Abstract
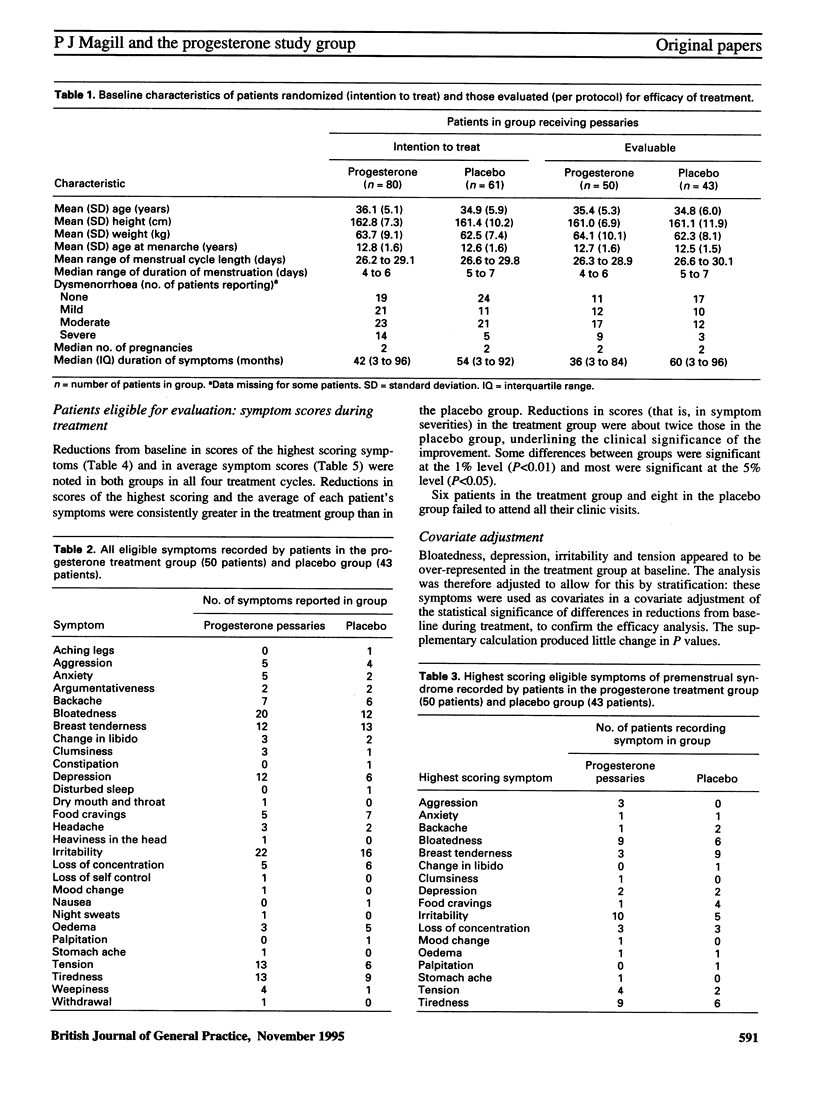
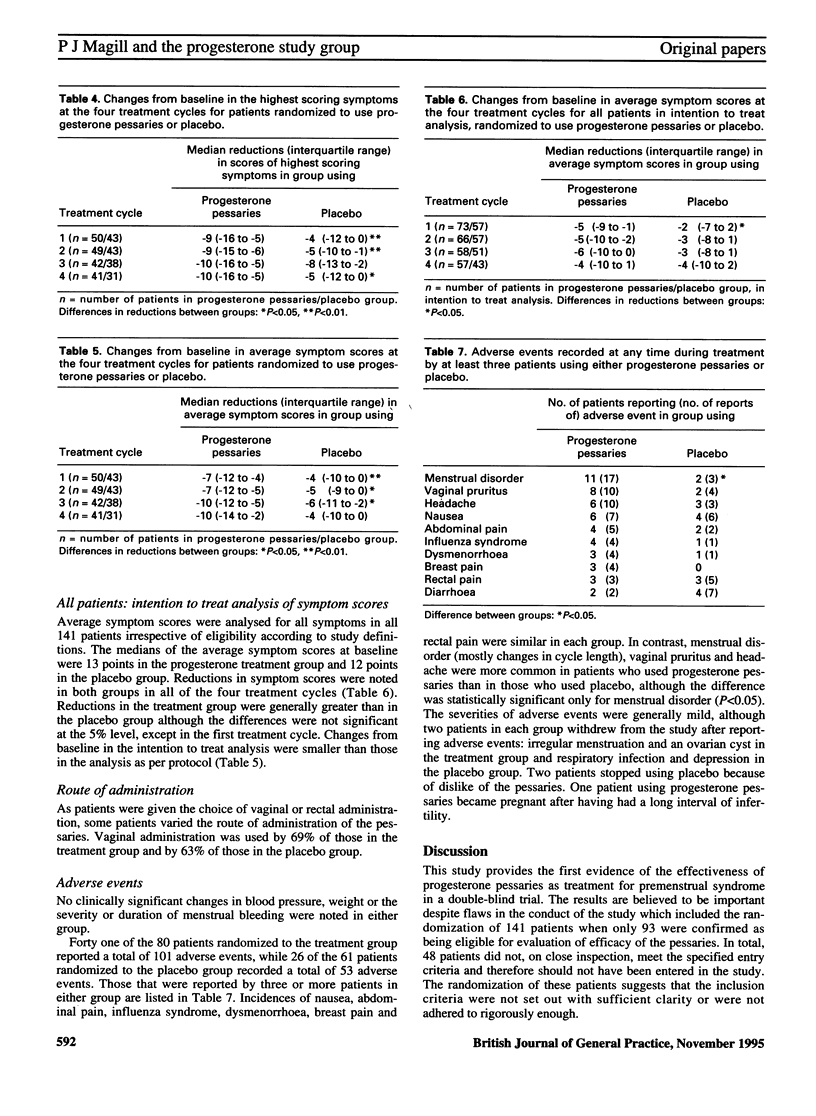
BACKGROUND. A variety of definitions have been applied to premenstrual syndrome. The severity of the syndrome is also variable. AIM. A study was undertaken to compare progesterone pessaries with placebo in the relief of symptoms of premenstrual syndrome. In this study the condition was characterized by a wide range of symptoms recurring in the late luteal phase but absent in the follicular phase (that is, the specific definition published by Dalton in 1953). METHOD. A multicentre, prospective, double-blind, randomized, parallel group study was undertaken by 45 general practitioners. Patients were deemed eligible after two prospective menstrual cycles of observation (selection phase) in which a precise definition of symptoms was applied. Patients were randomized to use either progesterone pessaries (400 mg twice a day) or matching placebo, by vaginal or rectal administration, from 14 days before the expected onset of menstruation until the onset of vaginal bleeding, for four consecutive cycles. Baseline data for the outcome variables were determined in the selection phase. The main outcome variables were changes in the severity (categorized as none, mild, moderate or severe) of each patient's most severe symptom, and in the average score of all the patient's symptoms characteristic of premenstrual syndrome. Spontaneous reports of adverse events were recorded. RESULTS. A total of 281 patients were screened for premenstrual syndrome; of these, 141 patients were randomized to treatment or placebo groups. Efficacy was evaluated in 93 patients. Reductions in the scores of the highest scoring, most severe, symptoms and in the average symptom score, were consistently observed in patients receiving progesterone pessaries and in those receiving placebo. The response to progesterone was greater