Abstract
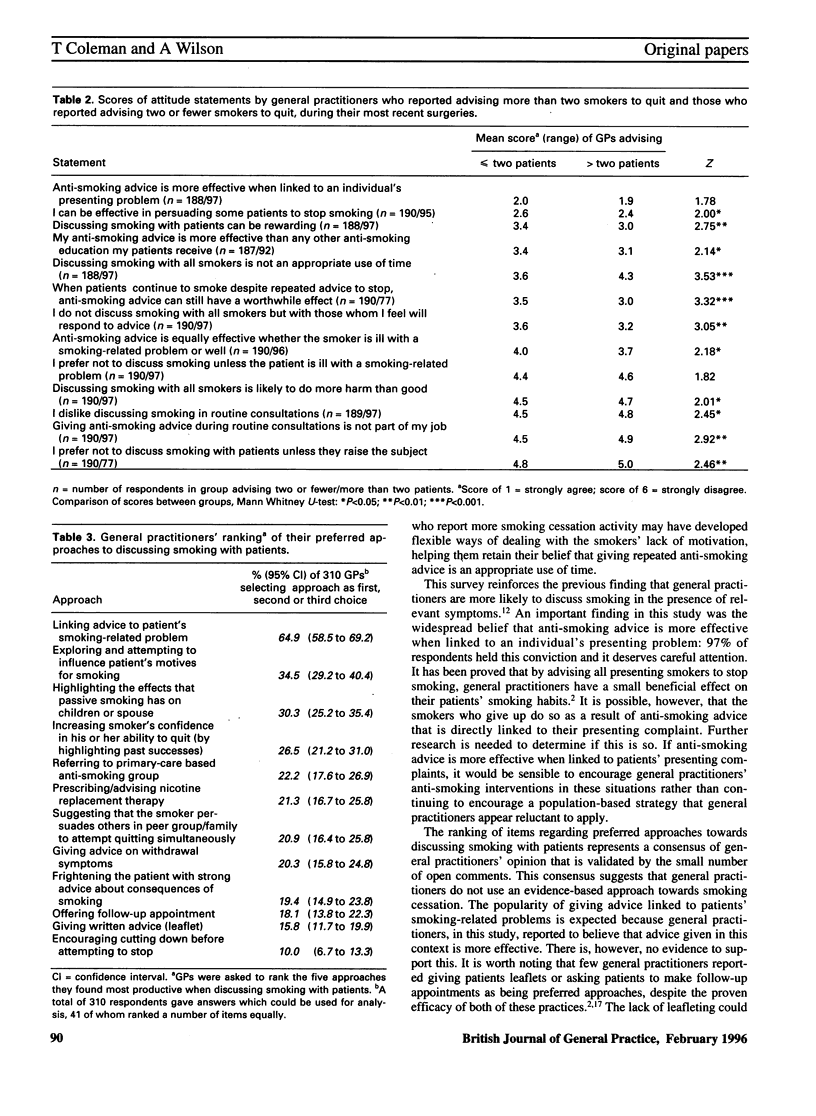
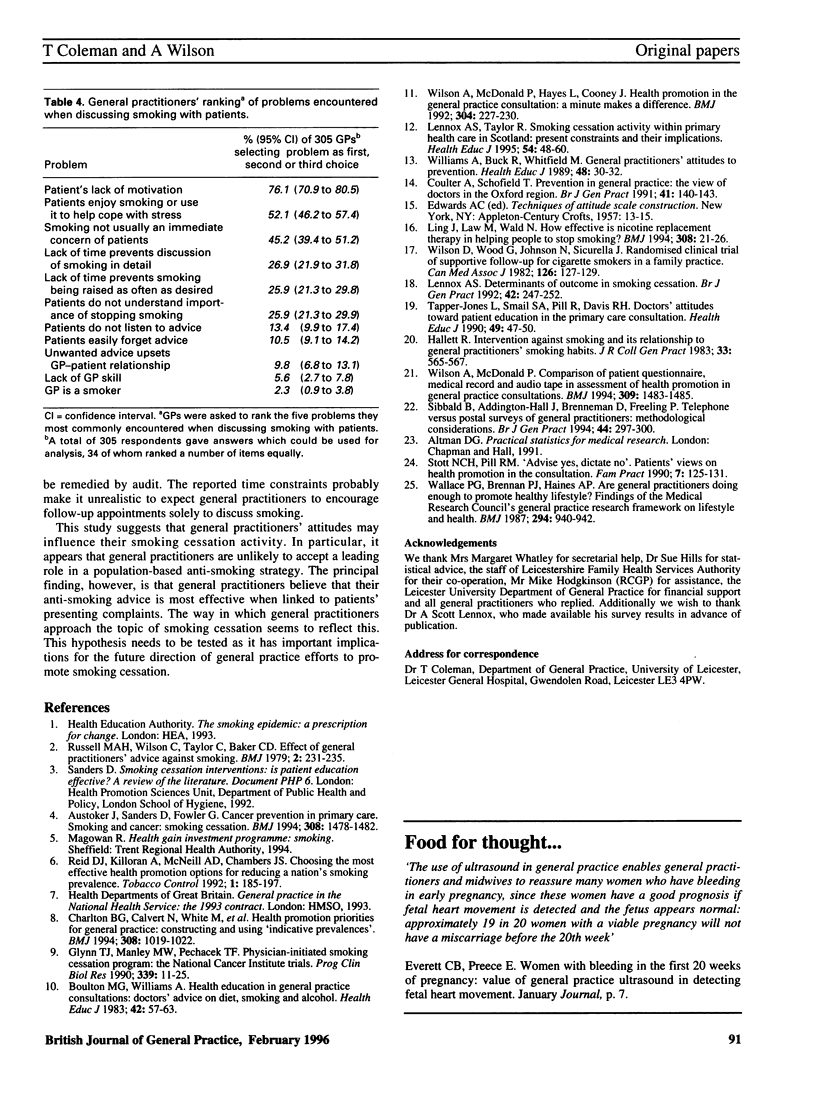
BACKGROUND: Anti-smoking advice from general practitioners has proven efficacy. However, general practitioners do not exploit a large proportion of opportunities to discuss smoking with patients. AIM: A study aimed to explore general practitioners attitudes towards discussing smoking with patients and to assess how these influence the quantity of anti-smoking advice that general practitioners report giving during routine consultations. It also aimed to determine the extent to which general practitioners report using evidence-based interventions against smoking and to discover the problems they experience when discussing smoking with patients. METHOD: A postal survey of all 468 general practitioners on the Leicestershire Family Health Services Authority list was conducted. General practitioners' attitudes were assessed by scoring 13 attitude statements using a six-point Likert-type scale. They were also asked to rank (from a list of 12 items) the five approaches that they found most productive and (from a list of 11 items) the five problems that they most commonly encountered when giving anti-smoking advice to patients. RESULTS: A total of 327 questionnaires (70%) were returned. Most respondents (97%) thought that their advice was more effective when linked to patients' presenting problems and 65% reported that linking their anti-smoking advice to patients' presenting complaints was one of their three most preferred approaches to discussing smoking. Advising all presenting smokers to quit was considered by 40% of respondents to be an appropriate use of time but 76% reported that patients' lack of motivation was one of the three most commonly encountered problems. An analysis of the ratings of the 13 statements suggested that general practitioners who reported the greatest smoking cessation activity during routine consultations held more positive attitudes towards discussing smoking with patients. CONCLUSION: This study suggests that general practitioners believe that their anti-smoking advice is more effective when linked to patients' presenting complaints, and this belief appears to be reflected in the way in which general practitioners approach smoking cessation with patients. The findings may indicate that general practitioners are unlikely to accept a role in a population-based anti-smoking strategy which demands that they discuss smoking with all presenting smokers.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Austoker J., Sanders D., Fowler G. Smoking and cancer: smoking cessation. BMJ. 1994 Jun 4;308(6942):1478–1482. doi: 10.1136/bmj.308.6942.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulton M. G., Williams A. Health education in the general practice consultation: doctors' advice on diet, alcohol and smoking. Health Educ J. 1983;42(2):57–63. doi: 10.1177/001789698304200211. [DOI] [PubMed] [Google Scholar]
