis and referral. Each observer examined the patients independently and in a blinded manner. The time from the primary care physician’s referral to the first in-person ophthalmology consultation was less than 1 month for all patients. Subsequently, the patients who requiring treatment for chronic conditions (eg, glaucoma, AMD) were managed within the hospital’s ophthalmology department, patients were scheduled for follow-up according to clinical needs, treatment initiation occurred at the same institution. Cases requiring subspecialty care (eg, retina, cornea) were referred to appropriate subspecialists within the same hospital. All referrals maintained continuity within the public healthcare system.
To ensure consistent triage classification, common criteria were established for the most frequent pathologies, following the guidelines of the Royal Brisbane & Women’s Hospital and the University Hospital of Wales (See Supplementary Material, Appendix 1 and 2).35,36
The collected data were analyzed, and statistical analyses were performed to assess inter-observer agreement. For inter-observer agreement analysis, 2 independent senior ophthalmologists (B.P.Z. and E.R.R.), uninvolved in initial assessments, adjudicated all discordant cases. These evaluators were blinded to both the original observer identities and prior diagnoses, using predefined criteria (Royal Brisbane Hospital and Wales guidelines) to confirm or reassign diagnoses and triage categories. This arm’s-length validation process eliminated self-verification bias while maintaining diagnostic consistency.
We study the quality of referrals, we refer to the appropriateness and accuracy of the referral decisions made by each healthcare provider involved in the study (Optometrists and ophthalmologists). This includes:
Correct triage classification: Whether the urgency level assigned (urgent, scheduled, or no referral needed) aligns with the patient’s actual condition as confirmed by in-person ophthalmologist evaluation.
Diagnostic accuracy: The degree to which the suspected diagnosis provided by the referring professional (family physician or optometrist) or the teleophthalmologist matches the final diagnosis from the in-person ophthalmologist.
Reduction of Unnecessary Referrals: The ability of the teleophthalmology system (with optometrist support) to filter out cases that do not require specialist intervention (eg, refractive errors or normal examinations), thereby optimizing resource use.
In our study, we evaluated:
The agreement in triage classification and diagnoses between optometrists, teleophthalmologists, and in-person ophthalmologists (using Kappa statistics).
The proportion of avoidable referrals identified through this collaborative system.
Thus, “referral quality” encompasses both the clinical validity of the referral decision and its efficiency in directing patients to the most suitable care pathway.
This study was designed and reported in accordance with the STROBE guidelines for cross-sectional observational studies, supplemented by the GRRAS recommendations for reliability and agreement studies. Additionally, the methodological principles from the CONSORT extension for non-inferiority trials were considered and adapted to the observational study context (See Supplmentary Material).37 -39
Statistical Analysis
Data analysis was carried out using IBM Statistics SPSS (version 29), R project (version 4.3), and Excel (version 2312). The main variables are represented by frequency tables and graphs. The Kappa coefficient was used to measure the level of agreement between 2 raters (<0 No agreement, 0–0.20 slight, 0.21-0.40 fair, 0.41-0.60 moderate, 0.61-0 0.80 substantial, and 0.81-1.0 perfect agreement.) 28 A P-value < 0.05 was considered significant for the kappa test.
Results
Of the total 220 patients studied, 79 were male (35.9%) and 141 female (64.1%). The age distribution was as follows: 21 patients (9.5%) were between 18 and 40 years old, 126 patients (57.3%) were aged 41 to 65, and 73 patients (33.2%) were between 65 and 100 years old.
Among these, 38 patients (17.3%) did not complete the study. Within this subgroup, 13 were male (34.21%) and 25 were female (65.79%). For the 38 patients who did not complete the study, the age distribution was: 7 patients (18.42%) were between 18 and 40 years old, 19 patients (50.0%) were between 18 and 40 years old and 12 patients (31.58%) were between 18 and 40 years old.
The diagnoses made by the ophthalmologist for the patients’ primary complaints were grouped into the following categories: refractive error in 43 patients (22.62%), cataracts in 45 (24.72%), anterior segment pathology in 46 (25.3%), posterior segment pathology in 23 (12.64%), strabismus in 3 (1.64%), normal examination in 19 (10.44%), and other diagnoses in 3 patients (1.64%)
In Table 1, we observe the distribution of diagnostic categories by age and sex. Notably, cataracts were the most frequent pathology in the 66 to 100 age group, while in the 41 to 65 age group, refractive error was the most common diagnosis, followed by anterior segment pathologies.
Table 1.
