Abstract
Introduction:
E-learning is increasingly replacing traditional methods in medical science education. The main purpose of this study is to identify opportunities, threats and required components of E-learning in nursing education.
Methods:
We conducted a comprehensive systematic review following Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines, searching Web of Science, Scopus, ProQuest, Cochrane Library, ScienceDirect, Medline/PubMed, Google Scholar, and SID, Irandoc, and Magiran databases without time or language restrictions. Two researchers assessed each systematic review using A Measurement Tool to assess systematic Reviews (AMSTAR). This overview includes 47 reviews published until the end of 2022.
Results:
Electronic education in nursing offers opportunities categorized into 10 areas: accessibility and flexibility, efficiency and effectiveness, strengthening clinical competencies, features of electronic education, improving educational processes, improving the quality of education, evaluation and feedback, diversity and practically of content, setting learning environment and promotion of nursing professors’ role. However, there are also challenges, grouped into 10 categories: challenges of evaluation and feedback, problems related to the of human resources development, structural and technical limitations, challenges related to communication and interaction, challenges related to the content of education, financial challenges, organizational challenges, cultural challenges, challenges of professional competence, challenges of ethics and information security. The essential components for effective electronic teaching in nursing education are organized into 6 categories: technological infrastructure, human infrastructure, pedagogical infrastructure, cultural and social infrastructure, economic infrastructure, and management and leadership infrastructure.
Conclusion:
E-learning offers an efficient and effective training method for nurses that should be embraced given advances in science and technology. Addressing infrastructure limitations will further enhance its benefits.
Keywords: E-Learning, Nursing education, Systematic review, Online education
Introduction
The digital transformation of education and information technology has established smart learning environments worldwide. The online education market is projected to reach $325 billion by 2025, tripling its value since 2015.1 Consequently, organizations, universities, researchers, and educators are increasingly focusing on educational technologies.2 The COVID-19 pandemic forced classroom closures globally, presenting unprecedented challenges, particularly in health science education, which had to shift to remote learning to protect medical and nursing students from potential COVID-19 exposure. This sudden transition affected 1.5 billion students and 63 million educators, revealing both strengths and weaknesses in educational systems amidst digitalization.3
E-learning in medical education is rapidly gaining ground as a viable alternative to traditional methods.4 A 2018 Cochrane review indicated that e-learning’s effectiveness is similar to traditional teaching, while other studies highlight numerous advantages, including on-demand access, control over content quality, and learning analytics.5 Nursing students must acquire the competencies required for safe, compassionate, and ethical care across various settings.6 Nursing education is also characterized by continuous professional development, promoting lifelong learning.7
Integrating innovative techniques not only enhances clinical learning within limited time frames but also supports nurses’ self-directed training and skill enhancement.6,8 Given that nurses constitute one of the largest professional groups in healthcare, it is crucial to investigate e-learning extensively within this field.6Most pre-COVID-19 studies on nursing e-learning primarily focused on participant satisfaction rather than skill improvement or changes in practice post-intervention.9,10 A pre-pandemic review of the field was not comprehensive in addressing e-learning’s opportunities and challenges.11,12 Therefore, with the shift toward electronic education and its cost-effectiveness, as well as the long-term impacts of crises like COVID-19, there is a pressing need for a new review of existing studies. This research aims to identify opportunities, threats and required components of E-learning in nursing education.
Material and Methods
This overview aims to identify the opportunities and threats of e-learning in nursing education based on the PRISMA systematic review and meta-analysis protocol. The structured questionnaire (PICOS) encompasses the following elements: Participants (nursing students, clinical nurses, professors, and instructors), Intervention (e-learning), Comparisons (traditional educational methods), Outcomes (opportunities, threats, and influencing factors), and Study Design (review studies with or without meta-analysis). A comprehensive and regular search without time and language restrictions was conducted in Web of Science, Scopus, ProQuest, Cochrane library, Science Direct, Medline/PubMed and Google Scholar and SID, Irandoc and Magiran database. In each of the databases, depending on how to search, articles were retrieved using the following keywords: (“e-learning” OR “digital learning” OR “Web-based learning” OR “online learning” OR “distributed learning” OR “computer assisted instruction” OR “Internet-based learning” OR “virtual mentor” OR “virtual learning”) AND (“healthcare education,” “medical education,” “nursing education”) (“computer” OR “web” OR “internet” OR “online” OR “information technology” OR “mobile” OR “phone*” OR “personal digital assistant*” OR “handheld*” OR “tablet*”) AND (“learning” OR “education” OR “instruction” OR “problem solving”) AND (“nurse* student*” OR “student* nurse *”). The period of retrieval and search of articles was unlimited, and considering the inclusion criteria, articles published until the end of 2022 were included in the study. There were no restrictions on language.
Eligibility criteria included studies that examined the opportunities and threats of learning in nursing education, specifically those involving nursing students and faculty, or those involving healthcare professionals that included nurses. Non-review studies and those irrelevant to the objectives were excluded. The PRISMA flowchart (Figure 1) illustrates the article selection process. Based on the initial search, 790 articles were retrieved, after reviewing the titles and abstracts, 489 articles were removed and 301 articles remained. In the re-examination and based on the inclusion criteria, 83 articles were excluded, and after qualitative assessment, 47 articles were identified that addressed the challenges, opportunities, and essential components of electronic education in nursing. Two researchers independently conducted the searching and screening, resolving any disputes with a third researcher. Finally, data was extracted into a form that included the article’s author, year of publication, title, purpose, type of review, results, and quality evaluation score. Each systematic review was assessed by two reviewers using A Measurement Tool to assess systematic Reviews (AMSTAR), which consists of 11 questions scored as Yes (1) or No (0). Scores of 8-11 indicate high quality, 4-7 medium quality, and 0-3 low quality.13
Figure 1.

PRISMA flow diagram
Results
In this overview of reviews study which is a comprehensive review of systematic reviews, three categories of results were extracted under the headings of advantages or opportunities, challenges or disadvantages, and required components of e-learning in nursing education. The first category, shown in Table 1, presents the opportunities or advantages of e-learning in nursing education. The second category, shown in Table 2, presents the challenges or disadvantages of e-learning in nursing education. The third category, shown in Table 3, presents the required components of e-learning in nursing education. All articles from 47 systematic reviews published between 2006 and 2022 were reviewed, and the characteristics of the studies reviewed are summarized in Table 4. This table lists characteristics such as first author, year of publication, purpose of the study, database searched, electronic training, and participants. The diversity of keywords of the selected studies is shown in Figure 2. As can be seen, the concepts of electronic education in nursing have gained more strength since 2014. In Figure 3, the names of authors who collaborated on different studies are displayed. The opportunities and benefits of electronic education in nursing education were obtained in 10 categories with the titles: accessibility and flexibility, efficiency and effectiveness, strengthening clinical competencies, features of electronic education, improving educational processes, improving the quality of education, evaluation and feedback, diversity and practically of content, setting learning environment and promotion of nursing professors’ role. The highest level of impact was related to the benefits of “accessibility and flexibility” with a score of 68, and the lowest was related to “learning environment” and “promotion of nursing professors’ role” with a score of 5. The advantages are presented in Figure 4. Challenges and disadvantages of electronic education in nursing education were obtained in 10 categories with the titles: challenges of evaluation and feedback, problems related to the of human resources development, structural and technical limitations, challenges related to communication and interaction, challenges related to the content of education, financial challenges, organizational challenges, cultural challenges, challenges of professional competence, challenges of ethics and information security. The highest level of impact on disadvantages was related to “challenges related to communication and interaction” with a score of 59, and the lowest was related to “organizational challenges” and “challenges ethics and information security” with a score of 4. Disadvantages are introduced in Figure 5. The required components of electronic teaching in nursing education were obtained in 6 floors with the titles: technological infrastructure, human infrastructure, pedagogical infrastructure, cultural and social infrastructure, economic infrastructure, management and leadership infrastructure. The highest level of impact in the required components is related to “Management and Leadership Infrastructure” with a score of 53 and the lowest is related to “Economic Infrastructure” with a score of 6. The required components are introduced in Figure 6.
