Abstract
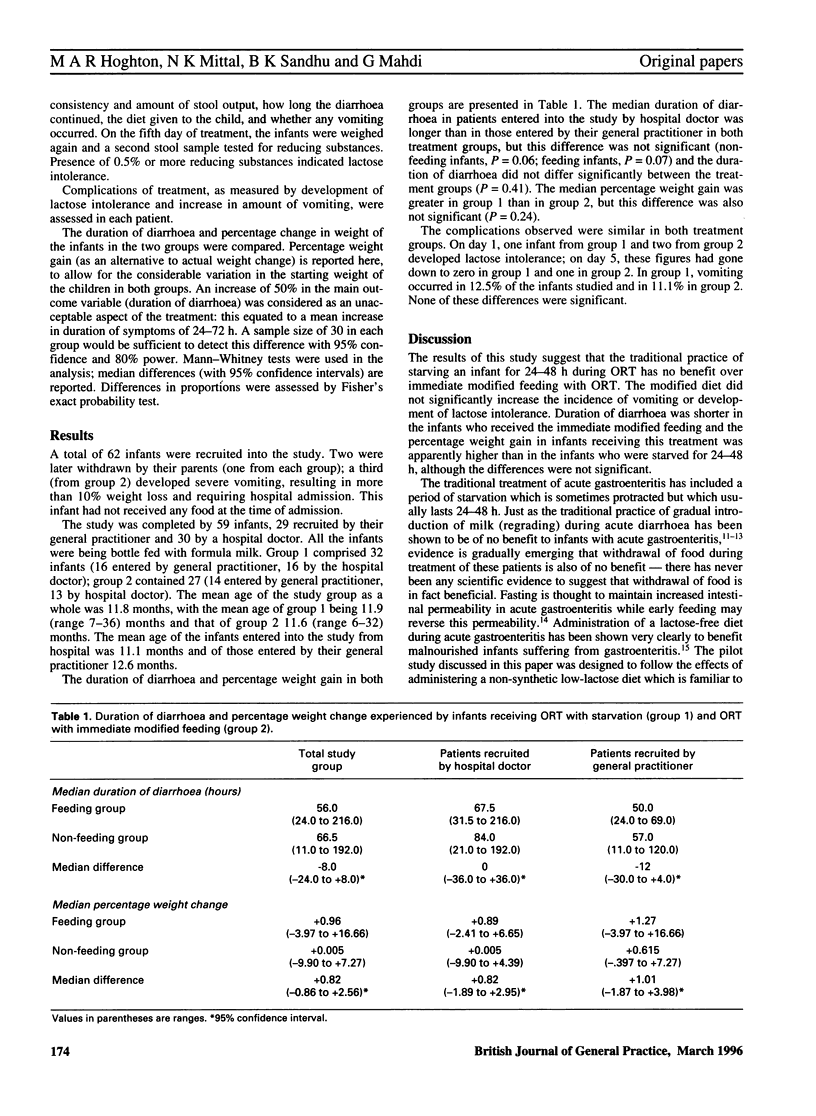
BACKGROUND: Standard treatment of infants who are dehydrated as a result of acute gastroenteritis is to administer oral rehydration therapy (ORT). Traditionally, food has been withdrawn for 24-48 h, but there is no conclusive evidence that this is of any real benefit to the patient. Immediate modified feeding, in which an infant on ORT is not starved but administered a limited diet, may have benefits in the treatment of gastroenteritis, especially in children who are nutritionally compromised before they develop the illness. AIM: A pilot study was carried out to investigate the effects of giving infants suffering from acute gastroenteritis a limited modified diet in conjunction with ORT. METHOD: Infants recruited into the study by their general practitioner or by a research doctor in the hospital casualty unit of Bristol Children's Hospital were randomly allocated to receive ORT with or without immediate modified feeding. The duration of diarrhoea, weight change, and incidence of vomiting and lactose intolerance were measured in both treatment groups, and the results were compared. RESULTS: Of the infants studied, 27 received ORT and immediate modified feeding, and 32 ORT alone. The duration of diarrhoea, and incidence of vomiting or lactose intolerance were no greater in the group receiving immediate modified feeding. Patients who received ORT and immediate modified feeding appeared to gain more weight than the infants who were starved for 24-48 h, but this difference was not statistically significant. CONCLUSION: Immediate modified feeding is safe and effective, and may have nutritional advantages over traditional ORT with starvation. A similar but multicentre study using unmodified diet, i.e. child's normal diet, is being carried out by a working group of The European Society of Paediatrics, Gastroenterology and Nutrition (ESPGAN).
