Abstract
Background
Thrombolytic therapy is indicated for patients with ST-segment elevation myocardial infarction (STEMI) presenting >120 minutes from a percutaneous coronary intervention–capable facility. Timely transfer is critical in thrombolytic failure.
Case Summary
A 46-year-old woman presented to a rural emergency department with an anterior STEMI. Thrombolytics failed. Transfer was delayed because of a snowstorm. She arrived at our facility hours later in cardiogenic shock. She was treated with rescue percutaneous coronary intervention and initiation of mechanical circulatory support with a percutaneous transvalvular microaxial flow pump. She ultimately recovered and has done well on follow-up.
Discussion
The patient presented to the emergency department promptly and was appropriately treated in a timely manner. However, geographic isolation and inclement weather posed insurmountable and potentially life-threatening delays in care.
Take-Home Messages
Rural-urban health disparities can complicate the STEMI pathway. Prompt recognition and treatment of thrombolytic failure and cardiogenic shock is critical to patient outcomes.
Key words: acute coronary syndrome, acute heart failure, cardiomyopathy, coronary angiography, percutaneous coronary intervention, reduced ejection fraction
Graphical Abstract
History of Presentation
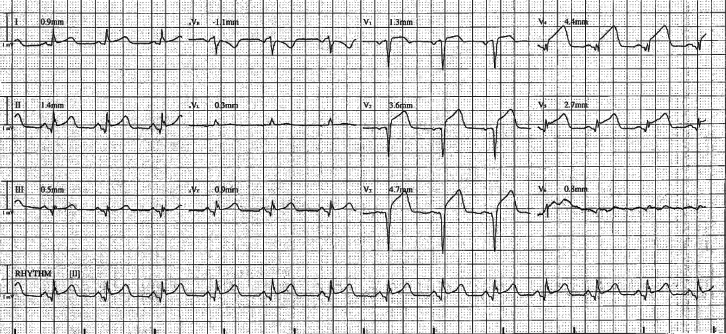
A 46-year-old woman was having dinner with her wife when she experienced sudden onset of chest discomfort. She presented to the emergency department at an outlying facility approximately 20 minutes later. An electrocardiogram (ECG) was obtained immediately on arrival which demonstrated an anterior ST-segment elevation myocardial infarction (STEMI) (Figure 1). Being the nearest percutaneous coronary intervention (PCI)–capable facility, our service was emergently contacted. The patient was >100 miles away in the mountains and would require >2 hours for transfer. Thus, she was promptly administered thrombolytic therapy with tenecteplase 45 mg intravenously, loading dose aspirin and clopidogrel, and a heparin bolus followed by drip. She continued to experience persistent ischemic symptoms. Serial ECGs demonstrated persistent ST-segment elevations (Figure 2).
Take-Home Messages
-
•
This case highlights the ways in which rural-urban health disparities can complicate the management of ST-segment elevation myocardial infarction.
-
•
This case furthermore highlights the importance of prompt recognition and treatment of patients with ST-segment elevation myocardial infarction presenting >120 minutes from a PCI capable facility, thrombolytic failure, and cardiogenic shock.
Figure 1.
Initial Electrocardiogram
Presenting electrocardiogram obtained at outside facility demonstrating anterior ST-segment elevation myocardial infarction.
Figure 2.
Serial Electrocardiogram
Follow-up electrocardiogram obtained at outside facility after administration of thrombolytics demonstrating persistent ST-segment elevations.
Unfortunately, a blizzard had blanketed Southern Colorado in several feet of snow. The mountain passes were frozen, and flights were grounded because of ongoing blizzards and poor visibility. Multiple attempts were made throughout the night to transfer the patient to our facility. However, neither flight nor ground transportation was an option because of the weather. The patient was stranded, and she was infarcting.
Our team remained in constant contact with the outlying facility regarding the patient's condition and estimated time of arrival. Finally, approximately 15 hours after symptom onset, the patient arrived via helicopter.
The patient arrived awake, alert, and understandably anxious. She had persistent mild to moderate chest pain despite narcotics administered during transfer. She was tachycardic and hypotensive.
Past Medical History
The patient had a personal history of type 2 diabetes mellitus, and a family history of early coronary artery disease.