Table 1. The opportunities or advantages of e-learning in nursing education .
| Parameters | Total percent | Impact rate | N (%) | Items | References |
| Accessibility and flexibility | 26.7 | 68 | 7 (2.7) | Access to a wide range of international knowledge and information | 14-20 |
| 31 (12.2) | Easy accessibility | 14-18,20-45 | |||
| 4 (1.6) | Accessible to a larger audience | 16,31,39,45 | |||
| 26 (10.2) | Flexibility in terms of time and place | 14,15,17-19,21-26,28,30,31,33-35,37,39,43,45-48 | |||
| Efficiency and effectiveness | 12.5 | 32 | 27 (10.6) | Cost-effectiveness | 15,17-19,21-26,28,30-37,39,42-45,47,49,50 |
| 5 (2.0) | Efficiency in time and cost | 14,27,29,43,50 | |||
| Strengthening clinical competencies | 25.1 | 63 | 53 (20.8) | Development of professional and clinical skills | 14,26,51-53 |
| 3 (1.2) | Strengthen critical thinking | 14,43,48 | |||
| 2 (0.8) | Strengthen cognitive skills | 14,48 | |||
| 2 (0.8) | Personal and professional growth | 14,48 | |||
| 2 (0.8) | Development of communication skills | 8,43 | |||
| 1 (0.4) | Development of clinical competencies | 54 | |||
| 1 (0.4) | Self-efficacy in performing nursing skills | 55 | |||
| Features of electronic education | 13.7 | 35 | 1 (0.4) | Completion of traditional education | 14 |
| 14 (5.5) | Self-directed learning | 14,17,20,22,28,31,33,36-39,43,46,56 | |||
| 18 (7.1) | Interactive and engaging learning experience | 15,17,18,20-22,25,30,31,34,35,37-40,45,47,49 | |||
| 2 (0.8) | Personal and spontaneous interaction between teacher and learner | 22,31 | |||
| Improving educational processes | 5.5 | 14 | 2 (0.8) | Reduce training time | 29,43 |
| 1 (0.4) | Providing continuous training | 31 | |||
| 2 (0.8) | Educational support and variety in it | 19,57 | |||
| 1 (0.4) | Facilitate individual training programs | 38 | |||
| 2 (0.8) | Responding to individual learning needs | 20,45 | |||
| 1 (0.4) | Facilitate the learning process | 41 | |||
| 5 (2.0) | Independence in learning | 14,28,31,40,58 | |||
| Improving the quality of education | 1.6 | 4 | 1 (0.4) | Achieving goals in the cognitive field | 31 |
| 1 (0.4) | Enhancing and encouraging learning in nursing education | 54 | |||
| 2 (0.8) | Bridging the gap between theory and practice | 43,51 | |||
| Evaluation and feedback | 6.3 | 16 | 3 (1.2) | Evaluating and closely monitoring the progress and performance of students | 26,30,59 |
| 2 (0.8) | Provide quick and immediate feedback to students | 15,51 | |||
| 2 (0.8) | Use of online assessment and test tools | 19,57 | |||
| 1 (0.4) | Self-assessment by the learner | 37,57 | |||
| 1 (0.4) | Providing detailed statistics and reports about student performance | 19 | |||
| 7 (2.7) | Student satisfaction | 29,32,40,55,56,58,59 | |||
| Diversity and practicality of content | 4.7 | 12 | 1 (0.4) | Access to various multimedia content | 18 |
| 1 (0.4) | Improve content and format | 46 | |||
| 1 (0.4) | Attractive content | 46 | |||
| 1 (0.4) | Communicate with content | 46 | |||
| 1 (0.4) | Utilization of content learning | 46 | |||
| 1 (0.4) | Standardized content | 35 | |||
| 1 (0.4) | Integrating nursing information and information into the curriculum | 21 | |||
| 1 (0.4) | Content focus on practical and communication skills in real situations | 26 | |||
| 1 (0.4) | The possibility of providing practical lessons virtually | 37,39,57 | |||
| 1 (0.4) | Providing up-to-date and new content with fast update capability | 18,21 | |||
| 2 (0.8) | Publish and share content with greater speed and breadth | 22,27 | |||
| Setting learning environment | 2.0 | 5 | 2 (0.8) | Information-based, interactive and constructivist learning environment | 18,31 |
| 1 (0.4) | Providing virtual reality conditions for training in job-related fields | 26 | |||
| 1 (0.4) | Creating a challenging learning environment | 52 | |||
| 1 (0.4) | Reduce noise pollution | 58 | |||
| Promotion of nursing professors' role | 2.0 | 5 | 1 (0.4) | Personal and professional growth of professors | 14 |
| 2 (0.8) | Promoting communication and cooperation between nursing professors | 23,27 | |||
| 1 (0.4) | Promoting the leadership role of nursing professors | 32 | |||
| 1 (0.4) | Improving the role of the developer and supporting the teacher | 22 |
Table 2. The challenges or disadvantages of e-learning in nursing education .