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avery M. E., Snyder J. D. Oral therapy for acute diarrhea. The underused simple solution. N Engl J Med. 1990 Sep 27;323(13):891–894. doi: 10.1056/NEJM199009273231307. [DOI] [PubMed] [Google Scholar]
- Brown K. H., Gastañaduy A. S., Saavedra J. M., Lembcke J., Rivas D., Robertson A. D., Yolken R., Sack R. B. Effect of continued oral feeding on clinical and nutritional outcomes of acute diarrhea in children. J Pediatr. 1988 Feb;112(2):191–200. doi: 10.1016/s0022-3476(88)80055-6. [DOI] [PubMed] [Google Scholar]
- Conway S. P., Ireson A. Acute gastroenteritis in well nourished infants: comparison of four feeding regimens. Arch Dis Child. 1989 Jan;64(1):87–91. doi: 10.1136/adc.64.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodburn E., Mattosinho S., Mongi P., Waterston T. Management of childhood diarrhoea by pharmacists and parents: is Britain lagging behind the Third World? BMJ. 1991 Feb 23;302(6774):440–443. doi: 10.1136/bmj.302.6774.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore S. M., Fontaine O., Pierce N. F. Impact of rice based oral rehydration solution on stool output and duration of diarrhoea: meta-analysis of 13 clinical trials. BMJ. 1992 Feb 1;304(6822):287–291. doi: 10.1136/bmj.304.6822.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isolauri E., Juntunen M., Wiren S., Vuorinen P., Koivula T. Intestinal permeability changes in acute gastroenteritis: effects of clinical factors and nutritional management. J Pediatr Gastroenterol Nutr. 1989 May;8(4):466–473. doi: 10.1097/00005176-198905000-00008. [DOI] [PubMed] [Google Scholar]
- Isolauri E., Vesikari T., Saha P., Viander M. Milk versus no milk in rapid refeeding after acute gastroenteritis. J Pediatr Gastroenterol Nutr. 1986 Mar-Apr;5(2):254–261. [PubMed] [Google Scholar]
- Molla A. M., Molla A., Nath S. K., Khatun M. Food-based oral rehydration salt solution for acute childhood diarrhoea. Lancet. 1989 Aug 19;2(8660):429–431. doi: 10.1016/s0140-6736(89)90601-6. [DOI] [PubMed] [Google Scholar]
- Nalin D. R., Levine M. M., Mata L., de Céspedes C., Vargas W., Lizano C., Loria A. R., Simhon A., Mohs E. Oral rehydration and maintenance of children with rotavirus and bacterial diarrhoeas. Bull World Health Organ. 1979;57(3):453–459. [PMC free article] [PubMed] [Google Scholar]
- Patra F. C., Mahalanabis D., Jalan K. N., Sen A., Banerjee P. Is oral rice electrolyte solution superior to glucose electrolyte solution in infantile diarrhoea? Arch Dis Child. 1982 Dec;57(12):910–912. doi: 10.1136/adc.57.12.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajah R., Pettifor J. M., Noormohamed M., Venter A., Rosen E. U., Rabinowitz L., Stein H. The effect of feeding four different formulae on stool weights in prolonged dehydrating infantile gastroenteritis. J Pediatr Gastroenterol Nutr. 1988 Mar-Apr;7(2):203–207. doi: 10.1097/00005176-198803000-00008. [DOI] [PubMed] [Google Scholar]
- Recommendations for composition of oral rehydration solutions for the children of Europe. Report of an ESPGAN Working Group. J Pediatr Gastroenterol Nutr. 1992 Jan;14(1):113–115. [PubMed] [Google Scholar]
- Rees L., Brook C. G. Gradual reintroduction of full-strength milk after acute gastroenteritis in children. Lancet. 1979 Apr 7;1(8119):770–771. doi: 10.1016/s0140-6736(79)91220-0. [DOI] [PubMed] [Google Scholar]
- Santosham M., Fayad I. M., Hashem M., Goepp J. G., Refat M., Sack R. B. A comparison of rice-based oral rehydration solution and "early feeding" for the treatment of acute diarrhea in infants. J Pediatr. 1990 Jun;116(6):868–875. doi: 10.1016/s0022-3476(05)80642-0. [DOI] [PubMed] [Google Scholar]
- el-Mougi M., Hegazi E., Galal O., el Akkad N., el-Abhar A., Nour N., el-Hadi Emam M., Ahmadi A. R. Controlled clinical trial on the efficacy of rice powder-based oral rehydration solution on the outcome of acute diarrhea in infants. J Pediatr Gastroenterol Nutr. 1988 Jul-Aug;7(4):572–576. doi: 10.1097/00005176-198807000-00016. [DOI] [PubMed] [Google Scholar]


