Abstract
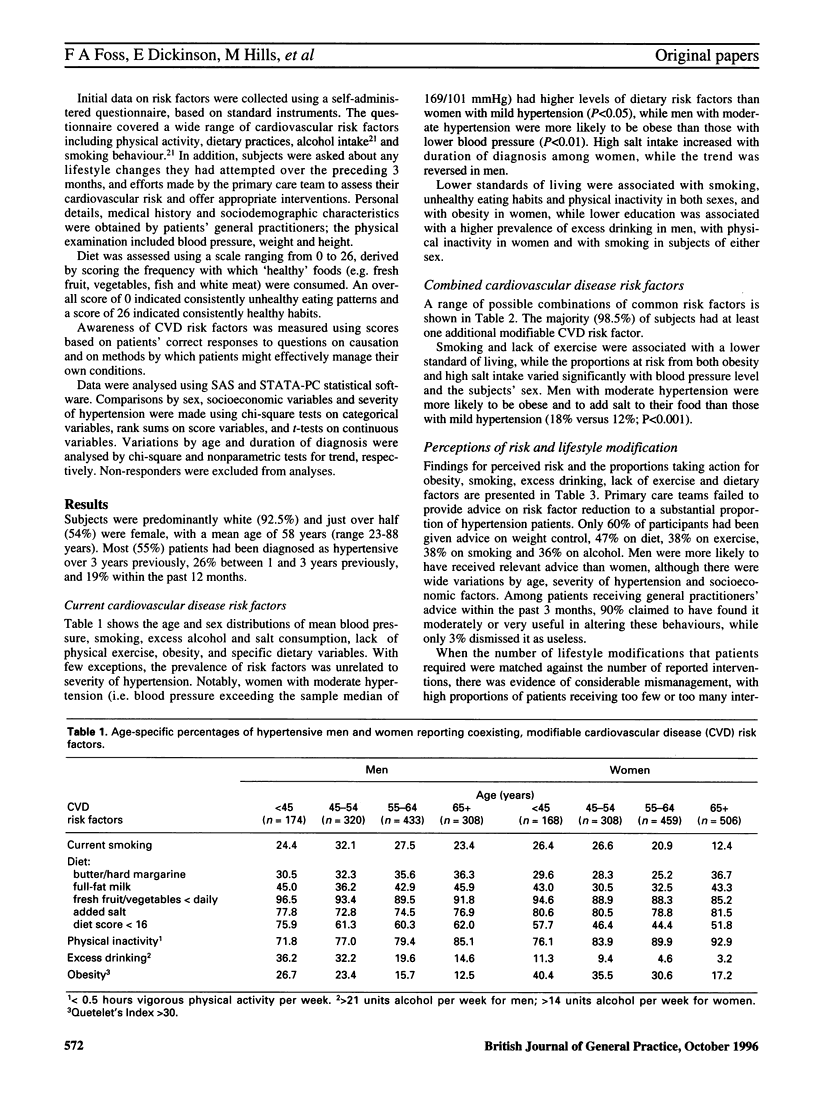
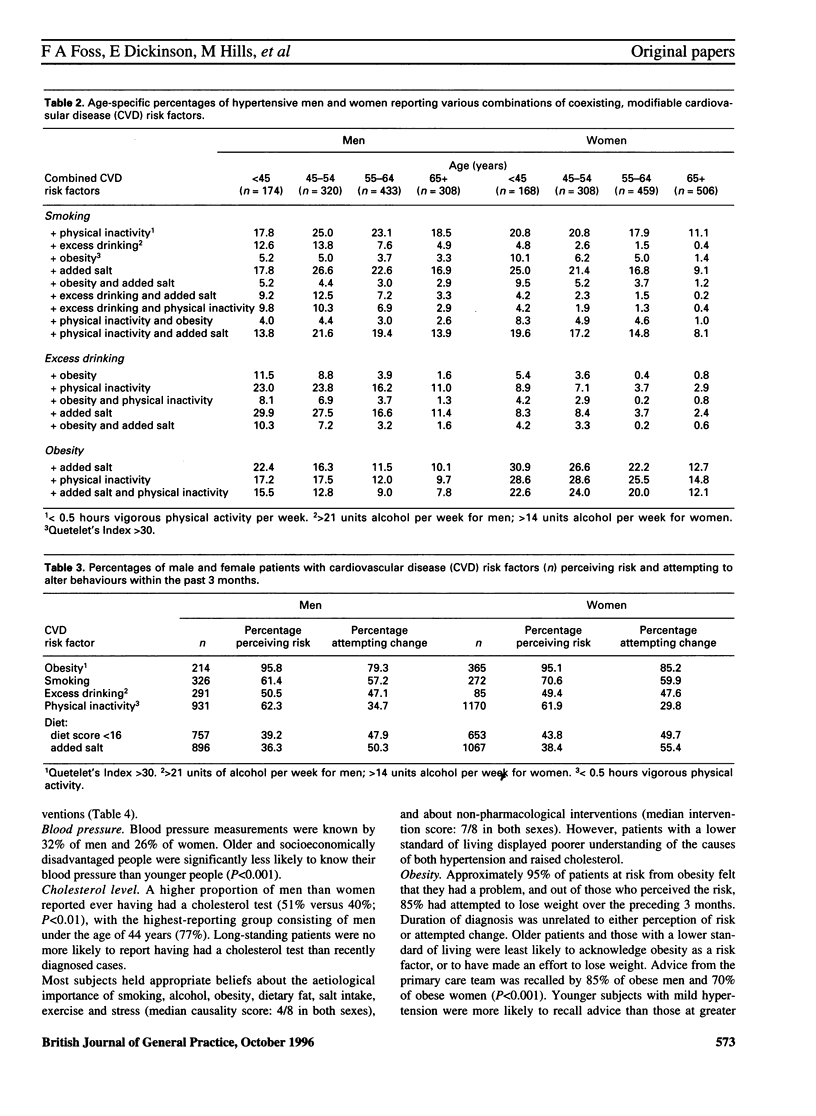
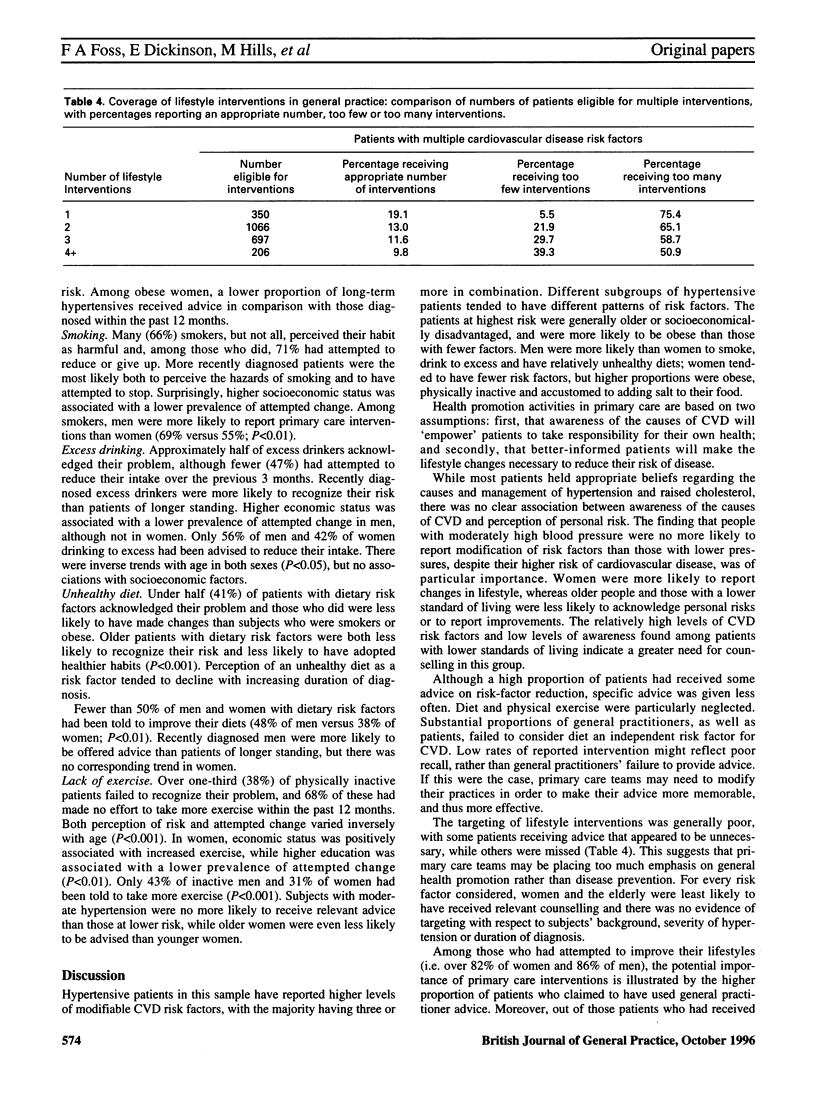
BACKGROUND: High-risk strategies for the prevention of cardiovascular disease (CVD) among hypertensive patients require knowledge of the prevalence and interaction of modifiable risk factors to ensure effective targeting of interventions. Comparatively little is known of risk-factor profiles and their modification among hypertensives in primary care. AIM: The present study was designed to explore relationships between patients' knowledge of CVD risk factors, their perception of personal risk and health behaviours, and their use of lifestyle interventions. METHOD: A cross-sectional survey of 2676 men and women with mild to moderate hypertension (diastolic blood pressure 95-115 mmHg), and their general practitioners, recruited from 1044 general practices throughout the UK, was conducted. RESULTS: Levels of modifiable risk factors were high, although there was considerable variation by age and sex; most (98.5%) patients had at least one additional CVD risk factor. A lower standard of living was associated with a higher prevalence of 'unhealthy' behaviours. Out of those with a current lifestyle problem, 85% of obese patients, 59% of smokers, 47% of excess drinkers, 49% of those with dietary risk factors and 32% of inactive patients claimed to have adopted healthier behaviours within the past 3 months. Older subjects and those