Total Diagnostic Categories According to the In-Person Ophthalmologist, by Age and Sex.
| Diagnostic category | Sex | Age | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | 18-40 | 41-65 | 66-100 | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Cataracts | 45 | 24.72 | 14 | 7.7 | 31 | 17 | 0 | 0 | 13 | 7.14 | 32 | 17.6 |
| Refractive error | 43 | 23.62 | 13 | 7.14 | 30 | 16.5 | 6 | 3.3 | 35 | 19.2 | 2 | 1.1 |
| Anterior pole | 46 | 25.3 | 17 | 9.34 | 29 | 16 | 5 | 2.75 | 25 | 13.7 | 16 | 8.8 |
| Posterior pole | 23 | 12.64 | 10 | 5.5 | 13 | 7.1 | 2 | 1.1 | 15 | 8.24 | 6 | 3.3 |
| Normal exam | 19 | 10.44 | 8 | 4.4 | 11 | 6 | 0 | 0 | 15 | 8.24 | 4 | 2.2 |
| Strabismus | 3 | 1.64 | 2 | 1.1 | 1 | 0.55 | 1 | 0.55 | 1 | 0.55 | 1 | 0.5 |
| Other | 3 | 1.64 | 2 | 1.1 | 1 | 0.55 | 0 | 0 | 3 | 1.65 | 0 | 0 |
| Total | 182 | 100 | 66 | 36.3 | 116 | 63.7 | 14 | 7.7 | 107 | 58.8 | 61 | 33.5 |
For the 38 patients who did not complete the study, the optometrist provided the following suspected diagnoses: refractive error in 11 patients (29%), normal examination in 10 (26.3%), anterior segment pathology in 8 (21.05%), cataracts in 8 (21.05%), and posterior segment pathology in 1 (2.6%).
Referral recommendations made by the ophthalmologist were classified into 3 groups: scheduled appointments, urgent appointments, and no referral needed. The results based on the ophthalmologist’s criteria during the in-person consultation are as follows: scheduled 118 (64.8%), urgent 10 (5.5%), and no referral 54 (29.7%).
In Table 2, we see the triage classification assigned by the in-person ophthalmologist for the entire sample, as well as by age and sex. The majority of referrals were scheduled appointments, and it is noteworthy that 29.7% of these were avoidable, with most of these cases occurring in female patients and in the 41 to 65 age group. Only 5.5% of the referrals were deemed urgent.
Table 2.
Triage Classification According to the In-Person Ophthalmologist, by Sex and Age Group.
| Triage classification | Total | Sex | Age | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | 18-40 | 41-65 | 66-100 | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Scheduled | 118 | 64.8 | 46 | 25.3 | 72 | 39.6 | 8 | 4.4 | 58 | 31.8 | 52 | 29 |
| Urgent | 10 | 5.5 | 7 | 3.8 | 3 | 1.6 | 1 | 0.5 | 8 | 4.4 | 1 | 0.5 |
| No referral | 54 | 29.7 | 13 | 7.1 | 41 | 22.5 | 5 | 2.7 | 41 | 22.5 | 8 | 4.4 |
| Total patients | 182 | 100 | 66 | 36.2 | 116 | 63.7 | 14 | 7.6 | 107 | 58.7 | 61 | 34 |
We analyzed the concordance between the 3 observers: the optometrist (OPT), the teleophthalmologist (TELEOPH), and the in-person ophthalmologist (IN-PERSON OPH). This is the core of our study. Our hypothesis is that with a teleophthalmology system in collaboration with an optometrist, 80% of patients can be correctly prioritized. This hypothesis has been confirmed by the following data (see Table 3).
Table 3.
Percentage of Agreement in Triage Classification Between In-Person Ophthalmology (IN-PERSON OPH), Teleophthalmology (TELEOPH), and Optician-Optometrist (OPT).
| Agreement | Triage classification | |||||
|---|---|---|---|---|---|---|
| IN-PERSON OPH. vs TELEOPH. | OPT. vs TELEOPH. | OPT. vs IN-PERSON OPH. | ||||
| N patients/% | N 182 | % | N 220 | % | N 182 | % |
| Agreement | 166 | 91.2 | 201 | 91.36 | 168 | 92.3 |
| No agreement | 16 | 8.8 | 19 | 8.64 | 14 | 7.7 |
In Table 3, we observe that the triage classification or referral of patients from primary care to ophthalmology supports our hypothesis. The triage classification by teleophthalmology matched that of in-person ophthalmology in 166 out of 182 total patients, which corresponds to a 91.2% concordance. This high level of agreement was also confirmed in the other 2 comparisons: between in-person ophthalmology and the optometrist, and between the teleophthalmologist and the optometrist. Data highlighted in table.