than to placebo during each cycle; the differences were clinically and statistically significant. Adverse events were reported by 51% of patients in the progesterone treatment group and by 43% in the placebo group. Irregularity of menstruation, vaginal pruritus and headache were reported more frequently by patients taking active therapy. CONCLUSION. In this study, progesterone, given as pessaries by vaginal or rectal administration, was more effective than placebo in the relief of symptoms of premenstrual syndrome in a population of patients selected by strict entry criteria.
Full text
PDF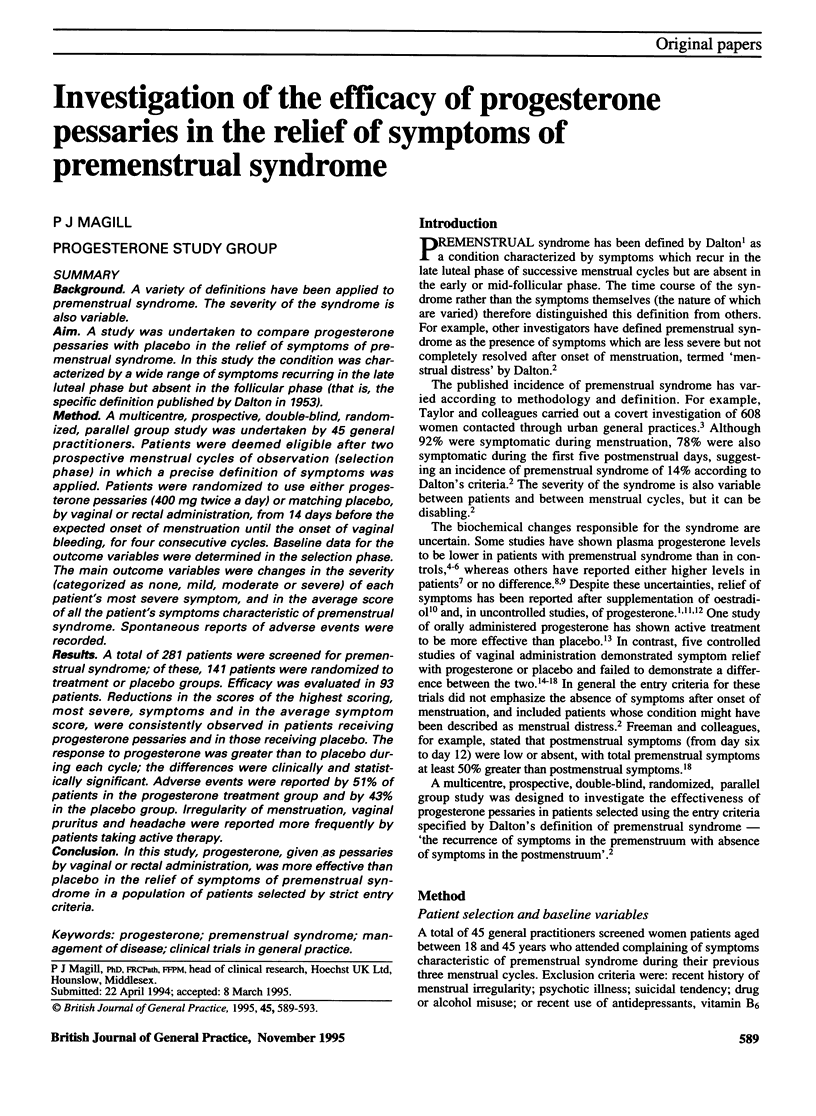


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersch B., Abrahamsson L., Wendestam C., Ohman R., Hahn L. Hormone profile in premenstrual tension: effects of bromocriptine and diuretics. Clin Endocrinol (Oxf) 1979 Dec;11(6):657–664. doi: 10.1111/j.1365-2265.1979.tb03121.x. [DOI] [PubMed] [Google Scholar]
- Bäckström T., Carstensen H. Estrogen and progesterone in plasma in relation to premenstrual tension. J Steroid Biochem. 1974 May;5(3):257–260. doi: 10.1016/0022-4731(74)90139-3. [DOI] [PubMed] [Google Scholar]
- Freeman E., Rickels K., Sondheimer S. J., Polansky M. Ineffectiveness of progesterone suppository treatment for premenstrual syndrome. JAMA. 1990 Jul 18;264(3):349–353. [PubMed] [Google Scholar]
- From the GMSC: Limited list: override procedure to be discussed. Br Med J (Clin Res Ed) 1985 Mar 30;290(6473):1017–1018. [PMC free article] [PubMed] [Google Scholar]
- Maddocks S., Hahn P., Moller F., Reid R. L. A double-blind placebo-controlled trial of progesterone vaginal suppositories in the treatment of premenstrual syndrome. Am J Obstet Gynecol. 1986 Mar;154(3):573–581. doi: 10.1016/0002-9378(86)90604-6. [DOI] [PubMed] [Google Scholar]
- Magos A. L., Brincat M., Studd J. W. Treatment of the premenstrual syndrome by subcutaneous estradiol implants and cyclical oral norethisterone: placebo controlled study. Br Med J (Clin Res Ed) 1986 Jun 21;292(6536):1629–1633. doi: 10.1136/bmj.292.6536.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. H. The development of a menstrual distress questionnaire. Psychosom Med. 1968 Nov-Dec;30(6):853–867. doi: 10.1097/00006842-196811000-00006. [DOI] [PubMed] [Google Scholar]
- Munday M. R., Brush M. G., Taylor R. W. Correlations between progesterone, oestradiol and aldosterone levels in the premenstrual syndrome. Clin Endocrinol (Oxf) 1981 Jan;14(1):1–9. doi: 10.1111/j.1365-2265.1981.tb00359.x. [DOI] [PubMed] [Google Scholar]
- O'Brien P. M., Selby C., Symonds E. M. Progesterone, fluid, and electrolytes in premenstrual syndrome. Br Med J. 1980 May 10;280(6224):1161–1163. doi: 10.1136/bmj.280.6224.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- REES L. Psychosomatic aspects of the premenstrual tension syndrome. J Ment Sci. 1953 Jan;99(414):62–73. doi: 10.1192/bjp.99.414.62. [DOI] [PubMed] [Google Scholar]
- Sampson G. A. Premenstrual syndrome: a double-blind controlled trial of progesterone and placebo. Br J Psychiatry. 1979 Sep;135:209–215. doi: 10.1192/bjp.135.3.209. [DOI] [PubMed] [Google Scholar]
- Steiner M., Haskett R. F., Carroll B. J. Premenstrual tension syndrome: the development of research diagnostic criteria and new rating scales. Acta Psychiatr Scand. 1980 Aug;62(2):177–190. doi: 10.1111/j.1600-0447.1980.tb00605.x. [DOI] [PubMed] [Google Scholar]
- Taylor J. W. Plasma progesterone, oestradiol 17 beta and premenstrual symptoms. Acta Psychiatr Scand. 1979 Jul;60(1):76–86. doi: 10.1111/j.1600-0447.1979.tb00267.x. [DOI] [PubMed] [Google Scholar]
- Taylor R. J., Alexander D. A., Fordyce I. D. A survey of paramenstrual complaints by covert and by overt methods. J R Coll Gen Pract. 1986 Nov;36(292):496–499. [PMC free article] [PubMed] [Google Scholar]