with a lower standard of living were less likely to acknowledge risks, and those who did were less likely to report improving their lifestyles. While 71% of patients recalled receiving lifestyle advice, the coverage and targeting of specific interventions was generally poor. Overall, 60% of the sample had received advice on weight control, 47% on diet, 38% on exercise, 38% on smoking and 36% on alcohol. Women and older people were less likely to be given relevant counseling, and there was no evidence of targeting with respect to subjects' social class, level of hypertension or duration of diagnosis. CONCLUSION: Lifestyle interventions are welcomed and are viewed as helpful by patients receiving them. Potential health gains among high-risk hypertensives are being lost because of poor targeting and coverage of those at greatest risk.
Full text
PDF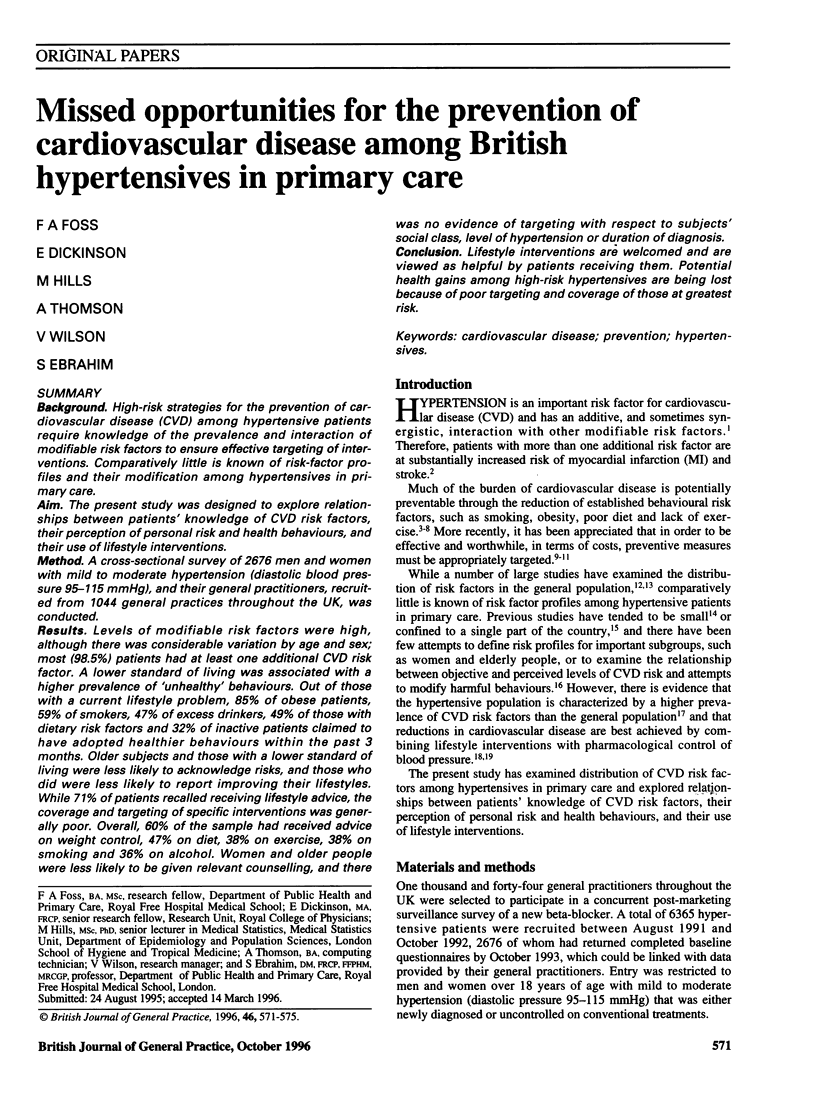
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anggard E. E., Land J. M., Lenihan C. J., Packard C. J., Percy M. J., Ritchie L. D., Shepherd J. Prevention of cardiovascular disease in general practice: a proposed model. Br Med J (Clin Res Ed) 1986 Jul 19;293(6540):177–180. doi: 10.1136/bmj.293.6540.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field K., Thorogood M., Silagy C., Normand C., O'Neill C., Muir J. Strategies for reducing coronary risk factors in primary care: which is most cost effective? BMJ. 1995 Apr 29;310(6987):1109–1112. doi: 10.1136/bmj.310.6987.