The values of the concordance index were in-person ophthalmology versus teleophthalmology, Kappa = 0.819; optometrist versus in-person ophthalmology, Kappa = 0.858; and optometrist versus teleophthalmology, Kappa = 0.851 (P < 0.01 for the null hypothesis K = 0 in each comparison). Therefore, there is almost perfect agreement in patient triage classification across all 3 comparisons.
Regarding the aspect of the hypothesis suggesting that we would be able to screen for the most relevant pathologies, this has been demonstrated by the following data.
Figure 1 illustrates the percentage of agreement in diagnostic categories among the 3 observer groups: the optometrist (OPT), the teleophthalmologist (TELEOPH), and the in-person ophthalmologist (IN-PERSON OPH). The results show a high percentage of agreement across all comparisons and diagnostic categories. However, in the “Other” category, there is low agreement between optometrists and teleophthalmologists, which can be explained by the nature of this category, encompassing non-ocular pathologies that presented ocular symptoms and consisted of only 3 cases.
Figure 1.
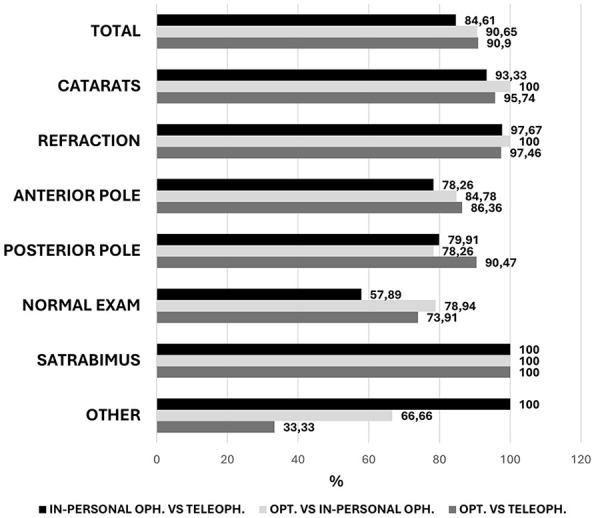
Percentage of inter-observer agreement in each diagnostic category.
Notably, the overall diagnostic agreement between teleophthalmology and in-person ophthalmology was 84.61%, highlighting the reliability of remote diagnosis compared to in-person evaluation. To assess inter-observer agreement in the diagnostic categories more accurately, the kappa index was employed.
In Figure 2, we observe the kappa index, (P < 0.01, for the contrast k = 0), which is very close to 1 across all diagnostic categories in all comparisons. This indicates that there is near-perfect agreement between the 2 observers in the 3 total comparisons and in each individual diagnostic category. The only exception is in the normal examination category, where the comparison between in-person ophthalmologists and teleophthalmology yields a kappa of 0.59, indicating a moderate level of agreement. This also occurs in the “Other” category between the optometrist and the teleophthalmologist and the in-person ophthalmologist. This category refers to non-ocular pathologies that present ocular symptomatology. There were only 4 cases (See Supplementary Material, Appendix 3).
Figure 2.

Kappa index for inter-observer agreement in each diagnostic category and in total.
To assess the potential for selection bias, we recalculated the diagnostic agreement (Kappa coefficient) between the optometrist and the tele-ophthalmologist, excluding the 38 patients who did not complete the study. The Kappa value obtained in diagnostic categories was 0.89 and in triage classification was 0.84, almost identical to the value obtained when including all participants (Kappa = 0.88 and k = 0.89). This suggests that the exclusion of these patients does not significantly influence the overall inter-observer agreement, and their loss to follow-up is unlikely to have introduced meaningful bias into the results.
The analysis of the multi-diagnostic platform Visionix showed that the reliability in the performance of corneal topography and tonometry was perfect since the measurement was correct in 100% of the cases. Reliability was very good in anterior tomography (99.10%), pachymetry (99.55%), cataract analysis (99.55%), and ocular observation (99.55%), nearly 100% correct performance. However, retinography showed the lowest reliability. In 70% of the patients, the image was perfect, in 23.20% the image quality was poor, although sufficient to see the retina, and in 6.80% the image was insufficient to see the retina. The retinography test errors are due to a low pupil diameter (less than 3 mm), lack of transparency of the ocular media (cataracts, corneal opacities), and to the difficulty in cooperation with certain patients. The use of pupillary dilation drugs would help to improve retinography measurements.