| Parameters | Total percent | Impact rate | N (%) | Items | References |
| Challenges of evaluation and feedback | 8.2 | 18 | 5 (2.3) | Failure to evaluate and control the quality of courses | 20,21,31,38,46 |
| 2 (0.9) | Uncertainty of maintenance and preservation of acquired clinical knowledge and skills | 38,44 | |||
| 2 (0.9) | Absence of course evaluation tools and online content | 38,44 | |||
| 9 (4.1) | Limited opportunities for immediate feedback and clarification of doubts | 16-18,22,28,34,38,51,58 | |||
| Problems related to human resource development | 11.8 | 26 | 2 (0.9) | Lack of personnel training in the development of online training courses | 38,44 |
| 2 (0.9) | Insufficient human resources | 18,27 | |||
| 6 (2.7) | Failure to strengthen information technology skills | 20,21,27,35,38,44 | |||
| 3 (1.4) | Not enough time | 28,31,38 | |||
| 5 (2.3) | lack of motivation | 15,20,25,30,38 | |||
| 2 (0.9) | Lack of familiarity with standards in design and implementation | 21,38 | |||
| 3 (1.4) | Lack of skills to design courses electronically | 21,26,38 | |||
| 3 (1.4) | Teachers' resistance | 21,31,38 | |||
| Structural and technical limitation | 19.1 | 42 | 3 (1.4) | Structural limitations of the course such as time and implementation method | 21,38,46 |
| 8 (3.6) | The relative low level of computer literacy of people | 15,18,21,27,31,42,45,50 | |||
| 4 (1.8) | Limits of access to the global Internet | 18,35,38,48 | |||
| 20 (9.1) | Technical problems related to hardware and software | 17-20,24-28,31,34,35,39,42,43,45,48,51,55,58 | |||
| 2 (0.9) | Lack of technical support from institutions. | 18,50 | |||
| 2 (0.9) | Lack of knowledge about working with tools | 14,38 | |||
| 3 (1.4) | Potential for distraction secondary to frequent disconnection and connection | 15,20,30 | |||
| Challenges related to communication and interaction | 26.8 | 59 | 30 (13.6) | Lack of face-to-face interaction | 15,17-20,22-28,30-36,39,42-45,49,51,54,55,58 |
| 19 (8.6) | Decreased social interactions and lack of socialization | 15-17,19,22,24-26,28,30-32,34,39,42,43,45,54 | |||
| 6 (2.7) | Limited interaction and communication between students and lecturers | 18,28,31,35,48,58 | |||
| 4 (1.8) | Lack of continuous and correct communication between experts in the three fields of information technology and educational technology and nursing | 18,38,44,46 | |||
| Challenges related to the content of education | 9.1 | 20 | 4 (1.8) | Incompatibility of content with reality and needs and goals | 18,38,44,46 |
| 4 (1.8) | Imbalance in information about e-learning in the world | 14,38,44 | |||
| 3 (1.4) | The possibility of breaking the necessary educational order | 18,38,44 | |||
| 3 (1.4) | Absence of drawing legal boundaries and educational regulations | 18,38,44 | |||
| 3 (1.4) | Lack of defined goals for training | 18,38,44 | |||
| 3 (1.4) | Lack of management roadmap and educational law and regulations | 18,38,44 | |||
| Financial challenges | 4.1 | 9 | 3 (1.4) | The cost of developing an e-learning program | 20,38,50 |
| 3 (1.4) | Hardware and software cost | 20,38,50 | |||
| 3 (1.4) | The cost of global Internet access | 20,38,50 | |||
| Organizational challenges | 1.8 | 4 | 2 (0.9) | Limits of institutional readiness in human resources and infrastructure | 18,38 |
| 2 (0.9) | Absence of an organ as the guardian of e-learning in organizations | 18,50 | |||
| Cultural challenges | 8.2 | 18 | 3 (1.4) | Lack of culture in use | 18,38,44 |
| 3 (1.4) | No change in traditional attitudes | 18,38,44 | |||
| 3 (1.4) | The existence of negative and pessimistic cultural attitudes towards the Internet | 18,38,44 | |||
| 3 (1.4) | Absence of culturally and socially defined content security supervisor | 18,38,44 | |||
| 3 (1.4) | Rejection | 18,38,44 | |||
| 3 (1.4) | Fear of the disappearance of the role of the teacher | 18,38,44 | |||
| Challenges of professional competence | 7.3 | 16 | 3 (1.4) | Limits of understanding concepts | 18,38,44 |
| 3 (1.4) | Short response time | 18,38,44 | |||
| 2 (0.9) | Uncertainty of achieving goals in the emotional and psychomotor field | 31,38 | |||
| 5 (2.3) | Limited opportunities to learn and develop practical skills | 15,26,30,31,55 | |||
| 3 (1.4) | Inability to influence professional performance | 18,38,44 | |||
| Challenges of ethics and information security | 3.6 | 8 | 3 (1.4) | The field of moral conflicts | 18,38,44 |
| 3 (1.4) | Security of personal information | 18,38,44 | |||
| 2 (0.9) | Political issues | 44,52 |
Table 3. The required components of e-learning in nursing education .
| Parameters | Total percent | Impact rate | N (%) | Items | References |
| Technology infrastructure | 22.75 | 38 | 23 (13.77) | Upgrading telecommunication systems and internet network | 16-18,23-26,28,32,33,36,38,42,44-48,51,53-55,58 |
| 9 (5.39) | Connecting educational systems to the Internet | 18,20,28,38,40,43,53-55 | |||
| 6 (3.59) | Embedding technical tools and defining process engineering | 18,19,27,39,53,55 | |||
| Human infrastructure | 13.77 | 23 | 8 (4.79) | Increasing cooperation between the main players of the virtual education system | 21,25,27,35,39,40,45,46 |
| 3 (1.8) | Improving information literacy and working skills with computers and software | 27,40,53 | |||
| 10 (5.99) | Changing the individual mindsets of the agents involved | 18,26-28,31,36,38,40,53,54 | |||
| 2 (1.2) | Reconstruction of roles and relationships | 18,53 | |||
| Pedagogical infrastructure | 11.98 | 20 | 2 (1.2) | Moving from teacher-centered to student-centered | 18,53 |
| 4 (2.4) | Determining the goals of e-learning projects | 18,34,40,53 | |||
| 9 (5.39) | Compilation of innovative educational resources and evaluation | 14,20,22,27,31,38,40,45,53 | |||
| 5 (2.99) | Research to choose the best platform | 26,27,40,47,53 | |||
| Cultural and social infrastructure | 16.17 | 27 | 9 (5.39) | Spreading the culture of netocracy | 14,17,18,26,33,39,43,44,53 |
| 2 (1.2) | Cultivating a global citizen by preserving indigenous and national values | 18,53 | |||
| 2 (1.2) | Trying to distribute learning and education fairly | 18,53 | |||
| 14 (8.38) | The spread of new pedagogical culture - independence in learning | 17,18,26,31,34,36,42,44,45,49,53,58 | |||
| Cultural and social infrastructure | 3.59 | 6 | 2 (1.2) | Planning for generating income from electronic education | 18,53 |
| 2 (1.2) | Investment in e-learning | 18,53 | |||
| 2 (1.2) | Report the costs associated with any type of training in the long term | 18,53 | |||
| Management and leadership infrastructure | 31.74 | 53 | 7 (4.19) | Formulation of policies, guidelines and executive laws of e-learning | 18-20,38,40,47,53 |
| 2 (1.2) | International and global approach to education | 18,53 | |||
| 2 (1.2) | Issuing licenses for intellectual property issues | 18,53 | |||
| 3 (1.8) | Quality assurance standards, authenticity and credibility | 40,53,56 | |||
| 28 (16.77) | Use of a recognized learning management system or platform | 15-17,19,23-26,30-36,39,42-45,47,49,51,53-55,58 | |||
| 4 (2.4) | Recruitment of academic staff | 18,40,47,53 | |||
| 7 (4.19) | Official support of the organization | 19,21,40,43,53,55,58 |
Table 4. Characteristics of the studies included in the analysis .