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjermann I., Velve Byre K., Holme I., Leren P. Effect of diet and smoking intervention on the incidence of coronary heart disease. Report from the Oslo Study Group of a randomised trial in healthy men. Lancet. 1981 Dec 12;2(8259):1303–1310. doi: 10.1016/s0140-6736(81)91338-6. [DOI] [PubMed] [Google Scholar]
- Kannel W. B. Role of blood pressure in cardiovascular morbidity and mortality. Prog Cardiovasc Dis. 1974 Jul-Aug;17(1):5–24. doi: 10.1016/0033-0620(74)90034-6. [DOI] [PubMed] [Google Scholar]
- Kurji K. H., Haines A. P. Detection and management of hypertension in general practices in north west London. Br Med J (Clin Res Ed) 1984 Mar 24;288(6421):903–906. doi: 10.1136/bmj.288.6421.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mant D., McKinlay C., Fuller A., Randall T., Fullard E. M., Muir J. Three year follow up of patients with raised blood pressure identified at health checks in general practice. BMJ. 1989 May 20;298(6684):1360–1362. doi: 10.1136/bmj.298.6684.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morisky D. E., Levine D. M., Green L. W., Shapiro S., Russell R. P., Smith C. R. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983 Feb;73(2):153–162. doi: 10.2105/ajph.73.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulter N. Management of multiple risk factors for coronary heart disease in patients with hypertension. Am Heart J. 1991 Jan;121(1 Pt 2):246–250. doi: 10.1016/0002-8703(91)90851-8. [DOI] [PubMed] [Google Scholar]
- Rowland L., Dickinson E. J., Newman P., Ford D., Ebrahim S. Look After Your Heart programme: impact on health status, exercise knowledge, attitudes, and behaviour of retired women in England. J Epidemiol Community Health. 1994 Apr;48(2):123–128. doi: 10.1136/jech.48.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper A. G., Pocock S. J., Phillips A. N., Walker M. Identifying men at high risk of heart attacks: strategy for use in general practice. Br Med J (Clin Res Ed) 1986 Aug 23;293(6545):474–479. doi: 10.1136/bmj.293.6545.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper A. G., Pocock S. J., Walker M., Cohen N. M., Wale C. J., Thomson A. G. British Regional Heart Study: cardiovascular risk factors in middle-aged men in 24 towns. Br Med J (Clin Res Ed) 1981 Jul 18;283(6285):179–186. doi: 10.1136/bmj.283.6285.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silagy C., Muir J., Coulter A., Thorogood M., Roe L. Cardiovascular risk and attitudes to lifestyle: what do patients think? BMJ. 1993 Jun 19;306(6893):1657–1660. doi: 10.1136/bmj.306.6893.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelmsen L., Berglund G., Elmfeldt D., Tibblin G., Wedel H., Pennert K., Vedin A., Wilhelmsson C., Werkö L. The multifactor primary prevention trial in Göteborg, Sweden. Eur Heart J. 1986 Apr;7(4):279–288. doi: 10.1093/oxfordjournals.eurheartj.a062065. [DOI] [PubMed] [Google Scholar]