Discussion
The distribution of the sample reflects the ages of the population according to City Council data. In our sample, the largest age group consists of patients aged 41 to 65 (57.3%), followed by those over 65 years (33.2%). This aligns with the population of the Eastern district of Seville, where the largest age group is also between 40 and 65 years. 40 However, the population over 65 years accounts for only 13.92% in the district, while in our sample, it is 33.2%. This finding makes sense, as many ocular diseases are more common in older age groups.
Regarding the sex of the patients, it is noteworthy that in our sample, the number of females (64.1%) nearly doubled that of males (35.9%). This suggests that women sought ophthalmological consultations more frequently than men. In contrast, the distribution of the population in the Eastern district of Seville does not reflect this proportion, with a distribution of 48.96% males and 51.03% females. It should be noted that comparison by sex is not the object of the study.
According to the in-person ophthalmologist, the most common diagnostic category was anterior pole pathology (25.3%), followed by cataracts (24.72%) and refractive errors (23.62%). It is important to note that anterior pole pathologies encompass a group of conditions affecting the same ocular area. This distribution helps determine the organizational needs of an ophthalmology service. Notably, refractive errors (23.62%) highlight the potential role of optometrists in public healthcare, allowing ophthalmologists to focus on other pathologies without the burden of managing refractive issues. Pediatric ophthalmological conditions are considered separately, as this population group is not included in our study.
Figure 2 shows that the combination of normal examinations and refractive errors account for 34.06% of the cases. In both instances, the level of concordance between our teleophthalmology system and in-person consultations is significant. This is crucial, as addressing just these 2 categories could substantially reduce referrals to ophthalmology consultations.
Many anterior pole pathologies, particularly dry eye, could be better managed by primary care physicians. Their treatment could be standardized in primary care settings. According to the 2007 International Dry Eye WorkShop (DEWS) report, the prevalence of dry eye ranges from 5% to 35%, depending on age. 41 Identifying cases of dry eye, as in our study, would enable primary care physicians to address treatment and reduce the number of referrals. Many other conditions, such as conjunctivitis, ocular allergies, etc., can be treated very satisfactorily by a general practitioner if there is a clear diagnosis.
According to the in-person ophthalmologist, applying the established criteria, 29.7% of referrals were deemed unnecessary or no referral needed (see Table 2). A higher number of these cases occurred in the age group between 41 and 65 years, possibly due to increased presbyopia-related referrals in this age group. However, it is noteworthy that within this age group and among those over 65, there were also more appropriate consultations (see Table 2).
The results of our study suggest that unnecessary referrals could be significantly reduced, allowing for faster and more appropriate care for those who genuinely need to see an ophthalmologist.
Additionally, 5.5% of the patients should have been prioritized as urgent cases (see Table 2). In a traditional system where patients are seen in the order in which they request an appointment, these individuals could have experienced significant delays in receiving care. Improving triage classification is an important area for enhancement, as these patients have conditions that jeopardize their vision, making immediate attention crucial.
Regarding observer concordance, the findings indicate a high degree of agreement in the 3 comparisons: teleophthalmology with in-person ophthalmology, optometry with in-person ophthalmology, and optometry with teleophthalmology, both in diagnostic categories and triage classification. Notably, the optometrist shows greater concordance with the other 2 observers than they do with each other (see Table 3 and Figure 1). It should be mentioned that prior to conducting the study, the optometrist completed an expert-level course in diagnostic and clinical optometric management (500 h). This underscores the importance of the optometrist’s training in ocular conditions for the future implementation of the system.
Strabismus is the condition with the highest concordance among all observers, although there were few cases. The next category is cataracts, which exhibits very high concordance and has the largest number of cases. The case with the lowest, though still good, concordance is in the normal examination between in-person ophthalmology and teleophthalmology. It is important to investigate the reasons for this decrease. In the other categories, concordance is similar across the 3 comparisons, indicating that the studied protocol is potentially very valid and applicable.