| First author | Electronic training | Searched databases | The purpose of the study | Participants |
| Bloomfield et al14 2008 | Using computer assisted learning | CINAHL, Medline, BNI, PsycInfo and ERIC | Assisted learning for clinical skills education in nursing, the ways in which it has been studied and the general findings. | Nursing students |
| Booth et al46 2009 | Workplace-based e-learning | Emerald, ERIC, IBSS, Index to Theses, LISA, MEDLINE, PsycINFO and Social Science Citation Index. | To address the question: Which Workplace-based e-learning (WBEL) techniques are most effective in enhancing the student learning experience? | Nurses, doctors, librarians and health information students |
| Button et al21 2014 | E-learning & information communication technology (ICT) | CINAHL, MEDLINE, OVID, the ProQuest Central, PubMed, ERIC | To identify research related To E-learning and associated technologies in preregistration nursing programs and to identify issues for both students and educators who are using E-learning. |
Nursing students and/or nurse educators |
| Carroll et al22 2009 | On-line learning | British Education Index, CINAHL, Emerald, ERIC, IBSS, LISA, MEDLINE, PsycINFO, and Social Science | To explore UK health-care professionals’ experience of on-line learning techniques | Nurses, midwives, and allied professions, general practitioners and hospital doctors |
| Cook et al23 2010-1 | Web-based learning | MEDLINE, EMBASE, ERIC, CINAHL and other databases | To describe the variation in configurations, instructional methods and presentation formats in WBL | Doctors, nurses, training nurses, dentists in training, dentists, pharmacists in training. |
| Cook et al24 2010-2 | Internet-based instruction | MEDLINE, CINAHL, EMBASE, and ERIC | To investigate time and learning efficiency in Internet-based learning | Physicians, nurses, pharmacists, dentists, veterinarians, and physical therapists |
| Cook et al25 2010-3 | Internet-based learning | MEDLINE, CINAHL, EMBASE, Web of Science, Scopus, ERIC, TimeLit, Dissertation Abstracts, and the University of Toronto Research | Two Investigate how to improve Inquiry-based learning (IBL) is needed. | Physicians, nurses, pharmacists, dentists, veterinarians, and physical therapists |
| Cook et al51 2008 | Internet-based learning | MEDLINE, Scopus, CINAHL, EMBASE, ERIC, TimeLit, Web of Science, Dissertation Abstracts, and the University of Toronto Research | To summarize the effect of Internet-based instruction for health professions learners compared with no intervention and with non-Internet interventions. | Student physicians, nurses, pharmacists, dentists, and other health care professionals |
| Du et al55 2013 | Web-based distance learning | PubMed and Embase | To examine the efficacy of the web-based distance education for nursing students and employed nurses. | Nursing students and employed nurses |
| Du et al8 2022 | Blended learning | PubMed and Embase, Web of Science, CINAHL and the Cochrane library | To determine the effectiveness of blended learning versus traditional face-to-face teaching in nursing education from the three aspects of knowledge, skills and satisfaction | Nursing students |
| Feng et al26 2013 | E-Learning | PubMed, Medline, CINAHL, ERIC, and Cochrane Library | To determine the effectiveness of situated e-learning in prelicensure and postlicensure medical and nursing education. | Nursing students and employed nurses, medical student |
| Frehywot et al27 2013 | E-learning | PubMed | Summarizes the literature on e-learning in low and middle-income countries (LMIC), and presents the spectrum of tools and strategies used. | Health professionals |
| Graafland et al52 2012 | PubMed, Embase, the Cochrane Database of Systematic Reviews, PsycINFO and CINAHL | Games for training | To review current serious games for training medical professionals and to evaluate the validity testing of such games. | Doctors, nurses, physiotherapists, paramedics |
| Hansen28 2008 |
3-D Healthcare Learning | YouTube, and social networks, such as Facebook, Twitter | To convey knowledge and ideas that have been established concerning the use of 3-D virtual worlds in medical and health professional education to date whilst describing, summarizing, evaluating, and clarifying the current literature. | Medicine professionals |
| Hosseini et al29 2016 | E-Learning | Science Direct, PubMed, SID | to evaluate the benefits of e-Learning in the Nursing Education. | Nursing students |
| Leijon et al15 2022 |
E-Learning | MEDLINE, CINAHL, OVID, and PubMed | Gamification and e-learning for young learners: A systematic literature review, bibliometric analysis, and future research agenda. | Undergraduate nursing students |
| Khatib Zanjani et al53 2012 | E-Learning | ERIC, ACM, Digital Learning, OECDT | The structured analysis of requirements, challenges, problems, and barriers in the application of e-learning in education and thus provide a model and guide for choosing, designing, and implementing an electronic course. | Medical Sciences students |
| Kleinpell et al30 2011 | Web-based | OVID-MEDLINE, PubMed, and CINAHL | To identify, catalog, and critically evaluate Web-based resources for critical care education. | Nurses |
| Klimova16 2018 | E-Learning | Web of Science, ScienceDirect, Scopus, and MEDLINE | two Use of eLearning in Medical Education and Healthcare Practice | Medical students, doctors, nurses, or other healthcare |
| Koch31 2014 |
E-Learning | Web of Science, ScienceDirect, Scopus, | to answer the following question: How does e-learning transform the role of nurse educators? | Nursing educators |
| Kokol et al 47 2006 |
E-Learning | Web of Science, ScienceDirect, Scopus, | Investigating the E-learning challenges faced by students during COVID-19 in Namibia. | Nursing Education students |
| Kuriplachova et al48 2021 |
E-Learning | PubMed, Medline | Moodle implementation for e-learning: A systematic review. | Nursing and healthcare students |
| Lahti et al32 2014 |
E-Learning | MEDLINE CINAHL PsycINFO and ERIC | To assess the impact of e-learning on nurses’ and nursing student’s knowledge, skills and satisfaction. | Nurses and student nurses |
| Lam-Antoniades et al49 2009 |
Electronic continuing education | MEDLINE, EMBASE, and CINAHL | Two provides an update on evidence from randomized controlled trials (RCTs) assessing the effectiveness of e-CE in the health professions. | Physicians, nurses, nursing aides, pharmacists, paramedics, and nursing home managers. |
| Lee54 2015 |
E-Learning | Using e-learning to enhance nurse education | Nurse education | |
| Liu et al33 2016 |
Blended learning | Medline, CINAHL, ScienceDirect, Ovid Embase, Web of Science, and ERIC | To assess the effectiveness of blended learning for health professional learners compared with no intervention and with nonblended learning | Health professional learners |
| Mancuso et al34 2009 | Distance education | PubMed, CINAHL, ERIC, and Health Sciences in ProQuest | What are nursing faculty members’ perceptions of distance education in nursing? | Nursing faculty members |
| Martinengo et al35 2019 | Digital education | CENTRAL) (Cochrane Library), MEDLINE (Ovid), Embase (Ovid), Web of Science, the Educational Resource Information Centre (ERIC) (Ovid), PsycINFO (Ovid), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO), the ProQuest Dissertation and Theses database, and trial registries. | To assess the effectiveness of digital education as a stand-alone approach or as part of a blended-learning approach in improving pre- and post-registration health care professionals’ knowledge, attitudes, practical skills, and behavior in the management of chronic wounds, as well as their satisfaction with the intervention. Secondary objectives are to evaluate patient-related outcomes, cost-effectiveness of the interventions, and any unfavorable or undesirable outcomes that may arise. | Health care professionals |
| Matava et al36 2017 | Mobile apps | App Store, Google Play, BlackBerry World, and Windows Store | To critically evaluate the quality of airway management apps and target revised Bloom's Taxonomy cognitive levels. | Emergency medical technicians, health care professionals, paramedics trainees nurses, anesthesiologists, emergency physicians critical care physicians, military medics, medical students, family medicine physicians, lifeguards firefighters, respiratory therapists |
| McCutcheon et al37 2015 |
Blended learning | MEDLINE, CINAHL, BREI, ERIC and AUEI | To determine whether the use of an online or blended learning paradigm has the potential to enhance the teaching of clinical skills in undergraduate nursing. | undergraduate nurse |
| McDonald et al12 2018 | E-learning | MEDLINE, CINAHL, Cochrane Library and ProQuest Nursing and Allied Health Source | To Examine the current evidence on the effectiveness of digital technologies or e-based learning for enhancing the skills and knowledge of nursing students in nursing assessment. | Nursing students |
