Abstract
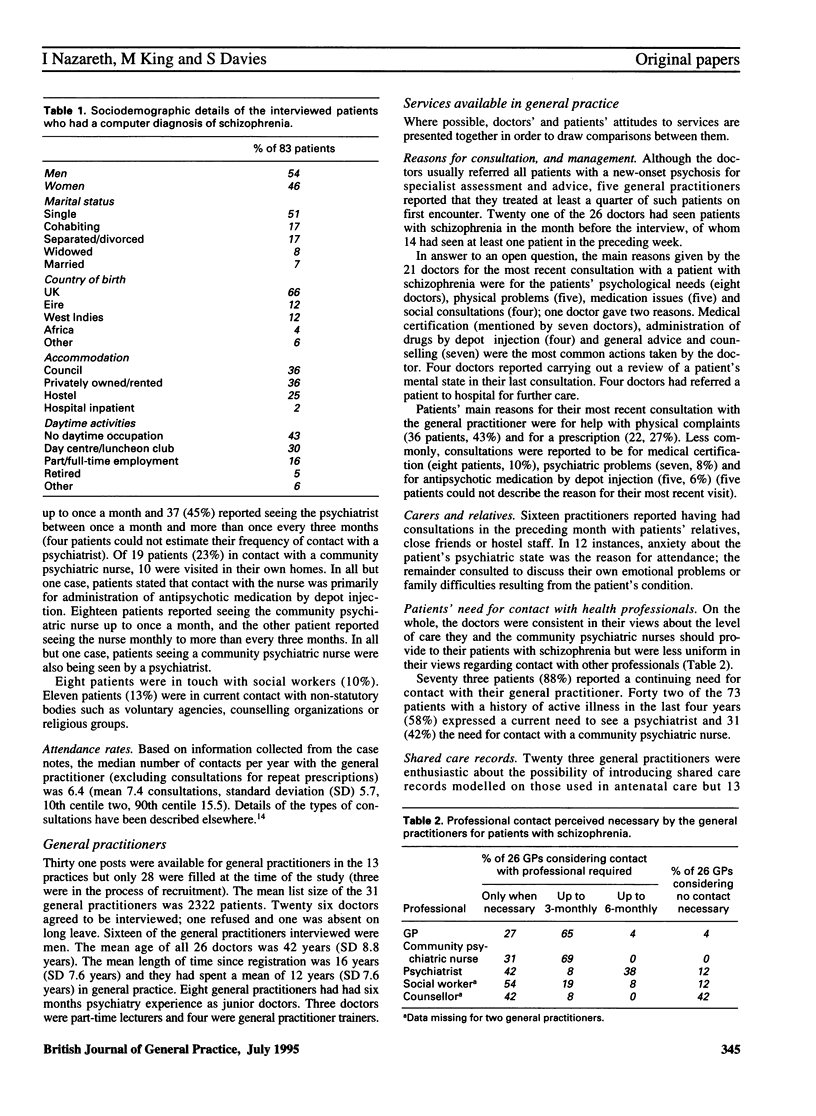
BACKGROUND. The transfer of patients with chronic schizophrenia from large mental hospitals into the community has had an impact on the role of the general practitioner in the effective delivery of primary care services to these patients. AIM. A study was undertaken to assess the care available in general practice for patients with schizophrenia, the attitudes of general practitioners and patients to the care provided and the factors influencing patients' use of services. METHOD. Eighty three patients with a diagnosis of schizophrenia and 26 doctors in 13 London practices registered on the VAMP research bank took part in a series of structured and semi-structured interviews. This was followed by a systematic examination of the patients' case notes. RESULTS. Only 14 patients (17%) had no active symptoms according to the present state examination interview and 52 (63%) were currently taking antipsychotic medication. Fifty three patients were in contact with a psychiatrist. Approximately one quarter of patients were visited by a community psychiatric nurse; in 18 of these 19 cases, the main reason for contact was reported to be for administration of medication by depot injection. In all but one case, patients seeing a community psychiatric nurse were also being seen by a psychiatrist. Sixteen doctors reported having had a consultation in the previous month with a patient's relative, friend or member of hostel staff. There were considerable differences between patients and their doctors in their attitudes to the use of services. Of the 26 general practitioners, 23 were enthusiastic about the possibility of introducing shared care records. Of the 54 patients in contact with a mental health professional, only 18 favoured the use of shared care records. Most of the doctors (19, 73%) reported they would welcome a psychiatric liaison service in their practice; 40% of 53 patients said they would not. Patients receiving antipsychotic drugs and patients registered with inner city practices attended their general practitioners more frequently than those not taking antipsychotic medication and those registered with suburban practices. Use of antipsychotic medication (adjusted odds ratio (OR) 8.2, 95% confidence interval (CI) 2.2 to 30.7, P < 0.01), male sex (OR 5.8, 95% CI 1.5 to 22.1, P < 0.01) and active symptoms on the present state examination (OR 4.1, 95% CI 1.0 to 17.5, P = 0.06) were all predictive of current contact with mental health professionals. CONCLUSION. Family doctors were closely involved with the care of patients with schizophrenia and their relatives and were eager for increased liaison with secondary care services. Although patients were more resistant than doctors to management innovations this may reflect lack of familiarity with changes in community services. Greater input is needed by mental health professionals, particularly community psychiatric nurses, and some consideration of the burden of care in inner city practices is necessary in health service planning.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J., Dayson D., Wills W., Gooch C., Margolius O., O'Driscoll C., Leff J. The TAPS Project. 13: Clinical and social outcomes of long-stay psychiatric patients after one year in the community. Br J Psychiatry Suppl. 1993 Apr;(19):45–56. [PubMed] [Google Scholar]
- Brewin C. R., Wing J. K., Mangen S. P., Brugha T. S., MacCarthy B. Principles and practice of measuring needs in the long-term mentally ill: the MRC needs for care assessment. Psychol Med. 1987 Nov;17(4):971–981. doi: 10.1017/s0033291700000787. [DOI] [PubMed] [Google Scholar]