Several errors in concordance were identified between observers. One such error is the discordant complaint, where the patient reports one reason for the consultation to the optometrist and a different reason to the in-person ophthalmologist. This discrepancy can lead to differing diagnoses and triage classification between the 2 observers. Instances of measurement errors or issues with suboptimal image quality from the Visionix VX 650 diagnostic equipment were also observed. These issues can hinder the teleophthalmologist’s ability to diagnose as effectively as the primary ophthalmologist. Optometrists face challenges in examining certain patients due to factors such as poor patient cooperation, lack of transparency of the media, or the inability to use mydriatic drugs to dilate the pupil (This could be resolved if general practitioners prescribed mydriatic medications). Based on our experience in this study, we believe integrating an optical coherence tomography system would greatly enhance the teleophthalmology system. We believe that in the future our model could be improved by implementing AI software.
Potential biases were systematically addressed: selection bias through consecutive patient enrollment; observer bias via blinding of the in-person ophthalmologist to prior assessments; and verification bias using standardized diagnostic protocols. Attrition was analyzed through documented dropout reasons, while technology limitations were mitigated by excluding poor-quality images. The high inter-observer agreement (Kappa > 0.8 across all comparisons) suggests minimal residual bias impact on study conclusions. However, a bias related to the ophthalmological specialty of each observer was noted. Depending on the subspecialty of the observing ophthalmologist, more weight may be given to one pathology over another presented by the patient, resulting in differing primary diagnoses for the same individual.
Various studies have assessed teleophthalmology for the care of individuals with vision loss in primary care settings. Electronic referral reduced unnecessary referrals by 37% compared to the traditional method. 3 This aligns with the findings of our study, in which 29.7% were not referred (see Table 2). The implementation of teleophthalmology reduced referrals to ophthalmology by half. 5 In our case, we can say that this is an achievable goal, given that the total of normal examinations and refractive errors accounted for 34.06% of the cases in our sample, to which we can add certain anterior pole pathologies that could be treated in primary care.
The collaboration between primary care physicians and ophthalmologists through teleophthalmology could provide better ophthalmologic care to the elderly population. 42 However, they suggest that adequate training of primary care physicians is needed to treat and refer older patients. This leads us to believe that the optometrist would be a good addition to primary care as an aid to primary care physicians.
The percentage of agreement between an in-person ophthalmology consultation and a teleophthalmology protocol (TECS) was high (84.3%-98.4%) for each of the disease categories. 43 The percentage of agreement in the diagnostic categories in our study was very similar (84.61%; see Figure 1).
In addition, reported near-perfect agreement between optometrists and a referral ophthalmologist in the diagnosis of ophthalmologic diseases (Κ = 0.882). 16 This is consistent with our study which found near-perfect agreement between optometrists and referring ophthalmologists across all diagnostic categories (k = 0.88). We believe that the collaboration between optometrists and general practitioners, supported by telemedicine and an ophthalmology team, ensures exceptional diagnostic accuracy while enhancing the quality and triage classification of referrals.
Although our results demonstrate a high level of interobserver agreement (Kappa > 0.8) among all evaluators, we acknowledge the presence of certain discrepancies. Hospitals implementing teleophthalmology systems should adopt the following safety measures to ensure diagnostic reliability and patient safety:
Establish standardized protocols: Clear and updated diagnostic and classification criteria must be defined to ensure consistency in clinical decision-making across all observers.
Incorporate a second-level review: Discordant or complex cases flagged by the teleophthalmology system should be automatically escalated to a second ophthalmologist for further evaluation prior to final referral decisions.
Invest in continuous training: As observed in our study, the elevated level of concordance was partially attributable to the advanced training of the participating optometrist. Continuous education in ocular pathology for both optometrists and teleophthalmology professionals is essential to maintain diagnostic accuracy.
Regular quality monitoring: Hospitals should perform periodic audits comparing teleophthalmology outcomes with face-to-face evaluations to refine diagnostic protocols and identify systematic deviations.
Technological enhancements: The integration of decision support systems based on Optical Coherence Tomography (OCT) and Artificial Intelligence (AI) can further reduce diagnostic uncertainty and improve the sensitivity for detecting urgent ocular pathologies.
Conclusions
Our study reveals a high level of concordance in triage classification and diagnostic categories between teleophthalmology and in-person consultations. In over 80% of cases, the in-person ophthalmologists reached the same conclusions as those made by the ophthalmologist using telemedicine. This underscores the validity of a collaborative teleophthalmology system that links optometrists and ophthalmologists, enabling efficient patient triage classification and referrals from primary care to specialized ophthalmology services.
Moreover, this teleophthalmology framework effectively categorizes patients according to their specific pathologies, optimizing ophthalmic resources and significantly reducing patient wait times for consultations.
Although this technology has the potential to substantially improve access to ophthalmic care and reduce waiting times, its clinical effectiveness relies on the rigorous application of structured validation processes and ongoing quality assurance.