Differential Diagnosis
The patient was assessed as having an anterior STEMI with failed thrombolytic therapy, now with cardiogenic shock. Mechanical complications of myocardial infarction were ruled out with a transthoracic echocardiogram.
Investigations
The patient was brought directly to the cardiac catheterization laboratory for emergent coronary angiography. Transthoracic echocardiogram demonstrated a left ventricular ejection fraction (LVEF) of 35% to 40% and anterior, anteroseptal, and apical wall akinesis (Video 1, Video 2, Video 3).
Management
The culprit lesion was identified in the mid-left anterior descending (LAD) (Videos 4 and 5). Flow was immediately restored with balloon angioplasty. The lesion was stented with a 3.00- × 38-mm drug-eluting stent. TIMI flow grade 2 was thereafter noted. Aspiration thrombectomy was performed along with administration of intracoronary adenosine and nitroglycerin. TIMI flow grade 3 was restored (Video 6).
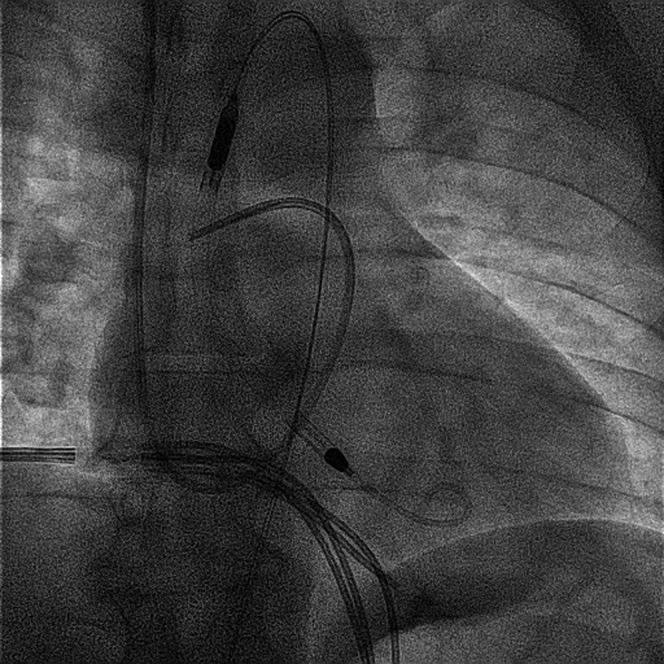
Hemodynamic data obtained via right heart catheterization included a pulmonary capillary wedge pressure of 18 mm Hg, a Fick cardiac index of 1.7 L/min/m2, and a cardiac power output of 0.5 W. Mechanical circulatory support was initiated with a percutaneous transvalvular microaxial flow pump (Figure 3). After initiation of mechanical circulatory support, right heart catheterization demonstrated a right atrial pressure of 4 mm Hg, a right ventricular pressure of 26/4 mm Hg, a pulmonary artery pressure of 26/12 mm Hg with a mean pulmonary arterial pressure of 14 mm Hg, and a pulmonary capillary wedge pressure of 14 mm Hg, with a cardiac output of 5.6 L/min and cardiac index of 2.8 L/min/m2 by Fick's method. The Swan-Ganz catheter was secured in the right internal jugular vein.
Figure 3.
Fluoroscopy After Swan-Ganz Catheter and Percutaneous Transvalvular Microaxial Flow Pump Placement
Fluoroscopic image after percutaneous coronary intervention showing Swan-Ganz catheter and mechanical circulatory support in place.
She was maintained on mechanical circulatory support in the cardiovascular intensive care unit for several days thereafter. Because her hemodynamics improved and her cardiogenic shock resolved, the psychological burden of her condition became more apparent. She was previously functional at baseline. She attended concerts regularly and was looking forward to attending a show the following month. She was extensively counseled regarding her diagnosis and provided with emotional support while working toward weaning her mechanical support.