- Briscoe M., Wilkinson G. General practitioners' use of community psychiatric nursing services: a preliminary survey. J R Coll Gen Pract. 1989 Oct;39(327):412–414. [PMC free article] [PubMed] [Google Scholar]
- Brown L. M., Tower J. E. Psychiatrists in primary care: would general practitioners welcome them? Br J Gen Pract. 1990 Sep;40(338):369–371. [PMC free article] [PubMed] [Google Scholar]
- Falloon I. R., Shanahan W., Laporta M., Krekorian H. A. Integrated family, general practice and mental health care in the management of schizophrenia. J R Soc Med. 1990 Apr;83(4):225–228. doi: 10.1177/014107689008300408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassall C., Stilwell J. A. Family-doctor support for patients on a psychiatric case register. J R Coll Gen Pract. 1977 Oct;27(183):605–608. [PMC free article] [PubMed] [Google Scholar]
- Horder E. Care for patients discharged from psychiatric hospital. Br J Gen Pract. 1991 Oct;41(351):399–400. [PMC free article] [PubMed] [Google Scholar]
- Jarman B. Underprivileged areas: validation and distribution of scores. Br Med J (Clin Res Ed) 1984 Dec 8;289(6458):1587–1592. doi: 10.1136/bmj.289.6458.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendell R. E. The future of Britain's mental hospitals. BMJ. 1989 Nov 18;299(6710):1237–1238. doi: 10.1136/bmj.299.6710.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick T., Sibbald B., Burns T., Freeling P. Role of general practitioners in care of long term mentally ill patients. BMJ. 1991 Mar 2;302(6775):508–510. doi: 10.1136/bmj.302.6775.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M. B. Psychological and social problems in HIV infection: interviews with general practitioners in London. BMJ. 1989 Sep 16;299(6701):713–717. doi: 10.1136/bmj.299.6701.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G., David A., Andréasson S., Allebeck P. Schizophrenia and city life. Lancet. 1992 Jul 18;340(8812):137–140. doi: 10.1016/0140-6736(92)93213-7. [DOI] [PubMed] [Google Scholar]
- Nazareth I., King M., Haines A., Rangel L., Myers S. Accuracy of diagnosis of psychosis on general practice computer system. BMJ. 1993 Jul 3;307(6895):32–34. doi: 10.1136/bmj.307.6895.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazareth I., King M., Haines A., Tai S. S., Hall G. Care of schizophrenia in general practice. BMJ. 1993 Oct 9;307(6909):910–910. doi: 10.1136/bmj.307.6909.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PARKES C. M., BROWN G. W., MONCK E. M. The general practitioner and the schizophrenic patient. Br Med J. 1962 Apr 7;1(5283):972–976. doi: 10.1136/bmj.1.5283.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pringle M. The new agenda for general practice computing. BMJ. 1990 Oct 13;301(6756):827–828. doi: 10.1136/bmj.301.6756.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullen I. M., Yellowlees A. J. Scottish psychiatrists in primary health-care settings. A silent majority. Br J Psychiatry. 1988 Nov;153:663–666. doi: 10.1192/bjp.153.5.663. [DOI] [PubMed] [Google Scholar]
- Shepherd M., Watt D., Falloon I., Smeeton N. The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychol Med Monogr Suppl. 1989;15:1–46. doi: 10.1017/s026418010000059x. [DOI] [PubMed] [Google Scholar]
- Strathdee G., King M. B., Araya R., Lewis S. A standardized assessment of patients referred to primary care and hospital psychiatric clinics. Psychol Med. 1990 Feb;20(1):219–224. doi: 10.1017/s0033291700013398. [DOI] [PubMed] [Google Scholar]
- Weller M. P., Tobiansky R., Hollander D. Destitution at the festive season. Lancet. 1989 Jan 28;1(8631):220–220. doi: 10.1016/s0140-6736(89)91237-3. [DOI] [PubMed] [Google Scholar]