| Meinert et al50 2021 | E-Learning | PubMed, Scopus, Education Resource Information Centre (ERIC), Web of Science, Embase, Global Health, Health Management Information Consortium (HMIC), Prospero, and OVID. | To explore the state of evidence concerning cost capture within eLearning in health professions education. | Health professions students |
| Mousazadeh et al58 2016 | E-Learning | Medline and CINAHL databases and Google | To evaluate the effectiveness of e learning in learning. | Medical and non-medical students |
| Naderifar et al38 2016 | E-Learning | Medline, Ovid, ProQuest, and PubMed | Challenge based learning in higher education–A systematic literature review. | Medical students |
| Nakhoda et al39 2021 | E-Learning | PubMed, Scopus, Elsevier, Google Scholar, Web of Science and Iranian Scientific Information Database (SID), IranDoc, Civilica and Magiran | To assess E-Learning Satisfaction (ELS) in medical and non-medical students during COVID-19 pandemic. | Medical and non-medical students |
| Patterson et al40 2012 |
Distance learning | CINAHL, Academic Search Premier, Educational Resource Information Centre, Health Source, Educational Research Complete, Computers and Applied Sciences Complete, and ProQuest Dissertation Abstracts. The search engine Google Scholar was also used | To describe the state of the qualitative and quantitative nursing research on student outcomes of distance learning. | Nursing students |
| Peng et al17 2017 |
Internet-based learning | Medline, Web of Science, ProQuest, Google scholar, ERIC and Elsevier | To explore the impact of Internet-based learning on students/professionals’ knowledge of public health compared with no intervention and with traditional face-to-face (FTF) formats. | Medical students, professionals of public health |
| Petty56 2013 |
E-Learning | CINAHL (Cumulative Index of Nursing and Allied Health Literature) with full text (EBSCO) and MEDLINE via the NHS Evidence Healthcare database | To identify literature that explores the effectiveness of interactive, TE tools on knowledge acquisition and learner satisfaction within healthcare with a view to evaluating their use for post-basic nurse education. | Healthcare professionals |
| Rahimi et al18 2013 |
E-Learning | PubMed- Embase, Magiran, Medline- Cochrane -Eric, SID - Iranmedex | E-learning, barriers to implementation, solutions | Medical science students |
| Regmi & Jones 41 2021 |
E-Learning | MEDLINE, EMBASE, Allied & Complementary Medicine, DH-DATA, PsycINFO, CINAHL, Global Health, BREI (British Education Index), AEI (Australian Education Index), Web of Science, CENTRAL, ERIC and Google Scholar | To measure the impact of e-learning as compared to traditional face-to-face learning, both measured and perceived, on health sciences education | Doctors, nurses and allied health professionals) |
| Richardson et al59 2017 | Learning in the online environment | EBSCO, PsycINFO, ERIC | To investigate Satisfaction and Learning in the Online Environment | Students from all science |
| River et al42 2016 |
Blending technology | Medline, CINAHL, ERIC and Embase | To identify how technology has been incorporated into TBL in higher education health disciplines | Nursing and other health science students |
| Rowe et al43 2012 |
Blended learning | CINAHL and MEDLINE | To determine the impact of blended learning in the clinical education of healthcare students. | Healthcare students |
| Sadeghi Mahali et al44 2022 |
Virtual education | PubMed, ScienceDirect, Scopus, Google Scholar, SID, IranDoc | Comparison of virtual education challenges in nursing before and after COVID-19 | Nursing education students |
| Vallée et al19 2020 |
Blended learning | MEDLINE | To assess the effectiveness of blended learning compared to that of traditional learning in health education. | Nursing, pharmacy, physiotherapy, dentistry students |
| Wilkinson et al45 2009 |
E-Learning | BNI, Medline, ERIC, BEI, AEI Web of Knowledge (ISI), PsycINFO | Describe and discuss the psychometric properties of instruments used in healthcare education settings measuring experience and attitudes of healthcare students’ regarding their ICT skills and their use of computers and the Internet for education | Students in the healthcare professions |
| Wolbrink & Burns20 2012 |
Internet-based learning | MEDLINE/PubMed | To Define the key concepts of Internet-based learning, summarize the current literature, and describe how Internet-based learning may be uniquely suited for the critical care provider | Medical students |
Figure 2.
The variety of keywords of selected studies
Figure 3.

The combination of authors of selected studies
Figure 4.
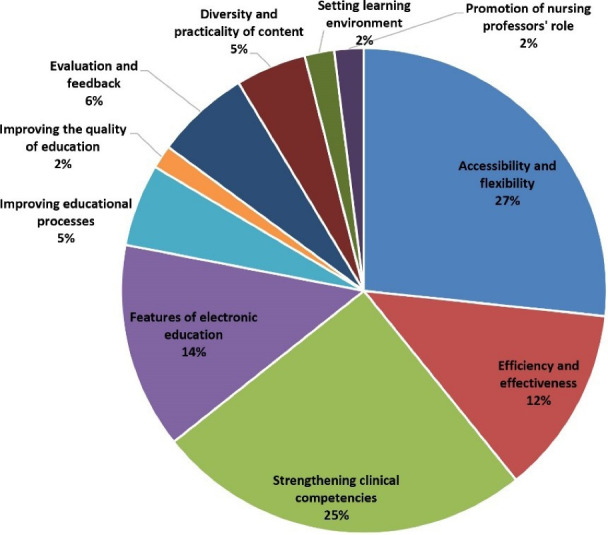
The opportunities or advantages of e-learning in nursing education
Figure 5.
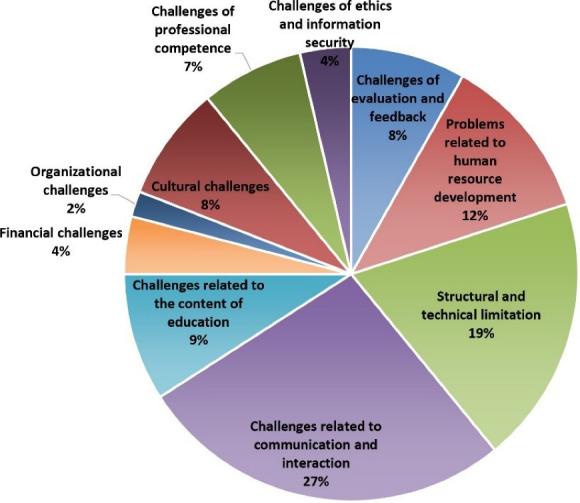
The challenges or disadvantages of e-learning in nursing education
Figure 6.
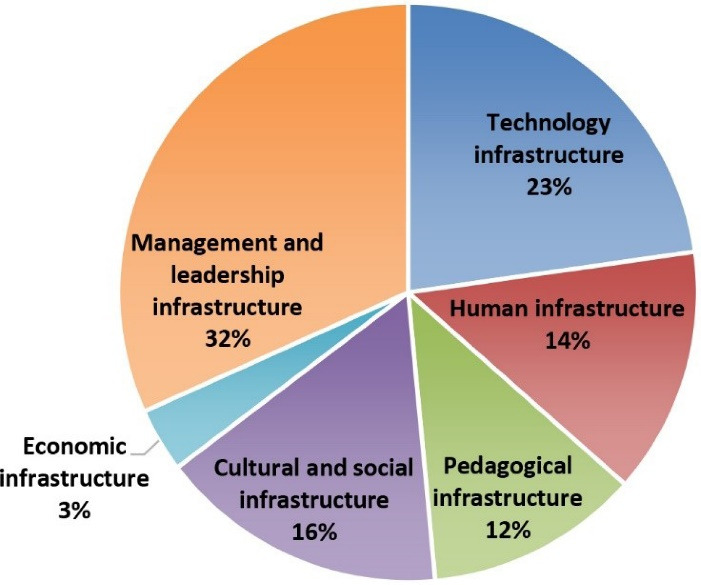
The required components of e-learning in nursing education
Discussion
The present study has been conducted with the three aims of identifying the advantages, disadvantages, and required components of electronic education in nursing. In general, in the two categories of advantages, disadvantages, access and flexibility (68 points) and strengthening of clinical competencies (64 points), communication and interaction (59 points), and structural and technical limitations (42 points) scored the most points. Also, in the required components, management and leadership infrastructure (53 points) and technology infrastructure (38 points) had the highest scores. One of the results obtained from the benefits of e-learning, in line with Naciri’s study, is accessibility, which can be useful in three areas (content, training, and location) and along with flexibility, it gives nurses the possibility to gain knowledge without having to be physically present at the place of training and update their skills.4 Another significant benefit of e-learning in nursing education is the strengthening of clinical competencies, which, in line with Feng and Liu studies, leads to encouraging nurses to continuously improve their clinical skills.26,33 For example, virtual communication with patients and treatment teams can help students to communicate better and more effectively with their patients and colleagues in times of crisis, and by strengthening communication skills, get to know the real conditions of clinical departments.57,60 In line with the results of the present study, learning improves students’ cognitive skills by providing interactive educational content and various evaluation techniques. The results of other studies also show that this makes students better able to absorb information, record it in their minds and use it in the hospital.9,27 Another important advantage in the current research is to improve educational processes and improve the quality of education in order to increase productivity and reduce the duration of education and skills for learners. In this regard, Najjar’s study show that the integration of e-learning has allowed students to have more access to higher education because it frees them from the requirement of physical presence and has a significant positive effect on their academic flexibility.61 The diversity and applicability of the content in electronic education in nursing is one of the other advantages of this educational method. In this regard, Ongor and Uslusoy showed that this educational method taking into account the cultural and linguistic differences, in a more attractive and diverse way, increases the possibility of the desire to learn and accompany the education process.62
In contrast to the advantages of electronic education, disadvantages are also mentioned in this study, which are usually caused by the reduction of face-to-face interaction between students and lecturers. This reduction of interaction may lead to a decrease in interactive opportunities, a feeling of lack of support and guidance, a feeling of isolation and a decrease in educational motivation in students. The reduction of interaction in other studies has also been expressed as an obstacle in education, and social interactions in regular face-to-face education such as classes, research groups, and workshops are far more than in electronic education.63,64 Another challenge obtained from this study was structural limitations and insufficient technical support. In this regard, Macdonald states that these limitations can lead to a lack of flexibility in the time and content of education and ultimately cause students uncertainty in using educational tools. 57 In other words, the contradiction in the results of the advantages or disadvantages of e-learning is derived from the technical infrastructure and equipment that usually manifests itself in low-income countries.