Outcome and Follow-Up
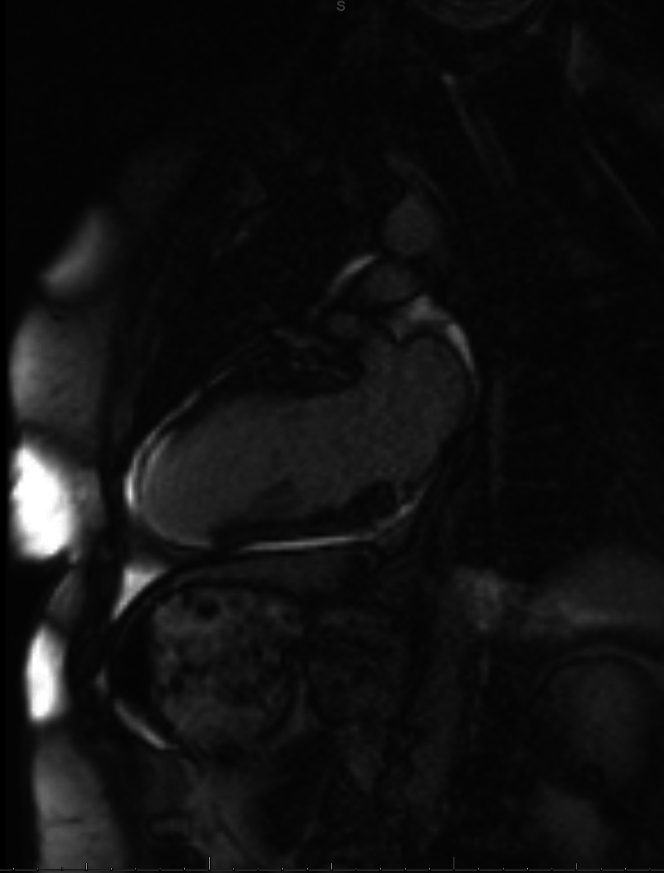
The patient's shock state resolved, and mechanical circulatory support was discontinued after 4 days. At the time of explant, she had a central venous pressure of 8 mm Hg and a pulmonary artery pressure of 29/18 mm Hg with a mean pulmonary arterial pressure of 24 mm Hg, with a Fick's cardiac output of 6.4 L/min and cardiac index of 3.3 L/min/m2. She tolerated introduction of guideline-directed medical therapies. A week after her initial presentation, she was discharged home. She participated in cardiac rehabilitation. A cardiac magnetic resonance obtained a few months later demonstrated LVEF of 50% with extensive infarction in the LAD territory (Figures 4 and 5, Videos 7 and 8). She continues to do well clinically and has moved forward with her life, working and attending concerts again.
Figure 4.
Late Gadolinium Enhancement Imaging From Cardiac Magnetic Resonance in Apical 2-Chamber View
Image from cardiac magnetic resonance in apical 2-chamber view demonstrating extensive late gadolinium enhancement uptake involving the mid- and distal segments of the anterior septum, inferoseptum, extending to apical anterior, apical inferior segment, in a transmural fashion, indicative of prior region of myocardial infarction without residual viability.
Figure 5.
Late Gadolinium Enhancement Imaging From Cardiac Magnetic Resonance in Short-Axis View
Image from cardiac magnetic resonance in short-axis view demonstrating extensive late gadolinium enhancement uptake involving the mid- and distal segments of the anterior septum, inferoseptum, extending to apical anterior, apical inferior segment, in a transmural fashion, indicative of prior region of myocardial infarction without residual viability.
Discussion
We present the case of a woman who presented promptly for care. She was triaged and treated appropriately on presentation to a rural facility. An ECG was obtained within 10 minutes of arrival to the outside facility emergency department. Noting no contraindications, thrombolytic therapy was administered well within 30 minutes of arrival. She was loaded on aspirin and clopidogrel, provided with a heparin bolus, and continued on a heparin drip pending revascularization. Arrangements were made to transfer the patient. Given ongoing ischemic symptoms and persistent ST-segment elevations after thrombolytics, the team was prepared to bring the patient directly to the cardiac catheterization laboratory for rescue PCI. However, the transfer was delayed by weather conditions. Options for further therapy were unfortunately limited pending the patient's arrival at our facility.
Conclusions
The patient faced insurmountable delays because of inclement weather and geographic challenges posed by harsh terrain. The patients' case highlights the critical responsibility which we have in assessing our patients quickly and correctly while maintaining robust systems of care.
Visual Summary.