Supplemental Material
Supplemental material, sj-docx-2-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-3-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-1-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-4-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
Thanks to the Carlos III Health Institute for its invaluable collaboration.
Footnotes
ORCID iD: Rafael Carrasco Solís  https://orcid.org/0009-0000-4131-9171
https://orcid.org/0009-0000-4131-9171
Ethical Considerations: The ethical committee of the Virgen Macarena and Virgen del Rocío university hospitals gave a favorable opinion for this study with internal code 2599-N-21.
Consent to Participate: All patients in the study were informed of the study protocol and signed an informed consent approved by the Ethics Committee.
Consent for Publication: Not applicable.
Author Contributions: RCS, optometrist, was responsible for patient review (Observer 1) and the preparation of reports for teleophthalmology. Additionally, RCS designed the study, drafted the initial manuscript, and contributed to the review and editing of the final version.
RRG was responsible for the statistical design of the study, including the calculation of the sample size and Kappa concordance indices. RRG also participated in the review and editing of the final manuscript.
BPZ, senior ophthalmologist, contributed to the study design and served as an independent validator for interobserver comparisons. BPZ was not involved in the clinical evaluation of patients but reviewed discordant cases using standardized diagnostic criteria. He also reviewed and edited the final manuscript.
BMA, tele-ophthalmologist (Observer 2), evaluated patients based on the reports received from the optometrist.
MLV, in-person ophthalmologist (Observer 3), evaluated patients during in-person consultations, considered the gold standard in this study.
MGT, primary care physician, coordinated patient selection by applying the study’s inclusion criteria.
RMP participated in the drafting, editing, and evaluation of the main manuscript and contributed to the final review and editing.
ERR, senior ophthalmologist, also contributed to the study design and served as an independent validator of interobserver comparisons. Like BPZ, ERR was not involved in the clinical evaluation of patients but reviewed discordant cases using standardized diagnostic criteria. ERR also reviewed and edited the final manuscript.
Each author approved the final version of the manuscript to be published and participated sufficiently in the work to assume public responsibility for the corresponding portions of the content.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financed by RD21/0002/0011; financed by the Carlos III Health Institute from the Next Generation EU Funds, which finance the actions of the recovery and resilience mechanism (MRR) integrated in the PRTR.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data Availability Statement: Aggregated data will be available upon reasonable request to the corresponding author.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. O'Day R, Smith C, Muir J, Turner A. Optometric use of a teleophthalmology service in rural Western Australia: comparison of two prospective audits. Clin Exp Optom. 2016;99(2):163-167. doi: 10.1111/cxo.12334 [DOI] [PubMed] [Google Scholar]
- 2. Bartnik SE, Copeland SP, Aicken AJ, Turner AW. Optometry-facilitated teleophthalmology: an audit of the first year in Western Australia. Clin Exp Optom. 2018;101(5):700-703. doi: 10.1111/cxo.12658 [DOI] [PubMed] [Google Scholar]
- 3. Annoh R, Patel S, Beck D, Ellis H, Dhillon B, Sanders R. Digital ophthalmology in Scotland: benefits to patient care and education. Clin Ophthalmol. 2019;13:277-286. doi: 10.2147/OPTH.S185186. Published 2019 Feb 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jeganathan VS, Hall HN, Sanders R. Electronic referrals and digital imaging systems in ophthalmology: a global perspective. Asia Pac J Ophthalmol. 2017;6(1):3-7. doi: 10.22608/APO.2016110 [DOI] [PubMed] [Google Scholar]