- Charlton B. G., Calvert N., White M., Rye G. P., Conrad W., van Zwanenberg T. Health promotion priorities for general practice: constructing and using "indicative prevalences". BMJ. 1994 Apr 16;308(6935):1019–1022. doi: 10.1136/bmj.308.6935.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter A., Schofield T. Prevention in general practice: the views of doctors in the Oxford region. Br J Gen Pract. 1991 Apr;41(345):140–143. [PMC free article] [PubMed] [Google Scholar]
- Glynn T. J., Manley M. W., Pechacek T. F. Physician-initiated smoking cessation program: the National Cancer Institute trials. Prog Clin Biol Res. 1990;339:11–25. [PubMed] [Google Scholar]
- Hallett R. Intervention against smoking and its relationship to general practitioners' smoking habits. J R Coll Gen Pract. 1983 Sep;33(254):565–567. [PMC free article] [PubMed] [Google Scholar]
- Lennox A. S. Determinants of outcome in smoking cessation. Br J Gen Pract. 1992 Jun;42(359):247–252. [PMC free article] [PubMed] [Google Scholar]
- Russell M. A., Wilson C., Taylor C., Baker C. D. Effect of general practitioners' advice against smoking. Br Med J. 1979 Jul 28;2(6184):231–235. doi: 10.1136/bmj.2.6184.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibbald B., Addington-Hall J., Brenneman D., Freeling P. Telephone versus postal surveys of general practitioners: methodological considerations. Br J Gen Pract. 1994 Jul;44(384):297–300. [PMC free article] [PubMed] [Google Scholar]
- Stott N. C., Pill R. M. 'Advise yes, dictate no'. Patients' views on health promotion in the consultation. Fam Pract. 1990 Jun;7(2):125–131. doi: 10.1093/fampra/7.2.125. [DOI] [PubMed] [Google Scholar]
- Tang J. L., Law M., Wald N. How effective is nicotine replacement therapy in helping people to stop smoking? BMJ. 1994 Jan 1;308(6920):21–26. doi: 10.1136/bmj.308.6920.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace P. G., Brennan P. J., Haines A. P. Are general practitioners doing enough to promote healthy lifestyle? Findings of the Medical Research Council's general practice research framework study on lifestyle and health. Br Med J (Clin Res Ed) 1987 Apr 11;294(6577):940–942. doi: 10.1136/bmj.294.6577.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson A., McDonald P. Comparison of patient questionnaire, medical record, and audio tape in assessment of health promotion in general practice consultations. BMJ. 1994 Dec 3;309(6967):1483–1485. doi: 10.1136/bmj.309.6967.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson A., McDonald P., Hayes L., Cooney J. Health promotion in the general practice consultation: a minute makes a difference. BMJ. 1992 Jan 25;304(6821):227–230. doi: 10.1136/bmj.304.6821.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson D., Wood G., Johnston N., Sicurella J. Randomized clinical trial of supportive follow-up for cigarette smokers in a family practice. Can Med Assoc J. 1982 Jan 15;126(2):127–129. [PMC free article] [PubMed] [Google Scholar]