In the following, the various infrastructure components required for the implementation and development of electronic education in nursing are proposed in the present study, which is in line with the results of other studies.23,24 The technological infrastructure includes the upgrading of telecommunication systems and the Internet network and the installation of technical and engineering tools that can be presented and managed through these modern technical tools, educational content and educational software.65 Human infrastructures that by using these infrastructures, people make the best use of educational technologies and achieve a more motivating and engaging learning experience.66 Pedagogical infrastructure can help improve the quality and experience of online learning by changing from teacher-centered to student-centered and students are encouraged to an autonomous and motivated learning process.67 Cultural and social infrastructure leads to the fair distribution of educational opportunities and facilities by promoting positive values and concepts in the educational society.18 Economic infrastructure facilitates and accelerates the development of education by using new technologies and the development of educational platforms and applications and leads to the formulation of policies, the use of an international approach, the issuance of intellectual property licenses, the determination of quality standards, the use of the learning management system attracts people.53 Finally, facilitating the creation of effective and efficient infrastructures resulting from the present study will improve the online learning experience and the quality of e-learning. In this regard, the experience of many countries in the COVID-19 pandemic for the rapid and timely creation of technical infrastructure and equipment has shown the increase in the skill of the medical group providing care.68
One of the strengths of this study is the broad and extensive search in the databases, which has led to the comprehensiveness of the results. One of the limitations of this study is the impossibility of categorizing studies according to low-income and high-income countries, as well as examining the results of electronic nursing education in the development of quality care skills.
Conclusion
This research found Opportunities and threats of E-learning and factors that influenced choosing it according to advantages and disadvantages. This research provides knowledge about criteria that can be used further in E-learning to benefit from its advantages depending on the infrastructure of different settings. The results of the present study indicate that the benefits of e-learning for training nurses can be an efficient and effective method, so with the growing progress of science and technology, this method cannot be ignored, but it should overcome obstacles and challenges. In this way, by modifying the infrastructure, it is possible to reduce the disadvantages and add to its advantages.
Acknowledgements
The authors would like to extend their deepest thanks to all librarians who helped them to access information resources in Mashhad University of Medical Sciences.
Competing Interests
The authors declare that they have no conflicts of interest.
Data Availability Statement
The Data could be available upon a reasonable request to the Abdollahpour with abdollahpourts2@yahoo.com and with the permission of the Mashhad University of Medical Science ethical committee.
Ethical Approval
This project was approved with the code (IR.MUMS.REC.1401.165) in the ethics committee of Mashhad University of Medical Sciences. Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Research Highlights
What is the current knowledge?
E-learning is increasingly replacing traditional methods in medical science education. The future likely lies in blended learning, which combines the strengths of both approaches for a more engaging, effective, and accessible learning experience.
What is new here?
Electronic education in nursing offers opportunities categorized into 10 areas: accessibility and flexibility, efficiency and effectiveness, strengthening clinical competencies, features of electronic education, improving educational processes, improving the quality of education, evaluation and feedback, diversity and practically of content, setting learning environment and promotion of nursing professors’ role.
Electronic education challenges, categorized into 10 groups: challenges of evaluation and feedback, problems related to the of human resources development, structural and technical limitations, challenges related to communication and interaction, challenges related to the content of education, financial challenges, organizational challenges, cultural challenges, challenges of professional competence, challenges of ethics and information security.
The essential components for effective electronic teaching in nursing education are organized into 6 categories: technological infrastructure, human infrastructure, pedagogical infrastructure, cultural and social infrastructure, economic infrastructure, and management and leadership infrastructure.
Funding Statement
This study was funded by Mashhad University of Medical Sciences [grant number4010090].
References
- 1. World Bank. World Bank Education COVID-19 School Closures Map. 2020. Available from: https://www.worldbank.org/en/data/interactive/2020/03/24/world-bank-education-and-covid-19. Accessed June 15, 2020.
- 2.Djeki E, Dégila J, Bondiombouy C, Alhassan MH. E-learning bibliometric analysis from 2015 to 2020. J Comput Educ. 2022;9(4):727–54. doi: 10.1007/s40692-021-00218-4. [DOI] [Google Scholar]
- 3.Rahayu NW, Ferdiana R, Kusumawardani SS. A systematic review of ontology use in e-learning recommender system. Comput Educ Artif Intell. 2022;3:100047. doi: 10.1016/j.caeai.2022.100047. [DOI] [Google Scholar]
- 4.Naciri A, Radid M, Kharbach A, Chemsi G. E-learning in health professions education during the COVID-19 pandemic: a systematic review. J Educ Eval Health Prof. 2021;18:27. doi: 10.3352/jeehp.2021.18.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaona A, Banzi R, Kwag KH, Rigon G, Cereda D, Pecoraro V, et al. E-learning for health professionals. Cochrane Database Syst Rev. 2018;1(1):CD011736. doi: 10.1002/14651858.CD011736.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pourghaznein T, Sabeghi H, Shariatinejad K. Effects of e-learning, lectures, and role playing on nursing students’ knowledge acquisition, retention and satisfaction. Med J Islam Repub Iran. 2015;29:162. [PMC free article] [PubMed] [Google Scholar]
- 7. Arian M, Nobahar M, Raiesdana N, Oghazian MB. Identifying the fields of activity, challenges and positive outcomes of nursing prescription: a systematic review. Hayat 2018; 24(3): 279-95. [Persian].