- 5. Kern C, Fu DJ, Kortuem K, et al. Implementation of a cloud-based referral platform in ophthalmology: making telemedicine services a reality in eye care. Br J Ophthalmol. 2020;104(3):312-317. doi: 10.1136/bjophthalmol-2019-314161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Muttuvelu DV, Buchholt H, Nygaard M, Rasmussen MLR, Sim D. Danish teleophthalmology platform reduces optometry referrals into the national eye care system. BMJ Open Ophthalmol. 2021;6(1):e000671. doi: 10.1136/bmjophth-2020-000671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Portney DS, Zhu Z, Chen EM, et al. COVID-19 and use of teleophthalmology (CUT group): trends and diagnoses. Ophthalmology. 2021;128(10):1483-1485. doi: 10.1016/j.ophtha.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sharma M, Jain N, Ranganathan S, et al. Tele-ophthalmology: need of the hour. Indian J Ophthalmol. 2020;68(7):1328-1338. doi: 10.4103/ijo.IJO_1784_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mastropasqua L, D'Aloisio R, Mastrocola A, et al. Epidemiological surveillance of eye disease and people awareness in the Abruzzo region, Italy. Medicinar. 2021;57(9):978. doi: 10.3390/medicina57090978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Domínguez-Serrano FB, Molina-Solana P, Infante-Cossío M, Sala-Turrens J, Seva-Silva N, Rodríguez-de-la-Rúa-Franch E. Ophthalmological emergencies. An epidemiological study: are resources been used properly? Arch Soc Esp Oftalmol. 2019;94(5):211-217. doi: 10.1016/j.oftal.2019.01.007 [DOI] [PubMed] [Google Scholar]
- 11. Carrasco Solís R, Rodríguez Griñolo MR, Ponte Zúñiga B, et al. Analysis of patient referrals from primary care to ophthalmology. The role of the optometrist. J Optom. 2024;17(4):100521. doi: 10.1016/j.optom.2024.100521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sanidad MD. Portal estadístico. España: Área de Inteligencia de Gestión. Accessed January 15, 2024. https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/siae/siae/hospitales/actividad-asistencial/actividad-en-consultas. 2022. [in Spanish]. [Google Scholar]
- 13. Russell TG, Martin-Khan M, Khan A, Wade V. Method-comparison studies in telehealth: Study design and analysis considerations. J Telemed Telecare. 2017;23(9):797-802. doi: 10.1177/1357633X17727772 [DOI] [PubMed] [Google Scholar]
- 14. Flack VF, Afifi AA, Lachenbruch PA, Schouten HJA. Sample size determinations for the two rater kappa statistic. Psychometrika. 1988;53:321-325. doi: 10.1007/BF02294215 [DOI] [Google Scholar]
- 15. Bujang M, Baharum N. Guidelines of the minimum sample size requirements for Cohen’s Kappa. Epidemiol Biostat Public Health. 2017;14:e12267. doi: 10.2427/12267 [DOI] [Google Scholar]
- 16. Todd D, Bartlett H, Thampy R, Dhawahir-Scala F, Wilson H, Tromans C. Agreement in clinical decision-making between independent prescribing optometrists and consultant ophthalmologists in an emergency eye department. Eye. 2020;34(12):2284-2294. doi: 10.1038/s41433-020-0839-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mas-Tur V, Jawaid I, Poostchi A, Verma S. Optometrist referrals to an emergency ophthalmology department: a retrospective review to identify current practise and development of shared care working strategies, in England. Eye. 2021;35(5):1340-1346. doi: 10.1038/s41433-020-1049-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fung M, Myers P, Wasala P, Hirji N. A review of 1000 referrals to Walsall's hospital eye service. J Public Health. 2016;38(3):599-606. doi: 10.1093/pubmed/fdv081 [DOI] [PubMed] [Google Scholar]
- 19. Lundmark PO, Luraas K. Survey of referrals and medical reports in optometric practices in Norway: midterm findings from a 3-year prospective Internet-based study. Clin Optom. 2017;9:97-103. doi: 10.2147/OPTO.S136510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wright HR, Diamond JP. Service innovation in glaucoma management: using a web-based electronic patient record to facilitate virtual specialist supervision of a shared care glaucoma programme. Br J Ophthalmol. 2015;99(3):313-317. doi: 10.1136/bjophthalmol-2014-305588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Phu J, Wang H, Khuu SK, et al. Anterior chamber angle evaluation using gonioscopy: consistency and agreement between optometrists and ophthalmologists. Optom Vis Sci. 2019;96(10):751-760. doi: 10.1097/OPX.0000000000001432 [DOI] [PubMed] [Google Scholar]
- 22. Tahhan N, Ford BK, Angell B, et al. Evaluating the cost and wait-times of a task-sharing model of care for diabetic eye care: a case study from Australia. BMJ Open. 2020;10(10):e036842. doi: 10.1136/bmjopen-2020-036842. Published 2020 Oct 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McLaughlin CR, Biehl M, Chan BJ, et al. Ophthalmology referrals from optometry: a comparative study (the R.O.C.S study). Can J Ophthalmol. 2018;53(5):491-496. doi: 10.1016/j.jcjo.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 24. LaMonica LC, Bhardwaj MK, Hawley NL, et al. Remote screening for optic nerve cupping using smartphone-based nonmydriatic fundus photography. J Glaucoma. 2021;30(1):58-60. doi: 10.1097/IJG.0000000000001680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barrett C, O'Brien C, Loughman J. Glaucoma referral refinement in Ireland: managing the sensitivity-specificity paradox in optometric practice. Ophthalmic Physiol Opt. 2018;38(4):400-410. doi: 10.1111/opo.12446 [DOI] [PubMed] [Google Scholar]