Timeline for Hospitalization
| Date | Events |
|---|---|
| Day 1 | A 46-year-old woman presented to the emergency department at an outlying facility. ECG showed anterior ST-segment elevation myocardial infarction. The patient failed thrombolytic therapy. Transfer was delayed because of inclement weather. |
| Day 2 | The patient arrived to PCI-capable facility by helicopter 15 h after initial presentation. Rescue PCI was performed. A Swan-Ganz catheter was placed, and hemodynamic support was initiated with a percutaneous transvalvular microaxial flow pump. |
| Day 3-4 | The patient was monitored in the CVICU. |
| Day 5 | The microaxial flow pump was discontinued, and Swan-Ganz catheter was removed. |
| Day 6 | Patient was noted to be ambulating around the unit and tolerated initiation of GDMT. |
| Day 7 | Patient was discharged home in stable condition and referred to cardiac rehabilitation. |
| Follow-up | Patient continues to do well clinically. CMR demonstrated recovered LVEF. |
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
For supplemental videos, please see the online version of this paper.
Appendix
Transthoracic Echocardiogram in the Apical 4-Chamber View
Transthoracic echocardiogram with contrast in the apical 4-chamber view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Transthoracic Echocardiogram in the Parasternal Long-Axis View
Transthoracic echocardiogram with contrast in the parasternal long-axis view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Transthoracic Echocardiogram in the Parasternal Short-Axis View
Transthoracic echocardiogram with contrast in the parasternal short-axis view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Diagnostic Coronary Angiography
Coronary angiogram demonstrating occlusion of the culprit vessel in the midsegment of the left anterior descending in the AP cranial view. AP = antero-posterior.
Diagnostic Coronary Angiography
Coronary angiography demonstrating occlusion of the culprit vessel in the midsegment of the left anterior descending in the AP caudal view. AP = antero-posterior.
Coronary Angiography After Percutaneous Coronary Intervention to the Midsegment of the Left Anterior Descending Artery
Coronary angiography demonstrating restoration of TIMI flow grade 3 after percutaneous coronary intervention to the midsegment of the left anterior descending artery in the AP cranial view. AP = antero-posterior.
Cardiac Magnetic Resonance Demonstrating Recovered Left Ventricular Ejection Fraction in the 2-Chamber View
Cardiac magnetic resonance demonstrating a left ventricular ejection fraction of 50% with extensive infarction in the left anterior descending artery territory in the 2-chamber view.
Cardiac Magnetic Resonance Demonstrating Recovered Left Ventricular Ejection Fraction in the Short-Axis View
Cardiac magnetic resonance demonstrating a left ventricular ejection fraction of 50% with extensive infarction in the left anterior descending artery territory in the short-axis view.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic Echocardiogram in the Apical 4-Chamber View
Transthoracic echocardiogram with contrast in the apical 4-chamber view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Transthoracic Echocardiogram in the Parasternal Long-Axis View
Transthoracic echocardiogram with contrast in the parasternal long-axis view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Transthoracic Echocardiogram in the Parasternal Short-Axis View
Transthoracic echocardiogram with contrast in the parasternal short-axis view demonstrating a left ventricular ejection fraction of 35% to 40% and anterior, anteroseptal, and apical wall akinesis.
Diagnostic Coronary Angiography
Coronary angiogram demonstrating occlusion of the culprit vessel in the midsegment of the left anterior descending in the AP cranial view. AP = antero-posterior.
Diagnostic Coronary Angiography
Coronary angiography demonstrating occlusion of the culprit vessel in the midsegment of the left anterior descending in the AP caudal view. AP = antero-posterior.
Coronary Angiography After Percutaneous Coronary Intervention to the Midsegment of the Left Anterior Descending Artery
Coronary angiography demonstrating restoration of TIMI flow grade 3 after percutaneous coronary intervention to the midsegment of the left anterior descending artery in the AP cranial view. AP = antero-posterior.
Cardiac Magnetic Resonance Demonstrating Recovered Left Ventricular Ejection Fraction in the 2-Chamber View
Cardiac magnetic resonance demonstrating a left ventricular ejection fraction of 50% with extensive infarction in the left anterior descending artery territory in the 2-chamber view.
Cardiac Magnetic Resonance Demonstrating Recovered Left Ventricular Ejection Fraction in the Short-Axis View
Cardiac magnetic resonance demonstrating a left ventricular ejection fraction of 50% with extensive infarction in the left anterior descending artery territory in the short-axis view.