- 8.Du L, Zhao L, Xu T, Wang Y, Zu W, Huang X, et al. Blended learning vs traditional teaching: the potential of a novel teaching strategy in nursing education - a systematic review and meta-analysis. Nurse Educ Pract. 2022;63:103354. doi: 10.1016/j.nepr.2022.103354. [DOI] [PubMed] [Google Scholar]
- 9.Voutilainen A, Saaranen T, Sormunen M. Voutilainen A, Saaranen T, Sormunen MConventional vse-learning in nursing education: a systematic review and meta-analysis. Nurse Educ Today. 2017;50:97–103. doi: 10.1016/j.nedt.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Divya KY, Binil V. E-learning challenges in nursing education during COVID-19 pandemic–a narrative review. Indian J Forensic Med Toxicol. 2021;15(2):2317–22. doi: 10.37506/ijfmt.v15i2.14718. [DOI] [Google Scholar]
- 11.Tabatabaei SH, Mirzaiean A, Keshmiri F. Opportunities and threats of e-learning in dental education in viewpoints of faculty members: a mixed method study. Dent Res J (Isfahan) 2022;19:89. [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald CJ, Backhaus I, Vanezi E, Yeratziotis A, Clendinneng D, Seriola L, et al. European Union Digital Education quality standard framework and companion evaluation toolkit. Open Learn. 2024;39(1):85–100. doi: 10.1080/02680513.2021.1936476. [DOI] [Google Scholar]
- 13.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bloomfield JG, While AE, Roberts JD. Using computer assisted learning for clinical skills education in nursing: integrative review. J Adv Nurs. 2008;63(3):222–35. doi: 10.1111/j.1365-2648.2008.04653.x. [DOI] [PubMed] [Google Scholar]
- 15.Leijon M, Gudmundsson P, Staaf P, Christersson C. Challenge based learning in higher education–a systematic literature review. Innov Educ Teach Int. 2022;59(5):609–18. doi: 10.1080/14703297.2021.1892503. [DOI] [Google Scholar]
- 16. Klimova B. The use of e-learning in medical education and healthcare practice–a review study. In: Auer M, Zutin D, eds. Online Engineering & Internet of Things. Vol 22. Cham: Springer; 2018. p. 933-9. 10.1007/978-3-319-64352-6_87 [DOI]
- 17. Peng Y, Yan W. Effect of Internet-Based Learning in Public Health Training: An Exploratory Meta-Analysis. International Conference e-Learning; 2017.
- 18. Rahimi B, Jebraeily M, Mehdi Oghli R, Rashidi A, Masomi R. The barriers of e-learning implementation in medical sciences domain and provided the necessary solutions. J Urmia Nurs Midwifery Fac 2013; 11(6): 461-7. [Persian].
- 19.Vallée A, Blacher J, Cariou A, Sorbets E. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22(8):e16504. doi: 10.2196/16504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolbrink TA, Burns JP. Internet-based learning and applications for critical care medicine. J Intensive Care Med. 2012;27(5):322–32. doi: 10.1177/0885066611429539. [DOI] [PubMed] [Google Scholar]
- 21.Button D, Harrington A, Belan I. E-learning & information communication technology (ICT) in nursing education: a review of the literature. Nurse Educ Today. 2014;34(10):1311–23. doi: 10.1016/j.nedt.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Carroll C, Booth A, Papaioannou D, Sutton A, Wong R. UK health-care professionals’ experience of on-line learning techniques: a systematic review of qualitative data. J Contin Educ Health Prof. 2009;29(4):235–41. doi: 10.1002/chp.20041. [DOI] [PubMed] [Google Scholar]
- 23.Cook DA, Garside S, Levinson AJ, Dupras DM, Montori VM. What do we mean by web-based learning? a systematic review of the variability of interventions. Med Educ. 2010;44(8):765–74. doi: 10.1111/j.1365-2923.2010.03723.x. [DOI] [PubMed] [Google Scholar]
- 24.Cook DA, Levinson AJ, Garside S. Time and learning efficiency in internet-based learning: a systematic review and meta-analysis. Adv Health Sci Educ Theory Pract. 2010;15(5):755–70. doi: 10.1007/s10459-010-9231-x. [DOI] [PubMed] [Google Scholar]
- 25.Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Instructional design variations in internet-based learning for health professions education: a systematic review and meta-analysis. Acad Med. 2010;85(5):909–22. doi: 10.1097/ACM.0b013e3181d6c319. [DOI] [PubMed] [Google Scholar]
- 26.Feng JY, Chang YT, Chang HY, Erdley WS, Lin CH, Chang YJ. Systematic review of effectiveness of situated e-learning on medical and nursing education. Worldviews Evid Based Nurs. 2013;10(3):174–83. doi: 10.1111/wvn.12005. [DOI] [PubMed] [Google Scholar]
- 27.Frehywot S, Vovides Y, Talib Z, Mikhail N, Ross H, Wohltjen H, et al. E-learning in medical education in resource constrained low- and middle-income countries. Hum Resour Health. 2013;11:4. doi: 10.1186/1478-4491-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hansen MM. Versatile, immersive, creative and dynamic virtual 3-D healthcare learning environments: a review of the literature. J Med Internet Res. 2008;10(3):e26. doi: 10.2196/jmir.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hosseini MA, Ghahremani AR, Mohammadi Shahbolaghi F, Hamadzadeh S, Tamizi Z. The advantages of electronic learning in nursing education: a review study. J Nurs Educ 2016; 4(4): 9-16. [Persian].
- 30.Kleinpell R, Ely EW, Williams G, Liolios A, Ward N, Tisherman SA. Web-based resources for critical care education. Crit Care Med. 2011;39(3):541–53. doi: 10.1097/CCM.0b013e318206b5b5. [DOI] [PubMed] [Google Scholar]
- 31.Koch LF. The nursing educator’s role in e-learning: a literature review. Nurse Educ Today. 2014;34(11):1382–7. doi: 10.1016/j.nedt.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 32.Lahti M, Hätönen H, Välimäki M. Impact of e-learning on nurses’ and student nurses knowledge, skills, and satisfaction: a systematic review and meta-analysis. Int J Nurs Stud. 2014;51(1):136–49. doi: 10.1016/j.ijnurstu.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 33.Liu Q, Peng W, Zhang F, Hu R, Li Y, Yan W. The effectiveness of blended learning in health professions: systematic review and meta-analysis. J Med Internet Res. 2016;18(1):e2. doi: 10.2196/jmir.4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mancuso JM. Perceptions of distance education among nursing faculty members in North America. Nurs Health Sci. 2009;11(2):194–205. doi: 10.1111/j.1442-2018.2009.00456.x. [DOI] [PubMed] [Google Scholar]
- 35.Martinengo L, Yeo NJY, Tang ZQ, Markandran KD, Kyaw BM, Tudor Car L. Digital education for the management of chronic wounds in health care professionals: protocol for a systematic review by the digital health education collaboration. JMIR Res Protoc. 2019;8(3):e12488. doi: 10.2196/12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matava C, Leo AM, Alam F. Mobile apps for teaching intubation: scoping review and critical analysis in e-learning. JMIR Med Educ. 2017;3(2):e15. doi: 10.2196/mededu.7919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCutcheon K, Lohan M, Traynor M, Martin D. McCutcheon K, Lohan M, Traynor M, Martin DA systematic review evaluating the impact of online or blended learning vsface-to-face learning of clinical skills in undergraduate nurse education. J Adv Nurs. 2015;71(2):255–70. doi: 10.1111/jan.12509. [DOI] [PubMed] [Google Scholar]
- 38. Naderifar M, Ghaljaie F, Jalalodini A, Rezaie N, Salar A. Challenges of e-learning in medical sciences: a review article. J Med Educ Dev 2016; 9(23): 102-11. [Persian].
- 39.Nakhoda K, Ahmady S, Gholami Fesharaki M, Gheshlaghi Azar N. COVID-19 pandemic and e-learning satisfaction in medical and non-medical student: a systematic review and meta-analysis. Iran J Public Health. 2021;50(12):2509–16. doi: 10.18502/ijph.v50i12.7933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patterson BJ, Krouse AM, Roy L. Student outcomes of distance learning in nursing education: an integrative review. Comput Inform Nurs. 2012;30(9):475–88. doi: 10.1097/NXN.0b013e3182573ad4. [DOI] [PubMed] [Google Scholar]
- 41.Regmi K, Jones L. Effect of e-learning on health sciences education: a protocol for systematic review and meta-analysis. High Educ Pedagog. 2021;6(1):22–36. doi: 10.1080/23752696.2021.1883459. [DOI] [Google Scholar]
- 42.River J, Currie J, Crawford T, Betihavas V, Randall S. A systematic review examining the effectiveness of blending technology with team-based learning. Nurse Educ Today. 2016;45:185–92. doi: 10.1016/j.nedt.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 43.Rowe M, Frantz J, Bozalek V. The role of blended learning in the clinical education of healthcare students: a systematic review. Med Teach. 2012;34(4):e216–21. doi: 10.3109/0142159x.2012.642831. [DOI] [PubMed] [Google Scholar]
- 44.Sadeghi Mahali N, Arsalani N, Rad M, Nematifard T, Khaki S, Fallahi-Khoshknab M. Comparison of virtual education challenges in nursing before and after COVID- 19; a systematic review. Iran J Syst Rev Med Sci. 2023;1(3):81–103. [Google Scholar]
- 45.Wilkinson A, While AE, Roberts J. Measurement of information and communication technology experience and attitudes to e-learning of students in the healthcare professions: integrative review. J Adv Nurs. 2009;65(4):755–72. doi: 10.1111/j.1365-2648.2008.04924.x. [DOI] [PubMed] [Google Scholar]
- 46.Booth A, Carroll C, Papaioannou D, Sutton A, Wong R. Applying findings from a systematic review of workplace-based e-learning: implications for health information professionals. Health Info Libr J. 2009;26(1):4–21. doi: 10.1111/j.1471-1842.2008.00834.x. [DOI] [PubMed] [Google Scholar]
- 47.Kokol P, Blazun H, Micetić-Turk D, Abbott PA. E-learning in nursing education--challenges and opportunities. Stud Health Technol Inform. 2006;122:387–90. [PubMed] [Google Scholar]
- 48.Kuriplachová G, Kováčková G, Magurová D, Kendrová L. Advantages and disadvantages of e-learning in nursing teaching process. J Health Syst Policies. 2019;1(2):45–54. [Google Scholar]
- 49.Lam-Antoniades M, Ratnapalan S, Tait G. Electronic continuing education in the health professions: an update on evidence from RCTs. J Contin Educ Health Prof. 2009;29(1):44–51. doi: 10.1002/chp.20005. [DOI] [PubMed] [Google Scholar]
- 50.Meinert E, Eerens J, Banks C, Maloney S, Rivers G, Ilic D, et al. Exploring the cost of e-learning in health professions education: scoping review. JMIR Med Educ. 2021;7(1):e13681. doi: 10.2196/13681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: a meta-analysis. JAMA. 2008;300(10):1181–96. doi: 10.1001/jama.300.10.1181. [DOI] [PubMed] [Google Scholar]
- 52.Graafland M, Schraagen JM, Schijven MP. Systematic review of serious games for medical education and surgical skills training. Br J Surg. 2012;99(10):1322–30. doi: 10.1002/bjs.8819. [DOI] [PubMed] [Google Scholar]
- 53. Khatib Zanjani N, Zandi B, Farajollahi M, Sarmadi MR, Ebrahim Zadeh I. The structured analysis of requirements and challenges of e-learning and proposing a practical model for successful implementation of e-courses in medical sciences. Iran J Med Educ 2012; 11(8): 995-1009. [Persian].
- 54.Lee P. Using e-learning to enhance nurse education. Nurs Times. 2015;111(43):18–9. [PubMed] [Google Scholar]
- 55.Du S, Liu Z, Liu S, Yin H, Xu G, Zhang H, et al. Web-based distance learning for nurse education: a systematic review. Int Nurs Rev. 2013;60(2):167–77. doi: 10.1111/inr.12015. [DOI] [PubMed] [Google Scholar]
- 56.Petty J. Interactive, technology-enhanced self-regulated learning tools in healthcare education: a literature review. Nurse Educ Today. 2013;33(1):53–9. doi: 10.1016/j.nedt.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 57.McDonald EW, Boulton JL, Davis JL. E-learning and nursing assessment skills and knowledge - an integrative review. Nurse Educ Today. 2018;66:166–74. doi: 10.1016/j.nedt.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 58.Mousazadeh S, Dehghani M, Mozaffari F, Ghasemnegad SM, Hakimi H, Bagherian S. The effectiveness of e-learning in learning: a review of the literature. Int J Med Res Health Sci. 2016;5(2):86–91. [Google Scholar]
- 59.Richardson JC, Maeda Y, Lv J, Caskurlu S. Social presence in relation to students’ satisfaction and learning in the online environment: a meta-analysis. Comput Human Behav. 2017;71:402–17. doi: 10.1016/j.chb.2017.02.001. [DOI] [Google Scholar]
- 60.Can Ş, Durgun H, Dalcalı BK. Effect of online communication skills training on effective communication and self-efficacy and self-regulated learning skills of nursing students: a randomized controlled study. Nurse Educ Pract. 2022;63:103371. doi: 10.1016/j.nepr.2022.103371. [DOI] [PubMed] [Google Scholar]
- 61.Najjar N, Ajjaka L. E-learning: innovations and challenges in the new millennia. EuroMed Journal of Management. 2023;5(1):71–82. doi: 10.1504/emjm.2023.10052606. [DOI] [Google Scholar]
- 62.Ongor M, Uslusoy EC. The effect of multimedia-based education in e-learning on nursing students’ academic success and motivation: a randomised controlled study. Nurse Educ Pract. 2023;71:103686. doi: 10.1016/j.nepr.2023.103686. [DOI] [PubMed] [Google Scholar]
- 63.Junco R, Elavsky CM, Heiberger G. Putting twitter to the test: assessing outcomes for student collaboration, engagement and success. Br J Educ Technol. 2013;44(2):273–87. doi: 10.1111/j.1467-8535.2012.01284.x. [DOI] [Google Scholar]
- 64.Means B, Toyama Y, Murphy R, Baki M. The effectiveness of online and blended learning: a meta-analysis of the empirical literature. Teach Coll Rec. 2013;115(3):1–47. doi: 10.1177/016146811311500307. [DOI] [Google Scholar]
- 65.Duderstadt JJ. New roles for the 21st-century university. Issues Sci Technol. 1999;16(2):37–44. [Google Scholar]
- 66.Farhan MK, Talib HA, Mohammed MS. Key factors for defining the conceptual framework for quality assurance in e-learning. J Inf Technol Manag. 2019;11(3):16–28. doi: 10.22059/jitm.2019.74292. [DOI] [Google Scholar]
- 67.Kebritchi M, Lipschuetz A, Santiague L. Issues and challenges for teaching successful online courses in higher education: a literature review. J Educ Technol Syst. 2017;46(1):4–29. doi: 10.1177/0047239516661713. [DOI] [Google Scholar]
- 68.Mirzakhani K, Jahani Shoorab N, Akbari A, Khadivzadeh T. High-risk pregnant women’s experiences of the receiving prenatal care in COVID-19 pandemic: a qualitative study. BMC Pregnancy Childbirth. 2022;22(1):363. doi: 10.1186/s12884-022-04676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The Data could be available upon a reasonable request to the Abdollahpour with abdollahpourts2@yahoo.com and with the permission of the Mashhad University of Medical Science ethical committee.