- 26. Stewart C, Coffey-Sandoval J, Reid MW, Ho TC, Lee TC, Nallasamy S. Reliability of telemedicine for real-time paediatric ophthalmology consultations. Br J Ophthalmol. 2022;106(8):1157-1163. doi: 10.1136/bjophthalmol-2020-318385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ford BK, Angell B, Liew G, White AJ, Keay LJ. Improving patient access and reducing costs for glaucoma with integrated hospital and community care: a case study from Australia. Int J Integr Care. 2019;19(4):5. doi: 10.5334/ijic.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 29. Heidari S, Babor TF, De Castro P, Tort S, Curno M. Publisher correction: sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2024;9:2. doi: 10.1186/s41073-024-00155-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carnevali T, Southaphanh P. A retrospective study on presbyopia onset and progression in a Hispanic population. Optometry. 2005;76(1):37-46. doi: 10.1016/s1529-1839(05)70253-0 [DOI] [PubMed] [Google Scholar]
- 31. Schuster AK, Erb C, Hoffmann EM, Dietlein T, Pfeiffer N. The diagnosis and treatment of glaucoma. Dtsch Arztebl Int. 2020;117(13):225-234. doi: 10.3238/arztebl.2020.0225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gheorghe A, Mahdi L, Musat O. Age-related macular degeneration. Rom J Ophthalmol. 2015;59(2):74-77. [PMC free article] [PubMed] [Google Scholar]
- 33. Hugosson M, Ekström C. Prevalence and risk factors for age-related cataract in Sweden. Ups J Med Sci. 2020;125(4):311-315. doi: 10.1080/03009734.2020.1802375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28(1):98-103. doi: 10.1097/ICU.0000000000000340 [DOI] [PubMed] [Google Scholar]
- 35. Ophthalmology - Metro North Health. n.d. Accessed January 15, 2024. https://metronorth.health.qld.gov.au/specialist_service/refer-your-patient/ophthalmology
- 36. Optometry Wales Library. n.d. Accessed 15 January, 2024. https://www.optometrywales.org.uk/library
- 37. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806-808. doi: 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kottner J, Audigé L, Brorson S, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64(1):96-106. doi: 10.1016/j.jclinepi.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 39. Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJ. Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement [published correction appears in JAMA. 2006 Oct 18;296(15):1842]. JAMA. 2006;295(10):1152-1160. doi: 10.1001/jama.295.10.1152 [DOI] [PubMed] [Google Scholar]
- 40. Sevilla AD. Anuario estadístico de la ciudad de Sevilla. Accessed July 20, 2024. https://www.sevilla.org/servicios/servicio-de-estadistica/datos-estadisticos/anuarios/anuario-estadistico-de-la-ciudad-de-sevilla-2022/indice/capitulo-ii-poblacion. 2024. [in Spanish].
- 41. The Definition and Classification Subcommittee of the International Dry Eye Workshop (DEWS). The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye WorkShop (2007). Ocul Surf. 2007;5(2):75-92. doi: 10.1016/s1542-0124(12)70081-2 [DOI] [PubMed] [Google Scholar]
- 42. Fatehi F, Jahedi F, Tay-Kearney ML, Kanagasingam Y. Teleophthalmology for the elderly population: a review of the literature. Int J Med Inform. 2020;136:104089. doi: 10.1016/j.ijmedinf.2020.104089 [DOI] [PubMed] [Google Scholar]
- 43. Maa AY, Medert CM, Lu X, et al. Diagnostic accuracy of technology-based eye care services: the technology-based eye care services compare trial part I. Ophthalmology. 2020;127(1):38-44. doi: 10.1016/j.ophtha.2019.07.026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-2-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-3-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-1-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-4-inq-10.1177_00469580251367231 for Effective Validation of Primary Care Patient Triage Classification Via Tele-Ophthalmology With Optometrist Support by Rafael Carrasco Solís, Mª Rosario Rodríguez Griñolo, Beatriz Ponte Zúñiga, Beatriz Mataix Albert, María Leticia Lledó de Villar, María José González Troncoso, Rocío Martínez de Pablos and Enrique Rodríguez de La Rúa Franch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing


